Abstract
Purpose
Few studies have evaluated patients’ characteristics and survival by dialysis modality in Brazil. We evaluated changes in dialysis modality and its survival in the country.
Methods
This is a retrospective database of a cohort with incident chronic dialysis patients from Brazil. Patients’ characteristics and one-year multivariate survival risk were assessed considering dialysis modality from 2011 to 2016 and 2017 to 2021. Survival analysis was also performed on a reduced sample after adjustment using propensity score matching.
Results
Of the 8295 dialysis patients, 5.3% were on peritoneal dialysis (PD) and 94.7% on hemodialysis (HD). PD patients had higher BMI, schooling and the prevalence of elective dialysis starting in the first period than those on HD. In the second period, PD patients were predominantly women, non-white, from the Southeast region, and funded by the public health system, having more frequent elective dialysis starting and predialysis nephrologist follow-ups than those on HD. There was no difference in mortality comparing PD and HD (HR 0.67, 95% CI 0.39–2.42; and HR 1.17, 95% CI 0.63–2.16; first and second period, respectively). This non-significantly different survival between both dialysis methods was also found in the reduced matched sample. Higher age and non-elective dialysis initiation were associated with higher mortality. In the second period, the lack of predialysis nephrologist follow-up and living in the Southeast region increased the mortality risk.
Conclusion
Some sociodemographic factors have changed according to dialysis modality over the last decade in Brazil. The one-year survival of the two dialysis methods was comparable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the all-cause mortality of patients on dialysis has decreased in the last decades [1], it is estimated that about 50% of patients who start some dialysis method will die within five years [2, 3]. Brazil has the third-largest absolute number of patients on dialysis worldwide [4]. However, studies have not directly evaluated differences in patients’ characteristics and survival by dialysis modality in the Brazilian population [5, 6].
Whilst optimal randomised control trials to compare peritoneal dialysis (PD) or hemodialysis (HD) are limited [7, 8], the data from observational cohort studies have not consistently demonstrated a difference in the survival by dialysis modality [7, 9, 10]. It is conceivable that non-diabetic and younger patients on PD have higher survival in the first two years of treatment compared with HD [11,12,13,14].
About 7% of the patients with kidney failure in dialysis treatment worldwide are in Brazil. Also, the Brazilian estimated prevalence of patients on chronic dialysis has increased from 405 per million population (pmp) in 2009 to 640 pmp in 2018, corresponding to an average annual increase of 6.4% [15]. Although the number of patients on PD is increasing in some countries [16], the prevalence in Brazil is decreasing, and the method continues to be more utilised in experienced centres from some country regions [6, 15]. One of the main reasons is the lower reimbursement to the staff working with PD than HD [17, 18]. Also, the lack of local data on survival differences by modality may be a contributing factor.
The objectives of the present study were to draw the profile of a large chronic dialysis population in Brazil and compare the 1-year survival in incident PD and HD patients across two time periods, considering several independent risk factors.
Methods
Study design
This is a retrospective analysis of the Brazilian Dialysis Registry (BDR), an electronic database to collect clinical and epidemiological information from patients undergoing dialysis therapy in the country. The BDR was created in 2010 and is coordinated by the Brazilian Society of Nephrology (BSN). The methods for the BDR data collection have been published in detail elsewhere [19]. The ethics committee of the Federal University of São Paulo approved this study.
Sampling
This study evaluated data from all adult (> 18 years old) incident dialysis patients included in the BDR from January 2011 to September 2021, with the first chronic dialysis data available. We excluded participants without age information and those with a follow-up shorter than 90 days. We compared HD and PD participants' characteristics across the population by dividing the study sample into two groups according to the year of dialysis start: 2011–2016 (first period) and 2017–2021 (second period). The studied variables were: gender, age, ethnicity, education, body mass index, CKD aetiology, dialysis funding, diabetes history, elective dialysis start, predialysis nephrologist follow-up, and geographical region. In addition, we combined the data of the geographical regions North, Northeast, and Middle West due to the small number of participants in each of these regions and compared them with Southeast and South. One-year survival after initiation of dialysis was considered as the endpoint.
