Abstract
Objectives
To study the possible renoprotective effect of sildenafil against renal ischemia/reperfusion (I/R) injury and its effect on the expression of some antioxidant, antiapoptotic gene and proinflammatory cytokine genes in rat model of renal I/R injury.
Materials and methods
One hundred and twenty male Sprague Dawley rats were subdivided into three equal groups: sham (underwent right nephrectomy without ischemia), control (underwent right nephrectomy and left ischemia for 45 min) and study [as control with 1 mg/kg sildenafil (per oral) 60 min before anesthesia]. Serum creatinine and BUN were measured at the baseline and the study endpoints (2, 24, 48 h and 7 days), and the left kidney was harvested at study endpoints for histopathological examination as well as for assessment of the expression of antioxidant genes (Nrf-2, HO-1 and NQO-1), antiapoptotic gene (Bcl-2) and inflammatory cytokines, e.g., TNF-a, IL-1β and ICAM-1.
Results
I/R caused significant increase in serum creatinine, BUN, histopathological damage score (p < 0.001) and significant reduction in antioxidant genes (nrf2, HO-1 and NQO-1) and antiapoptotic gene (Bcl2) with significant increase in TNF-a, IL-1β and ICAM-1 genes in kidney tissues. Pretreatment with sildenafil caused significant attenuation of serum creatinine and BUN as well as significant increase in the expression of antioxidant genes and Bcl-2 genes with significant reduction in the expression of proinflammatory cytokine genes (p value < 0.001).
Conclusion
The renoprotective effect of sildenafil against renal I/R might be due to the activation of antioxidant genes (Nrf2, HO-1 and NQO-1) and antiapoptotic gene (Bcl2) and attenuation of proinflammatory cytokines (TNF-a, IL-1β and ICAM-1).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal ischemia/reperfusion (I/R) injury is a common clinical problem that encountered in renal transplantation, nephron-sparing surgery, renal vascular surgery and aortic cross-clamping for abdominal aortic aneurisms [1]. It is a major cause of acute renal failure (ARF). In kidney transplantation, I/R injury is a common cause of renal cell death, ARF, delayed graft function and renal graft rejection [2]. Extensive efforts have been done using pharmacological and non-pharmacological agents to antagonize the deleterious effect of I/R injury [1, 3–5]. Yet, there are no consistent effective ways to prevent the damage of I/R injury other than generous preoperative hydration, prevention of hypotension during the period of anesthesia, avoidance of unnecessary manipulation or traction on the renal artery. These measures help to limit post-ischemic renal injury by ensuring optimal perfusion with absence of cortical vasospasm at the time of arterial occlusion [6].
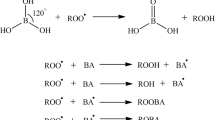
I/R injury is a multifactorial complex process which includes ATP depletion, accumulation of intracellular Ca2+ and reactive oxygen species (ROS), proinflammatory cytokine production and apoptotic pathway activation. ROS are involved in tissue damage that occurs following I/R [7], and their role in the pathophysiology of I/R injury is supported by the increased formation of lipid peroxidation and other toxic products that occur following such an injury [8]. The transcription nuclear factor erythroid 2-related factor 2 (Nrf2) is the master regulator of antioxidant defense genes such as including heme oxygenase-1 (HO-1), NAD (P) H: quinone oxidoreductase 1 (NQO1), glutathione reductase (GR), and glutathione peroxidase (GPx) and drug-metabolizing enzymes [9, 10]. In recent study by our group, we demonstrated activation and enhancement of the expression of nrf2 and its dependent genes HO-1 and NQO-1 as well as reduction in proinflammatory cytokines TNF-α, IL1β and ICAM-1 in a rat model of renal ischemia by ischemic preconditioning [4].
