Abstract
Purpose
To prospectively investigate diagnostic value of routine frozen section analysis (FSA) of urethral margin for male patients undergoing cystectomy for bladder cancer.
Materials and methods
One hundred consecutive male patients were subjected to radical cystectomy for bladder cancer with routine FSA obtained from distal prostatic urethral margin. Definitive pathological condition of the specimens was reviewed to diagnose urethral ± prostatic malignant involvement. The diagnostic value of FSA was identified and compared with different clinical and pathological predictors. Patients with false-negative results were followed for 5 years.
Results
Six patients showed evidence of malignancy by FSA of the prostatic urethral margin (one patient was false positive), and all were managed by urethrectomy. Prostatic ± urethral involvement was diagnosed in 15 patients by definitive histopathology (15 %). Sensitivity and specificity of urethral margin frozen section were 33.3 and 98.8 %, respectively, with overall accuracy of 89 % while positive and negative predictive values were 83.3 and 89.4 %, respectively. There was no significant correlation identified between tumor site or morphology, clinical staging, clinically suspicious prostate, cystoscopic involvement of bladder neck, tumor grade, and associated carcinoma in situ or nodal involvement with prostatic malignant involvement. Positive intraoperative FSA was the only predictor significantly associated with malignant urothelial involvement of the prostate. None of the 10 patients with false-negative results developed late urethral recurrence at 5 years.
Conclusion
Intraoperative urethral frozen section shows high predictive diagnostic value of malignant prostatic involvement. Nevertheless, its impact in preventing late urethral recurrence is doubtful.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical cystectomy and pelvic lymph node dissection are considered the standard treatment for muscle invasive bladder cancer. Orthotopic urinary diversion has gained increasing popularity over the past two decades owing to its long-term reliability, oncological safety, and potential improvement in quality of life compared with non-continent diversions [1–3]. Nevertheless, orthotopic substitutes could not be provided for all patients as it is essential to preserve sufficient urethral length free of tumors to ensure a successful safe urethro–ileal anastomosis. Therefore, high-risk patients with tumor located at the bladder neck, multifocal disease, CIS, or prostatic stromal invasion were traditionally deprived from orthotopic diversion [1, 3–7].
It has been estimated that the incidence of prostatic urethral involvement in patients undergoing radical cystectomy is in the order of 35–40 %. Furthermore, local pelvic recurrences have been reported in 10–15 % of radical cystectomy cohorts with 0.5–5 % of these recurrences occurring in the urethra [4–7]. Different approaches were suggested to investigate the prostatic malignant involvement in bladder cancer patients before deciding the best suitable form of urinary diversion [8–12]. The value of intraoperative frozen section analysis (FSA) of the distal urethral margin in these patients and its routine use in patients undergoing radical cystectomy has been questioned in a retrospective way [10, 12]. The aim of this study was to prospectively assess the value of pathological detection of urethral malignant involvement with FSA during cystectomy in comparison with other different clinical and pathological parameters and judge its long-term beneficial impact.
Materials and methods
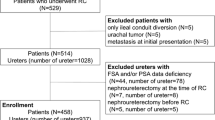
Between November 2004 and September 2005, 100 consecutive male patients with mean age of 59.5 ± 7.5 years underwent radical cystectomy and urinary diversion. All the patients had transitional cell carcinoma with tumor invasion into the muscularis propria, or Ta, T1, or carcinoma in situ refractory to transurethral resection with intravesical adjuvant therapy. Patients with non-transitional cell carcinoma were excluded from the study. No patient had distant metastatic disease at cystectomy. Clinical staging was based on a bimanual examination with the patient under anesthesia, endoscopic assessment and biopsy, and MRI. All patients had a standard radical cystectomy with bilateral iliac lymphadenectomy. Routine intraoperative frozen section biopsies were obtained from urethral margin of the operative specimen in all patients; patients with intraoperative positive margins were subjected to urethrectomy and excluded from orthotopic diversion. A detailed informed consent was obtained from all patients after approval from the local ethics committee.
