Abstract
Introduction and objectives
Reactive oxygen species (ROS) are produced during the interaction between oxalate/calcium oxalate monohydrate (COM) crystals and renal epithelial cells and are responsible for the various cellular responses through the activation of NADPH oxidase (Nox). Ox and COM also activate the renin–angiotensin–aldosterone system (RAAS). Aldosterone stimulates ROS production through activation of Nox with the involvement of mineralocorticoid receptor (MR), Rac1 and mitogen-activated protein kinases (MAPK). We investigated RAAS pathways in vivo in an animal model of hyperoxaluria and in vitro by exposing renal epithelial cells to COM crystals.
Methods
Hyperoxaluria was induced in male SD rats by administering ethylene glycol. One group of rats was additionally given spironolactone. Total RNA was extracted and subjected to genomic microarrays to obtain global transcriptome data. Normal rat kidney cell line (NRK-52E) was incubated with aldosterone(10−7 M) and COM(67 μg/cm2) with or without spironolactone(10−5 M), a selective inhibitor of SRC family of kinases; protein phosphatase 2(pp2) (10−5 M) and Nox inhibitor; diphenylene iodonium (DPI) (10−5 M).
Results
Relative expression of genes encoding for AGT, angiotensin receptors 1b and 2, Renin 1, Cyp11b, HSD11B2, Nr3c2, NOx4 and Rac1 was upregulated in the kidneys of rats with hyperoxaluria. Treatment with spironolactone reversed the effect of hyperoxaluria. Both aldosterone and COM crystals activated Nox and Rac1 expression in NRK52E, while spironolactone inhibited Nox and Rac1 expression. Increased Rac1 expression was significantly attenuated by treatment with PP2 and spironolactone.
Conclusions
Results indicate that hyperoxaluria-induced production of ROS, injury and inflammation are in part associated with the activation of Nox through renin–angiotensin–aldosterone pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcium oxalate (CaOx) is the major constituent of most kidney stones, and hyperoxaluria is one of the major risk factor for idiopathic urinary stone formation. Renal epithelial cells are injured by exposure to high oxalate and/or CaOx crystals, and injury is associated with development of oxidative stress and the production of reactive oxygen species (ROS). ROS are produced from many sources and involve a variety of signaling pathways. Nicotinamide adenine dinucleotide phosphate (NADPH) oxidase is the most important source of receptor-mediated ROS production during exposure to high oxalate and CaOx crystal–cell interaction. We previously demonstrated that NADPH oxidase is involved in the generation of free radicals causing gene upregulation and increased production of several urinary macromolecules, which modulate the nucleation, growth, aggregation and retention of crystals in the kidneys. It represents a second messenger system for induction of molecules such as monocyte chemoattractant-1 (MCP-1) and osteopontin (OPN) in renal epithelial cells exposed to CaOx crystals [1]. OPN and MCP-1 lead the recruitment of monocytes/macrophages to the renal interstitium during initial stages of crystal deposition and urinary stone formation. It has been shown that ROS production through the activation of NADPH oxidase is stimulated by aldosterone with the involvement of mineralocorticoid receptor (MR), Ras-related C3 botulinum toxin substrate 1 (Rac1) and mitogen-activated protein kinases (MAPK) [2–5]. Several reports of renal calculi in association with primary hyperaldosteronism have also been published [6, 7]. Both in vivo and in vitro studies have indicated the potential role of aldosterone and MR in the pathogenesis of renal injury [8, 9]. The renal damage is associated with activation of MAPKs through c-Src-dependent pathway in aldosterone-infused rat model study. A selective MR antagonist, eplerenone, prevented aldosterone-induced increases in ROS levels and MAPK activity and ameliorated renal injury.