Sildenafil is a drug that commonly used in the treatment of erectile dysfunction. Several recent studies have shown that sildenafil also offers benefits in pulmonary arterial hypertension and congestive heart failure. This is because of its vasodilatation and antiapoptotic actions [11]. Recently, few studies reported a beneficial effect of sildenafil to prevent the consequences of I/R injury in animal models [11–15]. Sildenafil was approved to increase the renal vein level of nitric oxide (NO) that improves renal hemodynamic [15]. NO is proved to have anti-inflammatory, antioxidant and antiapoptotic effect [16]. Therefore, we hypothesized that activation of Nrf2 and its dependent antioxidant genes (HO-1 and NQO-1) might be one of the potential mechanisms of the renoprotective action of sildenafil against renal ischemic injury. So, this study was designed to investigate the effect of sildenafil on renal I/R as well as its effect on the expression of Nrf2 and its dependent genes (NQO-1 and HO-1), antiapoptotic (Bcl-2) and proinflammatory cytokine (TNF-α, IL1β and ICAM-1) genes in a rat model of renal I/R injury.
Materials and methods
Experimental animals
The study included one hundred and twenty male Sprague Dawley rats weighing 200–250 g (aged 4–5 months) that were bred and housed in the animal house of the Urology and Nephrology center, Mansoura, Egypt. The animals were housed in separate cages with free access to the tape water. The experiment was performed according to the international guidelines for the care of the experimental animals and approved by local ethical committee of Mansoura, Faculty of Medicine.
Experimental design
Rats were randomly divided into three groups (40 rats each): (a) sham group (surgical exploration of the left renal pedicle without ischemia + right nephrectomy), (b) control group, (left renal ischemia for 45 min + right nephrectomy) and (c) study (sildenafil-treated) group; as control group with oral intake of sildenafil (1 mg/kg) 60 min before anesthesia. Each group is subdivided into four groups (10 each) according to the time of killing: 2, 24, 48 h and 7 days.
Experimental procedures
In all rat, anesthesia was induced by intraperitoneal (i.p) injection of a mixture of ketamine 75 mg/kg and diazepam 5 mg/kg. After anesthesia, the rat was fixed supine on a thermoregulated heating board to maintain a body temperature of 37 °C. All surgical procedures were done according to the previously described technique [1]. Briefly, in sham group, a midline laparotomy was performed, left kidney and its pedicle were dissected off the surrounding perirenal fat along the renal surface and the left kidney was exposed without vascular clamping for 45 min. Then, the right renal vascular pedicle was exposed and ligated using 3–0 silk sutures twice, and the kidney was removed. The abdomen was irrigated with isotonic saline, and the abdominal incision was closed by continuous stitches using 3/0 vicryl sutures. In control group, the same was done as sham group with clamping of the left renal artery using vascular clamp for 45 min, and right kidney was removed 5 min before the removal of the vascular clamp. For the sildenafil-treated group, the same procedure was performed as control group plus oral administration of sildenafil (Viagra, Pfizer, Egypt) 60 min before anesthesia. The sildenafil tablets were dissolved in sterile saline and given as a single dose 1 mg/kg via gastric gavage tube.
Collection of blood and urine samples and harvesting the kidney
Blood and urine samples were collected before the procedure (basal) and before killing the animal at 2, 24, 48 h and 7 days (endpoints). Blood samples were obtained under inhalational general anesthesia from the ophthalmic venous plexus. The blood sample was centrifuged, and the serum was isolated and stored at −20 °C for measurement of serum creatinine and blood urea nitrogen (BUN). At the end of the study, rats were anesthetized by high-dose intraperitoneal thiopental sodium. Midline laparotomy was done, and the left kidney was removed and bisected longitudinally into two halves by a scalpel. One half was placed in formalin 10 % for histopathological examination. The second half was kept at −80 °C for assessment of antioxidant (Nrf2, HO-1 and NQO-1) genes, proinflammatory cytokine (TNF-α, IL-1β, and ICAM-1) and antiapoptotic (Bcl-2) genes by real-time PCR.
Assessment of renal function
Serum creatinine and blood urea nitrogen (BUN) were estimated from blood samples by using an auto-analyzer (CX 7; Beckman, Foster City, CA, USA).
