Abstract
Shiga toxin-producing Escherichia coli (STEC) are zoonotic pathogens and may induce severe diarrheagenic diseases in humans and other animals. Non-O157 STEC have been emerging as important pathogens causing outbreaks worldwide. Bacterial resistance to antimicrobials has become a global public health problem, which involves different ecological spheres, including animals. This study aimed to characterize the resistance to antimicrobials, plasmids and virulence, as well as the serotypes and phylogenetic groups in E. coli isolated from sheep in Brazil. A total of 57 isolates were obtained and showed different antimicrobial resistance profiles. Nineteen isolates presented acquired antimicrobial resistance genes (ARGs) (blaCTX-M-Gp9, qnrB, qnrS, oqxB, oqxA, tetA, tetB, tetC, sul1 and sul2) and plasmid families (F, FIA, FIB, I1, K, HI1 and ColE-like). The stx1, stx2 and ehxA virulence genes were detected by PCR, being 50 isolates (87.7%) classified as STEC. A great diversity of serotypes was detected, being O176:HNM the most predominant. Phylogenetic group E was the most prevalent, followed by B1, A and B2. To the best of our knowledge, this is the first report in the world of blaCTX-M-Gp9 (O75, O114, O100, O128ac and O176 serogroups), qnrB and oqxB genes in non-O157 STEC in healthy sheep. The results obtained in the present study call attention to the monitoring of antimicrobial-resistant non-O157 STEC harboring acquired ARGs worldwide and indicate a zoonotic risk due to the profile of virulence, resistance and serotype found.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shiga toxin-producing Escherichia coli (STEC) are zoonotic pathogens related to the hemolytic uremic syndrome (HUS) and hemorrhagic colitis. STEC isolates colonize the gastrointestinal tract of sheep and bovine without causing any disease; however, may induce severe diarrheagenic diseases in humans and other animals (Ferens and Hovde 2011; Kumar et al. 2012). Outbreaks of STEC have been reported worldwide since the STEC O157:H7 is responsible for the most serious outbreaks; however, non-O157 STEC has emerged as important pathogens (Folster et al. 2011; Etcheverría and Padola 2013).
Bacterial resistance to antimicrobials has become a global public health problem, which involves different ecological spheres, including animals. This concern occurs due to the emergence of multidrug-resistant (MDR) bacteria, including E. coli. Increased attention has been given and more studies involving animal sampling have taken place because animals act as reservoirs and disseminators of acquired antimicrobial resistance genes (ARGs) (Salyers and Shoemaker 2006; Toner et al. 2015).
Antimicrobial-resistant STEC obtained from different sources, including animals, and belonging to different serotypes have been reported worldwide, which is worrying (Martin et al. 2015; Mukherjee et al. 2017). Therefore, this study aimed to characterize the resistance to antimicrobials, plasmids and virulence as well as the serotypes and phylogenetic groups in E. coli isolated from sheep in Brazil.
Materials and methods
Obtaining isolates
Fecal samples were collected between 2016 and 2017 from healthy sheep in two farms located in São Paulo State, Brazil. The farm A is 43 km away from Farm B with no reports of antimicrobials use in both farms. One gram of each fecal sample was added in 5 mL of sterile saline solution (0.9% NaCl). Then, the samples were seeded using disposable inoculating loops (10 µL) on MacConkey Agar (Oxoid, UK) and incubated at 37 °C for 18–24 h. Finally, the isolates with morphological characters of E. coli were selected and stocked at − 80 °C in Brain Heart Infusion broth (Oxoid, UK) with 15% glycerol for further identification by sequencing of the 16S rDNA gene.
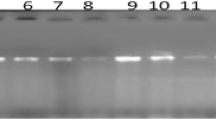
Extraction of genomic DNA, PCR conditions and amplicon sequencing
Genomic DNA extraction was performed using the GenElute™ Bacterial Genomic DNA Kit (Sigma-Aldrich, USA) according to the manufacturer's recommendations. All PCR reactions were performed using the 1.25U (2 μL) of JumpStart™ Taq DNA Polymerase (Sigma-Aldrich, USA), 5 μL of 10X PCR buffer without MgCl2, 25 mM (3.5 μL) of MgCl2, 10 mmol L−1 (1 μL) of deoxynucleotide solution mix, 25 μM (2 μL) of each primer, 100 ng (5 μL) of DNA and 29.5 μL of ultrapure water, totalizing a reaction mixture of 50 μL on a ProFlex™ PCR Thermocycler System (Applied Biosystems, Singapore). Positive and negative controls were used in all PCR reactions.