It is our hypothesis that COM crystal-induced activation of NADPH oxidase involves renin–angiotensin–aldosterone system (RAAS). Exposure of renal epithelial cells to COM crystals leads to upregulation of genes encoding the membrane and cytosolic units of NADPH oxidase [10, 11]. The activation appears to occur via angiotensin II/angiotensin II receptor-2 pathway [10]. Exposure leads to the production of various molecules including OPN which can be inhibited by blocking the angiotensin receptor [12]. NADPH oxidase is involved in the generation of free radicals which may represent a second messenger system for the induction of molecules such as MCP-1 and OPN in renal epithelial cell exposed to calcium oxalate crystals [1]. It was revealed that the efficacy of NOx inhibitor apocynin treatment in reducing the production of ROS associated renal injury and crystal deposition in the kidneys of hyperoxaluria rat model [13]. To continue investigating RAAS involvement in hyperoxaluria-induced activation of NADPH oxidase and subsequent injury and inflammation, we examined the relative expression of genes encoding for angiotensinogen (AGT), angiotensin receptors 2 and 1b (AGTr2, 1b), Renin 1 (Ren 1), aldosterone synthase (Cyp11b), corticosteroid 11-beta-dehydrogenase isozyme 2 (HSD11B2), MR (Nr3c2), Nox4, SOD-1 and Rac1 in vivo in the kidneys of rats with hyperoxaluria. Renin acts upon AGT to produce angiotensin which activates angiotensin receptors and mediates the production of aldosterone. Aldosterone binds to MR and stimulates the formation of ROS through increased expression of Nox2 and Nox 4 subunits of NADPH oxidase. The new point of this study is presented above gene expressions by spironolactone (MR inhibitor) treatment in hyperoxaluria rat model. We also studied the effect of inhibiting MR, SRC family of kinases and NADPH oxidase on its activation in vitro in tissue culture.
NRK52E rat renal epithelial cells were exposed in culture to aldosterone or COM crystals with or without spironolactone, a competitive antagonist of MR; diphenylene iodonium (DPI), an inhibitor of NADPH oxidase; or protein phosphatase 2 (PP2), a selective inhibitor of SRC family of kinases.
Materials and methods
Animal model
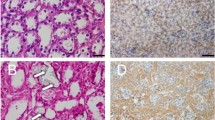
Eight-week- old, male Sprague-Dawley rats (n = 60), with average weight of about 110–120 grams, were bought from Harlan Laboratories (Harlan, Tampa, Florida). The rats were allowed to accustom for 2 weeks within the animal care facilities at University of Florida before any experimental procedures and prior to start their dietary regimen. Rats were divided into three groups (n = 5). Group 1 rats (control) were fed normal rat chow and sterile water. Group 2 rats had a similar diet to Group 1 and were additionally given 1.25 % ethylene glycol (EG) in drinking water. Group 3 rats were given EG in drinking water and 15 mg/kg/day of spironolactone mixed in rat chow. The rats were placed in metabolic cages for urine collection 1 day before killing and killed on day 28, and their kidneys were extracted.
One kidney was carefully divided into cortex and medulla and was stored in RNA later solution at −20° for RNA isolation and at −80° for protein isolation. The other kidney was cut into parts and was also kept in formalin to be embedded in paraffin for histological analysis. All the experimental procedures were approved by the University of Florida’s IACUC and were in accord with the recommendations of the NIH Guide for the Care and Use of Laboratory Animals. The volume, pH, protein and blood in the urine were also recorded.
Microscopic analyses, RNA extraction and differential expression of genes by microarray analyses were carried out as previously described. The total RNA from each of the different specimens was isolated from cortex and medulla of each rat within the three different treatment groups using the RNeasy Mini Kit (Qiagen, Valencia, CA), as per the manufacturer’s instructions and described in our previous study. The microarray analysis was done in the Interdisciplinary Center for Biotechnology Research (ICBR), University of Florida, using the Agilent 8 × 60 k single-color arrays under the Agilent microarray incentive program. The data analysis was done using the Bioconductor Limma (Linear models for microarray analysis) package using R. Before the analysis, the individual signal intensity values retrieved from the microarray probes were log-transformed (using 2 as a base), and normalization was done for all the individual samples within all the groups in this study. After normalizing the signal intensity values for each of the arrays, the Student’s t test was used to do a probe-by-probe comparison between two groups concurrently. For each comparison, the fold change (FC) and P value were calculated for each gene based on the n = 4 replicate samples within each experimental group and heat map, raw data box plot and relative log expression (RLE), and volcano plots were drawn for each comparison.
