Abstract
The objectives of this study were to determine the presence and prevalence of non-O157 shiga toxin-producing Escherichia coli (STEC) isolates from faeces of healthy fat-tailed sheep and detection of phylogenetic background and antibiotic resistance profile of isolates. One hundred ninety-two E. coli isolates were recovered from obtained rectal swabs and were confirmed by biochemical tests. Antibiotic resistance profiles of isolates were detected and phylogenetic background of isolates was determined according to the presence of the chuA, yjaA and TspE4.C2 genetic markers. The isolates were examined to determine stx 1 , stx 2 and eae genes. Non-O157 STEC isolates were identified by using O157 specific antiserum. Forty-three isolates (22.40 %) were positive for one of the stx 1 , stx 2 and eae genes, whereas 10.42 % were positive for stx 1 , 19.38 % for eae and 2.60 % for stx 2 gene. None of the positive isolates belonged to O157 serogroup. Twenty isolates possessed stx 1 were distributed in A (six isolates), B1 (13) and D (one) phylogroups, whereas stx 2 positive isolates fell into A (three isolates) and B1 (two) phylogenetic groups. Eighteen isolates contained eae gene belonged to A (five isolates), B1 (seven) and D (six) phylogroups. The maximum and minimum resistance rates were recorded against to penicillin and co-trimoxazole respectively. The positive isolates for stx 1 , stx 2 and eae genes showed several antibiotic resistance patterns, whereas belonged to A, B1 and D phylogroups. In conclusion, faeces of healthy sheep could be considered as the important sources of non-O157 STEC and also multidrug-resistant E. coli isolates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shiga toxin-producing Escherichia coli (STEC) or verotoxin-producing E. coli (VTEC) and particularly E. coli O157:H7, have emerged as the important zoonotic food-borne pathogens and confirming the risk to public health (Fernández et al. 2012; Paris et al. 2010). The most common STEC serotype associated with human disease is O157, but there is a growing recognition of over 100 non-O157 serotypes that also may result in human illness. Some of these non-O157 STEC strains cause outbreaks of diarrhoea and severe disease such as haemolytic uremic syndrome (HUS) and haemorrhagic colitis (Coombes et al. 2011; Nguyen and Sperandio 2012). Sources of human infection with STEC strains and outbreaks occur through ingestion of contaminated food or water including: undercooked meat, unpasteurised milk and dairy products, vegetables or water and contact with animal carriers or the environment (Pacheco and Sperandio 2012; Sanchez et al. 2010). Apparently, healthy cattle have been reported to be a major reservoir of STEC (VTEC); however, several studies suggest that other wild and domesticated ruminants may be important in contributing to human clinical cases (Ferens and Hovde 2011). The presence of E. coli O157:H7 has been reported in sheep and lamb products and/or faecal samples internationally (Kumar et al. 2012; Momtaz et al. 2012). On the other hand, cattle and sheep have been shown to carry non-O157 STEC strains, which mostly belong to O26, O111, O103, O121, O45 and O145 serogroups (Bai et al. 2012; Evans et al. 2008).
Two main virulence factors of STEC are Shiga toxins (Stx) 1 and 2 encoded by stx 1 and stx 2 genes respectively, which inhibit protein synthesis in mammalian cells. Several additional virulence factors, among many others, are a plasmid-encoded enterohemolysin and, in strains lacking intimin, an autoagglutinating adhesin (Saa) which could be involved in adhesion (Alonso et al. 2012; Andrade et al. 2012). The eae virulence gene, which encodes an outer membrane protein, intimin involved in the intimate attachment of the E. coli O157:H7 to the intestinal epithelium and induces attaching and effacing (AE) lesions (Bandyopadhyay et al. 2011).
The emergence of antibiotic resistance in both commensal and pathogenic strains has become an important public health issue (Saei et al. 2010). Development and persistence of antibiotic resistance in commensal and non-pathogenic bacteria is one of worldwide concerns, because they are thought to act as a reservoir of resistance genes capable of transferring genes to foodborne and other zoonotic pathogens (Zhang et al. 2009).