PCR assay of antioxidant genes, proinflammatory cytokine and antiapoptotic genes
Real-time PCR was used to identify mRNA encoding for proinflammatory cytokines; tumor necrosis factor-a (TNF-α), intercellular adhesion molecule-1 (ICAM-1) and interleukin-1β (IL-1β). Also, it was used to assay the expression of antioxidant genes, nuclear erythroid-related factor 2 (Nrf2), NAD (P) H: quinine oxidoreductase-1 (NQO1) and heme oxygenase-1 (HO-1) and the expression of antiapoptotic B cell lymphoma 2 (Bcl2) gene in renal tissue. According to the manufacturer’s instructions, total RNA from kidney tissue specimens was isolated. RNA was quantified spectrophotometrically, and its quality was determined by agarose gel electrophoresis and ethidium bromide staining. cDNA was synthesized from 1 µg total RNA and then buffered in a volume of 25 µl. Then, the 25 µl cDNA was diluted in a total volume of 100 µl. PCR was used to amplify the cDNA for TNF-a [5′-CAGCCTTGTCCCTTGAAGAGAACC-3′ (sense) 5′TACTGAACTTCGGGGTGATTGGTCC-3′ (antisense)], ICAM-1 [5′TGTTTCCTGCCTCTGAAGC-3′], IL-1ß [5′-AATACCACTTGTTGGCTTA-3′(sense) 5′-TGTGATGTTCCCATTAGAC-3′ (antisense)], Nrf2 [5′ATTGCTGTCCATCTCTGTCAG-3′.(sense) 5′-GCTATTTTCCATTCCCGAGTTAC-3′ (antisense)], NQO1 [5′-ACAGCCGTGGCAGAACTA-3′(sense) 5′-CATCATTTGGGCAAGTCC-3′(antisense)], HO-1 [5′TGCTTGTTTCGCTCTATCTCC-3′.(sense) 5′-CTTTCAGAAGGGTCAGGTGTC-3′, (antisense)] and Bcl2 [5′-AGAGACAGCCAGGAGAAATCAAAC3′ (sense) 5′ATCGCTCTGTGGATGACTGAGTAC3′(antisense)]. Amplification and detection were performed using a thermal cycler. The cycling parameters were as follows: initial denaturation at 95 °C for 10 min, followed by 40 cycles of denaturation 95 °C for 15 s, annealing at 60 °C for 1 min, extension at 72 °C for 1 min. The cDNA was quantified using the following formula: 2-ct (2-[(Ct of target gene-Ct of GAPDH in treated rats)-(Ct of target gene-Ct of GAPDH in sham rats)]) [18].
Immunohistochemical examination of Nrf2
For immunohistochemistry, 3-µm-thick sections were prepared on charged slides from paraffin blocks and deparaffinized. All sections were incubated for 30 min with 0.3 % hydrogen peroxide in methanol and microwave-heated in 10 mM citrate buffer, pH 6.0, for 10–20 min. Subsequently, an indirect immunoperoxidase technique was applied, using antibodies such as anti-Nrf2 polyclonal antibody (catalog # sc-13032 X; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Indirect immunoperoxidase was performed using ImmunoPure UltraSensitive ABC Peroxidase (catalogue number: 32052; Thermo Scientific, Waltham, MA, USA) with (DAB) as chromogen. Proper positive and negative controls were performed. Placenta was used as positive control for Nrf2. As a negative control, sections were stained without the addition of a primary antibody.
Histopathological examination
The kidney specimens were processed, embedded in paraffin blocks, sectioned in 4-µm-thick slices and stained with hematoxylin and eosin to be examined by light microscope in a double-blinded fashion. Tubulointerstitial regions were examined for tubular dilatation, distal tubular cast, loss of proximal tubular brush border, patchy loss of tubular cells, peritubular vascular congestion and endothelial damage and leukocyte accumulation [17]. A well-defined scoring system was used for evaluation of the degree of tubulointerstitial damage [8], where 0 = no abnormality, 1 = minimal damage involves 25 % of the cortex and outer medulla, 2 = mild damage involves 25–50 % of the cortex and outer medulla, 3 = moderate damage involves 50–75 % of the cortex and outer medulla and 4 = sever damage involves 75 % of the cortex and outer medulla.
Statistical analysis
The comparison between baseline and endpoint measures was tested using paired sample t test. The comparison between mean ± SD of the endpoint values of serum creatinine and BUN and the counts of mRNA products by RT-PCR were done using one-way ANOVA with Student–Newman–Keuls (SNK) post hoc test. Statistical analysis was performed using SPSS version 16 (SPSS, Chicago, IL, USA), with p value <0.05 considered significant.
