Abstract
Objective
No study in China has so far investigated the difference in patient survival rates between hemodialysis (HD) and peritoneal dialysis (PD). Therefore, the aim of the present single-center follow-up study was to determine and compare the survival rates associated with HD and PD at a Chinese hospital.
Methods
Clinical data were analyzed for all adult patients (age >18 years) with chronic renal failure who dialysis between 2006 and 2010.
Results
The study included 216 patients, 140 of whom underwent PD and 76 of whom underwent HD. Compared to patients in the HD group, patients in the PD group were older (61 ± 14 vs. 55 ± 14 years, P = 0.004) and had higher baseline blood uric acid levels (452 ± 136 vs. 388 ± 150 μmol/L, P = 0.002) and lower baseline iPTH (224 ± 260 vs. 305 ± 267 pg/ml, P = 0.036). Moreover, a higher number of PD patients had diabetes (40 vs. 27.6 %, P = 0.056). The average follow-up time was 25 months in the PD group and 36 months in the HD group. The 1-, 2- and 3-year survival rates were 98.7, 93.2, and 85.5 %, respectively, in the HD group and 90.9, 81.5, and 73.8 %, respectively, in the PD group. In the first 3 years, HD was associated with better survival compared to the PD group. However, when adjusted for age, diabetes and BMI, there was no significant difference between the PD and HD group.
Conclusion
The mode of dialysis itself has no effect on the survival rate of ESRD patients on dialysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the rapid rise in the prevalence and incidence of end-stage renal disease (ESRD) worldwide, the number of patients undergoing dialysis continues to increase. The popular dialysis methods in use are hemodialysis (HD) and peritoneal dialysis (PD). PD can give patients more freedom than HD. The effect of the different mode of dialysis on patient survival has always been an issue of concern. The best way to compare prognostic differences between PD and HD is randomized controlled trials, but it is quite difficult to conduct such trails, because almost no one was willing to randomized to receive HD or PD. Therefore, the main studies in this field are prospective, cohort studies, and enrolled studies using registration data. Currently, some of these studies show that PD patients have a better survival rate in the first 1 or 2 years, but in the next 3–5 years, this advantage does not seem to exist, and the survival of PD patients is even worse than that of HD patients [1]. However, after the data were adjusted for age, race, gender, complications, albumin levels, and primary disease, there was no significant difference between the two dialysis modes. In China, there is a lack of such research on patient survival with different dialysis methods. With the aim of bridging this gap, this cohort study was conducted on dialysis patients at Peking University People’s Hospital, who were followed up and analyzed to compare the survival rate of the two treatment modalities, and the factors associated with survival were determined.
Patients and methods
Patients
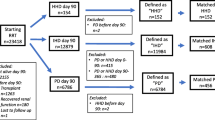
We selected adult (age ≥18 years) patients who started dialysis (PD or HD) at Peking University People’s Hospital between January 2006 and December 2010. We excluded (1) patients who were undergoing dialysis as a result of acute renal failure, (2) patients with limited life expectancy because of cancer or other serious organ disease, and (3) patients who had switched treatment from another mode of dialysis or renal transplantation. Patients were divided into the PD group and HD group.
Research methods
We collected demographic and clinical data, including gender, age, primary disease, previous history of cardiovascular disease (CVD), previous history of diabetes (DM), body mass index (BMI), blood pressure, hemoglobin, estimated glomerular filtration rate (eGFR), and levels of serum albumin, uric acid, calcium, phosphate, intact parathyroid hormone (iPTH), lipids, and electrolytes. Patients were followed up regularly, that is, at least once every 3 months, blood pressure and the levels of hemoglobin, albumin, uric acid, calcium, phosphate, lipids, and electrolytes were determined. Follow-up ended in June 2011. All end point events (deaths) and etiological factors were recorded.
The PD patients underwent continuous ambulatory PD 3–5 times per day, with 1,500–2,000 ml of dialysate (Baxter) exchanged per day. The HD patients underwent dialysis 2–3 times a week, 4 h each time, using a cellulose triacetate (Nipro) or polysulfone membrane (Fresenius) dialyzer.
Statistical analysis
All analyses and calculations were performed using the SPSS statistical package, version 17.0 (SPSS, Chicago, IL, USA). Normally distributed data are presented as mean ± standard deviation (SD). Comparison of measurement data between the two groups was performed using the independent student’s t test. Data with non-normal distribution are presented as median, and comparisons between two groups were conducted using the rank sum test. Comparison of enumeration data between the two groups was undertaken using the Chi-square test. Differences in survival rates between groups were determined using Kaplan–Meier survival analysis and the log-rank test. Factors that influenced survival were analyzed using Cox multifactor regression (gradual backward method). The statistical significance level was set at P < 0.05.