Cell culture
Aldosterone, spironolactone, pp2 and DPI were purchased from Sigma-Aldrich Corporation (Sigma, St.Lous, USA). Rac1 activation assay Biochem kit was obtained from Cytoskeleton, Inc., Denver, USA (cat. #BK035). Normal rat kidney epithelial cell line, NRK-52E (CRL-1571; Manassas, VA, USA), was obtained from American Type Culture Collection and cultured according to their recommendations. These cells were routinely sub-cultured by treatment with 0.05 % trypsin and 0.02 % EDTA. They were maintained as continuously growing monolayers in 100-mm culture dish in 1:1 ratio Dulbecco’s modified F-12 (DMEM/F-12, Gibco cat. #26010032) containing 4 % newborn calf serum, 2 % antibiotic–antimycotic solution (Sigma cat. #A5955) at 37 °C in a 5 % CO2 air atmosphere incubator. When cells achieved 80 % confluence, they were washed with serum and sodium pyruvate-free DMEM/F-12 media and incubated for 24 h under serum starvation to lead to much greater response to a given Rac1 activation. We evaluated superoxide anion level using the cell-permeable dye dihydroethidium (DHE), and 1 × 105/ml cells were seeded and cultured on Lab-Tek™ II chambered coverglass (cat. #155382) and 100-mm dish. The medium was DMEM/F-12 without phenol red and sodium pyruvate (Gibco cat. #51500-056) in case of DHE fluorescence.
LDL assay and hydrogen peroxide assay
NRK 52E cells were treated with aldosterone (10−7 M) and CaOx monohydrate (COM; 67 μg/cm2) for 12 h with or without preincubation of spironolactone, pp2 and DPI. We measured lactate dehydrogenase (LDH) in the medium using Cyto Tox 96 Non-Reactive Cytotoxicity Assay (cat. #PR-G1780, Promega, USA). The absorbance was read at 490 nm on a microplate reader (ELx808 BioTek). All determinations were made against appropriate medium blanks. We measured peroxides of medium using PeroXOquant™ Quantitative Peroxide Assay Kit (cat. #23285, Thermo Scientific, Inc.) The absorbance was read at 595 nm on the same microplate reader.
Measurement of superoxide anion levels
We determined superoxide levels by DHE using a confocal microscope (IX81-DSU, Olympus, Japan). We selected TRITC (tetramethylrhodamine isothiocyanate) under conditions of 560 nm excitation and 607 ± 36 nm band-pass filter. Cells were incubated on Lab-Tek™ II chambered coverglass with or without treatment of spironolactone (10−5 M), pp2 (10−5 M) and DPI (10−5 M) for 90 min and stimulated with or without treatment of aldosterone (10−7 M) and COM crystals (67 μg/cm2). The medium was used DMEM/F-12 without phenol red and sodium pyruvate. DHE stains were performed at 3, 6, 12, 24 h after added aldosterone and 6 h after exposed COM crystals. After washing with PBS, DHE (5 μmol/l) was applied topically to each slide and incubated for 30 min at 37 °C while protected from light. DHE is oxidized on reaction with superoxide to ethidium bromide, which binds to DNA in the nucleus and fluoresces red. We measured all cellular stain intensities using ImageJ software for at least three independent fields and evaluated superoxide anion levels.
