Abstract
Purpose
To assess the prevalence, awareness, and quality of life (QOL) impact of symptoms suggestive of underactive bladder (UAB) in the USA.
Methods
A thirteen-item paper survey was mailed to 25,000 individuals 60 years or older living in the USA. It aimed to collect information relating to demographics, familiarity with UAB, patient urinary symptoms, and QOL concerns.
Results
Nine hundred and seventy-seven survey participants were stratified into four groups based on the number of UAB symptoms (straining, retention, and difficulty emptying) present: zero, one, two, and three. As the number of reported UAB symptoms increased, there was an increase prevalence in nocturia, urge, and urinary frequency (p < 0.0001). Increased UAB symptoms were associated with an increased prevalence of concerns related to urgency, urge incontinence, nocturia, and overall urinary status (p < 0.0001). Urology visits were most common in individuals who reported the most UAB symptoms (p < 0.0001); however, there was no difference among groups with regard to UAB awareness. Women were less likely to report any UAB symptoms (p < 0.0001), symptoms of urge (p = 0.001), retention (p = 0.002), difficulty emptying their bladder (p < 0.0001), a history of catheter use for retention (P = 0.002), and urology visits in the past 3 years (p < 0.0001). This study is limited in its inability to differentiate UAB from disorders that may mimic UAB clinically, based on the survey questions asked.
Conclusions
Underactive bladder symptoms are common and can have a significant impact on ones QOL, although awareness is still lacking among potentially affected individuals. More must be done to allow one to better differentiate between UAB and conditions that are clinically similar.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Underactive bladder (UAB) is a poorly understood disorder due to a lack of research on this topic, a lack of consensus on its definition, and insufficient standardization of its diagnosis. There have been an ample of names used to describe UAB including detrusor underactivity (DU), urinary retention, incomplete bladder emptying, and high residual urine [1]. It is most often used synonymously with “DU”, which is defined as a contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or failure to achieve complete bladder emptying within a normal time span [2]. A working definition for UAB has been proposed by experts [4] in recent years as “a symptom complex suggestive of DU [that] is usually characterized by prolonged urination time with or without a sensation of incomplete bladder emptying, usually with hesitance, reduced sensation on filling, and a slow stream.”
Although there appears to be promise in the characterization of UAB, the prevalence of patients with this disorder is still not known. Recent studies have attempted to assess the awareness and prevalence of this disorder, and it has been shown that UAB symptoms (i.e., difficult bladder emptying) were prevalent in nearly 25 % of survey participants in metro Detroit [4]. It is difficult to ascertain what the prevalence of this disorder is in the general population, as it can present with various symptoms such as hesitancy, incomplete emptying, difficulty emptying, straining, decreased urinary stream, incontinence, and recurrent urinary tract infection (UTI) [1]. As a consequence of this disorder’s uncertainty with regard to its definition and prevalence, it is also difficult to assess the impact UAB has on those affected.
This study aims to assess the prevalence of UAB in the general population, as well as the extent UAB can have on one’s quality of life (QOL). Because lower urinary tract dysfunction is highly prevalent among the elderly, this group was targeted in this study [5].
Methods
After IRB approval, a 13-item paper survey was mailed to 25,000 individuals 60 years or older living in the USA to collect demographic data, medical history, questions regarding urinary symptoms, and familiarity with UAB, as well as questions pertaining to their QOL in relation to the urinary symptoms they experience. Residents randomly received a UAB-questionnaire (UAB-q). The mailing list was generated by an independent third party based on the study parameters. The International Continence Society (ICS) definition was used as a guideline. Participants were asked to quantify their UAB symptoms in the last week, as well as to quantify their concerns pertaining to various urinary symptoms.
Participants were grouped into four categories, based on their responses to the UAB-specific questions (Table 1). The data were analyzed with Pearson’s Chi-square tests and Fisher’s exact tests, when appropriate.
Results
In 1052 total survey responses, 586/1052 (55.7 %) were women and 466/1052 (44.3 %) were men. The mean age of survey respondents was 74.5 ± 9.2 years. Of these, 211/1002 (21.1 %) previously heard of UAB. There were 977 participants who completed the entire survey, and these individuals were subsequently grouped into various categories. 541/977 (55.4 %) were women, and 436/977 (44.6 %) were men. The mean age was 74 ± 9 years.