The TNM classification of the International Union against Cancer was used for pathological staging of the tumors [13]. The pathological diagnosis followed the WHO/ISUP (World Health Organization/International Society of Urologic Pathology) consensus classification of urothelial neoplasms [14]. Positive malignancy in frozen as well as in definitive specimens was diagnosed among patients harboring CIS (high-grade intraurothelial neoplasia), papillary carcinoma (low or high grade), and invasive neoplasms (with lamina propria or muscularis propria invasion). Those with hyperplasia, reactive atypia, or dysplasia (low-grade intraurothelial neoplasia) as well as those with incidentally discovered prostatic adenocarcinoma were considered negative for malignancy. The excised prostate in the cystectomy specimen was used for definitive histopathologic examination that comprised a 3-mm step-sectioning. Definitive pathological results of cystoprostatectomy specimens were reviewed to diagnose urethral and/or prostatic malignant involvement. The results of paraffin-embedded and frozen section analyses were compared. The FSA results were considered as the test while the results of prostatic urothelial malignancy obtained from step-sectioning in definitive histopathology were considered as the reference standard. The sensitivity was defined as the number of true-positive test results divided by the overall positive cases in the reference standard, and specificity as the number of true-negative test results divided by the overall negative cases from the reference standard. The accuracy was defined as true-positive and true-negative test results divided by the total number of specimens examined. The positive predictive value (PPV) was defined as the number of true-positive test results divided by the overall test-positive results, and the negative PV (NPV) as the number of true-negative test results divided by the overall test-negative results. The patients’ characteristics and incidence of urethral malignant involvement were recorded in an electronic database. The incidence of true urethral involvement (by the analysis of cystoprostatectomy specimen) was compared with different clinical and pathological variables. The Pearson Chi-square test was used, with P < 0.05 considered to indicate significance. Patients with false-negative results were closely followed for 5 years to detect distant, local pelvic or urethral recurrence.
Results
Among the 100 patients who had radical cystectomy, six patients had evidence of urothelial malignancy by FSA. There were 2 specimens showing CIS and 4 with invasive disease infiltrating the lamina propria. All these patients were managed by complementary urethrectomy and received cutaneous diversion.
By reviewing the definitive histopathology of the frozen specimens, there was one specimen with false-positive result while the results of the remaining 5 specimens were confirmed. On the other hand, step-sectioning of the prostate in the removed specimens revealed extra 10 urothelial malignant prostatic lesions in extra 10 patients (6 CIS and 4 with invasive disease infiltrating the lamina propria or the prostate). Therefore, the true incidence of urethral (±prostatic) urothelial malignant involvement included 15 patients (15 %). Table 1 shows the true- and false-positive and true- and false-negative results of FSA as controlled by final pathological results of specimen. The specificity of the FSA for detecting urothelial malignancy was 98.8 % while the sensitivity was 33.3 %, with an overall accuracy of 89 %. The positive predictive value was calculated to be 83.3 % while the negative predictive value was 89.4 %.
Table 2 shows that there was no significant correlation identified between tumor site or morphology, clinical staging, clinically suspicious prostate, cystoscopic involvement of bladder neck, tumor grade, and associated carcinoma in situ or nodal involvement with prostatic malignant involvement. Positive intraoperative frozen section was the only predictor significantly associated with malignant urothelial prostatic involvement. (P = <0.01). The 10 patients with false-negative results were followed up for at least 5 years to detect distant, local pelvic or distant metastasis. Four patients developed tumor recurrence within 2 years, 3 with distant bony metastasis, and 1 with local pelvic recurrence. None of these patients had an associated urethral recurrence. Five patients were free of tumor recurrence at 5 years. The last patient lost follow-up.
Discussion
The incidence of urethral recurrence of transitional cell carcinoma following radical cystectomy has been estimated to be as high as 0.5–5 % [4–7]. Appropriate patient selection for urethral preservation has gained significant attention especially in patients undergoing orthotopic urinary reconstruction as careful patient selection has at least contributed to a low rate of recurrence following orthotopic urinary creation [5, 6].
