Abstract
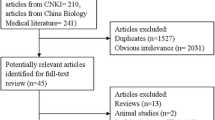
Urolithiasis is a common, highly recurrent disease with increasing prevalence worldwide. The association between vitamin D and calcium stones has often been investigated on the basis of the role of vitamin D in calcium homeostasis. Currently, there is no consensus on the management of vitamin D deficiency in patients with renal calculi, because of controversies about the relationship between vitamin D and calcium stones. However, the vitamin D deficiency is shown to be highly prevalent among kidney stone formers, and some studies found a higher prevalence in stone formers compared with non-stone formers. This article attempts to review the relationship between calcium stones and vitamin D, and propose a mechanism for the association between vitamin D deficiency and calcium-based calculi according to the substantial role of inflammation and oxidative stress in calcium stone formation and also the pro-inflammatory effect of vitamin D deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcium (Ca) stones, including calcium oxalate (CaOX) and calcium phosphate (CaP) stones, are the most prevalent type of kidney stones in most countries around the world [1,2,3]. Although many studies have attempted to find the risk factors and pathogenesis of the disease, several shortcomings are left in clarifying the pathophysiology of Ca stones, especially CaOX stones [4]. In this context, growing number of evidence has considered CaOX urolithiasis as a systemic disease, which is associated with other chronic conditions such as hypertension, cardiovascular disease, metabolic syndrome, and diabetes mellitus [5,6,7]. There are some hypotheses for such associations. One of the suggested theories is based on the studies which found an association between dietary factors and kidney stones. These studies suggest that this association could be explained by common dietary habits, like fewer fruits and vegetables and more red meat, which are common risk factors for the kidney stone formation and other chronic diseases [8]. Another hypothesis is the development of oxidative stress and related inflammation [9]. It is suggested that oxidative stress, which is a common risk factor for many chronic diseases, could cause tubular injury which results in crystal retention in renal tubules and stone formation [9].
Vitamin D deficiency has been known as a major health problem globally [10]. Vitamin D plays a critical role in calcium and phosphorus balance and bone health, and its deficiency has a deleterious effect on this context. Vitamin D deficiency causes decreased absorption of dietary calcium, low bone mass, and secondary hyperparathyroidism [11, 12]. In addition to this well-known role, the relationship between vitamin D deficiency and different chronic diseases such as cardiovascular disease [13], hypertension [14], insulin resistance, diabetes mellitus, metabolic syndrome [15, 16], and various cancers [17] has been assessed in several studies; however there are some controversies in their results [18]. It is suggested that the effect of vitamin D on the immune system, inflammatory status [19], and oxidative stress [20] is the basis for such relation.
The association between vitamin D and kidney stone have often been investigated on the basis of the role of vitamin D in calcium homeostasis. Currently, there is no consensus on the management of vitamin D deficiency in patients with kidney stones, because of controversies about the relationship between vitamin D and calcium-based calculi [21]. However, vitamin D deficiency was shown to be highly prevalent among kidney stone formers [22, 23], and some studies found a higher prevalence in stone formers compared with non-stone formers [24, 25]. This article attempts to review the relationship between Ca stones and vitamin D, and propose a mechanism for the association between vitamin D deficiency and CaOX kidney stone formation.
Deposition of calcium salts in the kidneys
Deposition of Ca in the kidneys may occur in the renal parenchyma (nephrocalcinosis), or renal tubules (calcium kidney stones) [26]. Nephrocalcinosis is generalized renal parenchymal calcification and includes both CaOX and CaP deposits [27, 28]. Nephrocalcinosis is classified into molecular, microscopic, and macroscopic calcifications [27]. Molecular nephrocalcinosis is defined as an increase in intracellular calcium concentration, which cannot be detected by microscopic or radiographic assessments [28]. In microscopic nephrocalcinosis, the calcium deposits could be detected by light microscopic examination or biopsy, but no evidence of calcification is seen in radiographic imaging. In macroscopic nephrocalcinosis, the calcifications are visible in plain abdominal X-ray [28]. Molecular nephrocalcinosis is reversed upon correction of the underlying risk factors. However, both microscopic and macroscopic nephrocalcinosis are associated with kidney injury [27, 28].
Nephrocalcinosis involves the renal medulla in most of the cases and rarely the cortex [28]. The most common risk factor for nephrocalcinosis is an increase in the urinary excretion of calcium. Other common risk factors of nephrocalcinosis are increase in the urinary excretion of phosphate and oxalate [29]. These metabolic abnormalities are also closely associated with kidney stones. However, the specific mechanism resulting in nephrocalcinosis progression rather than stone formation is elusive [28]. Nephrocalcinosis is a more severe condition and usually implies a serious metabolic defect such as primary hyperparathyroidism, distal renal tubular acidosis, and medullary sponge kidney disease [27, 30].
Calcium kidney stones
Ca stones are mainly consisted of CaOX (50%), CaP (5%), and mixtures of both compositions (45%) [1]. CaOX stones may contain different forms of crystal. The main crystal forms are CaOX monohydrate (COM) and CaOX dihydrate (COD), or a combination of both. COM is the most stable form of the crystals and is more frequently observed than COD in calcium stone formers [1]. Different factors may cause the formation of COM or COD crystals, e.g., formation of urinary COD crystals is predominantly associated with a high urinary calcium concentration, whereas formation of COM crystals is predominantly associated with a high oxalate concentration in urine [31].
Mechanisms for calcium stone formation
Renal stone formation or biomineralization is a complex process and has several steps, including urine supersaturation, crystal nucleation, growth and aggregation of crystals, and crystal retention in the kidney. Since some of the steps, such as urine supersaturation, may also develop in the normal population, there is a great controversy regarding the key step in the stone formation process [32]. All stones share similar events with respect to the mineral phase of stone formation. However, the sequence of events leading to stone formation differs depending on the stone composition, biochemistry of the urine, and the initial location of stone material precipitation [1].
According to various evidence such as human renal tissue biopsies and intra-operative endourologic imaging, different mechanisms have been developed to elucidate how the process of stone formation starts and proceeds in the urinary tract. The most considered mechanisms in this context are (1) free solution crystallization (free-particle), (2) crystal deposition in renal tubules (fixed-particle), and (3) overgrowth on interstitial CaP plaques (Randall’s plaque) [33] (Fig. 1). However, it should be kept in mind that no single model could explain the stone formation and probably all these models contribute to this process [34].