Statistical analysis
Qualitative variables were described by frequency and percentage; mean and standard deviation were used for quantitative variables. The Kolmogorov–Smirnov test assessed the normality of data distribution. We used a chi-square test and Student’s t test to compare frequencies or means of the secondary variables about the primary exposure (dialysis modality) for the whole sample and by period. The crude mortality ratio (RR) to death within the first year after starting HD versus PD was calculated per 1000 person-days per period. The Kaplan–Meier method performed a survival analysis concerning the dialysis modality to the outcome, and the log-rank test verified differences per period of BDR. Univariate analysis and multivariate Cox regression models were proposed to verify the association between the dialysis modality and mortality within the first year after starting dialysis per period (2011–2016 and 2017–2021). The multivariate Cox regression analysis included all variables with a p value lower than 0.20 to the outcome in the univariate method. A final multivariate model was proposed after using a manual backward elimination to adjust all more significant variables in the model, keeping fixed gender and age, considering their known confounder effect in the exposure and outcome studied. The likelihood test was used to evaluate any interaction factor for the principal exposure variable with the other variables. Important effect modification was considered when a significant effect by subgroups was found. For multivariate analysis, the linear effects for categorical variables BMI by tercile, schooling, and region were verified through a test of departure from linear trend. The proportional hazard assumption in the Cox regression analysis was verified by Nelson−Aalen plots and by a formal test of proportionality.
Sensitive analysis
Propensity score matching was performed to estimate the effect of the dialysis method on mortality risk accounting for confounder variables. Considering many cases with missing values for BMI, aetiology, schooling, predialysis nephrological care, and elective dialysis start, these variables were not included in the matching method. We used 1:1 nearest neighbour propensity score matching without replacement with a calliper of 0.1. Observations were discarded in both groups, and patients who could not be matched were deleted from the analyses. The propensity score was estimated using a logistic regression of the group (peritoneal dialysis/hemodialysis) on the covariates (age, sex, ethnicity, geographical region, diabetes, period of dialysis start, and health insurance type). Similarly, the Kaplan–Meier method performed a survival analysis of the dialysis modality in the whole period and univariate and multivariate Cox regression analysis testing the other covariates not included in the matching. All data were analysed using STATA/IC 15.1 software.
Results
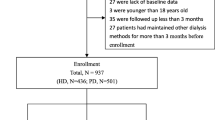
A total of 20,597 incident dialysis patients were identified from January 2011 to September 2021. Patients without dialysis modality data (n = 6371), with age lower than 18 years or no age data (n = 135), or without dialysis vintage of more than 90 days (n = 5796) were excluded. After applying the exclusion criteria, 8295 were selected for analysis. HD patients represented 94.7% (n = 7856) and PD patients 5.3% (n = 439) of the sample. When compared with patients excluded due to 90 days follow-up missing data, included participants had similar gender distribution, were younger, more educated, had a higher prevalence of white ethnicity, diabetes, and living in the Southeast region.
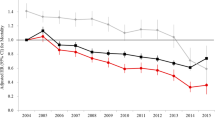
HD and PD patients’ characteristics are shown in Tables 1 (whole sample) and 2 (by periods of dialysis initiation). In the entire sample, except for age and gender, the distribution of all other studied variables differed between groups for the non-matched sample. Patients on PD had higher mean BMI values, were predominantly non-white, had a higher level of education, were more often funded by the public health system, had planned dialysis initiation, and were seen by a nephrologist in the predialysis phase of CKD. Besides, patients on PD were more often from the Southeast region and had a lower prevalence of diabetes. In the matched sample, there was no significant difference between the distribution of matched variables (age, sex, period, ethnicity, dialysis funding, geographical region, and diabetes history) according to the type of dialysis. The other characteristics remained similar to the non-matched sample. In the overall sample, the crude mortality ratio between PD and HD was 1.03 per 1000 person-years (95% CI 0.57–1.84, p = 0.922) in the first period (2011 to 2016) and 0.72 per 1000 person-years (95% CI 0.47–1.11, p = 0.135) in the second period (2017–2021). There was no difference in the cumulative mortality rate by modality within the first year after starting dialysis, both in the non-matched (Fig. 1) and the matched sample (Fig. 2, supplementary).