Results
Patient characteristics at the time of initiation of dialysis
The study included 216 patients, 140 of whom were in the PD group (65.1 %) and 76 of whom were in the HD group (34.9 %). Compared to the HD group, patients in the PD group were older at the time of initiation of dialysis (61 ± 14 vs. 55 ± 14 years; P = 0.004) and had higher serum uric acid (UA) concentration (452 ± 136 vs. 388 ± 150 μmol/L, P = 0.002) and lower iPTH (115.8 vs. 217.9 pg/ml, P = 0.000). Higher prevalence of DM was found in the PD group, but the difference was not statistically significant (40.7 vs. 27.6 %, P = 0.056). There were no significant differences in blood pressure or the levels of hemoglobin, albumin, lipids, and electrolytes between the two groups (Table 1).
Patient characteristics during dialysis
During dialysis, time-averaged values of PD and HD patients were compared. Patients in the PD group had a lower SBP, DBP, and MBP (96 vs. 105 mmHg, P = 0.000), a better serum uric acid, calcium, phosphate, iPTH, potassium and carbon dioxide combining power. But PD patients had a lower serum albumin (37.9 vs. 39.1 g/L, P = 0.014) and a higher cholesterol (Table 2).
Comparison of survival rates between the PD and HD groups
The 1-, 2- and 3-year survival rates in the PD group were 90.9, 81.5, and 73.8 %, respectively, and in the HD group, they were 98.7, 93.2, and 85.5 %, respectively. As can be seen, in the first 3 years, the survival rate of PD patients was worse than that of HD patients. Kaplan–Meier survival analysis showed that there was a significant difference in cumulative survival rates between the two groups (P = 0.026, Fig. 1).
Factors associated with survival in the dialysis patients
Sex, age, mode of dialysis, history of cardiovascular disease, history of DM, BMI, blood pressure, baseline eGFR, hemoglobin, serum albumin, calcium, phosphate, and uric acid at commencement of dialysis, time-averaged blood pressure, HGB, serum albumin, calcium, phosphate, and uric acid during the follow-up period were all included in the Cox model regression analysis. The results revealed that age (P = 0.000), history of DM (P = 0.002), and BMI (P = 0.002) were significantly associated with survival (Table 3).
Comparison of survival rates after adjustment for confounding factors
After adjustment for age, history of DM, and BMI, there were no significant differences in the survival curves between the PD and HD groups (Fig. 2).
Discussion
This study is the first to compare the survival of HD and PD patients in China, and it was found that the results were similar to those reported in other countries.
We compared 140 PD patients and 76 HD patients. We found that PD patients had poorer survival than HD patients. However, this is contradictory to the results of most studies, which have shown that early survival rates in PD are equal to or even better than those associated with HD [2, 3]. The results in our study may have been caused because the patients were not randomly assigned to either group: The PD patients were older than the HD patients, and the PD group also had a higher number of DM patients. This may have led to a bias in the results. Like the other published studies, Fenton [4] also found that the overall death risk associated with PD is lower than that associated with HD in Canada and that this advantage is more obvious in the first 2 years. Moreover, Termorshuizen [5] found that after 2 years of dialysis, the relative risk of death significantly increased in patients undergoing PD. A similar conclusion was made by Jaar [6] after he analyzed 1,041 new dialysis patients in the USA. The early survival advantage of PD patients may be associated with better residual renal function protection. However, with the extension of dialysis time, residual renal function decreases, and the early survival advantage cannot be maintained. Thus, even though PD is advantageous in the early treatment stages, this survival advantage is not evident later on.
In this study, after adjusting for some risk factors, there was no significant difference in the survival rate between the two groups. This is consistent with previous studies which have shown that there was no significant difference in the patient survival rate between PD and HD, for example, Vonesh’s study [7] on 398,940 dialysis patients in the USA and Huang’s study [8] on 45,820 HD patients and 2,809 PD patients in Taiwan. Consistent with the present study, these studies have shown that after adjusting for age, diabetes and other risk factors, PD and HD patients show similar outcomes. These results indicate that the dialysis mode itself does not affect the survival of dialysis patients. The difference in survival rate may thus be caused by other factors.