The three mechanisms of kidney stone formation. (1) Free solution crystallization (free-particle), (2) crystal deposition in renal tubules (fixed-particle), and (3) overgrowth on interstitial calcium phosphate plaques (Randall’s plaque). The figure is adapted from [36]
The first essential step in the stone formation process is the increased supersaturation of stone-forming salts, responsible for the process of crystal nucleation and formation [32]. ‘Free-particle theory’ emphasizes the role of the highly saturated urine as the cornerstone of the process of the kidney stone formation [4, 35]. The theory indicates that the nucleation, formation, and aggregation of crystals occur within the supersaturated urine of the renal tubules or within the calyces or renal collecting system, without attachment to the tubular cells [34, 36]. The higher the degree of supersaturation, the more driving force for crystallization [34]. This mechanism is probably involved in the formation of cystine, uric acid, and CaOX stones associated with primary and enteric hyperoxaluria [34, 37].
The ‘Fixed-particle theory’ suggests that because of the short transit time of tubular fluid through the kidney, free particles cannot grow fast enough to cause stone disease in the upper urinary tract, and ‘crystal retention’ is the mandatory step in the stone formation [38]. The retention is caused by the attachment of crystals to the luminal side of the renal tubular cells or endocytosis of crystals by these cells [32]. The attachment of the crystals to the cells creates fixed nuclei which could interact with the supersaturated urinary environment and result in crystal growth [2, 32, 39].
Normally, there are some protective mechanisms, such as macromolecule production in tubules that inhibit crystal adhesion or endocytosis [40]. However, renal cell injury could interrupt these protective mechanisms. The injury could promote crystal retention in the tubules and upgrade numerous molecules on the tubular cells which could readily attach to crystals [32, 38, 41, 42]. The injured cells have more affinity for COM crystals than COD crystals [1]. Moreover, crystal nucleation could occur at lower supersaturation in the presence of renal epithelial injury [43].
Different factors could cause tubular cell injury. CaOX crystals, high urinary oxalate concentrations, or even physiological concentrations of oxalate could cause renal epithelial cell injury [32, 41, 44, 45]. It is suggested that oxidative stress and inflammatory response caused by cell injury is responsible for the retention of the crystals in renal tubules [32].
The last theory discusses the role of subepithelial-calcified plaques known as Randall’s plaque in stone formation. This theory believes that idiopathic calcium oxalate stones are formed attached to this calcified plaques on the papillary surface [34] (Fig. 1).
Randall’s plaques are crystalline deposits of interstitial CaP [36]. The plaques originate in the basement membranes of the thin loops of Henle, collecting ducts, or vasa recta [46]. Some of these plaques become very dense and appear to spread through the surrounding interstitium [47] to beneath the urothelium [46]. The spreading plaques then move through the interstitium toward the renal papillary epithelium, where they ulcerate to the surface [48], and become a place for CaOX crystal attachment [49].
Randall’s plaques are specific to CaOX stone formers, who have no systemic or bowel diseases [46]. Several risk factors and mechanisms are suggested to be responsible for plaque formation. Hypercalciuria and low urine volume are found to be risk factors for plaque formation in the interstitium [50]. One suggested mechanism is the vascular theory for the formation of Randall’s plaque [51]. This theory is based on the findings which found the association of Randall’s plaques with collagen and membrane-bound vesicles, which is similar to pathologic vascular calcification [52]. This hypothesis is in line with the association found between cardiovascular disease and urolithiasis [6].
A recent hypothesis for the formation of Randall’s plaques is the probable role of oxidative stress and inflammation in the formation of Randall’s plaques [48]. Some in vitro and experimental studies suggested that plaque formation is triggered by oxidative stress and related inflammatory responses [48]. A recent study which compared the gene expression of Randall’s plaques with the surrounding tissue in the kidney of CaOX stone formers found activation of genes associated with oxidative stress and inflammation in Randall’s plaques [53]. This hypothesis is also in line with the association found between chronic diseases and urolithiasis [9].
Role of oxidative stress and inflammation in urinary stone formation
Reactive oxygen species (ROS) are highly reactive chemical agents, including free radicals, atoms, or molecules with unpaired electrons. They are produced in the human body in many physiological signaling and regulatory pathways, such as the mitochondrial respiratory chain. Various enzymes, including nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, xanthine oxidase, and other active oxidases, are involved in their production [54, 55].
The conditions of ROS overproduction or decreased antioxidant status are called oxidative stress [54]. The oxidative stress could damage or modify cellular proteins. These changes in cellular proteins could activate transcription factors responsible for the regulation of immune system and inflammation. All of these transcription factors are known to have a role in the pathogenesis of many chronic diseases, such as cardiovascular disease and hypertension [9].
In vitro and animal studies demonstrated that crystal retention is mediated by the excess generation of ROS and consequent oxidative stress and inflammation. Both oxalate and CaOX crystals can cause cell injury that activates NADPH oxidase, which results in ROS production [41]. Oxalate could also activate renin–angiotensin–aldosterone system (RAAS). Hyperoxaluric rats were shown to have higher renin and angiotensin ΙΙ gene expressions [56, 57]. RAAS independently stimulates NADPH oxidase and ROS production [56]. Finally, the produced ROS stimulate transcription factors like mitogen-activated protein (MAP) kinase, c-Jun N-terminal kinase [58, 59], and the nuclear factor-κB (NFκB) [60] which are all factors responsible for the regulation of immune system and inflammation. The activation of these transcription factors enhances the expression of adhesion molecules, such as hyaluronan, CD44, osteopontin, and monocyte chemoattractant protein-1 (MCP-1), on injured cells [42, 61]. Finally, the crystals adhere to these adhesion molecules and result in the retention of crystals in the kidney [42].
Consistent with the above-mentioned findings, human cross-sectional studies revealed elevated oxidative stress markers in the urine and kidney tissues adjacent to the stones in renal lithiasis patients [62,63,64]. Furthermore, adhesion molecules such as MCP-1 [65] and vascular cell adhesion molecule-1 [66] are shown to be elevated in the serum of kidney stone patients compared to healthy controls. Higher oxidative stress was shown to be associated with larger stone size and more renal tubular damage [67, 68].
As mentioned earlier, oxidative stress and inflammation are suggested to have a role in Randall’s plaque formation [48, 53]. CaP deposits in the interstitium are considered as foreign bodies by the adjacent cells and trigger these cells to generate ROS and produce adhesion molecules such as MCP-1 and osteopontin [53]. Persistent formation of CaP deposits causes local injury and inflammation, followed by fibrosis and collagen deposition and mineralization around the CaP crystal deposits, which leads to plaque growth [48].