According to phylogenetic studies, E. coli strains can be assigned to one of the four main phylogenetic groups, A, B1, B2 and D, which can be divided into seven subgroups (Carlos et al. 2010). A study on molecular characterization of STEC isolates from ruminant and donkey raw milk samples and traditional dairy products in Iran showed that samples from sheep were positive for O157 and non O157 STEC strains (Momtaz et al. 2012). According to FAOSTAT (2010) report on livestock numbers of Iran, sheep are by far the most numerous farm animal, followed by goats, cattle, donkeys, horses, water buffalo and mules. The objectives of this study were (1) to determine the presence and prevalence of O157 and non-O157 STEC isolates from faeces of healthy sheep in southeastern of Iran; (2) to investigate the phylogenetic distribution and antibiotic resistance profile of the shiga toxin and intimin genes possessed isolates.
Materials and methods
Bacterial isolates
Rectal swab samples were obtained from 192 apparently healthy fat-tailed sheep between June 2010 and February 2011. The sampled animals were originated from eight flocks in Kerman province (southeastern), Iran. The flocks were in traditional husbandry conditions and there was not any history of previous antibiotic therapy. Each of the sampled flocks included nearly 80–120 sheep, which 20–25 sheep were chosen for sampling from each flock. One hundred and sixty-eight of the sampled sheep were 2–3 years old and 24 animals were 4 years old. Among the 192 sampled sheep, 153 were female and 39 were male. Swab samples were streaked onto Mac Conkey agar (Biolife Laboratories, Milan, Italy) and the plates were incubated at 37 °C for 24 h. After overnight incubation, suggestive of E. coli colonies were further streaked onto eosin methylene blue and incubated overnight at 37 °C again. Green metallic sheen colonies indicative of E. coli were subjected to biochemical tests, which included indole, methyl red, Voges–Proskauer and Simmons citrate tests for E. coli identification. The confirmed E. coli isolates were stored in Luria-Bertani broth (Invitrogen, Paisley, Scotland) with 30 % sterile glycerol at −80 °C. From each sample, one confirmed isolate were chosen for serology and antibiotic susceptibility tests and PCR assays.
Reference strains of Sakaï (eae+, stx 1 + and stx 2 +) and ECOR62 (chuA+, yjaA+ and TspE4 C2+) were used as positive controls. Non-pathogenic E. coli strain MG1655 was used as a negative control for target genes.
Antimicrobial susceptibility test
Antibiotic resistance profile of isolates against eight selected antibacterial agents was determined by disc diffusion method according to Clinical and Laboratory Standards Institute’s guidelines (CLSI 2004). The following antimicrobial discs (Padtan-Teb, Tehran, Iran) were used in disc diffusion assay: co-trimoxazole (SXT; 25 μg), cephalexin (CN; 30 μg), ciprofloxacin (CP; 5 μg), enrofloxacin (NFX; 5 μg), kanamycin (K; 30 μg), oxytetracycline (T; 30 μg), penicillin (P; 10 μg) and streptomycin (S; 10 μg).
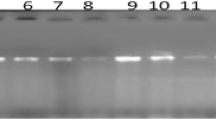
PCR assays
Freshly grown over night cultures of E. coli isolates and reference strains were used for DNA extraction by boiling. Two multiplex PCR reactions were used to screen each E. coli isolate for the presence of stx 1 , stx 2 , eae, chuA, yjaA and TspE4 C2 genes. Specific primers (TAG Copenhagen, Denmark) used for amplification of the genes are presented in Table 1. DNA extracts of isolates were tested by PCR assay for the presence of the stx 1 , stx 2 and eae genes as described by China et al. (1996). According to the presence and/or absence of the three genetic markers (chuA, yjaA and TspE4.C2) four main phylogenetic groups (A, B1, B2 and D) and seven phylogenetic subgroups (A0, A1, B1, B22, B23, D1 and D2) were determined (Clermont et al. 2000; Gordon et al. 2008).
O157 serogroup determination
O serogroup of stx 1 , stx 2 and eae-positive E. coli isolates were examined for the presence and/or absence of O157 serogroup by using of specific O157 antiserum according to the manufacturer’s recommendations. (Mast Diagnostics, Mast Group Ltd., Merseyside, England).