It has been documented that prostatic urethral involvement in cases of transitional cell carcinoma of the bladder is the most important risk factor for urethral recurrence [5, 15, 16]. The importance of determining disease in the prostatic urethra is more critical when one considers that this presence is almost a prerequisite for possible subsequent development of malignancy more distally in the urethra. In fact, it is uncommon to find disease in the distal urethra without some disease involving the prostatic urethra [17]. Nixon et al. [18] demonstrated that the presence of CIS and/or tumor multifocality was valuable prognostic indicators of prostatic urethral involvement. In their absence, however, prostatic urethral involvement was rare. Prostatic urethral involvement was found in 30 (15.6 %) of 192 patients. In a multiple-variable logistic regression model, the odds of prostatic urethral involvement were 12 and 15 times greater when CIS and tumor multifocality were present, respectively. Interestingly, these documented risk factors for prostatic involvement were not sustained as risk factors for urethral recurrence as reported by 2 independent groups of investigators [5–19]. Our data confirmed in a prospective way that clinical risk factors as papillary tumors, multicentricity, and tumors close to bladder neck as well as pathological factors as high-grade tumors and CIS were not sufficient in predicting prostatic involvement. Therefore, identification of actual prostatic involvement in cases of bladder cancer has therefore been considered critical for decision making regarding the mode of urinary diversion.
Various methods have been adopted for actual detection of prostatic urethral malignant involvement prior to urinary diversion. Two decades ago, Wood et al. [8] investigated prostate needle biopsy and fine-needle prostatic aspiration in bladder cancer patients to preoperatively judge prostatic involvement and concluded low detection rates of these modalities. They advocated transurethral biopsy of the prostatic urethra as an important diagnostic tool in deciding the type of urinary diversion with accuracy detection rate of 90 %. In two different experiences, the sensitivity of transurethral biopsy of the prostatic urethra ranged between 52 % [9] and 82 % [11]. Nevertheless, further experiences abandoned this approach. Donat et al. [9] denied the ability of transurethral biopsy to accurately predict prostatic malignant involvement. Furthermore, Lebert et al. [10] found that preoperative transurethral biopsy may indeed overestimate patients with disease. The urethra was preserved in 8.5 % of patients, despite a positive transurethral biopsy of the prostatic urethra prior to cystectomy. None of these patients showed urethral recurrence at a 10-year minimum follow-up. Extirpating the area of tumor with the biopsy procedure could be considered as an explanation for this overestimation. Others confirmed the limited usefulness of routine preoperative transurethral prostate biopsies in patients with bladder cancer [11, 12]. All these described experiences included multiple transurethral lateromontanal loop biopsies rather than single cold-cup biopsy.
Currently, FSA of prostatic urethral margin at the time of cystectomy is accepted as the modality of choice in judging the malignant prostatic involvement. In a recent study, Kassouf et al. [12] showed that optimal negative predictive value (100 %) is obtained with FSA. Up to our knowledge, the current contribution is the first study documenting the high predictive diagnostic value of intraoperative urethral FSA in detecting prostatic involvement in a prospective way. Furthermore, it shows that positive intraoperative frozen section was the only predictor significantly associated with prostatic urethral malignant involvement compared with other clinical or pathological parameters.
Lebert et al. [10] reviewed more than 100 patients and 10-year minimum follow-up, and no urethral recurrence was observed in these patients with negative frozen cut section. We looked for those with negative FSA and positive prostatic involvement. Surprisingly, we failed to identify a real advantage of this prediction upon long-term protection against urethral recurrence. None of the 10 patients with malignant urothelial involvement of the prostate who were not detected by FSA and kept their urethra connected to the orthotopic substitute developed urethral recurrence up to 5 years of follow-up. This finding raises the question of the real value of detecting subclinical prostatic involvement and gives the space to exclude only those with gross prostatic involvement from orthotopic substitution. Main limitation of the study includes weak power in the study to detect an infrequent event, that is, urethral recurrence, as well as limited power to correlate tumor characteristics to the presence of urothelial carcinoma of the prostate.
Conclusion
Intraoperative urethral frozen section shows high predictive diagnostic value of malignant prostatic involvement in male patients undergoing radical cystectomy for bladder cancer. This predictive value is superior to other clinical, cystoscopic, or pathological parameters suggestive of prostatic involvement. Nevertheless, its impact in preventing late urethral recurrence is doubtful.