The effectiveness of anti-inflammatory agents and antioxidants in preventing crystal retention is shown in in vitro and animal studies [69,70,71,72,73]. However, their effect on preventing human nephrolithiasis has been assessed in limited observational studies [74]. Further randomized controlled trials in this context are warranted.
Vitamin D and its role in calcium metabolism and chronic diseases
Vitamin D is a fat-soluble vitamin, which primarily has been considered as an essential element for establishing and maintaining bone structure. Since average human diet is not rich in vitamin D and humans have to rely on the endogenous production of the vitamin in the UVB-exposed skin, it has been known as a hormone [19, 75].
The vitamin D got from the diet or produced in the skin is metabolized first in the liver to make 25-hydroxyvitamin D, and then in the kidney to make 1,25-dihydroxy vitamin D, which is the final biologically active form of the vitamin D. The renal production of 1,25-dihydroxy vitamin D is tightly regulated mainly by serum parathyroid hormone (PTH), calcium, and phosphorus levels, and 1,25-dihydroxy vitamin D itself [76]. Although 1,25-dihydroxy vitamin D is the active form of the vitamin, 25-hydroxyvitamin D is the major circulating form of vitamin D and is the best index for the body stores of vitamin D [11, 77]. Vitamin D deficiency is defined by low circulatory 25-hydroxyvitamin D [10]. The Endocrine Society recommended that vitamin D deficiency to be defined as a 25(OH)D level of 20 ng/mL or less, vitamin D insufficiency as 21–29 ng/mL, and vitamin D sufficiency as 30 ng/mL or greater for children and adults [77].
The receptor for 1,25-dihydroxy vitamin D, which is called vitamin D receptor (VDR), is located in the cell nucleus and found in most of the tissues, such as intestine, bones, kidneys, muscles, cells, and organs of the immune system and fat tissue [12, 19]. The wide distribution of VDR in the body was the basis to find out the physiological roles of the vitamin D beyond bone tissue mineralization [17, 75] and the relationship between vitamin D deficiency and different chronic inflammatory diseases [13, 14, 16].
The absorption of renal and intestinal calcium is increased in the presence of 1,25-dihydroxy vitamin D [12]. Vitamin D deficiency decreases the efficiency of intestinal calcium absorption, which results in an increase in PTH levels, called secondary hyperparathyroidism [77]. Secondary hyperparathyroidism maintains serum calcium in the normal range at the expense of mobilizing calcium from the skeleton and increasing calcium resorption from the kidneys [77]. This process results in normal blood levels for calcium and a low 24-h urine calcium excretion rate [78]. Serum 1,25-dihydroxy vitamin D is frequently either normal or even elevated in those with vitamin D deficiency, due to secondary hyperparathyroidism [77]. Increased levels of PTH and low 24-h urine calcium levels should prompt suspicion for vitamin D deficiency in some patient [78].
In the context of the relationship between vitamin D and chronic diseases, vitamin D deficiency has been found to be a risk factor for cardiovascular disease [13]. The association between vitamin D deficiency and chronic diseases like diabetes mellitus, metabolic syndrome, hypertension, and different cancers has been shown in observational studies [15,16,17, 79]; however, clinical trials that studied the effect of vitamin D supplementation on these diseases had controversial results [14, 80]. Although Institute of Medicine (IOM) did not confirm these health outcomes of vitamin D in its 2011 report because of the controversies in the studies [18], recent meta-analyses reported that favorable effects of vitamin D in some of these chronic diseases such as diabetes mellitus are probable [79, 81]. Moreover, a comprehensive review on the findings from meta-analyses summarizing non-skeletal health effects of vitamin D supplementation concluded that most of the studies included both patients with low and normal vitamin D levels for the levels for the supplementation of the vitamin D and this may be the reason for controversial results of the clinical trials [82].
The probable association between vitamin D deficiency and chronic disease could be explained by the modulating effect of vitamin D on the immune system, inflammation [17], and oxidative stress [20]. Increasing evidence indicates that vitamin D is involved in different cellular inflammatory and antioxidant pathways [83]. Vitamin D acts as a steroid hormone by regulating expression of inflammatory genes [17, 83]. It has been found that vitamin D inhibits the production of pro-inflammatory cytokines like interleukin 6 or tumor necrosis factor alpha by inhibiting MAP kinase [84, 85]. Furthermore, activation of VDR has been shown to inhibit NF-κB activation and reduce expression of adhesion molecules such as MCP-1 [86].
The relationship between vitamin D and oxidative stress may also be explained by the potential link between vitamin D and RAAS [14]. Vitamin D-deficient patients were found to have more active RAAS and higher Angiotensin ΙΙ levels [14, 87]. In vitro and animal studies have shown that VDR activation by vitamin D inhibits renin gene transcription [88,89,90], which could suppress oxidative stress [91, 92]. However, clinical trials that studied the effect of vitamin D supplementation on plasma renin had conflicting results [93, 94].
Vitamin D and kidney stone: the current knowledge and a proposal
The association between vitamin D and kidney stone has often been investigated considering the role of vitamin D in calcium homeostasis. Vitamin D intoxication can lead to hypercalciuria and formation of CaOX stoned [95], mainly consisted of COD crystals. In the terms of normal serum vitamin D or vitamin D deficiency, the results of the studies on the relationship between 25-hydroxyvitamin D and kidney stone formation risk are conflicting. Therefore, physicians hesitate to treat vitamin D deficiency in urolithiasis patients [21]. Different observational studies and few clinical trials had tried to find an association between serum vitamin D and risk of kidney stones or assessed the effect of vitamin D supplementation on the kidney stone formation without including patients with toxic serum levels of 25-hydroxyvitamin D. A recent meta-analysis of observational studies showed that the serum levels of 25-hydroxyvitamin D were the same between stone formers and non-stone formers [96], whereas hypercalciuric stone formers had higher serum levels of 25-hydroxyvitamin D, compared with normocalciuria stone patients and non-stone formers. The results also revealed that the serum levels of 1,25-dihydroxy vitamin D were higher in stone formers compared with non-stone formers. The authors discussed that higher serum levels of 1,25-dihydroxy vitamin D could be the result of VDR gene polymorphisms or genetic mutations in genes that control 1,25-dihydroxy vitamin D catabolism. Other recent meta-analysis showed that although long-term vitamin D supplementation resulted in increased risks of hypercalcemia and hypercalciuria, it did not increase the risk of kidney stones [97]. A non-controlled clinical trial on stone formers with vitamin D deficiency showed that intaking 50,000 IU vitamin D for 8 weeks did not increase urinary levels of calcium [98]. Another randomized clinical trial, investigating the effect of low-dose and high-dose vitamin D supplementation (receiving 1000 IU daily or 50,000 IU weekly of vitamin D for 6 weeks, respectively) in stone formers with vitamin D deficiency, also showed that vitamin D supplementation did not increase urine calcium excretion or calcium oxalate supersaturation [99]. Despite insufficient evidence about the safety of vitamin D supplementation in kidney stone patients with vitamin D deficiency, the recent edition of Canadian Urological Association guideline on the evaluation and medical management of the kidney stone patient recommends treating vitamin D deficiency in urolithiasis patients, with monitoring for hypercalciuria [100]. The guideline also suggests that more clinical trials in this field are warranted [100].