The amplicons were purified using the Illustra™ GFX™ PCR DNA and Gel Band Purification Kit (GE Healthcare, UK). The sequencing was performed on an ABI 3500xL Genetic Analyzer (Applied Biosystems, USA) using the BigDye™ Terminator v3.1 Cycle Sequencing Kit (Thermo Fisher Scientific, USA). The sequences were analyzed using tools available in GenBank (https://blast.ncbi.nlm.nih.gov/Blast.cgi).
Identification of isolates
The isolates were identified by sequencing of the 16S rDNA gene using the following primers: fD1 (5′-AGAGTTTGATCCTGGCTCAG-3′) and rP2 (5′-ACGGCTACCTTGTTACGACTT-3′) (Weisburg et al. 1991).
Antimicrobial susceptibility testing
The antimicrobial susceptibility testing was performed as recommended by the Clinical and Laboratory Standards Institute (CLSI 2017) using the disk diffusion method. A total 36 antimicrobials was tested for each isolate, including ampicillin, amoxicillin-clavulanate, ampicillin-sulbactam, piperacillin-tazobactam, ticarcillin-clavulanate, cefazolin, cefoxitin, cefuroxime, cefaclor, ceftazidime, ceftriaxone, cefotaxime, cefepime, aztreonam, ertapenem, imipenem, meropenem, gentamicin, tobramycin, amikacin, nalidixic acid, lomefloxacin, ofloxacin, ciprofloxacin, norfloxacin, levofloxacin, streptomycin, tetracycline, doxycycline, minocycline,, trimethoprim-sulfamethoxazole, sulfonamide, trimethoprim, chloramphenicol and nitrofurantoin. E. coli ATCC® 25922 and Pseudomonas aeruginosa ATCC® 27853 strains were used as control.
Detection of acquired ARGs
Acquired ARGs were screened by PCR in non-susceptible (intermediate or resistant) isolates for β-lactams (blaCTX-M groups 1, 2, 8 and 9, blaSHV, blaCMY and blaOXA-1-like), tetracyclines (tetA, tetB, tetC, tetD, tetE, tetG, tetJ, tetL, tetM, tetO, tetS, tetP, tetQ and tetX), quinolone and fluoroquinolones (qnrA, qnrB, qnrS, qepA, oqxA and oqxB), aminoglycosides (aac(3′)-Ia, aac(3′)-IIa, ant(2″)-Ia, aac(6′)-Ih, aph(3′)-VI, aac(6′)-Ib and aph(3′)-Ia) and sulfonamides (sul1, sul2 and sul3) (Noppe-Leclercq et al. 1999; Ng et al. 2001; Kerrn et al. 2002; Perreten and Boerlin 2003; Cattoir et al. 2007; Dallenne et al. 2010; Karczmarczyk et al. 2011; Chen et al. 2012).
Detection of virulence genes
Detection of the diarrheagenic virulence genes was performed by PCR. The genes ipaH stx1, stx2, ehxA, aaiC, aatA, eaeA, bfpA, aggR, elt est, aap, aggR and AA probe were detected using the primers described by Schmidt et al. (1995), Paton and Paton (1998), Aranda et al. (2007), Lima et al. (2013) and Cerna et al. (2003).
Plasmid replicon typing
Twenty plasmid families (IncHI2, IncHI1, IncI1, IncFIB, IncFIA, IncFIC, IncF, IncFIIA, IncL/M, IncW, IncP, IncA/C, IncK, IncN, IncY, IncT, IncX, IncU, IncR and ColE-like) were researched by PCR-based replicon typing according to Carattoli et al. (2005) and García-Fernández et al. (2009).
Escherichia coli serotyping
Escherichia coli serotyping was performed using rabbit antisera against antigens [O1 to O187 somatic (O) and 53 flagellar (H)] by agglutination assays using 96-well Microtiter™ microplates (Thermo Scientific, USA) according to Orskov and Orskov (1984) and Scheutz et al. (2004).