References
Yossepowitch O, Dalbagni G, Golijanin D, Donat S, Bochner B, Herr H, Fair W, Russo P (2003) Orthotopic urinary diversion after cystectomy for bladder cancer: implications for cancer control and patterns of disease recurrence. J Urol 169:177–181
Gore J, Yu H, Setodji C, Hanley J, Litwin M, Urologic Diseases in America Project (2010) Urinary diversion and morbidity after radical cystectomy for bladder cancer. Cancer 116:331–339
Lee C (2009) Quality of life following incontinent cutaneous and orthotopic urinary diversions. Curr Treat Options Oncol 10:275–286
Varol C, Thalmann G, Burkhard F, Studer U (2004) Treatment of urethral recurrence following radical cystectomy and ileal bladder substitution. J Urol 172:937–942
Stein J, Clark P, Miranda G, Cai J, Groshen S, Skinner D (2005) Urethral tumor recurrence following cystectomy and urinary diversion: clinical and pathological characteristics in 768 male patients. J Urol 173:1163–1168
Hassan J, Cookson M, Smith J Jr, Chang S (2004) Urethral recurrence in patients following orthotopic urinary diversion. J Urol 172:1338–1341
Ghoneim M, Abdel-Latif M, el-Mekresh M, Abol-Enein H, Mosbah A, Ashamallah A, el-Baz M (2008) Radical cystectomy for carcinoma of the bladder: 2,720 consecutive cases 5 years later. J Urol 180:121–127
Wood D Jr, Montie J, Pontes J, Levin H (1989) Identification of transitional cell carcinoma of the prostate in bladder cancer patients: a prospective study. J Urol 142:83–85
Donat S, Wei D, McGuire M, Herr H (2001) The efficacy of transurethral biopsy for predicting the long-term clinical impact of prostatic invasive bladder cancer. J Urol 165:1580–1584
Lebret T, Herve J, Barre P, Gaudez F, Lugagne P, Barbagelatta M, Botto H (1998) Urethral recurrence of transitional cell carcinoma of the bladder. Predictive value of preoperative latero-montanal biopsies and urethral frozen sections during prostatocystectomy. Eur Urol 33:170–174
Bulbul M, Wazzan W, Nasr R, Hemady K (2001) The value of cystoscopy, prostate biopsy and frozen-section urethral biopsy prior to orthotopic neobladder substitution. Can J Urol 8:1290–1292
Kassouf W, Spiess P, Brown G, Liu P, Grossman H, Dinney C, Kamat A (2008) Prostatic urethral biopsy has limited usefulness in counseling patients regarding final urethral margin status during orthotopic neobladder reconstruction. J Urol 180:164–167
Sobin LH, Gospodariwicz M, Wittekind C (eds) (2009) TNM classification of malignant tumors, UICC International Union Against Cancer, 7th edn. Wiley, London, pp 262–265
Epstein J, Amin M, Reuter V, Mostofi F, Bladder Consensus Conference Committee (1998) The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Am J Surg Pathol 22:1435–1448
Hardeman S, Soloway M (1990) Urethral recurrence following radical cystectomy. J Urol 144:666–669
Sarosdy M (1992) Management of the male urethra after cystectomy for bladder cancer. Urol Clin North Am 19:391–396
Tobisu K, Kanai Y, Sakamoto M, Fujimoto H, Doi N, Horie S, Kakizoe T (1997) Involvement of the anterior urethra in male patients with transitional cell-carcinoma of the bladder undergoing radical cystectomy with simultaneous urethrectomy. Jpn J Clin Oncol 27:406–409
Nixon R, Chang S, Lafleur B, Smith J, Cookson M (2002) Carcinoma in situ and tumor multifocality predict the risk of prostatic urethral involvement at radical cystectomy in men with transitional cell carcinoma of the bladder. J Urol 167:502–505
Tobisu K, Tanaka Y, Mizutani T, Kakizoe T (1991) Transitional cell carcinoma of the urethra in men following cystectomy for bladder cáncer: multivariate analysis for risk factors. J Urol 146:1551–1554
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Osman, Y., Mansour, A., El-Tabey, N. et al. Value of routine frozen section analysis of urethral margin in male patients undergoing radical cystectomy in predicting prostatic involvement. Int Urol Nephrol 44, 1721–1725 (2012). https://doi.org/10.1007/s11255-012-0276-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0276-z