Contrary to the traditional hypothesis regarding the role of higher serum 25-hydroxyvitamin D in kidney stone formation, hypovitaminosis D may also exacerbate kidney stone formation or severity. Some recent studies showed a considerable prevalence of vitamin D deficiency in stone formers [22, 101], and even higher prevalence of vitamin D deficiency in stone formers compared with non-stone formers [24, 25]. Different explanations for such probable association could be provided:
-
Secondary hyperparathyroidism in the vitamin D-deficient group has been suggested as a reason for the higher risk of kidney stone in this group [25]. However, as it is mentioned earlier, secondary hyperparathyroidism often results in low 24-h urine calcium excretion rate and not accompanied by hypercalciuria [78, 102]. More studies should assess this hypothesis.
-
Another proposal may be the similar risk factors for vitamin D deficiency and kidney stone formation. Some major risk factors for vitamin D deficiency are living at higher latitudes, older age, female sex, low socioeconomic status, malnutrition, and obesity [10, 12, 80]; among them obesity is the only common risk factor. Some dietary risk factors are also hypothesized as risk factors for vitamin D deficiency [103]. These suggested dietary factors include decreased dietary calcium level, high dietary consumption of phytates, and low dietary intake of animal proteins [103]. Among them decreased dietary calcium level is the common risk factor. Decreased dietary calcium level is suggested to increase serum PTH level and also catabolism of 25-hydroxyvitamin D and finally may cause vitamin D deficiency [103]. More studies in this field are needed to elucidate this proposal.
-
According to the findings regarding the relationship between vitamin D and inflammation, we propose that the correlation between calcium stones and vitamin D deficiency may result from the role of vitamin D deficiency in inducing oxidative stress and inflammation in kidney tissue (Fig. 2). As mentioned earlier, vitamin D has been shown to modulate transcription factors responsible for the regulation of inflammation, such as NFκB and MAP kinase, and also adhesion molecules such as MCP-1 [84,85,86]. Since all these mediators are shown to play a role in kidney stone pathogenesis [41, 58,59,60], we propose that vitamin D deficiency increases the risk of kidney stone formation by overexpression of these inflammatory mediators. This condition is consistent with the formation of COM rather than COD crystals.
Schematic representation of the fixed-particle and Randall’s plaque pathways for stone formation and the proposed mechanism for the potential association between vitamin D deficiency and calcium oxalate nephrolithiasis. Since vitamin D has been shown to modulate inflammation and oxidative stress by inhibiting transcription factors (A) and also may inhibit renin gene transcription (B), the authors propose that vitamin D deficiency may exacerbate kidney stone formation or severity by inducing tubular inflammation and oxidative stress. JNK c-Jun N-terminal kinase, MAP kinase mitogen-activated protein kinase, MCP-1 monocyte chemoattractant protein-1, NADPH oxidase nicotinamide adenine dinucleotide phosphate oxidase, NFκB nuclear factor-κB, ROS reactive oxygen species
In the context of inflammation and oxidative stress, the relationship between vitamin D deficiency and kidney stone could also be discussed by the potential effect of vitamin D on RAAS (Fig. 2). RAAS activation by vitamin D deficiency increases NADPH oxidase activity and raises ROS production consequently [91, 92]. Since RAAS activation is shown to play a role in kidney stone formation by increasing oxidative stress and crystal retention, the potential effect of vitamin D deficiency on RAAS is also proposed as a casualty for the relationship between vitamin D deficiency and kidney stone.
Conclusion
Although higher serum vitamin D was previously considered as a risk factor for Ca stone formation, vitamin D deficiency may also exacerbate kidney stone formation or severity. The suggested mechanisms for this association are secondary hyperparathyroidism and the similar risk factors for vitamin D deficiency and Ca stone formation. Since vitamin D deficiency has been shown to cause inflammation and oxidative stress, the authors propose that the correlation between CaOX urolithiasis and vitamin D deficiency may result from the role of vitamin D deficiency in inducing oxidative stress and inflammation in kidney tissue. Further studies are warranted to assess this proposal.