Phylogenetic group determination
Phylogenetic groups (A, B1, B2, C, D, E and F) were determined using the phylo-typing method according to Clermont et al. (2013). The phylogenetic groups were determined using the quadruplex genotype (arpA, chuA, yjaA, TspE4.C2), being A ( + − −), B1 ( + − + ), B2 (− + + −, − + + + or − + − + ) and F (− + –). C- and E-specific primers (trpA and arpA) were used for classification of phylogenetic groups C ( + − + −, C + ), D ( + + – or + + − + , E-) and E ( + + – or + + − + , E + ).
Results
Isolates, genes and phylogenetic groups
In this study, 57 bacterial isolates were obtained, being 42 from farm A and 15 from farm B. These isolates showed different antimicrobial resistance profiles, several acquired ARGs and different plasmid families, including ColE-like, F, FIB, FIA, I1, K and HI1. The stx1, stx2 and ehxA virulence genes were detected, being 50 isolates (87.7%) classified as STEC and a great diversity of serotypes was observed, being O176:HNM the most prevalent. Four phylogenetic groups were detected (A, B1, B2 and E) and four isolates (A4, A5, A6 and A27) were not classified into any phylogenetic group, being denominated as unknown (Tables 1, 2).
The results were divided into two groups for a better presentation. In the first one were reported the isolates that presented acquired ARGs, which also presented non-susceptibility for several antimicrobials and the presence of plasmids. In group 2 were gathered the isolates with no acquired ARGs, being some of them susceptible to all tested antimicrobials and other non-susceptible to at least one antimicrobial. The sequences obtained from the 16S rRNA and acquired ARGs were deposited in the GenBank (www.ncbi.nlm.nih.gov/Genbank) with accession numbers MK506922-MK506978, MK532862-MK532896, MK543886 and MK543887.
Characterization of Group 1
Group 1 has 19 isolates [Farm 1 (15) and Farm 2 (4)], being 11 (57.9%) non-susceptible to sulfonamide, nine (47.3%) to ampicillin, cefazolin, cefoxitin and cefaclor, seven (36.8%) to tetracycline and doxycycline, five (26.3%) to ciprofloxacin, levofloxacin, norfloxacin, lomefloxacin and ofloxacin, and four (21%) to trimethoprim-sulfamethoxazole, nalidixic acid, streptomycin and trimethoprim. A total of 38 amplicons from different acquired ARGs were detected and according to this profile, the blaCTX-M-Gp9 (9) was the most prevalent, followed by tetB (6), qnrS (5), tetA (4), qnrB (4), sul1 (2), sul2 (2), oqxB (2), oqxA (2) and tetC (1) (Table 1).
Seven plasmid families were found in the group 1, being the ColE-like (12) the most prevalent, followed by FIB (7), F (6), I1 (4), K (4), FIA (1) and HI1 (1). The stx1 gene was detected in 12 isolates, followed by ehxA (11) and stx2 (1) genes. Twelve isolates were classified as STEC. Thirteen serotypes were detected in this group, including O154:H9 (4), O176:HNM (3), O185:HNM (2), O70:HNM (1), O75:HNM (1), O86:H2 (1), O100:H21 (1), O114:H14 (1), O129:H20 (1), A128ac:H2 (1), O176:H19 (1), O185:H16 (1) and ONT:HNM (1). Seven isolates were classified into phylogenetic group B1, four into A and unknown, three into E and one into B2 (Table 1).
Characterization of Group 2
In group 2, 38 isolates were gathered [Farm 1 (27) and Farm 2 (11)]. Among them, 24 (63.1%) were non-susceptible to sulfonamide, 14 (36.8%) to cefazolin, 12 (31.5%) to cefaclor, three (7.9%) to ampicillin, and one (2.6%) to chloramphenicol, cefuroxime, gentamicin, tobramycin and amikacin. The stx1 gene was detected in all isolates, followed by ehxA (31) and stx2 (5) genes. Thus, all isolates were classified as STEC. The O176:HNM (24) serotype was the most prevalent, followed by O91:HNM (3); O75:HNM (2), O48:H16 (1), O88:H4 (1), O88:H25 (1), O114:H4 (1), O93:H52 (1), O139:H19 (1), O75:H8 (1), O8:H19 (1) and ONT:HNM (1) The majority of isolates was classified into phylogenetic group E (25), followed by B1 (11), A (1) and B2 (1) (Table 2). In general, it was observed that isolates belonging to the group 1 presented a higher resistance profile, while the group 2 showed a greater virulence potential, with all isolates classified as STEC since the eaeA gene was not detected.