With regard to the risk factors associated with survival, we found that age, history of DM, and BMI were risk factors. However, the risk factors reported by other studies are not totally consistent. Matos [9] followed up 3,082 HD patients for 5 years and found that age, diabetes, and serum albumin level were prognostic factors. Moreover, Sanabria [10] observed 923 patients on dialysis and discovered that age, history of cardiovascular disease, and history of diabetes were the risk factors associated with death. In addition, Kao [11] reported that age and diabetes were risk factors for survival. Overall, most studies found that age and diabetes are factors affecting survival in dialysis patients, which is consistent with our findings. In addition to this, many studies have suggested the association of hypoalbuminemia with poor prognosis. For example, Chan [12] observed 167 HD patients and found that hypoalbuminemia is an independent risk factor for death in dialysis patients, and Goodkin [13] reported that hypoalbuminemia was a poor prognostic factor in 18,000 dialysis patients. In this study, we did not find albumin was independently associated with prognosis, but we found that another nutrition-related indicators—BMI was an independent predictor of death. Actually, in 2005, Kalantar-Zadeh [14] reported the phenomenon of “reverse epidemiology” in HD patients, wherein contrary to the trend in the general population, dialysis patients with low BMI were characterized by increased mortality compared to high BMI patients. Subsequently, the Dutch NECOSAD study [15] also confirmed the presence of the “reverse epidemiology” phenomenon in PD patients. This phenomenon was also observed in our study. Therefore, it seems that the findings in the Chinese population are more or less similar to those in other populations.
There are several limitations to the present study. First, it is a single-center study in which the patients were not randomly assigned to either group. Second, the study population is small (216 patients), and only the survival rates of the first 3 years have been compared. Therefore, there is a need to conduct a multicenter controlled study with a large sample and longer follow-up period in order to confirm all these findings.
Conclusion
In the first 3 years of dialysis, survival in the PD group was worse than that in the HD group. However, after adjustment for age, history of DM, and BMI, the survival in the PD and HD groups was found to be equal. The results demonstrate that the two modes of dialysis are not significantly different with regard to patient survival.
References
Yeates K, Zhu N, Vonesh E et al (2012) Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant 27(9):3568–3575
Schaubel DE, Morrison HI, Fenton SS (1998) Comparing mortality rates on CAPD/CCPD and hemodialysis. The Canadian experience: fact or fiction? Perit Dial Int 18(5):478–484
Rufino JM, Garcia C, Vega N et al (2011) Current peritoneal dialysis compared with haemodialysis: medium-term survival analysis of incident dialysis patients in the Canary Islands in recent years. Nefrologia 31(2):174–184
Fenton SS, Schaubel DE, DesmelIles M et al (1997) Hemodialysis versus peritoneal dialysis: a comparison of adjnsted mortality rates. Am J Kidney Dis 30(3):334–342
Termorshuizen F, Komvaar JC, Dekker FW et al (2003) Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis—analysis of the Netherlands Cooperative Study on the adequacy of Dialysis 2. J Am Soc Nephml 14(11):2851–2860
Jaar BG, Coresh J, Plantinga LC et al (2005) Comparing the risk for death with peritoneal dialysis and hemodialysis in a national cohort of patients with chronic kidney disease. Ann Intern Med 143(3):174–183
Vonesh EF, Snyder JJ, Foley RN et al (2004) The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int 66(6):2389–2401
Huang CC, Chent KF, Wu HD (2008) Survival analysis: comparing peritoneal dialysis and hemodialysis in Taiwan. Perit Dial Int 28(Suppl 3):S15–S20
Matos JP, Almeida JR, Guinsburg A et al (2011) Assessment of a five–year survival on hemodialysis in Brazil: a chort of 3082 incident patients. J Bras Nefrol 33(4):436–441
Sanabria M, Munoz J, Trillos C et al (2008) Dialysis out comes in Colombia(DOC)study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Kidney Int Suppl 108:S165–S172
Kao TW, Huang JW, Hung KY et al (2010) Life expectancy, expected years of life lost and survival of hemodialysis and peritoneal dialysis patients. J Nephrol 23(6):677–682
Chan M, Kelly J, Matterham M et al (2012) Malnutrition (subjective global assessment) scores and serum albumin levels, but not body mass index values, at initiation of dialysis are independent predictors of mortality: a 10-year Clinical Cohort Study. J Ren Nutr 22(6):547–557
Goodkin DA, Mapes DL, Held PJ (2001) The dialysis outcomes and practice patterns study (DOPPS): how can we improve the care of hemodialysis patients? Semin Dial 14(3):157–159
Kalantar-Zadeh K, Abbott KC, Salahudeen AK et al (2005) Survival advantages of obesity in dialysis patients. Am J Clin Nutr 81(3):543–554
De Mutsert R, Grootendorst DC, Boeschoten EW et al (2009) Is obesity associated with a survival advantage in patients starting peritoneal dialysis? Contrib Nephrol 163:124–131
Acknowledgments
The authors gratefully acknowledge the substantial contributions of the entire staff of peritoneal dialysis center and hemodialysis center in providing information.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, B., Wang, M., Gan, L. et al. Comparison of patient survival between hemodialysis and peritoneal dialysis in a single Chinese center. Int Urol Nephrol 46, 2403–2407 (2014). https://doi.org/10.1007/s11255-014-0819-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-014-0819-6