Results
In bacteriological examinations, 192 E. coli were isolated from same number of recta swab samples. Analysis of PCR results for determination of phylogenetic groups showed that the E. coli isolates belonged to three main groups A (42.71 %), B1 (48.44 %) and D (8.85 %). None of the isolates belonged to B2 group or its subgroups. Phylogenetic subgroups classification revealed that 93 isolates fell in to B1 group, whereas 99 isolates (51.56 %) fell into four phylogenetic subgroups: 34 isolates (17.71 %) into A0, 48 isolates (25.00 %) into A1, 12 isolates (6.25 %) into D1 and 5 isolates (2.60 %) into D2 (Table 2).
Multiplex PCR tests results showed that 43 isolates (22.40 %) were positive for one of the stx 1 , stx 2 and eae genes. According to the results all of the positive isolates had only one of the stx 1 , stx 2 and eae genes and there is not any combination of the examined genes in the positive isolates. Out of positive E. coli isolates, 20 (10.42 %) were positive for stx 1 , 18 (9.38 %) for eae and 5 isolates (2.60 %) for stx 2 gene.
According to serological tests none of the Stx- and intimin-positive isolates belonged to O157 serogroup. Twenty isolates possessed stx 1 were distributed in A (six isolates), B1 (13 isolates) and D (one isolate) phylogroups, whereas belonged to phylogenetic subgroups A0, A1, B1 and D1 (Table 2). The stx 2 -positive isolates fell into A (three isolates) and B1 (two isolates) phylogenetic groups. Eighteen isolates contained eae gene belonged to A (five isolates), B1 (seven isolates) and D (six isolates) phylogroups, which fell into A1, B1, D1 and D2 phylogenetic subgroups (Table 2).
Antibiogram of isolates against eight antibiotics showed that all of the 192 isolates were resistant against two or more examined antibacterial agents. The most prevalent resistance were recorded against to penicillin (98.44 %), cephalexin (94.79 %) and oxytetracycline (91.15 %). The minimum resistance rates were against co-trimoxazole (51.04 %) and ciprofloxacin (61.98 %), respectively (Table 3). The resistant isolates were distributed in all of the detected phylogenetic groups and subgroups, whereas their prevalence in each phylogroup differed in relation to tested antibiotics (Table 3).
Results of antibiotic susceptibility tests showed that 192 E. coli isolates could be classified in 16 different groups according to antibiotic resistance patterns. Fifty-five isolates (28.65 %) were resistant to all of the tested antibiotic, which were the most prevalent antibiotic resistance pattern followed by CN, K, NFX, P, S, T and CN, CP, K, NFX, P, S, T patterns were found in 14.58 and 14.06 % of isolates, respectively. Prevalence of 16 detected antibiotic resistance patterns in each phylogenetic group and subgroups are presented in Table 4.
The 43 positive isolates for one of the stx 1 , stx 2 and eae genes showed several antibiotic resistance patterns which were distributed in three phylogenetic groups A, B1 and D. Distribution of positive E. coli isolates in phylogenetic groups according to multi-drug resistance patterns are presented in Table 5.