Measurement of Rac1 activation
The GTP-bound form of active Rac1 was measured by the Rac1 activation assay Biochem kit. The Rho switch operates by alternating between an active, GTP-bound state, and inactive, GDP bound state. Understanding the mechanisms that regulate activation/inactivation of the GTPases is of obvious biological significance and is a subject of intense investigation. The fact that many Rho family effector proteins will specifically recognize the GTP-bound form of the protein has been exploited experimentally to develop a powerful affinity purification assay that monitors Rac1 and Cdc42 protein activation. This assay is available of the binding domain of p21-activated kinase 1(PAK). The cells were grown on 100-mm dishes and lysed with 500 µl ice-cold lysis buffer (50 mM tris pH 7.5, 10 mM MgCl2, 0.5 M NaCl and 2 % Igepal) with protease inhibitor cocktail (100 × solution: 62 μg/ml leupeptin, 62 μg/ml pepstatin A, 14 mg/ml benzamidine and 12 mg/ml tosyl arginine methyl ester). Cell lysate samples were collected at 1, 3, 6, 12, 24 h after stimulated by aldosterone and 6, 12, 24 h after exposed to COM crystals with or without treatment of drugs (spironolactone, PP2 and DPI). We measured the protein concentrations of lysate samples by BCA™ Protein Assay Kit (Piece Chemical Company, Rockford, USA), and equal protein concentration in all samples is a prerequisite for accurate comparison between sample in Rac1 activation assay. Samples of 250 μg total cell lysate per sample should be sufficient to detect total Rac1. PAK-PBD protein beads were diluted to be 10 μg per one assay, and pull down assay was performed. The beads were washed once with 500 μl each of wash buffer composed of 25 mM Tris pH 7.5, 30 mM MgCl2 and 40 mM NaCl. The samples (included non-pull down assay) were ready to be analyzed by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and Western blot analysis. Solutions were prepared as follows: running buffer, from 10 × Tris/glycine/SDS buffer (BioRed, Cat# 161-0732); transfer buffer, from 250 M Tris, 1.92 M glycine and 20 % methanol; 5 % nonfat milk as a blocking buffer. Sample buffer was purchased from Boston BioProducts, Inc. (Cat. # BP-111R), and gel was from Bio RAD (Criterion™ Precast Gel, Cat# 345-0042). Goat antimouse HRP-conjugated IgG (1:5000) was used as a second antibody. Equal amounts of membrane protein were subjected to SDS-PAGE and transferred on to nitrocellulose membranes. Immunoreactive bands were visualized with an ECL Plus Western blotting detection system (GE Healthcare, Cat. # RPN2132).
Statistical analysis
Results are expressed as mean ± standard error. Welch’s t test is used to evaluate differences between two groups using StatFlex software. P < 0.05 is considered to indicate statistical significance.
Results
Animal model studies
As we have previously shown, administration of ethylene glycol resulted in hyperoxaluria and deposition of crystals in the kidneys. Spironolactone administration did not appear to have any effect on hyperoxaluria or crystal deposition (results not shown).
Genes encoding for angiotensinogen (AGT), Renin 1 (Ren 1), angiotensin receptor 2 (AGTr2), angiotensin receptor 1b (AGTr1b), aldosterone synthase (Cyp11b), MR (Nr3c2), Rac1, Nox4 and superoxide dismutase (SOD) was assessed. Relative expression of AGT, Ren 1, AGTr2, AGTr1b, Cyp11b, Nr3c2, Rac1 and Nox 4 was upregulated in kidneys of rats with hyperoxaluria receiving only ethylene glycol. Treatment with spironolactone reversed the effect of EG treatment on expression of various genes (Fig. 1). There was many fold increase in the SOD-1 gene expression. On the other hand, there were many fold decreases in the expression of AGT, Ren 1, AGTr2, AGTr1b, Cyp11b, Nr3c2, Rac1 and Nox4 genes.
Genes encoding for angiotensinogen (AGT), renin 1 (Ren 1), angiotensin receptor 2 (AGTr2), angiotensin receptor 1b (AGTr1b), aldosterone synthase (Cyp11b), mineralocorticoid receptor (Nr3c2), Rac1, Nox 4 and superoxide dismutase (SOD) were assessed. Relative expression of AGT, Ren 1, AGTr2, AGTr1b, Cyp11b, Nr3c2, Rac1, and Nox 4 was upregulated in kidneys of rats with hyperoxaluria receiving only ethylene glycol. Treatment with spironolactone reversed the effect of EG treatment on expression of various genes on day 28
Cell culture studies
Aldosterone induced Rac1 activation in the cultured epithelial cells. Increase in Rac1 activity was observed as early as 3 h, peaking at 6 h (Fig. 2). Aldosterone exposure also resulted in the production of superoxide, as evidenced by increased DHE stain intensity. Intracellular superoxide production was significantly inhibited by pretreatment with MR inhibitor spironolactone (Fig. 3).
