Abstract
The aim of this study was to evaluate the prevalence and awareness of symptoms suggestive of underactive bladder (UAB) in a heterogeneous, non-specific population to garner additional epidemiologic information about UAB. After IRB approval, an 18-item survey was mailed to 5,000 people living in metro Detroit to collect demographic data and questions regarding clinical urinary symptoms and familiarity with UAB. A total of 633 subjects (13; 54 % men, 46 % women) returned the survey. Nearly one quarter (23 %, n = 137) of respondents reported difficulty emptying his/her bladder, yet only 11 % (n = 70) had ever heard of UAB. The study results indicated that patient-reported bladder emptying symptoms are prevalent, as common in women as men, and significantly associated with comorbidity and poor self-reported health. The results suggest that the burden and impact of UAB might be significant and that a syndromic concept of UAB warrants research to determine the true burden of disease, increase awareness, and broaden efforts to investigate therapeutic directions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Underactive bladder (UAB) is a term that remains underutilized clinically due to a paucity of research, lack of consensus on terminology, and insufficient standardization of diagnostic criteria. Whereas detrusor underactivity (DU) is urodynamically defined, underactive bladder may be a more appropriate clinical syndromic term that encompasses the symptoms and signs of DU. While a variety of descriptors, symptom constellations, and related terms have been used interchangeably, the only formal definition for the underactive bladder is maintained by the International Continence Society (ICS). According to the ICS, DU is defined as “a contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying within a normal time span” [1]. Though this definition serves as an adequate foundation, it allows for broad subjectivity and lacks strict parameters. Without hard-and-fast guidelines, diagnosis and classification will remain imprecise. Further, accurate epidemiology depends upon having a clearly defined population.
Yet, despite its limited clinical recognition, the breadth of the effect of UAB should not be underestimated. Lower urinary tract dysfunction is especially prevalent among the elderly population and as the US population continues to grow older, the number of people affected and the associated costs will escalate [2]. Largely due to the aging ‘baby boomer’ generation, from 2000 to 2010, the US population aged 45–64 has grown at a rate of 31.5 % compared to 2.6 % growth in those <18 years old, which makes improving our understanding and treatment options of UAB a tremendous priority [2, 3]. The goal was to evaluate the prevalence and awareness of symptoms suggestive of UAB in a heterogeneous, non-specific population to garner additional epidemiologic information about UAB.
Methods
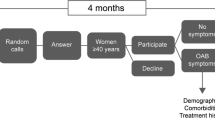
After IRB approval, an 18-item survey was mailed to 5,000 people living in metro Detroit to collect demographic data, medical and surgical history, and questions regarding clinical urinary symptoms and familiarity with UAB. Residents aged 60 and above living in Wayne, Oakland, or Macomb Counties in the greater Detroit, MI area received the self-administered UAB questionnaire (UAB-q) via targeted mailing. The mailing list was randomly generated by an independent third party based on the study parameters. Using the ICS definition as a guideline, questions that targeted symptoms were used to evaluate for UAB. Specifically, “difficulty completely emptying” the bladder was used as a proxy for UAB. Self-reported difficulty emptying the bladder (DESx) and various participant variables including demographic data, history of catheter use, and concurrent medical conditions were evaluated for association using χ 2 tests. P ≥ 0.05 was considered to be significant.
Results
A total of 633 subjects (13; 54 % men, 46 % women) returned the survey. Respondents ranged from 33 to 92 years old, though 97 % were aged 60 and above, with a mean of 74.3 years and a median age of 74. Nearly one quarter (23 %, n = 137) of respondents reported difficulty emptying his/her bladder (DESx), yet only 11 % (n = 70) had ever heard of UAB. There was no significant association between DESx and gender (p = 0.079) or age (p = 0.075) (Fig. 1). While 52 % of all respondents reported never having to strain to empty their bladder, the other 48 % recounted needing to push, bear down, or strain to empty, at least rarely to very often.
Though the exact pathophysiology of UAB is unclear, multiple coexisting conditions have been implicated in its development and progression. The DESx group were more likely to report diabetes (65 vs. 35 %, p = 0.0012), stroke (60 vs. 40 %, p = 0.066), and recurrent bladder infections (≥3 per year) (68 vs. 32 %, p < 0.0001) (Table 1). Additionally, women with a history of hysterectomy (p = 0.0008) or prolapse/incontinence surgery (p < 0.0001) were significantly more likely to have difficulty with bladder emptying. UAB was more common in men with prior prostate surgery (17 vs. 7 %, p = 0.016).
Lower urinary tract symptoms (LUTS) including those caused by UAB have an appreciable impact on daily living and quality of life. Persons reporting DESx were twice as likely to describe their health as ‘poor’ or ‘fair’ compared to those without the complaint (26 vs. 12 %, p < 0.001). Those with difficulty emptying their bladder were 70 % more likely to describe their health as ‘poor’ or ‘fair’ than expected on the basis of the null hypothesis.