Discussion
E. coli O157 STEC strains known to cause sporadic cases and outbreaks of potentially life-threatening illness in human. Non-O157 STEC isolates are also associated with HUS, whereas retrospective reports have estimated that 37–50 % of STEC infections per year are caused by non-O157 STEC organisms (Schaffzin et al. 2012). In general, human infections with STEC strains occurs after consumption of contaminated food or contact with an infected animal or human, therefore identification of the sources of infection is an important step towards decreasing the prevalence of this pathogen and thus decreasing the risk of infection of humans (Ayala et al. 2010; Pedersen et al. 2006). Cattle and sheep are thought to be the major reservoir of STEC and often carry STEC in their intestinal flora and serve as source of food contamination (Martin and Beutin 2011). Although there are several reports of isolation and characterization of STEC from cattle, there is limited information about the prevalence of STEC in small ruminants (Bhat et al. 2008; Coombes et al. 2011). In the present study, 25 isolates (13.02 %) were positive for Stx1 (20 isolates) and Stx2 (five isolates) coding genes, which do not belonged to O157 serogroup. Therefore, these isolates were considered as non-O157 STEC isolates. In Spain, STEC O157:H7 strains were isolated from one percent of animals in six flocks, whereas non-O157 STEC strains were isolated from 35 % of lambs in 33 flocks (Rey et al. 2003). Another study on E. coli isolates from healthy cattle, sheep and swine herds in northern Spain revealed that 8.7 and 50.8 % of ovine isolates were positive for O157:H7 and non-O157 STEC serotypes, respectively (Oporto et al. 2008). Blanco et al. (2003) have isolated STEC O157:H7 strains from 0.4 % faecal swabs of healthy lambs in 93 flocks and non-O157 STEC strains were isolated from 36 % lambs in 63 flocks. In India, a study on E. coli isolates from lambs with and without diarrhoea indicated that 9.6 and 24.1 % of isolates belonged to STEC pathotype, respectively (Wani et al. 2009). Contamination of meat and raw milk by the main pathogenic O157 and non-O157 (O26, O103, O111 and O145) STEC O-serogroups representing a major public health concern (Perelle et al. 2007). Similarly, non-O157 STEC pathotype were isolated from Spanish raw ewe’s milk cheese, whereas the isolates belonged to O14 and nontypeable groups (Caro and García-Armesto 2007). Evans et al. (2008) have recovered O26 vtx 1 + and/or vt 2 + E. coli isolates from 4 % of faecal samples of healthy sheep, whereas all of the positive isolates carried eaeA gene. PCR analysis of carcass, faeces and fleece samples from Irish lambs showed that both the vt 1 and vt 2 genes were carried by E. coli O157:H7 isolates (Lenahan et al. 2007).
In this study, any combination of examined virulence genes was detected. In contrast to these results, various combinations of stx 1 , stx 2 and eae genes in non-O157 STEC isolates from sheep were reported previously (Evans et al. 2008; Momtaz et al. 2012). In non-O157 STEC strains from lamb 55 % of strains carried the stx 1 gene, 3 % possessed the stx 2 gene and 42 % carried both the stx 1 and the stx 2 genes (Rey et al. 2003). According to the results, 18 isolates 9.38 % possessed eae gene. Enteropathogenic E. coli (EPEC) strains are defined as intimin-containing diarrhoeagenic E. coli isolates that possess the ability to form AE lesions on intestinal cells and that do not possess genes coding for shiga toxins (Alonso et al. 2012; Bhat et al. 2008). STEC and EPEC isolates are commonly recovered from the faeces of food-producing animals and pose threats to health of humans and livestock (Wani et al. 2009). Vettorato et al. (2009) showed that eae-positive isolates from faeces of Brazilian sheep belonged to non-O157 serogroups O128, O145, O153 and O178.
Regarding to the results, all of the stx 1 and stx 2 -positive isolates were negative for intimin coding gene. The absence of the eae gene in the VTEC strains could indicate that these strains are less virulent for humans that the classical eae-positive enterohaemorrhagic E. coli types (Cortes et al. 2005). Wani et al. (2009) have detected eae gene in 46.2 and 36.8 % of STEC isolates from lambs with and without diarrhoea, respectively.
In the current study, phylogenetic background of E. coli isolates were detected, which were distributed in A (42.71 %), B1 (48.44 %) and D (8.85 %) groups. Phylogenetic group determination of faecal E. coli isolates from human and animals indicated that strains from group B1 were present in all hosts analysed but were more prevalent in sheep, goat and cow samples (Carlos et al. 2010). Similar to the results of this study, none of the faecal isolates from domesticated animals in South Korea belonged to B2 group (Unno et al. 2009). Johnson et al. (2005) reported that conversion to antibiotic resistance occurs more readily in non-B2 phylogenetic groups of E. coli strains. This link between strain phylogeny and antibiotic resistance could explain why in farm animals subjected to antibiotic pressure, A and B1 strains are selected and B2 strains counter selected (Escobar-Paramo et al. 2006). Examination of 29 E. coli from sheep revealed that the isolates fell into three B1 (20 isolates), D (five) and A (four) phylogroup (Carlos et al. 2010). The possible influence of geographic conditions, dietary factors, use of antibiotics and/or host genetic factors on the distribution of phylogenetic groups has been reported (Unno et al. 2009).