References
Alelign T, Petros B (2018) Kidney stone disease: an update on current concepts. Adv Urol https://doi.org/10.1155/2018/3068365
Knoll T (2010) Epidemiology, pathogenesis, and pathophysiology of urolithiasis. Eur Urol Suppl 9(12):802–806. https://doi.org/10.1016/j.eursup.2010.11.006
Hosseini MM, Shakeri S, Manaheji F, Aminsharifi A, Ezatzadegan S, Pakfetrat M, Basiratnia M, Hosseini M (2014) Stone composition in patients who undergo renal stone surgery: review of 423 stone analyses in southern Iran. Iran J Med Sci 39(1):75–76
Tiselius HG (2011) A hypothesis of calcium stone formation: an interpretation of stone research during the past decades. Urol Res 39(4):231–243. https://doi.org/10.1007/s00240-010-0349-3
West B, Luke A, Durazo-Arvizu RA, Cao G, Shoham D, Kramer H (2008) Metabolic syndrome and self-reported history of kidney stones: the National Health and Nutrition Examination Survey (NHANES III) 1988–1994. Am J Kidney Dis 51(5):741–747. https://doi.org/10.1053/j.ajkd.2007.12.030
Kohjimoto Y, Sasaki Y, Iguchi M, Matsumura N, Inagaki T, Hara I (2013) Association of metabolic syndrome traits and severity of kidney stones: results from a nationwide survey on urolithiasis in Japan. Am J Kidney Dis 61(6):923–929. https://doi.org/10.1053/j.ajkd.2012.12.028
Polat EC, Ozcan L, Cakir SS, Dursun M, Otunctemur A, Ozbek E (2015) Relationship between calcium stone disease and metabolic syndrome. Urol J 12(6):2391–2395
Lieske JC (2014) New insights regarding the interrelationship of obesity, diet, physical activity, and kidney stones. J Am Soc Nephrol 25(2):211–212. https://doi.org/10.1681/asn.2013111189
Khan SR (2012) Is oxidative stress, a link between nephrolithiasis and obesity, hypertension, diabetes, chronic kidney disease, metabolic syndrome? Urol Res 40(2):95–112. https://doi.org/10.1007/s00240-011-0448-9
Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, El-Hajj Fuleihan G, Josse RG, Lips P, Morales-Torres J, Group IOFCoSANW (2009) Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 20(11):1807–1820. https://doi.org/10.1007/s00198-009-0954-6
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22(4):477–501. https://doi.org/10.1210/edrv.22.4.0437
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281. https://doi.org/10.1056/NEJMra070553
Kendrick J, Targher G, Smits G, Chonchol M (2009) 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis 205(1):255–260. https://doi.org/10.1016/j.atherosclerosis.2008.10.033
Carbone F, Mach F, Vuilleumier N, Montecucco F (2014) Potential pathophysiological role for the vitamin D deficiency in essential hypertension. World J Cardiol 6(5):260–276. https://doi.org/10.4330/wjc.v6.i5.260
Prasad P, Kochhar A (2016) Interplay of vitamin D and metabolic syndrome: a review. Diabetes Metab Syndr 10:105–112. https://doi.org/10.1016/j.dsx.2015.02.014
Chiu KC, Chu A, Go VL, Saad MF (2004) Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 79(5):820–825
Moukayed M, Grant WB (2013) Molecular link between vitamin D and cancer prevention. Nutrients 5(10):3993–4021. https://doi.org/10.3390/nu5103993
IOM (Institute of Medicine) (2011) Dietary reference Intakes for calcium and vitamin D. National Academies Press, US, Washington, D. C. https://doi.org/10.17226/13050
Carlberg C (2014) The physiology of vitamin D-far more than calcium and bone. Front Physiol 5:335. https://doi.org/10.3389/fphys.2014.00335
Sharifi N, Amani R, Hajiani E, Cheraghian B (2014) Does vitamin D improve liver enzymes, oxidative stress, and inflammatory biomarkers in adults with non-alcoholic fatty liver disease? a randomized clinical trial. Endocrine 47(1):70–80. https://doi.org/10.1007/s12020-014-0336-5
Tang J, Chonchol MB (2013) Vitamin D and kidney stone disease. Curr Opin Nephrol Hypertens 22(4):383–389. https://doi.org/10.1097/MNH.0b013e328360bbcd
Elkoushy MA, Sabbagh R, Unikowsky B, Andonian S (2012) Prevalence and metabolic abnormalities of vitamin D-inadequate patients presenting with urolithiasis to a tertiary stone clinic. Urology 79(4):781–785. https://doi.org/10.1016/j.urology.2011.09.004
Johri N, Jaeger P, Ferraro PM, Shavit L, Nair D, Robertson WG, Gambaro G, Unwin RJ (2017) Vitamin D deficiency is prevalent among idiopathic stone formers, but does correction pose any risk? Urolithiasis 45:535–543
Ticinesi A, Nouvenne A, Ferraro PM, Folesani G, Lauretani F, Allegri F, Guerra A, Cerundolo N, Aloe R, Lippi G, Maggio M, Gambaro G, Borghi L, Meschi T (2016) Idiopathic calcium nephrolithiasis and hypovitaminosis D: a case-control study. Urology 87:40–45. https://doi.org/10.1016/j.urology.2015.10.009
Giron-Prieto MS, Del Carmen Cano-Garcia M, Arrabal-Polo MA, Poyatos-Andujar A, Quesada-Charneco M, de Haro-Munoz T, Arias-Santiago S, Arrabal-Martin M (2016) Analysis of vitamin D deficiency in calcium stone-forming patients. Int Urol Nephrol. https://doi.org/10.1007/s11255-016-1290-3
Vestergaard P (2015) Primary hyperparathyroidism and nephrolithiasis. Ann Endocrinol (Paris) 76(2):116–119. https://doi.org/10.1016/j.ando.2015.03.002
Sayer JA, Carr G, Simmons NL (2004) Nephrocalcinosis: molecular insights into calcium precipitation within the kidney. Clin Sci (Lond) 106(6):549–561. https://doi.org/10.1042/cs20040048
Shavit L, Jaeger P, Unwin RJ (2015) What is nephrocalcinosis? Kidney Int 88(1):35–43. https://doi.org/10.1038/ki.2015.76
Oliveira B, Kleta R, Bockenhauer D, Walsh SB (2016) Genetic, pathophysiological, and clinical aspects of nephrocalcinosis. Am J Physiol Renal Physiol 311(6):F1243–Ff1252. https://doi.org/10.1152/ajprenal.00211.2016
Bhojani N, Paonessa JE, Hameed TA, Worcester EM, Evan AP, Coe FL, Borofsky MS, Lingeman JE (2015) Nephrocalcinosis in calcium stone formers who do not have systemic disease. J Urol 194(5):1308–1312. https://doi.org/10.1016/j.juro.2015.05.074