Discussion
The majority of outbreaks caused by STEC are related to the consumption of contaminated products with animal feces, including sheep. STEC produces Shiga toxins 1 (Stx1) and 2 (Stx2), which are encoded by stx1 and stx2 genes, respectively. In addition, some virulence markers such as enterohemolysin (ehxA) may be associated with these toxins and some studies have reported that Stx2 is more commonly reported in cases of HUS (Paton and Paton 1998; Ferens and Hovde 2011; Kumar et al. 2012; Etcheverría and Padola 2013).
The Center for Disease Control and Prevention report (CDC 2015) showed an increase in the incidence rate of infections caused by non-O157 STEC between 1996 and 2015 in the United States, especially in children aged 1 to 4 years and Tseng et al. (2016) also reported a significant increase of non-O157 STEC cases over time. Among the large diversity of reported non-O157 STEC serotypes are O8, O70, O75, O86, O88, O91, O93, O100, O114, O128, O129, O154 and O185, which are the same reported in the present study.
Amézquita-López et al. (2016), Kusumoto et al. (2016) and Ghanbarpour and Kiani (2013) reported non-O157 STEC obtained from animals, including sheep, which were non-susceptible to several antimicrobials, such as β-lactams, tetracyclines, aminoglycosides, fluoroquinolones and sulfonamides. In Brazil, similar results were also reported with strains collected from animals and humans (Cergole-Novella et al. 2011).
Many studies have characterized the phenotypic profile of antimicrobial resistance in non-O157 STEC isolates; however, there are few reports of acquired ARGs. β-lactamases belonging to CTX-M-group stand out among ESBLs because of their spectrum of action and dissemination in isolates from a variety of sources, including animals (Cantón et al. 2012). Some non-O157 STEC have already been detected carrying blaCTX-M-group in serogroups not detected in this work, such as O5, O104, O111 and O145 (Valat et al. 2012; Ewers et al. 2014; Ferdous et al. 2016). However, this is the first report of blaCTX-M-Gp9 in non-O157 STEC belonging to O75, O114, O100, O128ac and O176 serogroups.
There are few descriptions of non-O157 STEC carrying multiple acquired ARGs worldwide. Bai et al. (2016), Ferdous et al. (2016) and Srinivasa et al. (2011) reported a diversity of non-O157 STEC carrying acquired resistance genes for fluoroquinolones (qnrS and oqxA), tetracyclines (tetA, tetB, tetC, tetM) and sulfonamides (sul1 and sul2) associated with different plasmid families, but there are no reports of qnrB and oqxB in non-O157 STEC.
Some plasmid families are correlated with the presence of acquired ARGs in STEC as well as in non-STEC, including those detected in the present study (Carattoli 2013; Ewers et al. 2014). Among the plasmid families, ColE-like and IncF are prevalent and have been detected worldwide carrying blaCTX-M-groups, plasmid-mediated quinolone resistance genes (PMQR), tet genes and sul genes (Pallecchi et al. 2010; Carattoli 2013; Lyimo et al. 2016; Yang et al. 2015).
A diversity of phylogenetic groups was detected (A, B1, B2 and E) in STEC isolates resistant and susceptible to antimicrobials obtained of two Brazilian farms, including that classified as unknown. Stoppe et al. (2017) showed that there is no correlation between geographic location, date or feeding habits and phylogenetic groups in isolates obtained worldwide, even in Brazil. Mora et al. (2012) and Carlos et al. (2010) reported that phylogenetic group B1 was the most prevalent in STEC and non-STEC isolates from different sources, including sheep, and that phylogenetic groups A and B2 were also reported. Interesting, the majority of STEC isolates from the present study was classified into phylogenetic group E, which is probably less reported due to its recent identification (Clermont et al. 2013).