Discussion
Patient-reported bladder emptying symptoms are prevalent, as common in women as men, and significantly associated with comorbidity and poor self-reported health. Despite the lack of attention this condition has received, its burden is appreciable. LUTS exert both an economic and emotional burden; studies have found that incontinence is an important predictor of institutionalization in the elderly [4]. The symptoms of DU—straining, incontinence, loss of bladder sensation—range from physically bothersome to socially restrictive [5]. A recent study by Jeong et al. [6] examined the prevalence of DU in 1,179 elderly men and women aged over 65 years with non-neurogenic voiding dysfunction presenting with LUTS and found that upwards of 40 % of men and 13.3 % of women met urodynamic parameters for DU, and the numbers increased with age in both groups. Another study of 181 community-dwelling elderly with LUTS identified impaired detrusor contractility (IDC) in urodynamic studies in 48 % of men and 12 % of women. Of the men in this study, 40 % were found to have concomitant bladder outlet obstruction (BOO); 10 % of those with IDC had BOO [7]. These studies suggest the prevalence of UAB is higher among men than women; they only included participants using urodynamic parameters. Thus, identification of UAB based upon symptomatology may be epidemiologically divergent. Further, the presence of diabetes, BOO, neurologic dysfunction, history of catheterization, and retention complicate the picture and appear to be positively associated with UAB. These studies and our own imply that DU is common and morbid, yet the true prevalence remains largely unknown.
A number of conditions complicate the picture of DU. Despite finding no association between DESx and age in this study population, research does indicate that age-related changes and BOO in particular are common and extremely difficult to distinguish from a purely underactive bladder. DU may occur concurrently with other disorders such as detrusor overactivity and BOO. Consequently, diagnosis of DU based upon clinical symptoms is complex [8]. A recently published paper by Osman et al. [9] reviewed the current understanding of UAB in the clinical literature and concluded that attempts at redefinition must address the limitations of the ICS definition as well as the inability to distinguish DU from other LUTS on the basis of symptoms alone. Our study also supports the overlap and lack of recognition in patients between UAB and other LUTS. There is much research and education that remains to be done to bridge the gap between academic research and patient-physician communication.
Limitations to this study include the narrow sample size and region, which may restrict the generalizability of the results. Additionally, this was a self-administered survey, which required literacy and given the relatively low response rate we must acknowledge the potential for significant non-response bias, specifically that those who did not answer the survey disregarded it due to lack of relevance.
Conclusions
In a population-based survey, nearly one quarter (23 %, 137/633) of respondents reported difficulty emptying his/her bladder, yet only 11 % had ever heard of UAB. The pathogenesis, epidemiology, clinical management, and treatment options for the condition of the underactive bladder remain largely opaque because of a profound gap in awareness and understanding. This gap has been perpetuated by a lack of objective standards by which to quantify and confidently diagnose. A syndromic concept of UAB warrants research to determine the true burden of disease, increase awareness among patients and providers, and broaden efforts to investigate therapeutic directions.
Abbreviations
- BOO:
-
Bladder outlet obstruction
- DESx:
-
Difficulty emptying bladder symptoms
- DU:
-
Detrusor underactivity
- ICS:
-
International Continence Society
- IDC:
-
Impaired detrusor contractility
- LUTS:
-
Lower urinary tract symptoms
- UAB:
-
Underactive bladder
- UAB-q:
-
Underactive bladder questionnaire
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A, Standardisation Sub-committee of the International Continence S (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21(2):167–178
Dubeau CE (2006) The aging lower urinary tract. J Urol 175(3 Pt 2):S11–S15. doi:10.1016/S0022-5347(05)00311-3
Howden LM, Meyer JA (2011) Age and sex composition: 2010. United States Census Bureau. http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf
Nuotio M, Tammela TL, Luukkaala T, Jylha M (2003) Predictors of institutionalization in an older population during a 13-year period: the effect of urge incontinence. J Gerontol A Biol Sci Med Sci 58(8):756–762
Miyazato M, Yoshimura N, Chancellor MB (2013) The other bladder syndrome: underactive bladder. Rev Urol 15(1):11–22
Jeong SJ, Kim HJ, Lee YJ, Lee JK, Lee BK, Choo YM, Oh JJ, Lee SC, Jeong CW, Yoon CY, Hong SK, Byun SS, Lee SE (2012) Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms: a comparison between men and women. Korean J Urol 53(5):342–348. doi:10.4111/kju.2012.53.5.342
Abarbanel J, Marcus EL (2007) Impaired detrusor contractility in community-dwelling elderly presenting with lower urinary tract symptoms. Urology 69(3):436–440. doi:10.1016/j.urology.2006.11.019
Taylor JA 3rd, Kuchel GA (2006) Detrusor underactivity: clinical features and pathogenesis of an underdiagnosed geriatric condition. J Am Geriatr Soc 54(12):1920–1932. doi:10.1111/j.1532-5415.2006.00917.x
Osman NI, Chapple CR, Abrams P, Dmochowski R, Haab F, Nitti V, Koelbl H, van Kerrebroeck P, Wein AJ (2014) Detrusor underactivity and the underactive bladder: a new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol 65(2):389–398. doi:10.1016/j.eururo.2013.10.015
Acknowledgments
Funding for this conference was made possible (in part) by 1R13AG047010 from the National Institute on Aging. The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the NIH; nor does mention by trade names, commercial practices, or organizations imply endorsement by the US Government.
Conflict of interest
Michael B Chancellor has conflicts of interest related to Allergan, Astellas, Cook, Lipella, Medtronic, Pfizer, Targacept. There are no conflicts of interest for Sara Valente, Catherine DuBeau, David Chancellor, Justin Okonski, Andrew Vereecke, Florence Doo, Michelle Lajiness, and Ananias Diokno.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valente, S., DuBeau, C., Chancellor, D. et al. Epidemiology and demographics of the underactive bladder: a cross-sectional survey. Int Urol Nephrol 46 (Suppl 1), 7–10 (2014). https://doi.org/10.1007/s11255-014-0811-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-014-0811-1