Phylogenetic analysis of stx 1 - and stx 2 -positive isolates showed that the isolates belonged to B1 (15 isolates), A (nine) and D (one isolate) groups. In the USA, 2 % of E. coli isolates from diverse human and animal sources belonged to STEC strains. On the other hand, the majority of the STEC strains, which were initially isolated from the ruminants sheep, goats and deer, carried the stx 1c and/or stx 2d, ehxA and saa genes and belonged to E. coli phylogenetic group B1 (Ishii et al. 2007). Phylotyping of enterohaemorrhagic (EHEC) and intimin-positive STEC isolates from animals mostly segregated in B1 (38.7 %) and A (35.5 %) phylogenetic groups (Tramuta et al. 2008). Phylogenetic study on human diarrheagenic E. coli isolates showed that EHEC strains were distributed in phylogroups A and B1 (Gordon et al. 2008).
In the current study, prevalence of antibiotic resistance was detected and phylogenetic background of multi-drug resistant isolates was determined. In comparison to the results of current study, different prevalences of antibiotic-resistant isolates have been reported in ovine isolates from Great Britain, Greece and New Zealand (Enne et al. 2008; Solomakos et al. 2009; Yu et al. 2010). Due to the enormous exploitation of antibiotics in the field of veterinary medicine, problems associated with the presence of antibiotic-resistant bacteria have reached epidemic proportions in recent years (Saei et al. 2010). It is believed that retail foods, and especially meat and meat products, may be an important vehicle for community-wide dissemination of antimicrobial-resistant E. coli and extraintestinal pathogenic E. coli (Sunde and Norstrom 2006). On the other hand, a study on the effect of antibiotic (tetracycline or streptomycin)-supplemented feed on faecal enterohaemorrhagic E. coli O157:H7 population in lambs showed reduction in total number of E. coli O157:H7 shed in the faeces (Lema and Nahashon 2006).
In conclusion, in this part of world, faeces of healthy sheep could be considered as the important sources of non-O157 STEC pathotype and also multidrug-resistant E. coli isolates. Regarding the presence of the isolates which were positive only for eae gene, the researches on initial screening of eae-positive bacteria and eae gene subtyping from ovine sources would help elucidate the role and importance of these isolates. According to the high prevalence of multi-drug resistance, it is important to monitor the resistance to antibiotics not only in pathogenic isolates but also in commensal bacteria of sheep origin.
References
Alonso, M.Z., Lucchesi, P.M.A., Rodríguez, E.M., Parma, A.E. and Padola, N.L., 2012. Enteropathogenic (EPEC) and Shigatoxigenic Escherichia coli (STEC) in broiler chickens and derived products at different retail stores. Food Control, 23, 351–355
Andrade, G.I., Coura, F.M., Santos, E.L., Ferreira, M.G., Galinari, G.C., Facury Filho, E.J., de Carvalho, A.U., Lage, A.P. and Heinemann, M.B., 2012. Identification of virulence factors by multiplex PCRin Escherichia coli isolated from calves in Minas Gerais, Brazil. Tropical Animal Health and Production, doi:10.1007/s11250-012-0139-8
Ayala, C.O., Moreno, R.A.C, Martinez, M.B., Castro, P.A.F. and Bando, S.Y., 2010. Determination of flagellar types by PCR-RFLP analysis of enteropathogenic Escherichia coli (EPEC) and Shiga toxin-producing E. coli (STEC) strains isolated from animals in São Paulo, Brazil. Research in Veterinary Science, 92, 18–23
Bai, J., Paddock, Z.D., Shi, X., Li, S., An, B. and Nagaraja, T.G., 2012. Applicability of a multiplex PCR to detect the seven major shiga toxin–producing Escherichia coli based on genes that code for serogroup-specific O-antigens and major virulence factors in cattle feces. Foodborne Pathogens and Diseases, doi:10.1089/fpd.2011.1082