The results found in the present study call attention to the monitoring of antimicrobial-resistant non-O157 STEC harboring acquired ARGs worldwide. These isolates can spread to different sources, as humans and animals, and disseminate ARGs through horizontal gene transfer to other pathogens. To the best of our knowledge, this is the first report in the world of blaCTX-M-Gp9 (O75, O114, O100, O128ac and O176 serogroups), qnrB and oqxB genes in non-O157 STEC in healthy sheep. The results indicate a zoonotic risk due to the profile of virulence, resistance and serotype found.
References
Amézquita-López BA, Quiñones B, Soto-Beltrán M, Lee BG, Yambao JC, Lugo-Melchor OY, Chaidez C (2016) Antimicrobial resistance profiles of Shiga toxin-producing Escherichia coli O157 and Non-O157 recovered from domestic farm animals in rural communities in Northwestern Mexico. Antimicrob Resist Infect Control 5:1. https://doi.org/10.1186/s13756-015-0100-5
Aranda K, Fabbricotti SH, Fagundes-Neto U, Scaletsky ICA (2007) Single multiplex assay to identify simultaneously enteropathogenic, enteroaggregative, enterotoxigenic, enteroinvasive and Shiga toxin producing Escherichia coli strains in Brazilian children. FEMS Microbiol Lett 267:145. https://doi.org/10.1111/j.1574-6968.2006.00580.x
Bai L, Hurley D, Li J, Meng Q, Wang J, Fanning S, Xiong Y (2016) Characterisation of multidrug-resistant Shiga toxin-producing Escherichia coli cultured from pigs in China: co-occurrence of extended-spectrum β-lactamase- and mcr-1-encoding genes on plasmids. Int J Antimicrob Agents 48:445–448. https://doi.org/10.1016/j.ijantimicag.2016.06.021
Cantón R, González-Alba JM, Galán JC (2012) CTX-M enzymes: origin and diffusion. Front Microbiol 3:110. https://doi.org/10.3389/fmicb.2012.00110
Carattoli A (2013) Plasmids and the spread of resistance. Int J Med Microbiol 303(6–7):298–304. https://doi.org/10.1016/j.ijmm.2013.02.001
Carattoli A, Bertini A, Villa L, Falbo V, Hopkins KL, Threlfall EJ (2005) Identification of plasmids by PCR-based replicon typing. J Microbiol Methods 63:219–228. https://doi.org/10.1016/j.mimet.2005.03.018
Carlos C, Pires MM, Stoppe NC, Hachich EM, Sato MI, Gomes TA, Amaral LA, Ottoboni LM (2010) Escherichia coli phylogenetic group determination and its application in the identification of the major animal source of fecal contamination. BMC Microbiol 10:161. https://doi.org/10.1186/1471-2180-10-161
Cattoir V, Poirel L, Rotimi V, Soussy CJ, Nordmann P (2007) Multiplex PCR for detection of plasmid-mediated quinolone resistance qnr genes in ESBL-producing enterobacterial isolates. J Antimicrob Chemother 60:394–397. https://doi.org/10.1093/jac/dkm204
Centers for Disease Control and Prevention (CDC). National STEC Surveillance Annual Report, 2015. Atlanta, Georgia: US Department of Health and Human Services, CDC, 2017. Retrieved from https://www.cdc.gov/nationalsurveillance/pdfs/STEC_Annual_Summary_2015-508c.pdf. Accessed 10 Jan 2019.