Daudon M, Letavernier E, Frochot V, Haymann JP, Bazin D, Jungers P (2016) Respective influence of calcium and oxalate urine concentration on the formation of calcium oxalate monohydrate or dihydrate crystals. C R Chim 19(11–12):1504–1513. https://doi.org/10.1016/j.crci.2016.08.009
Tsujihata M (2008) Mechanism of calcium oxalate renal stone formation and renal tubular cell injury. Int J Urol 15(2):115–120. https://doi.org/10.1111/j.1442-2042.2007.01953.x
Coe FL, Evan AP, Worcester EM, Lingeman JE (2010) Three pathways for human kidney stone formation. Urol Res 38(3):147–160. https://doi.org/10.1007/s00240-010-0271-8
Khan SR, Pearle MS, Robertson WG, Gambaro G, Canales BK, Doizi S, Traxer O, Tiselius HG (2016) Kidney stones. Nat Rev Dis Primers 2:16008. https://doi.org/10.1038/nrdp.2016.8
Kok DJ, Khan SR (1994) Calcium oxalate nephrolithiasis, a free or fixed particle disease. Kidney Int 46(3):847–854
Evan AP (2010) Physiopathology and etiology of stone formation in the kidney and the urinary tract. Pediatr Nephrol 25(5):831–841. https://doi.org/10.1007/s00467-009-1116-y
Evan AP, Worcester EM, Coe FL, Williams J Jr, Lingeman JE (2015) Mechanisms of human kidney stone formation. Urolithiasis 43(Suppl 1):19–32. https://doi.org/10.1007/s00240-014-0701-0
Verkoelen CF (2006) Crystal retention in renal stone disease: a crucial role for the glycosaminoglycan hyaluronan? J Am Soc Nephrol 17(6):1673–1687. https://doi.org/10.1681/ASN.2006010088
Sakhaee K (2009) Recent advances in the pathophysiology of nephrolithiasis. Kidney Int 75(6):585–595. https://doi.org/10.1038/ki.2008.626
Wiessner JH, Hung LY, Mandel NS (2003) Crystal attachment to injured renal collecting duct cells: influence of urine proteins and pH. Kidney Int 63(4):1313–1320. https://doi.org/10.1046/j.1523-1755.2003.00866.x
Umekawa T, Iguchi M, Uemura H, Khan SR (2006) Oxalate ions and calcium oxalate crystal-induced up-regulation of osteopontin and monocyte chemoattractant protein-1 in renal fibroblasts. BJU Int 98(3):656–660. https://doi.org/10.1111/j.1464-410X.2006.06334.x
Asselman M, Verhulst A, De Broe ME, Verkoelen CF (2003) Calcium oxalate crystal adherence to hyaluronan-, osteopontin-, and CD44-expressing injured/regenerating tubular epithelial cells in rat kidneys. J Am Soc Nephrol 14(12):3155–3166
Khan SR (2006) Renal tubular damage/dysfunction: key to the formation of kidney stones. Urol Res 34(2):86–91. https://doi.org/10.1007/s00240-005-0016-2
Thamilselvan V, Menon M, Thamilselvan S (2009) Oxalate-induced activation of PKC-alpha and -delta regulates NADPH oxidase-mediated oxidative injury in renal tubular epithelial cells. Am J Physiol Renal Physiol 297(5):F1399–F1410. https://doi.org/10.1152/ajprenal.00051.2009
Thamilselvan V, Menon M, Thamilselvan S (2014) Oxalate at physiological urine concentrations induces oxidative injury in renal epithelial cells: effect of alpha-tocopherol and ascorbic acid. BJU Int. https://doi.org/10.1111/bju.12642
Evan AP, Lingeman JE, Coe FL, Parks JH, Bledsoe SB, Shao Y, Sommer AJ, Paterson RF, Kuo RL, Grynpas M (2003) Randall’s plaque of patients with nephrolithiasis begins in basement membranes of thin loops of Henle. J Clin Invest 111(5):607–616. https://doi.org/10.1172/JCI200317038
Evan A, Lingeman J, Coe FL, Worcester E (2006) Randall’s plaque: pathogenesis and role in calcium oxalate nephrolithiasis. Kidney Int 69(8):1313–1318. https://doi.org/10.1038/sj.ki.5000238
Khan SR (2013) Reactive oxygen species as the molecular modulators of calcium oxalate kidney stone formation: evidence from clinical and experimental investigations. J Urol 189(3):803–811. https://doi.org/10.1016/j.juro.2012.05.078
Evan AP, Coe FL, Lingeman JE, Shao Y, Sommer AJ, Bledsoe SB, Anderson JC, Worcester EM (2007) Mechanism of formation of human calcium oxalate renal stones on Randall’s plaque. Anat Rec (Hoboken) 290(10):1315–1323. https://doi.org/10.1002/ar.20580
Kuo RL, Lingeman JE, Evan AP, Paterson RF, Parks JH, Bledsoe SB, Munch LC, Coe FL (2003) Urine calcium and volume predict coverage of renal papilla by Randall’s plaque. Kidney Int 64(6):2150–2154. https://doi.org/10.1046/j.1523-1755.2003.00316.x
Taylor ER, Stoller ML (2015) Vascular theory of the formation of Randall plaques. Urolithiasis 43(Suppl 1):41–45. https://doi.org/10.1007/s00240-014-0718-4
Khan SR, Rodriguez DE, Gower LB, Monga M (2012) Association of Randall plaque with collagen fibers and membrane vesicles. J Urol 187(3):1094–1100. https://doi.org/10.1016/j.juro.2011.10.125
Taguchi K, Hamamoto S, Okada A, Unno R, Kamisawa H, Naiki T, Ando R, Mizuno K, Kawai N, Tozawa K, Kohri K, Yasui T (2017) Genome-wide gene expression profiling of Randall’s plaques in calcium oxalate stone formers. J Am Soc Nephrol 28(1):333–347. https://doi.org/10.1681/asn.2015111271
Joshi S, Peck AB, Khan SR (2013) NADPH oxidase as a therapeutic target for oxalate induced injury in kidneys. Oxid Med Cell Longev. https://doi.org/10.1155/2013/462361
Khan SR (2014) Reactive oxygen species, inflammation and calcium oxalate nephrolithiasis. Transl Androl Urol 3(3):256–276. https://doi.org/10.3978/j.issn.2223-4683.2014.06.04
Tsuji H, Wang W, Sunil J, Shimizu N, Yoshimura K, Uemura H, Peck AB, Khan SR (2016) Involvement of renin-angiotensin-aldosterone system in calcium oxalate crystal induced activation of NADPH oxidase and renal cell injury. World J Urol 34(1):89–95. https://doi.org/10.1007/s00345-015-1563-y
Umekawa T, Hatanaka Y, Kurita T, Khan SR (2004) Effect of angiotensin II receptor blockage on osteopontin expression and calcium oxalate crystal deposition in rat kidneys. J Am Soc Nephrol 15(3):635–644