Bandyopadhyay, S., Mahanti, A., Samanta, I., Dutta, T.K., Ghosh, M.K., Bera, A.K. Bandyopadhyay, S. and Bhattacharya, D., 2011. Virulence repertoire of Shiga toxin-producing Escherichia coli (STEC) and enterotoxigenic Escherichia coli (ETEC) from diarrhoeic lambs of Arunachal Pradesh, India. Tropical Animal Health and Production, 43, 705–710
Bhat, M.A., Nishikawa, Y. and Wani, S.A., 2008. Prevalence and virulence gene profiles of Shiga toxin-producing Escherichia coli and enteropathogenic Escherichia coli from diarrhoeic and healthy lambs in India. Small Ruminant Research, 75, 65–70
Blanco, M., Blanco, J.E., Mora, A., Rey, J.J., Alonso, M., Hermoso, M., Hermoso, J., Alonso, M.P., Dahbi, G., Gonzalez, E.A., Bernardez, M.I. and Blanco, J., 2003. Serotypes, virulence genes, and intimin types of Shiga toxin (Verotoxin)-producing Escherichia coli isolates from healthy sheep in Spain. Journal of Clinical Microbiology, 41, 1351–1356
Carlos, C., Pires, M.M., Stoppe, N.C., Hachich, E.M., Sato, M.I., Amaral, L.A., Gomes, T.A. and Ottoboni, L.M., 2010. Escherichia coli phylogenetic group determination and its application in the identification of the major animal source of fecal contamination. BMC Microbiology, 10, 161
Caro, I. and García-Armesto, M.R., 2007. Occurrence of Shiga toxin-producing Escherichia coli in a Spanish raw ewe’s milk cheese. International Journal of Food Microbiology, 116, 410–413
China, B., Pirson, V. and Mainil, J., 1996. Typing of bovine attaching and effacing Escherichia coli by multiplex in vitro amplification of virulence-associated genes. Applied and Environmental Microbiology, 62, 3462–3465
Clermont, O., Bonacorsi, S. and Bingen, E., 2000. Rapid and simple determination of the Escherichia coli phylogenetic group. Applied and Environmental Microbiology, 66, 4555–4558
CLSI, Clinical Laboratory Standards Institute guidelines, 2004. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals; approved standard M31-S1, Villanova, Pennsylvania.
Coombes, B.K., Gilmour, M.W. and Goodman, C.D., 2011. The evolution of virulence in non-O157 Shiga toxin-producing Escherichia coli. Forntiers in Microbiology, 2, 1–3
Cortes, C., De la Fuente, R., Blanco, J., Blanco, M., Blanco, J.E., Dhabi, G., Mora, A., Justel, P., Contreras, A., Sanchez, A., Corrales, J.C. and Orden, J.A., 2005. Serotypes, virulence genes and intimin types of verotoxin-producing Escherichia coli and enteropathogenic E. coli isolated from healthy dairy goats in Spain. Veterinary Microbiology, 110, 67–76
Enne, V.I., Cassar, C., Sprigings, K., Woodward, M.J. and Bennett, P.M., 2008. A high prevalence of antimicrobial resistant Escherichia coli isolated from pigs and a low prevalence of antimicrobial resistant E. coli from cattle and sheep in Great Britain at slaughter. FEMS MicrobiologyLetter, 278, 193–199
Escobar-Paramo, P., Le Menac’h, A., Le Gall, T., Amorin, C., Gouriou, S., Picard, B., Skurnik, D. and Denamur, E., 2006. Identification of forces shaping the commensal Escherichia coli genetic structure by comparing animal and human isolates. Environmental Microbiology, 8, 1975–1984
Evans, J., Knight, H.I., Smith, A.W., Pearce, M.C., Hall, M., Foster, G., Low, J.C. and Gunn, G.J., 2008. Cefixime–tellurite rhamnose MacConkey agar for isolation of Vero cytotoxin-producing Escherichia coli serogroup O26 from Scottish cattle and sheep faeces. Letters in Applied Microbiology, 47, 148–152
FAOSTAT. 2010. http://www.fao.org/economic/ess/ess-publications/ess-yearbook/ess-yearbook2010/yearbook2010-reources/en/. Accessed May 9, 2012
Ferens, W.A. and Hovde, C.J., 2011. Escherichia coli O157:H7: animal reservoir and sources of human infection. Foodborne Pathogens and Diseases, 8, 465–487