When comparing the characteristics of all patients by dialysis modality by period (Table 2), patients on PD in the first period had higher BMI, schooling, and prevalence of elective dialysis starts, and more often from the Southeast region compared to those on HD. In the second period, patients on PD had a higher proportion of women, non-white skin colour, public dialysis funding, elective starting of dialysis, and predialysis nephrology care, and, more often, derived from the Southeast region. In this period (2017–2021), patients starting on PD had a lower prevalence of diabetes than those starting on HD.
Associations and predictors of death within the first year after dialysis initiation by period are shown in Table 3. In the overall sample, the independent predictors of mortality in both periods were higher age and non-elective dialysis initiation. In the first period, men had a lower mortality risk. In the second period, the lack of predialysis nephrologist follow-up and living in the Southeast region also increased the mortality risk. For both periods, the dialysis modality was not associated with higher mortality risk after adjusting for other variables (HR 0.67, 95% CI 0.39–2.42, p = 0.963; and HR 1.17, 95% CI 0.63–2.16, p = 0.626; first and second periods, respectively).
In the matched sample, there was a trend towards lower mortality for patients on PD compared to those on HD (HR = 0.63; 95% CI 0.38–1.05; p = 0.075) in the univariate analysis. However, this association lost strength after adjustment for other confounding variables not included in the matching.
Discussion
In this large observational study, PD was not associated with higher mortality risk in the first year after starting dialysis compared with those on HD. Whilst increasing age and non-elective dialysis initiation were associated with a higher chance of mortality in both periods, differences in the region of origin and the frequency of predialysis follow-up by a nephrologist were found in the second period. To the best of our knowledge, this is the first study to assess the impact of the type of dialysis modality on short-term mortality considering a large Brazilian dataset.
The distribution of incident HD and PD patients in the whole sample was the same in both periods. However, compared to the national data of prevalent dialysis patients, in which the PD prevalence ranged from around 10% in the earliest 2010 years and close to 7.5% in the latest decade years [15], our population comprised a lower percentage of PD patients. When compared with a large Brazilian cohort of incident PD patients (BRAZPD) that started dialysis in 2004–2011 (n = 5707) [6], our participants had similar ages, a slightly higher prevalence of men (54% vs 48%), and a lower prevalence of diabetic kidney disease (18 vs 37%). However, that cohort represented 65–70% of all PD patients in the country and was limited to patients using supplies from only one company [6]. Regarding incident HD patients, comparing our data with another large Brazilian study that included 3,082 patients from 2000 to 2004 [5], our participants were older (58 vs 52 years) and had a similar prevalence of men (59% vs 58%) and diabetic nephropathy (22 vs 20%). However, that large study was limited to patients from 7 of the 26 states in Brazil, with all centres run by the same dialysis franchise company.
When considering the whole sample, except for age and gender, all other parameters evaluated in the present study differed significantly between PD and HD patients. Patients on PD had higher BMI, lower prevalence of diabetes, were more often non-white, from the Southeast region, funded by the public health system, and with a more common planned dialysis start than those on HD. These characteristics have been found in other Brazilian studies about PD patients [20, 21]. People starting PD in the second period tended to be older. We also found a higher prevalence of illiteracy amongst PD patients and more frequent funding by the public health system in the second period compared with the first one. Low schooling has been accounted for as one of the reasons for the lower prevalence of PD in Brazil. However, the proportion of illiterates has not been lower in PD patients compared with the general population [20]. These differences in public dialysis funding and illiteracy amongst PD patients in the analysed periods may reflect the better socioeconomic characteristics of the Southeastern region, where the largest number of PD patients are concentrated. When compared with the public system, the lower proportion of patients on PD than HD with non-public funding may reflect the higher reimbursement paid for HD by private health insurance companies.