Chaturvedi LS, Koul S, Sekhon A, Bhandari A, Menon M, Koul HK (2002) Oxalate selectively activates p38 mitogen-activated protein kinase and c-Jun N-terminal kinase signal transduction pathways in renal epithelial cells. J Biol Chem 277(15):13321–13330. https://doi.org/10.1074/jbc.M108203200
Han HJ, Lim MJ, Lee YJ (2004) Oxalate inhibits renal proximal tubule cell proliferation via oxidative stress, p38 MAPK/JNK, and cPLA2 signaling pathways. Am J Physiol Cell Physiol 287(4):C1058–C1066. https://doi.org/10.1152/ajpcell.00063.2004
Tugcu V, Ozbek E, Kemahli E, Cekmen MB, Caner N, Somay A, Erturkuner P, Seckin I, Demir CG, Altug T, Tasci AI (2007) Rapid communication: protective effect of a nuclear factor kappaB inhibitor, pyrolidium dithiocarbamate, in the kidney of rats with nephrolithiasis induced by ethylene glycol. J Endourol 21(9):1097–1106. https://doi.org/10.1089/end.2007.0074
Umekawa T, Tsuji H, Uemura H, Khan SR (2009) Superoxide from NADPH oxidase as second messenger for the expression of osteopontin and monocyte chemoattractant protein-1 in renal epithelial cells exposed to calcium oxalate crystals. BJU Int 104(1):115–120. https://doi.org/10.1111/j.1464-410X.2009.08374.x
Carrasco-Valiente J, Anglada-Curado FJ, Aguilar-Melero P, Gonzalez-Ojeda R, Muntane-Relat J, Padillo-Ruiz FJ, Requena-Tapia MJ (2012) State of acute phase markers and oxidative stress in patients with kidney stones in the urinary tract. Actas Urol Esp 36(5):296–301. https://doi.org/10.1016/j.acuro.2011.08.004
Huang HS, Ma MC, Chen CF, Chen J (2003) Lipid peroxidation and its correlations with urinary levels of oxalate, citric acid, and osteopontin in patients with renal calcium oxalate stones. Urology 62(6):1123–1128
Kittikowit W, Waiwijit U, Boonla C, Ruangvejvorachai P, Pimratana C, Predanon C, Ratchanon S, Tosukhowong P (2014) Increased oxidative DNA damage seen in renal biopsies adjacent stones in patients with nephrolithiasis. Urolithiasis 42(5):387–394. https://doi.org/10.1007/s00240-014-0676-x
Liu Z, Wang T, Yang J, Wang S, Yang W, Liu J, Ye Z (2012) Calcium oxalate monohydrate crystals stimulate monocyte chemoattractant protein-1 and transforming growth factor beta1 expression in human renal epithelial cells. Mol Med Rep 5(5):1241–1244. https://doi.org/10.3892/mmr.2012.813
Tsao KC, Wu TL, Chang PY, Sun CF, Wu LL, Wu JT (2007) Multiple risk markers for atherogenesis associated with chronic inflammation are detectable in patients with renal stones. J Clin Lab Anal 21(6):426–431. https://doi.org/10.1002/jcla.20215
Boonla C, Wunsuwan R, Tungsanga K, Tosukhowong P (2007) Urinary 8-hydroxydeoxyguanosine is elevated in patients with nephrolithiasis. Urol Res 35(4):185–191. https://doi.org/10.1007/s00240-007-0098-0
Ma MC, Chen YS, Huang HS (2014) Erythrocyte oxidative stress in patients with calcium oxalate stones correlates with stone size and renal tubular damage. Urology 83(2):510, e519–e517. https://doi.org/10.1016/j.urology.2013.09.050
Fujii Y, Okada A, Yasui T, Niimi K, Hamamoto S, Hirose M, Kubota Y, Tozawa K, Hayashi Y, Kohri K (2013) Effect of adiponectin on kidney crystal formation in metabolic syndrome model mice via inhibition of inflammation and apoptosis. PLoS ONE 8(4):e61343. https://doi.org/10.1371/journal.pone.0061343
Hong SH, Lee HJ, Sohn EJ, Ko HS, Shim BS, Ahn KS, Kim SH (2013) Anti-nephrolithic potential of resveratrol via inhibition of ROS, MCP-1, hyaluronan and osteopontin in vitro and in vivo. Pharmacol Rep 65(4):970–979
Huang HS, Chen J, Chen CF, Ma MC (2006) Vitamin E attenuates crystal formation in rat kidneys: roles of renal tubular cell death and crystallization inhibitors. Kidney Int 70(4):699–710. https://doi.org/10.1038/sj.ki.5001651
Lee HJ, Jeong SJ, Park MN, Linnes M, Han HJ, Kim JH, Lieske JC, Kim SH (2012) Gallotannin suppresses calcium oxalate crystal binding and oxalate-induced oxidative stress in renal epithelial cells. Biol Pharm Bull 35(4):539–544
Davalos M, Konno S, Eshghi M, Choudhury M (2010) Oxidative renal cell injury induced by calcium oxalate crystal and renoprotection with antioxidants: a possible role of oxidative stress in nephrolithiasis. J Endourol 24(3):339–345. https://doi.org/10.1089/end.2009.0205
Holoch PA, Tracy CR (2011) Antioxidants and self-reported history of kidney stones: the National Health and Nutrition Examination Survey. J Endourol 25(12):1903–1908. https://doi.org/10.1089/end.2011.0130
DeLuca HF (2004) Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr 80(6 Suppl):1689s–1696s
Hossein-nezhad A, Holick MF (2013) Vitamin D for health: a global perspective. Mayo Clin Proc 88(7):720–755. https://doi.org/10.1016/j.mayocp.2013.05.011
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine S (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930. https://doi.org/10.1210/jc.2011-0385
Kennel KA, Drake MT, Hurley DL (2010) Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc 85(8):752–758. https://doi.org/10.4065/mcp.2010.0138
Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP (2014) Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ 348:g2035. https://doi.org/10.1136/bmj.g2035
Beveridge LA, Struthers AD, Khan F, Jorde R, Scragg R, Macdonald HM, Alvarez JA, Boxer RS, Dalbeni A, Gepner AD, Isbel NM, Larsen T, Nagpal J, Petchey WG, Stricker H, Strobel F, Tangpricha V, Toxqui L, Vaquero MP, Wamberg L, Zittermann A, Witham MD (2015) Effect of Vitamin D supplementation on blood pressure: a systematic review and meta-analysis incorporating individual patient data. JAMA Intern Med 175(5):745–754. https://doi.org/10.1001/jamainternmed.2015.0237
Wu C, Qiu S, Zhu X, Li L (2017) Vitamin D supplementation and glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Metabolism 73:67–76. https://doi.org/10.1016/j.metabol.2017.05.006