Results
Effects of sildenafil administration on renal function (serum creatinine, BUN)
Basal values of serum creatinine and BUN were comparable among the three groups (sham, control and study). Compared to their basal values, the endpoint values of serum creatinine and BUN were significantly increased at 2, 24, 48 and 7 days in all groups (p < 0.05). The endpoint values of serum creatinine and BUN showed statistically insignificant increase in control group when compared with sham group at 2 h. At 24, 48 h and 7 days, control group showed significant increase in serum creatinine and BUN in comparison with the sham group (p ≤ 0.008). Sildenafil-treated group showed statistically significant increase in serum creatinine and BUN compared to control group at 24, 48 h and 7 days after renal ischemia (p < 0.01) (Table 1).
Effects of sildenafil on the expression of antioxidants, antiapoptotic genes and proinflammatory cytokine genes at the level of mRNA
Control group showed significant decrease in the expression of antioxidant genes (Nrf2, HO-1 and NQO-1) at level of mRNA compared to sham group at different time intervals (2, 24, 48 h and 7 days) (p < 0.05). Moreover, administration of sildenafil caused statistically significant increase in the expression of these genes at different time intervals (p < 0.05) (Table 2). Also, the expression of Bcl-2 antiapoptotic gene by real-time PCR was significantly lower in control group compared to sham group (p < 0.001) and pretreatment with sildenafil caused significant increase in its expression compared to control group at 24, 48 h and 7 days (p value < 0.01) (Table 2).
The expression of proinflammatory cytokine (TNF-α, ICAM-1 and IL-ß) genes at the level of mRNA was statistically significantly higher in the control group when compared to the sham group at 2, 24, 48 h and 7 days (p value < 0.001). Sildenafil-treated group showed statistically significant decrease in the expression of the inflammatory cytokines compared to the control group at different time intervals (p < 0.001) (Table 2).
Effects of sildenafil administration on renal histopathological changes and nrf2 expression at the level of protein
Histopathological damage score showed significant increase in the damage score in control group compared to sham group (p < 0.001). On the other hand, kidneys obtained from sildenafil-treated rats showed significant attenuation of histopathological damage score (p < 0.001) (Fig. 1a). Kidney specimens obtained from sham group showed normal cortex architecture (Fig. 1b) and high nrf2 protein expression with average expression of 30 % (Fig. 1c). Kidneys specimens obtained from the control group showed the severe and pronounced injury in the cortex and the outer stripe of the outer medulla (OSOM), with a pattern of acute tubular necrosis, which included widespread degeneration of tubular architecture, detachment of epithelial cells from the basement membrane, tubular cell necrosis, intratubular cast formation and luminal congestion with extensive loss of brush border (Fig. 1d), marked neutrophil infiltration in the renal cortex (Fig. 1e) and low nrf2 protein expression with average expression of 17 % (Fig. 1f). On the other hand, renal sections obtained from the sildenafil-treated (study) group showed a marked reduction in the histological features of renal injury, consisting of mild individual tubular necrosis and minimal tubular dilatation (Fig. 1g, h) and highest nrf2 protein expression in the cortical tissues with average 37 % (Fig. 1i).
Effect of sildenafil on kidney morphology and nrf2 protein expression by immunohistochemistry, a histopathological tubulointerstitial damage score in different groups at different times. *Significant versus sham group, #significant versus control group. Sham group showed normal kidney tissues at 48 h, b (H&E ×250) and high nrf2 protein expression with average expression of 30 % at 24 h, c (immunoperoxidase DAB ×200) in the cortex, control group showed marked tubular necrosis in the outer strip of outer medulla (OSOM) (attenuated tubular lining, dilated lumen, necrosis, hyaline casts and apoptosis) at 48 h, d (H&E ×250), marked neutrophil infiltrate in the inner part of the renal cortex at 24 h, e (H&E ×250) and low nrf2 protein expression with average expression of 17 % at 48 h in the cortex, f (immunoperoxidase DAB ×400) and sildenafil-treated group showed few tubular dilatation, hydropic degeneration of tubular cells at 48 h, g (H&E ×250) and mild medullary affection (attenuated tubular lining and hyaline casts) at 48 h, h (H&E ×250) and high nrf2 protein expression with average expression of 37 % at 48 h, i (immunoperoxidase DAB ×400) in the cortex
Discussion
Despite the advances in surgical, medical and pharmacological fields, I/R remains a serious problem with early and delayed consequences after renal transplantation and renal vascular surgeries [19]. So, in the present study we investigated the possible protective effect of sildenafil in renal I/R injury and explore its underlying potential mechanisms. Renal I/R injury is a complex syndrome involving different mechanisms, including persistent vasoconstriction, reduction in medullary blood flow, ATP depletion, accumulation of intracellular Ca2+ and reactive oxygen species, mitochondrial dysfunction, proinflammatory cytokine production and neutrophils accumulation. Together, renal ischemia and reperfusion initiate a multiple and interrelated sequence of events, resulting in the injury and eventually the death of renal cells as a combination of both apoptosis and necrosis [20]. In the present study, renal ischemic injury was manifested by significant elevation in serum creatinine and BUN in control group compared to sham group. Moreover, histopathological examination revealed significant elevation in tubulointerstitial damage score in the form of acute tubular necrosis, tubular dilatation and loss of brush border of the proximal convoluted tubules as well as marked leukocytic (neutrophil) infiltration in the kidney tissues. All of these findings confirmed damaging effect of renal I/R and in agreement with previous studies [1, 3, 4].