Brazil has a large territory extension, with many dialysis patients living more than 50 km from the dialysis centre [22]. Although regions with lower public health investment per capita are associated with higher mortality of patients on PD [21], such dialysis modality has a lower overall cost [18] and could be a feasible alternative to reduce the patient dislocation. However, our findings indicate that the PD method is still centralised in the country’s most developed region (Southeastern), and that pattern has not changed over time. Besides, although urgent-start peritoneal dialysis has increased in the latest years in our country [23, 24], HD is still the most prevalent modality to start non-elective dialysis. Notably, there was a higher proportion of PD patients with elective dialysis start and predialysis nephrology care than HD patients. Late diagnosis of CKD and lack of early nephrology care are still rife in Brazil. Conceivably, the improvement in predialysis assistance could contribute to the expansion of PD modality.
Adjusted mortality at one year did not differ between incident patients on PD and HD, regardless of the period analysed, even after balancing the sample by propensity score matching. The lack of short-term survival advantage between both modalities has been shown in some populations worldwide [25,26,27,28]. In contrast, in others, survival favoured PD in the first years of dialysis [29, 30]. The increase in age and the non-elective indication to start dialysis were associated with higher mortality in multivariate models of both periods. Ageing has been a known factor associated with higher mortality in dialysis patients [11, 31]. Regarding non-elective dialysis, patients starting dialysis in an unplanned way have shown higher mortality risk [32,33,34], especially the elderly ones [35]. In the second period, patients from other regions of Brazil presented a lower risk of mortality when compared to the region with the largest contingent of patients on dialysis, the Southeastern. The population residing in the Southeastern is older than in the other regions grouped in the analysis [15]. This may be a factor accounting for the higher mortality. However, considering the smaller number of patients from the North and Northeast regions in the present study, this protective effect needs further investigation. Despite the impossibility of evaluating the role of other comorbidities due to the lack of information, diabetes had a marginally protective effect on mortality in the univariate analysis in the second period, and it was not significant in the multivariate analysis. Diabetes and poor glycemic control have been considered risk factors for mortality amongst dialysis patients [36, 37]. The short-term follow-up and the lack of precision in the diabetes classification may have influenced our findings.
There are some limitations in the present study. First, despite our efforts, several missing data limited the final sample size. Although this is a large national study and some major sample characteristics have been similar to some previous Brazilian reports, it is impossible to rule out a selection bias. Besides, other comorbidities, medications used, and laboratory parameters were not possible to include in the analysis, limiting the adjustments for confounders.
The strengths of our study include the assessment of a large population of incident dialysis patients in a country that is the third-largest in kidney replacement therapy worldwide, something that has increased the interest of international dialysis corporations in the Brazilian dialysis market.