Cergole-Novella MC, Pignatari AC, Castanheira M, Guth BE (2011) Molecular typing of antimicrobial-resistant Shiga-toxin-producing Escherichia coli strains (STEC) in Brazil. Res Microbiol 162:117–123. https://doi.org/10.1016/j.resmic.2010.09.022
Cerna JF, Nataro JP, Estrada-Garcia T (2003) Multiplex PCR for detection of three plasmid-borne genes of enteroaggregative Escherichia coli strains. J Clin Microbiol 41:2138–2140
Chen X, Zhang W, Pan W, Yin J, Pan Z, Gao S, Jiao X (2012) Prevalence of qnr, aac(6')-Ib-cr, qepA, and oqxAB in Escherichia coli isolates from humans, animals, and the environment. Antimicrob Agents Chemother 56:3423–3427. https://doi.org/10.1128/AAC.06191-11
Clermont O, Christenson JK, Denamur E, Gordon DM (2013) The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep 5:58–65. https://doi.org/10.1111/1758-2229.12019
CLSI (2017) Performance standards for antimicrobial susceptibility testing: twenty-seventh informational supplement. CLSI document M100–S27. Clinical and Laboratory Standards Institute, Wayne, PA
Dallenne C, Costa A, Decré D, Favier C, Arlet G (2010) Development of a set of multiplex PCR assays for the detection of genes enconding importante beta-lactamases in Enterobacteriaceae. J Antimicrob Chemother 65:490–495. https://doi.org/10.1093/jac/dkp498
Etcheverría AI, Padola NL (2013) Shiga toxin-producing Escherichia coli: factors involved in virulence and cattle colonization. Virulence 4:366–372. https://doi.org/10.4161/viru.24642
Ewers C, Stamm I, Stolle I, Guenther S, Kopp PA, Fruth A, Wieler LH, Scheufen S, Bauerfeind R, Bethe A, Prenger-Berninghoff E (2014) Detection of Shiga toxin- and extended-spectrum β-lactamase-producing Escherichia coli O145:NM and Ont:NM from calves with diarrhoea. J Antimicrob Chemother 69:2005–2007. https://doi.org/10.1093/jac/dku042
Ferdous M, Friedrich AW, Grundmann H, de Boer RF, Croughs PD, Islam MA, Kluytmans-van den Bergh MF, Kooistra-Smid AM, Rossen JW (2016) Molecular characterization and phylogeny of Shiga toxin-producing Escherichia coli isolates obtained from two Dutch regions using whole genome sequencing. Clin Microbiol Infect 22:642.e1–9. https://doi.org/10.1016/j.cmi.2016.03.028
Ferens WA, Hovde CJ (2011) Escherichia coli O157:H7: animal reservoir and sources of human infection. Foodborne Pathog Dis 8:465–487. https://doi.org/10.1089/fpd.2010.0673
Folster JP, Pecic G, Taylor E, Whichard J (2011) Characterization of Isolates from an outbreak of multidrug-resistant, Shiga toxin-producing Escherichia coli O145 in the United States. Antimicrob Agents Chemother 55:5955–5956. https://doi.org/10.1128/AAC.05545-11
García-Fernández A, Fortini D, Veldman K, Mevius D, Carattoli A (2009) Characterization of plasmids harbouring qnrS1, qnrB2 and qnrB19 genes in Salmonella. J Antimicrob Chemother 63:274–281. https://doi.org/10.1093/jac/dkn470
Ghanbarpour R, Kiani M (2013) Characterization of non-O157 shiga toxin-producing Escherichia coli isolates from healthy fat-tailed sheep in southeastern of Iran. Trop Anim Health Prod 45:641–648. https://doi.org/10.1007/s11250-012-0271-5
Karczmarczyk M, Abbott Y, Walsh C, Leonard N, Fanning S (2011) Characterization of multidrug-resistant Escherichia coli isolates from animals presenting at a university veterinary hospital. Appl Environ Microbiol 77:7104–7112. https://doi.org/10.1128/AEM.00599-11
Kerrn MB, Klemmensen T, Frimodt-Mǿller N, Espersen F (2002) Susceptibility of Danish Escherichia coli strains isolated from urinary tract infections and bacteraemia, and distribution of sul genes conferring sulphonamide resistance. J Antimicrob Chemother 50:513–516. https://doi.org/10.1093/jac/dkf164
Kumar A, Taneja N, Kumar Y, Sharma M (2012) Detection of Shiga toxin variants among Shiga toxin-forming Escherichia coli isolates from animal stool, meat and human stool samples in India. J Appl Microbiol 113:1208–1216. https://doi.org/10.1111/j.1365-2672.2012.05415.x