Fernández, D., Sanz, M.E., Parma, A.E. and Padola, N.L., 2012. Characterization of Shiga toxin producing Escherichia coli isolated from newborn, milk-fed, and growing calves in Argentina. Journal of Dairy Science, 95, 5340–5343
Gordon, D.M., Clermont, O., Tolley, H. and Denamur, E., 2008. Assigning Escherichia coli strains to phylogenetic groups: multi-locus sequence typing versus the PCR triplex method. Environmental Microbiology, 10, 2484–2496
Ishii, S., Meyer, K.P. and Sadowsky, M.J., 2007. Relationship between phylogenetic groups, genotypic clusters, and virulence gene profiles of Escherichia coli strains from diverse human and animal sources. Applied and Environmental Microbiology, 73, 5703–5710
Johnson, J.R., Johnston, B., Kuskowski, M.A., Colodner, R. and Raz, R., 2005. Spontaneous conversion to quinolone and fluoroquinolone resistance among wild-type Escherichia coli isolates in relation to phylogenetic background and virulence genotype. Antimicrobial Agents and Chemotherapy, 49, 4739–4744
Kumar, A., Taneja, N., Kumar, Y. and Sharma, M., 2012. Detection of Shiga toxin variants among Shiga toxin-forming Escherichia coli isolates from animal stool, meat and human stool samples in India. Journal of Applied Microbiology, doi:10.1111/j.1365-2672.2012.05415.x
Lema, M. and Nahashon, S., 2006. Effect of antibiotic-supplemented feed on fecal enterohemorrhagic Escherichia coli O157:H7 population in lambs. Small Ruminant Research, 63, 256–261
Lenahan, M., O’Brien, S., Kinsella, K., Sweeney, T. and Sheridan, J.J., 2007. Prevalence and molecular characterization of Escherichia coli O157:H7 on Irish lamb carcasses, fleece and in faeces samples. Journal of Applied Microbiology, 103, 2401–2409
Martin, A. and Beutin, L., 2011. Characteristics of Shiga toxin-producing Escherichia coli from meat and milk products of different origins and association with food producing animals as main contamination sources. International Journal of Food Microbiology, 146, 99–104
Momtaz, H., Farzan, R., Rahimi, E., Dehkordi, F.S. and Souod, N., 2012. Molecular characterization of shiga toxin-producing Escherichia coli isolated from ruminant and donkey raw milk samples and traditional dairy products in Iran. The Scientific World Journal, doi:10.1100/2012/231342
Nguyen, Y. and Sperandio, V., 2012, Enterohemorrhagic E. coli (EHEC) pathogenesis. Frontiers in Cellular and Infection Microbiology. doi:10.3389/fcimb.2012.00090
Oporto, B., Esteban, J.I., Aduriz, G., Juste, R.A. and Hurtado, A., 2008. Escherichia coli O157:H7 and non-O157 Shiga toxin-producing E. coli in healthy cattle, sheep and swine herds in northern Spain. Zoonoses and Public Health, 55, 73–81
Pacheco, A.R. and Sperandio, V., 2012. Shiga toxin in enterohemorrhagic E. coli: regulation and novel anti-virulence strategies. Forntiers in Cellular and Infection Microbiology, doi:10.3389/fcimb.2012.00081
Paris, A., Bonardi, S., Bacci, C., Boni, E., Salmi, F., Bassi, L. and Brindani, F., 2010. Improvement of biomolecular methods for the identification and typing of Escherichia coli O157:H7 isolated from raw meat. Veterinary Research Commutation, 34, S145–S148
Pedersen, K., Clark, L., Andelt, W.F. and Salman, M.D., 2006. Prevalence of Shiga toxin-producing Escherichia coli and Salmonella enterica in rock pigeons captured in Fort Collins, Colorado. Journal of Wildlife Disease, 42, 46–55
Perelle, S., Dilasser, F., Grout, J. and Fach, P., 2007. Screening food raw materials for the presence of the world’s most frequent clinical cases of shiga toxin-encoding Escherichia coli O26, O103, O111, O145 and O157. International Journal of Food Microbiology, 113, 284–288