DHE (dye dihydroethidium) stains were performed, and stain intensities were measured. Aldosterone-induced fluorescence intensities of microscopic images were maximal at 6 hours and decreased after that to 24 hours. And increased superoxide levels induced by aldosterone were significantly inhibited for 12 hours by pretreatment of mineralocorticoid receptor (MR) inhibitor; spironolactone on NRK52E cells
Exposure of cells in culture to CaOx crystals for 6 h also led to increased Rac1 protein expression which was attenuated by NADPH oxidase inhibitor diphenyleneiodonium chloride(DPI), Src inhibitor (PP2) and MR inhibitor spironolactone (Fig. 4). In DHE staining of renal epithelial cells to estimate intracellular superoxide levels, DHE stain intensity was increased by exposure to CaOx crystals, and this increased intensity was significantly diminished by treatment with spironolactone, PP2 as well as DPI (Fig. 5).
Rac1 protein expression levels of renal epithelial cells were demonstrated after exposure of CaOx crystals. At 6 hours after CaOx crystals exposure, Rac1 protein expression level was increased compared with control. And increased levels of Rac1 expression were attenuated by NADPH oxidase inhibitor; DPI (diphenyleneiodonium chloride), Src inhibitor; PP2 and spironolactone (Spi)
We also studied the production of OPN by NRK 52 E cells exposed to COM crystals for 6 or 12 h. As we have previously shown, OPN production was increased. Treatment of cells with spironolactone, DPI as well as PP2, resulted in the reduction in OPN production. DPI and PP2 showed best inhibition at 6 h and spironolactone at 12 h.
Discussion
The formation of kidney stones is a result of crystal nucleation, growth and aggregation and occurs in renal tubular lumens. Hyperoxaluria is one of the major risk factors for kidney stone formation, and approximately 70–80 % of kidney stones are composed of calcium oxalate crystals [14]. An increase in urinary excretion of oxalate is associated with high levels of urinary lactate dehydrogenase (LDH), H2O2 as well as lipid peroxides, indicating renal cell injury induced by development of oxidative stress. Renal cellular exposure to high oxalate and/or CaOx crystals leads to the production of ROS, followed by renal cellular injury and inflammation.
ROS are involved in the activation of signaling molecules such as protein kinase C (PKC), c-Jun-NH2-terminal kinase (JNK) and p38 mitogen-activated protein kinase (MAPK), with influence over transcription factors such as NF-κB and activated protein-1 (AP-1). Activation of these transcription factors leads to upregulation of genes and production of crystallization modulators such as OPN, bikunin and α-1-microglobulin, which affect all aspects of nephrolithiasis including crystal formation, growth, aggregation as well as their retention within the kidneys [15–17]. Clinical studies have also demonstrated development of oxidative stress and renal injury in kidney stone patients [18, 19]. In LLC-PK1 cells, an epithelial cell line from pig kidney with properties of proximal tubular cells and oxalate exposure increases Nox activity via PKC signaling pathway, which stimulates superoxide production and resultant cellular injury [20]. Blockade of PKC signaling by PKC a and d inhibitors attenuates Rac1 activation in oxalate-treated cells suggesting that PKC resides upstream of Rac1 in the pathway that regulates NADPH oxidase [21].
There is increasing evidence that aldosterone induces renal injury causing inflammation and fibrosis. In rats, chronic treatment with aldosterone and salt results in severe proteinuria and renal tissue injury, characterized by glomerulosclerosis and tubulointerstitial fibrosis. Aldosterone-induced renal injury is associated with increases in ROS levels and activation of MAPKs or Rho-kinase, and treatment with a selective MR antagonist, eplerenone, prevents aldosterone-induced increases in ROS levels and MAPK activity and ameliorates renal injury. And it is suggested that MR blocker and Rho-kinase inhibitor prevents the progression of renal injury through several target molecules. In vitro exposure of cultured rat podocytes to aldosterone induced their apoptosis through inhibition of PI3-K/Akt and stimulation of p38 MAPK signaling pathways. This deleterious effect could be attenuated by spironolactone treatment.