Our study provides information about kidney failure patients starting KRT on PD or HD, including their sociodemographic profile, some features of their predialysis assistance, dialysis funding, and one-year adjusted mortality risk. These data provide valuable information to help choose the modality to start dialysis and bring to light the need for changes in the dialysis reimbursement policy to boost PD in the country.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Boenink R, Stel VS, Waldum-Grevbo BE, Collart F, Kerschbaum J, Heaf JG, de Meester J, Finne P, Garcia-Marcos SA, Evans M, Ambuhl PM, Arici M, Ayav C, Steenkamp R, Cases A, Traynor JP, Palsson R, Zoccali C, Massy ZA, Jager KJ, Kramer A (2020) Data from the ERA-EDTA Registry were examined for trends in excess mortality in European adults on kidney replacement therapy. Kidney Int 98(4):999–1008. https://doi.org/10.1016/j.kint.2020.05.039
Kramer A, Boenink R, Stel VS, Santiuste de Pablos C, Tomovic F, Golan E, Kerschbaum J, Seyahi N, Ioanou K, Beltran P, Zurriaga O, Magaz A, Slon Roblero MF, Gjorgjievski N, Garneata L, Arribas F, Galvao AA, Bell S, Ots-Rosenberg M, Munoz-Terol JM, Winzeler R, Hommel K, Asberg A, Spustova V, Palencia Garcia MA, Vazelov E, Finne P, Ten Dam M, Lopot F, Trujillo-Aleman S, Lassalle M, Kolesnyk MO, Santhakumaran S, Idrizi A, Andrusev A, Comas Farnes J, Komissarov K, Resic H, Palsson R, Kuzema V, Garcia Bazaga MA, Ziginskiene E, Stendahl M, Bonthuis M, Massy ZA, Jager KJ (2021) The ERA-EDTA registry annual report 2018: a summary. Clin Kidney J 14(1):107–123. https://doi.org/10.1093/ckj/sfaa271
Saran R, Robinson B, Abbott KC, Bragg-Gresham J, Chen X, Gipson D, Gu H, Hirth RA, Hutton D, Jin Y, Kapke A, Kurtz V, Li Y, McCullough K, Modi Z, Morgenstern H, Mukhopadhyay P, Pearson J, Pisoni R, Repeck K, Schaubel DE, Shamraj R, Steffick D, Turf M, Woodside KJ, Xiang J, Yin M, Zhang X, Shahinian V (2020) US renal data system 2019 annual data report: epidemiology of kidney disease in the united states. Am J Kidney Dis 75(1 Suppl 1):A6–A7. https://doi.org/10.1053/j.ajkd.2019.09.003
Thurlow JS, Joshi M, Yan G, Norris KC, Agodoa LY, Yuan CM, Nee R (2021) Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am J Nephrol 52(2):98–107. https://doi.org/10.1159/000514550
Matos JP, Almeida JR, Guinsburg A, Marelli C, Barra AB, Vasconcellos MS, Jose D’Almeida Filho E, Hoette M, Ruzany F, Lugon JR (2011) Assessment of a five-year survival on hemodialysis in Brazil: a cohort of 3,082 incident patients. J Bras Nefrol 33(4):436–441
de Moraes TP, Figueiredo AE, de Campos LG, Olandoski M, Barretti P, Pecoits-Filho R, Investigators B (2014) Characterization of the BRAZPD II cohort and description of trends in peritoneal dialysis outcome across time periods. Perit Dial Int 34(7):714–723. https://doi.org/10.3747/pdi.2013.00282
Vale L, Cody J, Wallace S, Daly C, Campbell M, Grant A, Khan I, Donaldson C, Macleod A (2004) Continuous ambulatory peritoneal dialysis (CAPD) versus hospital or home haemodialysis for end-stage renal disease in adults. Cochrane Database Syst Rev 4:CD003963. https://doi.org/10.1002/14651858.CD003963.pub2