Administration of sildenafil, orally 60 min before surgery in a dose of 1 mg/kg, caused significant improvement in renal ischemic injury at the level of kidney functions and morphology (manifested by the lower serum creatinine and BUN and tubulointerstitial damage score in the sildenafil-treated group). These findings are in agreement with previous studies done by Choi et al. [11] who demonstrated the renoprotective effect for sildenafil after intraperitoneal injection. The timing and dose of sildenafil in the present study were chosen to reach the therapeutic plasma level at the time of warm ischemia taking into consideration the bioavailability of 40–49 % of the drug after oral intake [15].
Sildenafil is a commonly used drug for treatment of erectile dysfunction because of its vasodilator effect. The mechanism of action involves inhibition of phosphodiesterase-5 (PDE5), resulting in increase of cGMP. Also, sildenafil induces upregulation of endothelial nitric oxide synthase (eNOS) and inducible NOS (iNOS), which generate NO which activates guanylate cyclase, resulting in enhanced formation of cGMP, which activates PKG leading to smooth muscle relaxation (vasodilatation) [21, 22]. In the present study, we investigated one of the potential mechanisms for the protective action of sildenafil in renal I/R injury. We studied its effect on the expression of mRNA of Nrf2 transcription factor, NQO-1 and HO-1 genes. Also, we examined its effect on the expression of nrf2 protein by immunohistochemistry. The expression of Nrf2, HO-1 and NQO-1 genes has been proved to guard against oxidative injury after renal I/R injury [23–25]. Here in this study, administration of sildenafil resulted in over expression of these antioxidant genes when compared to the control group. So, to the best of our knowledge, this study is the first study demonstrated enhanced expression of Nrf2 by sildenafil in renal I/R injury at the level of mRNA and protein.
Inflammatory response that is initiated by endothelial dysfunction is proved to play a major role in renal ischemic injury. It is associated with the expression of proinflammatory cytokines like TNF-α and IL1β [20]. In this study, control group has higher expression of the proinflammatory cytokines than the sham group, while sildenafil administration caused significant attenuation of the expression of TNF-α and IL-1β. This demonstrated the possible role of sildenafil in protection against renal I/R injury by interrupting the inflammatory cascade initiated by the damaged proximal tubular cells. This is explained by the increased production of NO through activation of eNOS and iNOS as well as increasing the activity of soluble guanylyl cyclase that downregulates the inflammatory process by many mechanisms [12, 21]. However, the levels of NO or NOS were not measured in this study. Similar results of the anti-inflammatory effect of sildenafil through the iNOS/NO pathway were obtained while studying the inflammatory demyelination and pulmonary hypertension in animal models [26, 27]. Raposo et al. [26] demonstrated that sildenafil reduces the expression of IL-1β, but has no effect on the TNF-α in neuroinflammatory demyelinating model. Also, Gilchrist et al. [28] reported that NO downregulates the mast cells and decreases release of inflammatory cytokines including TNF-α which is similar to the result of this study.