The small G protein Rac1 is one of the major adapter proteins which regulate NADPH oxidase activity. It regulates gene expression, cell cycle progression, cell spreading, rearrangement of the actin cytoskeleton and activation of nonphagocytic NADPH oxidase [22–24]. In rat aortic endothelial cells, there is evidence that aldosterone induces superoxide generation via Nox and Rac1 activation through MR [2]. In mice lacking Rho GDP-dissociation inhibitor-α (Arhgdia−/− mice), renal abnormalities, including heavy albuminuria and podocyte damage, were associated with increased Rac1 (but not RhoA) and MR signaling in the kidney, without alteration in systemic aldosterone status. Pharmacological intervention with a Rac-specific small-molecule inhibitor diminished MR overactivity and renal damage in this model. Furthermore, albuminuria and histological changes in Arhgdia−/− mice were suppressed by MR blockade, confirming the pathological role of Rac1–MR interaction [25].
Our in vitro study using NRK52E rat renal epithelial cells demonstrates that MR antagonist prevented both COM and aldosterone-induced increases in the generation of superoxide. Exposure to either COM or aldosterone also led to increased expression of Rac1. COM-induced Rac1 expression was inhibited by mineralocorticoid inhibitor, spironolactone; NADPH oxidase inhibitor, DPI; and SRC inhibitor, PP2. Same inhibitors were also responsible for reduction in the production of superoxide by cells exposed to COM crystals. These results indicate that Rac1 plays an important role in Nox-dependent ROS generation by renal epithelial cell exposure to COM crystals. Results also suggest potential involvement of MR in the generation of superoxide.
Results of our in vivo animal model study show that hyperoxaluria is associated with increased expression of genes for angiotensinogen, renin as well as angiotensin receptors in the kidneys confirming our similar earlier observations using ethylene glycol as hyperoxaluria-inducing agent. Results also show upregulation of genes for aldosterone synthase and MR indicating the involvement of aldosterone pathway. Hyperoxaluria was also associated with increased expression of Rac1, and Nox4 as well as reduction in superoxide dismutase-1. Mineralocorticoid inhibitor spironolactone was able to reverse the effect of hyperoxaluria on the expression of genes for angiotensinogen, renin, angiotensin receptor as well as those of aldosterone synthase and mineralocorticoid receptor. Rac1, Nox4 and SOD1 expressions were also reversed. Results of in vivo and in vitro studies indicate a cross talk between angiotensin and aldosterone receptors and pathways though Rac1. Hyperoxaluria and CaOx crystal deposition induce the production of angiotensinogen and renin, followed by angiotensin II and activation of angiotensin receptor 2 and protein kinase C. This leads to the production of Rac1 which activates mineralocorticoid receptor.
References
Miyata K, Rahman M, Shokoji T et al (2005) Aldosterone stimulates reactive oxygen species production through activation of NADPH oxidase in rat mesangial cells. J Am Soc Nephrol 16:2906–2912
Iwashima F, Yoshimoto T, Minami I, Sakurada M, Hirono Y, Hirata Y (2008) Aldosterone induces superoxide generation via rac1 activation in endothelial cells. Endocrinology 149:1009–1014
Shibata S, Nagase M, Yoshida S, Kawachi H, Fujita T (2007) Podocyte as the target for aldosterone roles of oxidative stress and Sgk1. Hypertension 49:355–364
Paravicini TM, Montezano AC, Yusuf H, Touyz RM (2012) Activation of vascular p38MAPK by mechanical stretch is independent of c-Src and NADPH oxidase: influence of hypertension and angiotensin II. J Am Soc Hypertens 6:169–178
Shey J, Cameron MA, Sakhaee K, Moe OW (2004) Recurrent calcium nephrolithiasis associated with primary aldosteronism. Am J Kidney Dis 44:e7–e12
Kabadi UM (1995) Renal calculi in primary hyperaldosteronism. J Postgrad Med 41:17–18
Kiyomoto H, Rafiq K, Mostofa M, Nishiyama A (2008) Possible underlying mechanism responsible for aldosterone and mineralcorticoid receptor-dependent renal injury. J Pharmacol Sci 108:399–405