Four groups based on response to UAB symptoms were categorized: A: no UAB symptoms, B: one symptom, C: two symptoms, and D: three symptoms. UAB symptoms that were considered include straining, difficulty emptying, and urinary retention. Participant characteristics are shown in Table 2. The category with the largest proportion of females was A or no UAB symptoms (p < 0.0001).
As UAB symptom number increased (from 0 to 3), there was an increase in reported bladder concerns, history of catheter use for urinary retention, as well as urology visits in the past 3 years (p < 0.0001). Although increased UAB symptoms were associated with increased urology visits, there was no difference between the four groups regarding UAB awareness. Individuals with three symptoms also reported the highest frequency of multiple bladder infections in the past year and the highest prevalence of ambulation difficulty (p < 0.0001).
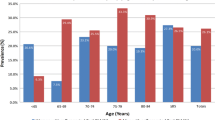
We assessed the various urinary symptoms that participants experience (Fig. 1) and showed that as UAB symptoms increased throughout the four groups, the frequency of reported nocturia (>1 episodes in the past week), sensations of urge, and episode of urge incontinence (UI) also increased (p < 0.0001).
Participants were also asked to state their level of concern regarding aspects of their urinary status (Fig. 2). Levels of concern regarding urinary urgency, UI, nocturia, and overall urinary condition increased as the prevalence of UAB symptoms increased (p < 0.0001). Concerns regarding urinary frequency were also highest in the group with three symptoms, but did not increase with increasing UAB symptoms (p < 0.0001).
Quality of life impact of urinary symptoms. As the number of UAB symptoms increased, there was an increased level of concern among participants pertaining to other urinary symptoms (urgency, urge incontinence, nocturia), as well as an increase concern about ones overall urinary status. Concerns about frequency were also highest in the group that reported the most UAB symptoms. *p < 0.0001
When looking directly at gender-associated variables (Fig. 3), males were more likely to report symptoms of urge, retention, and difficult emptying their bladders. Men were also more likely to have visited an urologist in the past 3 years and to have a history of urinary retention that required a catheter for relief. There was no evidence of a difference in UAB awareness between the genders.
Males versus females. Differences were shown between the genders with symptoms of urge (p = 0.001; OR 1.53, 95 % CI [1.19, 1.98]), retention (p = 0.002; OR 1.52, 95 % CI [1.16, 1.98]), difficulty emptying bladder (p < 0.0001; OR 2.16 95 % CI [1.63, 2.85]); history of catheter for retention (p = 0.002; OR 1.80, 95 % CI [1.23, 2.62]), and urology visits (p < 0.0001; OR 3.51, 95 % CI [2.67, 4.61])
Discussion
Underactive bladder remains an under-researched, poorly understood, and underused term due to a lack of consensus of terminology, epidemiology and standardization of diagnostic criteria. It can be a difficult entity to identify, as its symptoms may overlap with other urinary conditions, be associated with medications or comorbidities, or result as a consequence of previous pelvic surgeries [6]. Suggestive symptoms of UAB include hesitancy, incomplete emptying, difficulty emptying, and straining, but these patients can also present with urgency, frequency, nocturia, incontinence, and recurrent UTI [1]. Because these symptoms can be present in patients with various urinary conditions, identifying patients with UAB can be difficult.
Urinary tract disorders are common in the elderly, as these individuals are more likely to suffer with lower urinary tract dysfunction, overactive bladder (OAB), urinary incontinence, as well as UAB [7, 8]. Because our population is aging, with a projected 72 million, or 20 %, individuals expected to be 65 years or older by 2030, clinicians can expect to encounter a high volume of patients with urinary tract issues [9]. This is likely to have an economic burden on these patients, as well as society, as urinary tract dysfunction has already been shown to be costly. One study found that the overall cost of OAB with UI was 65.9 billion dollars in 2007 [10]. This does not include other urinary conditions and complications that these individuals may be at risk for, such as UTI, which can be very costly [11]. Because of this, it is extremely important to identify and manage the various urinary issues that these patients may present with.
Because there is not a current consensus on diagnosing UAB, it is difficult to know how many people are truly affected with this disorder. We attempted to identify patients with UAB based on positive responses to typical UAB symptoms (difficulty emptying, retention, straining). Our results indicate that positive responses to all three questions are associated with increased bladder concerns, a higher prevalence of difficult ambulation, and a higher prevalence of reported bladder infections in the previous year. We were able to show that as the number of UAB symptoms increased, the prevalence of symptoms of nocturia, urge, and frequency also increased. This supports previous studies that report an association and/or overlap of UAB with other urinary disorders [1, 4, 6].