Also, sildenafil-treated group has lowered the expression ICAM-1 that promotes endothelial leukocyte interaction which becomes a widely accepted fundamental process in mechanism of renal I/R. These findings suggested that sildenafil might reduce recruitment and migration of leukocytes to the ischemic kidney tissues. This is evidenced by reduction in the leukocytic infiltration demonstrated by histopathological examination. Suppression of this gene and use of specific antibodies rendered mice resistant to ischemic AKI [23]. Similar results of the effect of sildenafil in reduction of ICAM-1 was reported by Rapôso et al. [26] which is attributed to the stimulation of iNOS/NO pathway [27]. Similar results by Ahluwalia et al. [29] demonstrated cGMP-dependent downregulation of P-selectin expression and leukocyte recruitment in vascular endothelial cells.
Bcl-2 is an antiapoptotic molecule that inhibits the intrinsic pathway of apoptosis through prevention of the first step of the process of apoptosis by inactivation of Bcl-2-associated X protein (BAX). BAX activates release of caspase which initiates the final morphological cascade of apoptosis. Inhibition of this pathway is a promising therapeutic option to prevent ischemia-induced AKI [20]. Similar to the previous report of the increased expression of Bcl-2 in sildenafil-treated renal ischemia rat model [11], sildenafil-treated group has statistically significantly higher expression of this gene which proves the antiapoptotic effect of sildenafil. Also, this is due to release of NO which is previously reported to increase expression of Bcl-2 gene [30]. Although the present study demonstrated the antioxidant, antiapoptotic and anti-inflammatory effects for sildenafil in renal I/R injury, we did not investigate the effect of sildenafil on endothelial dysfunctions demonstrated in renal I/R injury in the form of imbalance between NO and endothelin-1 that resulted in arteriolar and venous vasoconstriction [20]. This point is considered as a limitation of the present study and it will be considered in next studies.
Conclusion
We conclude that pretreatment with oral sildenafil before renal ischemia reduces the deleterious effect of renal I/R injury. This effect might be due to enhancement of the expression of antioxidant (Nrf2, NQO-1 and HO-1) genes, antiapoptotic (Bcl-2) genes and attenuation of the expression of the proinflammatory cytokine (ICAM-1, IL-1β and TNF-α) genes.
References
Hussein AA, Shokeir AA, Sarhan ME et al (2011) Effects of combined erythropoietin and epidermal growth factor on renal ischaemia/reperfusion injury: a randomized experimental controlled study. BJU Int 107(2):323–328
Grinyo JM (2001) Role of ischemia-reperfusion injury in the development of chronic renal allograft damage. Transplant Proc 33:3741–3742
Shokeir AA, Hussein AM, Awadalla A et al (2012) Protection against renal ischaemia/reperfusion injury: a comparative experimental study of the effect of ischaemic preconditioning vs. postconditioning. Arab J Urol 10(4):41824
Shokeir AA, Hussein AM, Barakat N et al (2014) Activation of nuclear factor erythroid 2-related factor 2 (Nrf2) and Nrf-2-dependent genes by ischaemic preconditioning and post-conditioning: new adaptive endogenous protective responses against renal ischaemia/reperfusion injury. Acta Physiol 210(2):342–353
Arany I (2008) Dual role of the activated epidermal growth factor receptor in renal tubular cells during stress. Kidney Int 72:5–7
Sheridan AM, Bonventre JV (2001) Pathophysiology of acute renal failure. Contrib Nephrol 132:7–21
McCord JM (1985) Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med 312:159–163
Beckman JK, Yoshioka T, Knobel SM, Greene HL (1991) Biphasic changes in phospholipid hydroperoxide levels during renal ischemia/reperfusion. Free Radic Biol Med 11:335–340
Zhang M, An C, Gao Y, Leak RK, Chen J, Zhang F (2013) Emerging roles of Nrf2 and phase II antioxidant enzymes in neuroprotection. Prog Neurobiol 100:30–47
Kensler TW, Wakabayashi N, Biswal S (2007) Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu Rev Pharmacol Toxicol 47:89–116