Korevaar JC, Feith GW, Dekker FW, van Manen JG, Boeschoten EW, Bossuyt PM, Krediet RT, Group NS (2003) Effect of starting with hemodialysis compared with peritoneal dialysis in patients new on dialysis treatment: a randomized controlled trial. Kidney Int 64(6):2222–2228. https://doi.org/10.1046/j.1523-1755.2003.00321.x
Elsayed ME, Morris AD, Li X, Browne LD, Stack AG (2020) Propensity score matched mortality comparisons of peritoneal and in-centre haemodialysis: systematic review and meta-analysis. Nephrol Dial Transplant 35(12):2172–2182. https://doi.org/10.1093/ndt/gfz278
Ross S, Dong E, Gordon M, Connelly J, Kvasz M, Iyengar M, Mujais SK (2000) Meta-analysis of outcome studies in end-stage renal disease. Kidney Int 57:S28–S38. https://doi.org/10.1046/j.1523-1755.2000.07406.x
Collins AJ, Hao W, Xia H, Ebben JP, Everson SE, Constantini EG, Ma JZ (1999) Mortality risks of peritoneal dialysis and hemodialysis. Am J Kidney Dis 34(6):1065–1074. https://doi.org/10.1016/S0272-6386(99)70012-0
Liem YS, Wong JB, Hunink MG, de Charro FT, Winkelmayer WC (2007) Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int 71(2):153–158. https://doi.org/10.1038/sj.ki.5002014
Schaubel DE, Morrison HI, Fenton SS (1998) Comparing mortality rates on CAPD/CCPD and hemodialysis. The Canadian experience: fact or fiction? Perit Dial Int 18(5):478–484
Xue J, Li H, Zhou Q, Wen S, Zhou Q, Chen W (2019) Comparison of peritoneal dialysis with hemodialysis on survival of diabetic patients with end-stage kidney disease: a meta-analysis of cohort studies. Ren Fail 41(1):521–531. https://doi.org/10.1080/0886022X.2019.1625788
Neves P, Sesso RCC, Thome FS, Lugon JR, Nasicmento MM (2020) Brazilian dialysis census: analysis of data from the 2009–2018 decade. J Bras Nefrol 42(2):191–200. https://doi.org/10.1590/2175-8239-JBN-2019-0234
Jain AK, Blake P, Cordy P, Garg AX (2012) Global trends in rates of peritoneal dialysis. J Am Soc Nephrol 23(3):533–544
Sesso R, Lugon JR (2020) Global dialysis perspective: Brazil. Kidney 360(1):216–219
de Abreu MM, Walker DR, Sesso RC, Ferraz MB (2013) A cost evaluation of peritoneal dialysis and hemodialysis in the treatment of end-stage renal disease in Sao Paulo. Brazil Perit Dial Int 33(3):304–315. https://doi.org/10.3747/pdi.2011.00138
Lugon JR, Gordan PA, Thome FS, Lopes AA, Watanabe YJA, Tzanno C, Sesso RC (2018) A web-based platform to collect data from ESRD patients undergoing dialysis: methods and preliminary results from the brazilian dialysis registry. Int J Nephrol 2018:9894754. https://doi.org/10.1155/2018/9894754
Fernandes N, Bastos MG, Cassi HV, Machado NL, Ribeiro JA, Martins G, Mourao O, Bastos K, Ferreira Filho SR, Lemos VM, Abdo M, Vannuchi MT, Mocelin A, Bettoni SL, Valenzuela RV, Lima MM, Pinto SW, Riella MC, Qureshi AR, Divino Filho JC, Pecoits-Filho R, Brazilian Peritoneal Dialysis Multicenter S (2008) The Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD): characterization of the cohort. Kidney Int Suppl 108:S145-151. https://doi.org/10.1038/sj.ki.5002616
Loesch G, Cruz JAW, Pecoits-Filho R, Figueiredo AE, Barretti P, de Moraes TP (2020) Public health investments and mortality risk in Brazilian peritoneal dialysis patients. Clin Kidney J 13(6):1012–1016. https://doi.org/10.1093/ckj/sfaa118