Reported urology visits also increased with increased UAB symptoms, but interestingly there was no difference in UAB awareness among these individuals, suggesting that information regarding this disorder is not being relayed to patients who are potentially affected. Decreased patient education about this disorder may be associated with the lack of consensus among clinicians regarding various aspects of UAB as a diagnosis. Despite this lack of awareness, our figure of 21 % is higher than a previous metro-Detroit-based study, which showed that only 11 % of participants heard of UAB [4].
When looking at gender differences, we were able to show that women were more likely to report no UAB symptoms and a higher percentage of men reported two or more UAB symptoms. We compared men and women and noted that men were more likely to report symptoms of difficult bladder emptying and retention than women, and more likely to have a history of catheter requirement for the relief of retention. This suggests that men may be more commonly affected by UAB, as this is supported by some studies [5, 12, 13]. Conversely, our previous study showed no association between UAB and gender, when using “difficulty bladder emptying” as a proxy for UAB [4].
One barrier with assessing the prevalence among genders is that men more commonly present with bladder outlet obstruction (BOO), most commonly to due benign prostatic hyperplasia (BPH), and this can be clinically indistinguishable from UAB [3]. Because of the potential symptom overlap between UAB, BOO, and other disorders, it was proposed that UAB be approached as a symptom complex to aid clinicians in screening patients [3].
One recent study was able to confirm the presence of the classic symptoms of UAB in DU-confirmed patients, as well as identify features that differentiated DU from BOO [14]. It found that when comparing normal pressure flow studies (PFS) to DU patients, DU patients were significantly more likely to have decreased urinary stream, incomplete bladder emptying, palpable bladder, hesitancy, and decreased sensation to void. Men with DU were more likely to experience straining, versus BOO and normal PFS patients, and both men and women with DU more commonly experienced enuresis versus BOO [14]. This provides useful information for urologists and other clinicians once UAB complex is suspected, either via a survey or clinical presentation, as it allows one to better workup and accurately diagnose DU in these patients.
Additionally, in our study, increased UAB symptoms were also associated with increasing subjective concerns about topics related to urgency, UI, frequency, nocturia, and overall urinary status. This also suggests that an increase in urinary symptoms that are commonly associated with UAB may be associated with a decrease in ones outlook on their quality of life, which has been shown in previous studies [15, 16].
Limitations to this study include that this was a self-administered survey, which required adequate patient literacy. This may contribute to the low response rate, which introduces a possible non-response bias into this study. Another limitation is that although we were able to quantify UAB symptoms in our population, we were not able to identify patients who are truly diagnosed with UAB. This disorder is still not clearly defined by clinicians and although certain responses to the given questions may imply UAB, there is no definitive way to know that a patient has UAB, based solely on their answers. UAB can present similarly to various issues that result in BOO (i.e., BPH, bladder neck contracture, urethral stricture, pelvic surgeries affecting the outflow tract). Additionally, one should be aware that poorly controlled diabetes can result in diabetic cystopathy, which can also present similar to UAB [1]. Thus, it would be ideal to identify these issues of complicated urinary tracts and poor glycemic control in our population, as we would then be able to stratify individuals reporting UAB symptoms as (1) individuals with an underlying etiology causing UAB symptoms and (2) individuals with likely true UAB. Because our survey did not ask about any of these issues and these participants cannot be identified due to the nature of the study’s random, de-identified design, we were not able to ask these follow-up questions after surveys were collected. In the future, it would also be interesting to administer both a validated BPH questionnaire (i.e., the International Prostate Symptom Score or American Urological Association Symptom Index) and our survey to a population to observe how patients suspected to have true UAB score on those evaluations.
Conclusions
Underactive bladder symptoms are common and can have a significant impact on ones QOL, but awareness of the disorder is lacking among individuals who are potentially affected. Increased UAB symptoms were more common in men. UAB can be difficult to identify because symptoms may overlap with other urinary conditions. More must be done to increase patient and physician awareness of UAB, as well as to better understand its prevalence, consequences on one’s QOL, diagnosis, and management.