Choi DE, Jeong JY, Lim BJ et al (2009) Pretreatment of sildenafil attenuates ischemia-reperfusion renal injury in rats. Am J Physiol Renal Physiol 297(2):F36270
Medeiros PJ, Villarim Neto A, Lima FP et al (2010) Effect of sildenafil in renal ischemia/reperfusion injury in rats. Acta Cir Bras 25(6):490–495
Whitaker RM, Wills LP, Stallons LJ, Schnellmann RG (2013) cGMP selective phosphodiesterase inhibitors stimulate mitochondrial biogenesis and promote recovery from acute kidney injury. J Pharmacol Exp Ther 347(3):626–634
Oruc O, Inci K, Aki FT, Zeybek D, Muftuoglu SF, Kilinc K, Ergen A (2010) Sildenafil attenuates renal ischemia reperfusion injury by decreasing leukocyte infiltration. Acta Histochem 112(4):337–344
Lledó-García E, Subirá-Ríos D, Rodríguez-Martínez D et al (2009) Sildenafil as a protecting drug for warm ischemic kidney transplants: experimental results. J Urol 182(3):1222–1225
Tousoulis D, KampoliAM Tentolouris C, Papageorgiou N, Stefanadis C (2012) The role of nitric oxide on endothelial function. Curr Vasc Pharmacol 10(1):4–18
Molitoris BA, Sutton TA (2004) Endothelial injury and dysfunction: role in the extension phase of acute renal failure. Kidney Int 66(2):496–499
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(–DDC (t)). Methods 25(4):402–408
Shah KG, Rajan D, Jacob A et al (2010) Attenuation of renal ischemia and reperfusion injury by human adrenomedullin and its binding protein. J Surg Res 163(1):110–117
Devarajan P (2006) Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17:1503–1520
Salloum F, Yin C, Xi L, Kukreja RC (2003) Sildenafil induces delayed preconditioning through inducible nitric oxide synthase-dependent pathway in mouse heart. Circ Res 92:595–597
Barakat N, Hussein AAM, Abdel-Maboud M et al (2010) Ischaemia-reperfusion injury in renal transplantation: the role of nitric oxide in an experimental rat model. BJU Int 106:1230–1236
Raposo C, Nunes AK, Luna RL, et al., (2013) Sildenafil (Viagra) protective effects on neuroinflammation: the role of iNOS/NO system in an inflammatory demyelination model. Mediators Inflamm 321460. doi:10.1155/2013/321460
Bogdan S, Seferian A, Totoescu A et al (2012) Sildenafil reduces inflammation and prevents pulmonary arterial remodeling of the monocrotaline -induced disease in the Wistar Rats. Maedica (Buchar) 7(2):109–116
Gilchrist M, Hesslinger C, Befus AD (2003) Tetrahydrobiopterin, a critical factor in the production and role of nitric oxide in mast cells. J Biol Chem 278:50607–50614
Friedewald JJ, Rabb H (2004) Inflammatory cells in ischemic acute renal failure. Kidney Int 66(2):486–491
Ahluwalia A, Foster P, Scotland RS et al (2004) Anti-inflammatory activity of soluble guanylate cyclase: cGMP-dependent down-regulation of P-selectin expression and leukocyte recruitment. Proc Natl Acad Sci USA 101(5):1386–1391
Zuniga-Toala A, Zatarain-Barron ZL, Hernandez-Pando R et al (2013) Nordihydroguaiaretic acid induces Nrf2 nuclear translocation in vivo and attenuates renal damage and apoptosis in the ischemia and reperfusion model. Phytomedicine 20(10):775–779
Gang GT, Hwang JH, Kim YH et al (2014) Protection of NAD (P) H: quinine oxidoreductase 1 against renal ischemia/reperfusion injury in mice. Free Radic Biol Med 67:139–149
Chung HT, Pae HO, Choi BM, Billiar TR, Kim YM (2001) Breakthrough and views: nitric oxide as a bioregulator of apoptosis. Biochem Biophys Res Commun 282:1075–1079
Acknowledgments
This work was funded by project # CEP1-031-MANS by ministry of higher education, Egypt.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict interest
Authors declare that there is no any conflict of interest.
Additional information
Handling editor: Dr. Peter R. Merten.
Rights and permissions
About this article
Cite this article
Zahran, M.H., Hussein, A.M., Barakat, N. et al. Sildenafil activates antioxidant and antiapoptotic genes and inhibits proinflammatory cytokine genes in a rat model of renal ischemia/reperfusion injury. Int Urol Nephrol 47, 1907–1915 (2015). https://doi.org/10.1007/s11255-015-1099-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1099-5