Rey, J., Blanco, J.E., Blanco, M., Mora, A., Dahbi, G., Alonso, J.M., Hermoso, M., Hermoso, J., Alonso, M.P., Usera, M.A., Gonzalez, E.A., Bernardez, M.I. and Blanco, J., 2003. Serotypes, phage types and virulence genes of shiga-producing Escherichia coli isolated from sheep in Spain. Veterinary Microbiology, 94, 47–56
Saei, D.H., Ahmadi, E., Kazemnia, A. and Ahmadinia, M., 2010. Molecular identification and antibiotic susceptibility patterns of Escherichia coli isolates from sheep faeces samples. Comparative Clinical Pathology, 21, 467–473
Sanchez, S., Martınez, R., Rey, J., Garcıa, A., Blanco, J., Blanco, M., Blanco, J.E., Mora, A., Herrera-Leon, S., Echeita, A. and Alonso, J.M., 2010. Pheno-genotypic characterisation of Escherichia coli O157:H7 isolates from domestic and wild ruminants. Veterinary Microbiology, 142, 445–449
Schaffzin, J.K., Dumas, N.B., Root, T.P., Halse, T.A., Schoonmaker-Bopp, D.J., Lurie, M.M., Nicholas, D., Gerzonich, B., Johnson, G.S., Wallace, B.J. and Musser, K.A., 2012. Public health approach to detection of non-O157 Shiga toxin-producing Escherichia coli: summary of two outbreaks and laboratory procedures. Epidemiology and Infection, 140, 283–289
Solomakos, N., Govaris, A., Angelidis, A.S., Pournaras, S., Burriel, A.R., Kritase, S.K. and Papageorgiou, D.K., 2009. Occurrence, virulence genes and antibiotic resistance of Escherichia coli O157 isolated from raw bovine, caprine and ovine milk in Greece. Food Microbiology, 26, 865–871
Sunde, M. and Norstrom, M., 2006. The prevalence of associations between and conjugal transfer of antibiotic resistance genes in Escherichia coli isolated from Norwegian meat and meat products. Journal of Antimicrobial Chemotherapy, 58, 741–747
Tramuta, C., Robino, P. and Nebbia, P., 2008. Phylogenetic background of attaching and effacing Escherichia coli isolates from animals. Veterinary Research Communication, 32, 433–437
Unno, T., Han, D., Jang, J., Lee, S.N., Ko, G.P., Choi, H.Y., Kim, J.H., Sadowsky, M.J. and Hur, H.G., 2009. Absence of Escherichia coli phylogenetic group B2 strains in humans and domesticated animals from Jeonnam province, Republic of Korea. Applied and Environmental Microbiology, 75, 5659–5666
Vettorato, M.P., de Castro, A.F.P., Cergole-Novella, M.C., Camargo, F.L.L., Irino, K. and Guth, B.E.C., 2009. Shiga toxin-producing Escherichia coli and atypical enteropathogenic Escherichia coli strains isolated from healthy sheep of different populations in Sao Paulo, Brazil. Letters in Applied Microbiology, 49, 53–59
Wani, S.A., Hussain, I., Fayaz, I., Mir, M.A. and Nishikawa, Y., 2009. Subtype analysis of stx1, stx2 and eae genes in Shiga toxin-producing Escherichia coli (STEC) and typical and atypical enteropathogenic E. coli (EPEC) from lambs in India. The Veterinary Journal, 182, 489–490
Yu, P.L., Cross, M.L. and Haverkamp, R.G., 2010. Antimicrobial and immunomodulatory activities of an ovine proline/arginine-rich cathelicidin. International Journal of Antimicrobial Agents, 35, 288–291
Zhang, X.Y., Ding, L.J. and Fan, M.Z., 2009. Resistance patterns and detection of aac(3)-IV gene in apramycin-resistant Escherichia coli isolated from farm animals and farm workers in northeastern of China. Research in Veterinary Science, 87, 449–454
Acknowledgments
This work was supported by a grant from the Shahid Bahonar University of Kerman.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghanbarpour, R., Kiani, M. Characterization of non-O157 shiga toxin-producing Escherichia coli isolates from healthy fat-tailed sheep in southeastern of Iran. Trop Anim Health Prod 45, 641–648 (2013). https://doi.org/10.1007/s11250-012-0271-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11250-012-0271-5