Rejnmark L, Bislev LS, Cashman KD, Eiriksdottir G, Gaksch M, Grubler M, Grimnes G, Gudnason V, Lips P, Pilz S, van Schoor NM, Kiely M, Jorde R (2017) Non-skeletal health effects of vitamin D supplementation: a systematic review on findings from meta-analyses summarizing trial data. PLoS ONE 12(7):e0180512. https://doi.org/10.1371/journal.pone.0180512
Wobke TK, Sorg BL, Steinhilber D (2014) Vitamin D in inflammatory diseases. Front Physiol 5:244. https://doi.org/10.3389/fphys.2014.00244
Zhang Y, Leung DY, Richers BN, Liu Y, Remigio LK, Riches DW, Goleva E (2012) Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1. J Immunol 188(5):2127–2135. https://doi.org/10.4049/jimmunol.1102412
Jain SK, Micinski D (2013) Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem Biophys Res Commun 437(1):7–11. https://doi.org/10.1016/j.bbrc.2013.06.004
Sanchez-Nino MD, Bozic M, Cordoba-Lanus E, Valcheva P, Gracia O, Ibarz M, Fernandez E, Navarro-Gonzalez JF, Ortiz A, Valdivielso JM (2012) Beyond proteinuria: VDR activation reduces renal inflammation in experimental diabetic nephropathy. Am J Physiol Renal Physiol 302(6):F647–F657. https://doi.org/10.1152/ajprenal.00090.2011
Perez-Hernandez N, Aptilon-Duque G, Nostroza-Hernandez MC, Vargas-Alarcon G, Rodriguez-Perez JM, Blachman-Braun R (2016) Vitamin D and its effects on cardiovascular diseases: a comprehensive review. Korean J Intern Med 31(6):1018–1029. https://doi.org/10.3904/kjim.2015.224
Yuan W, Pan W, Kong J, Zheng W, Szeto FL, Wong KE, Cohen R, Klopot A, Zhang Z, Li YC (2007) 1,25-dihydroxyvitamin D3 suppresses renin gene transcription by blocking the activity of the cyclic AMP response element in the renin gene promoter. J Biol Chem 282(41):29821–29830. https://doi.org/10.1074/jbc.M705495200
Weng S, Sprague JE, Oh J, Riek AE, Chin K, Garcia M, Bernal-Mizrachi C (2013) Vitamin D deficiency induces high blood pressure and accelerates atherosclerosis in mice. PLoS ONE 8(1):e54625. https://doi.org/10.1371/journal.pone.0054625
Kong J, Zhu X, Shi Y, Liu T, Chen Y, Bhan I, Zhao Q, Thadhani R, Li YC (2013) VDR attenuates acute lung injury by blocking Ang-2-Tie-2 pathway and renin-angiotensin system. Mol Endocrinol 27(12):2116–2125. https://doi.org/10.1210/me.2013-1146
Deng X, Cheng J, Shen M (2016) Vitamin D improves diabetic nephropathy in rats by inhibiting renin and relieving oxidative stress. J Endocrinol Invest 39(6):657–666. https://doi.org/10.1007/s40618-015-0414-4
Garcia IM, Altamirano L, Mazzei L, Fornes M, Cuello-Carrion FD, Ferder L, Manucha W (2014) Vitamin D receptor-modulated Hsp70/AT1 expression may protect the kidneys of SHRs at the structural and functional levels. Cell Stress Chaperones 19(4):479–491. https://doi.org/10.1007/s12192-013-0474-3
Carrara D, Bernini M, Bacca A, Rugani I, Duranti E, Virdis A, Ghiadoni L, Taddei S, Bernini G (2014) Cholecalciferol administration blunts the systemic renin-angiotensin system in essential hypertensives with hypovitaminosis D. J Renin Angiotensin Aldosterone Syst 15(1):82–87. https://doi.org/10.1177/1470320312471149
Bernini G, Carrara D, Bacca A, Carli V, Virdis A, Rugani I, Duranti E, Ghiadoni L, Bernini M, Taddei S (2013) Effect of acute and chronic vitamin D administration on systemic renin angiotensin system in essential hypertensives and controls. J Endocrinol Invest 36(4):216–220. https://doi.org/10.1007/bf03347275
Ozkan B, Hatun S, Bereket A (2012) Vitamin D intoxication. Turk J Pediatr 54(2):93–98
Hu H, Zhang J, Lu Y, Zhang Z, Qin B, Gao H, Wang Y, Zhu J, Wang Q, Zhu Y, Xun Y, Wang S (2017) Association between circulating vitamin D level and urolithiasis: a systematic review and meta-analysis. Nutrients 9(3):E301. https://doi.org/10.3390/nu9030301
Malihi Z, Wu Z, Stewart AW, Lawes CM, Scragg R (2016) Hypercalcemia, hypercalciuria, and kidney stones in long-term studies of vitamin D supplementation: a systematic review and meta-analysis. Am J Clin Nutr 104(4):1039–1051. https://doi.org/10.3945/ajcn.116.134981
Leaf DE, Korets R, Taylor EN, Tang J, Asplin JR, Goldfarb DS, Gupta M, Curhan GC (2012) Effect of vitamin D repletion on urinary calcium excretion among kidney stone formers. Clin J Am Soc Nephrol 7(5):829–834. https://doi.org/10.2215/CJN.11331111
Ferroni MC, Rycyna KJ, Averch TD, Semins MJ (2017) Vitamin D repletion in kidney stone formers: a randomized controlled trial. J Urol 197(4):1079–1083. https://doi.org/10.1016/j.juro.2016.10.057
Dion M, Ankawi G, Chew B, Paterson R, Sultan N, Hoddinott P, Razvi H (2016) CUA guideline on the evaluation and medical management of the kidney stone patient: 2016 update. Can Urol Assoc J 10(11–12):E347–E358. https://doi.org/10.5489/cuaj.4218
Pipili C, Oreopoulos DG (2012) Vitamin D status in patients with recurrent kidney stones. Nephron Clin Pract 122(3–4):134–138. https://doi.org/10.1159/000351377
Girón-prieto MS, Del Carmen Cano-garcía M, Arrabal-polo M, Poyatos-andujar A, Quesada-charneco M, de Haro-Muñoz T, Arias-santiago S, Arrabal-martín M (2016) Analysis of vitamin D deficiency in calcium stone-forming patients. Int Urol Nephrol 48(8):1243–1246. https://doi.org/10.1007/s11255-016-1290-3
Hashemipour S, Larijani B, Adibi H, Javadi E, Sedaghat M, Pajouhi M, Soltani A, Shafaei AR, Hamidi Z, Fard AR, Hossein-Nezhad A, Booya F (2004) Vitamin D deficiency and causative factors in the population of Tehran. BMC Public Health 4:38. https://doi.org/10.1186/1471-2458-4-38
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant interests to declare.
Rights and permissions
About this article
Cite this article
Tavasoli, S., Taheri, M. Vitamin D and calcium kidney stones: a review and a proposal. Int Urol Nephrol 51, 101–111 (2019). https://doi.org/10.1007/s11255-018-1965-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-018-1965-z