Fernandes NM, Chaoubah A, Bastos K, Lopes AA, Divino-Filho JC, Pecoits-Filho R, Bastos MG (2010) Geography of peritoneal dialysis in Brazil: analysis of a cohort of 5,819 patients (BRAZPD). J Bras Nefrol 32(3):268–274
Bitencourt Dias D, Mendes ML, Burgugi Banin V, Barretti P, Ponce D (2017) Urgent-start peritoneal dialysis: the first year of brazilian experience. Blood Purif 44(4):283–287. https://doi.org/10.1159/000478970
Ferreira HC, Nerbass FB, Calice-Silva V (2021) Assessment of patients referred to urgent start peritoneal dialysis: when does the nurse contraindicate? J Bras Nefrol 43(1):47–51. https://doi.org/10.1590/2175-8239-JBN-2020-0072
Wong B, Ravani P, Oliver MJ, Holroyd-Leduc J, Venturato L, Garg AX, Quinn RR (2018) Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis 71(3):344–351. https://doi.org/10.1053/j.ajkd.2017.08.028
Huang CC, Cheng KF, Wu HD (2008) Survival analysis: comparing peritoneal dialysis and hemodialysis in Taiwan. Perit Dial Int 28(Suppl 3):S15-20
Choi JY, Jang HM, Park J, Kim YS, Kang SW, Yang CW, Kim NH, Cho JH, Park SH, Kim CD, Kim YL, Clinical Research Center for End Stage Renal Disease I (2013) Survival advantage of peritoneal dialysis relative to hemodialysis in the early period of incident dialysis patients: a nationwide prospective propensity-matched study in Korea. PLoS One 8(12):e84257. https://doi.org/10.1371/journal.pone.0084257
Zhou H, Sim JJ, Bhandari SK, Shaw SF, Shi J, Rasgon SA, Kovesdy CP, Kalantar-Zadeh K, Kanter MH, Jacobsen SJ (2019) Early mortality among peritoneal dialysis and hemodialysis patients who transitioned with an optimal outpatient start. Kidney Int Rep 4(2):275–284. https://doi.org/10.1016/j.ekir.2018.10.008
Yeates K, Zhu N, Vonesh E, Trpeski L, Blake P, Fenton S (2012) Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant 27(9):3568–3575. https://doi.org/10.1093/ndt/gfr674
Kumar VA, Sidell MA, Jones JP, Vonesh EF (2014) Survival of propensity matched incident peritoneal and hemodialysis patients in a United States health care system. Kidney Int 86(5):1016–1022. https://doi.org/10.1038/ki.2014.224
Tazza L, Di Napoli A, Bossola M, Valle S, Pezzotti P, Luciani G, Di Lallo D, Lazio Dialysis R (2009) Ageing of patients on chronic dialysis: effects on mortality–a 12-year study. Nephrol Dial Transplant 24(3):940–947. https://doi.org/10.1093/ndt/gfn575
Metcalfe W, Khan ZH, Prescott GJ, Simpson K, MacLeod AM (2000) Can we improve early mortality in patients receiving renal replacement therapy? Kidney Int 57:2539–2545
Shimizu Y, Nakata J, Yanagisawa N, Shirotani Y, Fukuzaki H, Nohara N, Suzuki Y (2020) Emergent initiation of dialysis is related to an increase in both mortality and medical costs. Sci Rep 10(1):19638. https://doi.org/10.1038/s41598-020-76765-0
Sesso R, Belasco AG (1996) Late diagnosis of chronic renal failure and mortality on maintenance dialysis. Nephrol Dial Transplant 11(12):2417–2420. https://doi.org/10.1093/oxfordjournals.ndt.a027207
Roy D, Chowdhury AR, Pande S, Kam JW (2017) Evaluation of unplanned dialysis as a predictor of mortality in elderly dialysis patients: a retrospective data analysis. BMC Nephrol 18(1):364. https://doi.org/10.1186/s12882-017-0778-0
Soleymanian T, Kokabeh Z, Ramaghi R, Mahjoub A, Argani H (2017) Clinical outcomes and quality of life in hemodialysis diabetic patients versus non-diabetics. J Nephropathol 6(2):81–89. https://doi.org/10.15171/jnp.2017.14