Patni H, Mathew JT, Luan L, Franki N, Chander PN, Singhal PC (2007) Aldosterone promotes proximal tubular cell apoptosis: role of oxidative stress. Am J Physiol Renal Physiol 293:F1065–F1071
Umekawa T, Tsuji H, Uemura H, Khan SR (2009) Superoxide from NADPH oxidase as second messenger for the expression of osteopontin and monocyte chemoattractant protein-1 in renal epithelial cells exposed to calcium oxalate crystals. BJU Int 104:115–120
Joshi S, Saylor BT, Wang W, Peck AB, Khan SR (2012) Apocynin-treatment reverses hyperoxaluria induced changes in NADPH oxidase system expression in rat kidneys: a transcriptional study. PLoS One 7:e47738
Khan SR, Khan A, Byer K (2011) Temporal changes in the expression of mRNA of NADPH oxidase subunits in renal epithelial cells exposed to oxalate or calcium oxalate crystals. Nephrol Dial Transpl 26:1778–1785
Umekawa T, Hatanaka Y, Kurita T, Khan SR (2004) Effect of angiotensin II receptor blockage on osteopontin expression and calcium oxalate crystal deposition in rat kidneys. J Am Soc Nephrol 15:635–644
Zuo J, Khan A, Glenton PA, Khan SR (2011) Effect of NADPH oxidase inhibition on the expression of kidney injury molecule and calcium oxalate crystal deposition in hydroxy-L-proline-induced hyperoxaluria in the male Sprague-Dawley rats. Nephrol Dial Transpl 26:1785–1796
Kaufman DW, Kelly JP, Curhan GC, Anderson TE, Dretler SP, Preminger GM, Cave DR (2008) Oxalobacter formigenes may reduce the risk of calcium oxalate kidney stones. J Am Soc Nephrol 19:1197–1203
Scheid CR, Koul H, Hill WA, Luber-Narod J, Kennington L, Honeyman T, Jonassen J, Menon M (1996) Ox toxicity in LLCPK1 cells: role of free radicals. Kidney Int 49:413–419
Thamilselvan S, Hackett RL, Khan SR (1997) Lipid peroxidation in ethylene glycol induced hyperoxaluria and calcium oxalate nephrolithiasis. J Urol 157:1059–1063
Khan SR (1997) Tubular cell surface events during nephrolithiasis. Curr Opin Urol 7:240
Huang HS, Ma MC, Chen CF, Chen J (2003) Lipid peroxidation and its correlations with urinary levels of oxalate, citric acid, and osteopontin in patients with renal calcium oxalate stones. Urology 61:1123–1128
Tungsanga K, Sriboonlue P, Futrakul P, Yachantha C, Tosukhowong P (2005) Renal tubular cell damage and oxidative stress in renal stone patients and the effect of potassium citrate treatment. Urol Res 33:65–69
Thamilselvan V, Menon M, Thamilselvan S (2009) Oxalate-induced activation of PKC-alpha and-delta regulates NADPH oxidase-mediated oxidative injury in renal tubular epithelial cells. Am J Physiol Ren Physiol 297:F1399–F1410
Thamilselvan V, Menon M, Thamilselvan S (2012) Selective Rac1 inhibition protects renal tubular epithelial cells from oxalate-induced NADPH oxidase-mediated oxidative cell injury. Urol Res 40:415–423
Hordijk PL (2006) Regulation of NADPH oxidases: the role of Rac proteins. Circ Res 98:453–462
Li SM, Zeng LW, Feng L, Chen DB (2010) Rac1-dependent intracellular superoxide formation mediates vascular endothelial growth factor-induced placental angiogenesis in vitro. Endocrinology 151:5315–5325
Moldovan L, Irani K, Moldovan NI, Finkel T, Goldschmidt-Clermont PJ (1999) The actin cytoskeleton reorganization induced by Rac1 requires the production of superoxide. Antioxid Redox Signal 1:29–43
Nagase M, Fujita T (2008) Aldosterone and glomerular podocyte injury. Clin Exp Nephrol 12:233–242
Acknowledgments
The studies were approved by the University of Florida’s IACUC and were conducted in accord with the recommendations of the NIH Guide for the Care and Use of Laboratory Animals. The funding for the research was provided by National Institute of Health (NIH) grant number RO1-DK078602.
Conflict of interest
The authors declare that they have no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsuji, H., Wang, W., Sunil, J. et al. Involvement of renin–angiotensin–aldosterone system in calcium oxalate crystal induced activation of NADPH oxidase and renal cell injury. World J Urol 34, 89–95 (2016). https://doi.org/10.1007/s00345-015-1563-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1563-y