Abbreviations
- BOO:
-
Bladder outlet obstruction
- DU:
-
Detrusor underactivity
- ICS:
-
International Continence Society
- LUTS:
-
Lower urinary tract symptoms
- UAB:
-
Underactive bladder
- UAB-q:
-
Underactive bladder questionnaire
- UTI:
-
Urinary tract infection
- QOL:
-
Quality of life
- OAB:
-
Overactive bladder
- PFS:
-
Pressure flow studies
- BPH:
-
Benign prostatic hyperplasia
- UI:
-
Urge incontinence
References
Miyazato M, Yoshimura N, Chancellor MB (2013) The other bladder syndrome: underactive bladder. Rev Urol 15(1):11–22. doi:10.3909/riu0558
Van Koeveringe GA, Vahabi B, Andersson KE et al (2011) Detrusor underactivity: a plea for new approaches to a common bladder dysfunction. Neurourol Urodyn 30:723–728. doi:10.1002/nau.21097
Chapple CR, Osman NI, Birder L et al (2015) The underactive baldder: a new clinical concept? Eur Urol 68(3):351–353. doi:10.1016/j.eururo.2015.02.030
Valente S, DuBeau C, Chancellor D et al (2014) Epidemiology and demographics of the underactive bladder: a cross-sectional survey. Int Urol Nephrol 46(1):S7–S10. doi:10.1007/s11255-014-0811-1
Jeuong SJ, Kim JH, Lee JY et al (2012) Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms: a comparison between men and women. Korean J Urol 53(5):342–348. doi:10.4111/kju.2012.53.5.342
Hoag N, Gani J (2015) Underactive bladder: clinical features, urodynamic parameters and treatment. Int Neurourol J 19:185–189. doi:10.5213/inj.2015.19.3.185
Chuang YC, Plata M, Lamb LE, Chancellor MB (2015) Underactive bladder in older adults. Clin Geriatr Med 31(4):523–533. doi:10.1016/j.cger.2015.06.002
Dubeau CE (2006) The aging lower urinary tract. J Urol 175(3):S11–S15. doi:10.1016/S0022-5347(05)00311-3
Ortman JM, Velkoff VA, Hogan H (2016) An aging nation: the older population in the United States. United States Census Bureau Website. http://www.census.gov/library/publications/2014/demo/p25-1140.html. Accessed 14 May 2016
Coyne KS, Wein A, Nicholson S et al (2014) Economic burden of urgency urinary incontinence in the United States: a systematic review. J Manag Care Pharm 20(2):130–140. doi:10.18553/jmcp.2014.20.2.130
Foxman B, Barlow R, D’Arcy H et al (2000) Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol 10(8):509–515. doi:10.1016/S1047-2797(00)00072-7
Abarbanel J, Marcus EL (2007) Impaired detrusor contractility in community-dwelling elderly presenting with lower urinary tract symptoms. Urology 69(3):436–440. doi:10.1016/j.urology.2006.11.019
Kadow BT, Tyagi P, Chermansky CJ (2015) Neurogenic causes of detrusor underactivity. Curr Bladder Dysfunct Rep 10(4):325–331. doi:10.1007/s11884-015-0331-6
Gammie A, Kaper M, Dorrepaal C et al (2016) Signs and symptoms of detrusor underactivity: an analysis of clinical presentation and urodynamic tests from a large group of patients undergoing pressure flow studies. Eur Urol 69(2):361–369. doi:10.1016/j.eururo.2015.08.014
Liuz Z, Uchiyama T, Sakakibara R et al (2015) Underactive and overactive bladders are related to motor function and quality of life in Parkinson’s disease. Int Urol Nephrol 47(5):751–757. doi:10.1007/s11255-015-0951-y
Griebling TL, DuBeau CE, Kuchel G et al (2014) Defining and advancing education and conservative therapies of underactive bladder. Int Urol Nephrol 46:S29–S34. doi:10.1007/s11255-014-0799-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This project was supported by the Aikens Center for Neurourology Research at Beaumont Health.
Research involving human participants
This study was IRB approved at Beaumont Health System.
Rights and permissions
About this article
Cite this article
Faraj, K., Doo, F., Boura, J. et al. A cross-sectional study in the USA of the epidemiology and quality of life of underactive bladder symptoms. Int Urol Nephrol 48, 1797–1802 (2016). https://doi.org/10.1007/s11255-016-1382-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1382-0