Broumand B (2007) Diabetes: changing the fate of diabetics in the dialysis unit. Blood Purif 25(1):39–47. https://doi.org/10.1159/000096396
Acknowledgements
Brazilian Dialysis Register Investigators: Beatriz Veneza; Carlos Eduardo Comin; Yoshimi Watanabe; João Carlos Biernat; Patrícia Sigolo Teixeira; Sérgio Gardano Elias Bucharles; Elzo Ribeiro Junior; Geraldo Antunes Córdova; Marcelo Augusto Gonçalves; Gisele Fernandes Furtado; Roberto Eduardo Salon; Milene Cristina Devito Guilhem; Hotone Dallacosta; Marco Túlio; Renato Jorge Palmeira de Medeiros; Elisa de Albuquerque Sampaio; Jorge Luiz Zanette Ramos; Gelson Antonio dos Santos; Orlando Belin Junior; Neyde Vinhacico Pontes; Ana Cristina Matos; Ciro Tavares Costa; Luiz Felipe B. de Figueiredo; Sílvia Corradi Faria de Medeiros; Cyro Nogueira Fraga Moreira Filho; Homero Neto de Cunha e Agra Sul; Wagner Santa Catharina; Sandra Teresa de Souza Neiva Coelho; Manif Curi Jorge; Mendell Douglas Lemos; Rodrigo Motta Pereira; Maziael Moraes; Helio Enzio Galvão; Rosilene Coelho; Ronaldo Luiz Ennes Allão; Luiz Claudio Albuquerque Gonçalves; Jair Batista Miguel; Rosa Malta; Jorge Arnaldo Valente de Menezes; Raimundo Martins Neto; Maria Emilia Duarte Diniz; Sinaria Amaral Ojeda; Flávio José Dutra de Moura; Luciana Fernandes Serpa; Tania Duran Sobral; Marcos Ari Mura; Ana Cláudia Vaz do Amaral Barbosa; Marcos Gevert ; Nelson José; Zita Maria Leme; Márcio Azevedo Moraes; Fabia Fernandez; Natasha Silva Constancio; Roberto Benvenutti; Ian Robert Rehfeldt; Julio Cesar; Marilia Bahiense Oliveira; Flavio Menezes de Paula; Nilsa do Rosario Martins; Dra. Denise de Melo; Ismar Caetano Monteiro Junior; Jeronimo Ruiz Centeno; Luiz Antonio C. Pais; Consuelo Veloso de Carvalho; Aparecida Paula Gondim Visoná; Maria Goretti Polito; Januário Gonçalves Roberto; Glória Maria Furatado dos Reis; João Damásio Sottero Simões; Tânia Brandão; Fernando Saldanha Thomé; Ana Lydia Cabeça; Marcos Scheidemantel; Márcia Beatriz Hexsel Abichequer; Eli Nogueira da Silva; Silvana Mourão Oliveira; Renata Lamego Starling; José Miguel Viscarra Obregón; Marcelo Freire Ruas; Antonio Alberto Coelho de Brito; Ana Bela de Barros Palazzo; Mario Ernesto Rodrigues; Rafael Cruzeiro Siqueira; Aluizio da Costa e Silva; Nilso Moreira; Maria de Fátima Alvarenga; João Carvalho Filho; André Luiz Marassi; Rodrigo Braz; Cristiano Viana da Silva; Fernanda Salomão Gorayeb Polacchini; Henrique Luiz Carrascossi; Leandro Júnior Lucca; Gelzie Sorrentino Ennes.
Funding
This study has been done without funding or support grants.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest in relation to the study performed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Brazilian Dialysis Register Investigators are listed in Acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
do Nascimento Lima, H., Nerbass, F.B., Lugon, J.R. et al. Characteristics and 1-year survival of incident patients on chronic peritoneal dialysis compared with hemodialysis:a large 11-year cohort study. Int Urol Nephrol 55, 2025–2033 (2023). https://doi.org/10.1007/s11255-023-03489-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03489-1