Kusumoto M, Hikoda Y, Fujii Y, Murata M, Miyoshi H, Ogura Y, Gotoh Y, Iwata T, Hayashi T, Akiba M (2016) Emergence of a multidrug-resistant Shiga toxin-producing enterotoxigenic Escherichia coli lineage in diseased swine in Japan. J Clin Microbiol 54:1074–1081. https://doi.org/10.1128/JCM.03141-15
Lima IF, Boisen N, Quetz Jda S, Havt A, de Carvalho EB, Soares AM, Lima NL, Mota RM, Nataro JP, Guerrant RL, Lima AÂ (2013) Prevalence of enteroaggregative Escherichia coli and its virulence-related genes in a case-control study among children from north-eastern Brazil. J Med Microbiol 62:683–693. https://doi.org/10.1099/jmm.0.054262-0
Lyimo B, Buza J, Subbiah M, Temba S, Kipasika H, Smith W, Call DR (2016) IncF plasmids are commonly carried by antibiotic resistant Escherichia coli isolated from drinking water sources in Northern Tanzania. J Med Microbiol 2016:3103672. https://doi.org/10.1155/2016/3103672
Martin MJ, Thottathil SE, Newman TB (2015) Antibiotics overuse in animal agriculture: a call to action for health care providers. Am J Public Health 105:2409–2410. https://doi.org/10.2105/AJPH.2015.302870
Mora A, López C, Dhabi G, López-Beceiro AM, Fidalgo LE, Díaz EA, Martínez-Carrasco C, Mamani R, Herrera A, Blanco JE, Blanco M, Blanco J (2012) Seropathotypes, phylogroups, Stx subtypes, and intimin types of wildlife-carried, shiga toxin-producing Escherichia coli strains with the same characteristics as human-pathogenic isolates. Appl Environ Microbiol 78:2578–2585. https://doi.org/10.1128/AEM.07520-11
Mukherjee S, Mosci RE, Anderson CM, Snyder BA, Collins J, Rudrik JT, Manning SD (2017) Antimicrobial drug-resistant Shiga toxin-producing Escherichia coli infections, Michigan, USA. Emerg Infect Dis 23:1609–1611. https://doi.org/10.3201/eid2309.170523
Ng LK, Martin I, Alfa M, Mulvey M (2001) Multiplex PCR for the detection of tetracycline resistant genes. Mol Cell Probes 15:209–215. https://doi.org/10.1006/mcpr.2001.0363
Noppe-Leclercq I, Wallet F, Haentjens S, Courcol R, Simonet M (1999) PCR detection of aminoglycoside resistance genes: a rapid molecular typing method for Acinetobacter baumannii. Res Microbiol 150:317–322
Orskov F, Orskov I (1984) Serotyping of Escherichia coli. Methods Microbiol 14:43–112
Pallecchi L, Riccobono E, Sennati S, Mantella A, Bartalesi F, Trigoso C, Gotuzzo E, Bartoloni A, Rossolini GM (2010) Characterization of small ColE-like plasmids mediating widespread dissemination of the qnrB19 gene in commensal enterobacteria. Antimicrob Agents Chemother 54:678–682. https://doi.org/10.1128/AAC.01160-09
Paton AW, Paton JC (1998) Detection and characterization of Shiga toxigenic Escherichia coli by using multiplex PCR assays for stx1, stx2, eaeA, enterohemorrhagic E. coli hlyA, rfbO111, and rfbO157. J Clin Microbiol 36:598–602
Perreten V, Boerlin P (2003) A new sulfonamide resistance gene (sul3) in Escherichia coli is widespread in the pig population of Switzerland. Antimicrob Agents Chemother 47:1169–1172
Salyers A, Shoemaker NB (2006) Reservoirs of antibiotic resistance genes. Anim Biotechnol 17:137–146. https://doi.org/10.1080/10495390600957076
Scheutz F, Cheasty T, Woodward D, Smith HR (2004) Designation of O174 and O175 to temporary O groups OX3 and OX7, and six new E. coli O groups that include Verocytotoxin-producing E. coli (VTEC): O176, O177, O178, O179, O180 and O181. APMIS 112:569–584. https://doi.org/10.1111/j.1600-0463.2004.apm1120903.x
Schmidt H, Knop C, Franke S, Aleksic S, Heesemann J, Karch H (1995) Development of PCR for screening of enteroaggregative Escherichia coli. J Clin Microbiol 33:701–705
Srinivasa TR, Gill JPS, Kumar GVVPS, Ghatak S (2011) Multi drug resistance patterns of Shiga toxin–producing Escherichia coli (STEC) and non–STEC isolates from meats, RTE meat foods, drinking water and human diarrhoeic samples of Punjab. India Arch Clin Microbiol 2:3. https://doi.org/10.3823/225
Stoppe NC, Silva JS, Carlos C, Sato MIZ, Saraiva AM, Ottoboni LMM, Torres TT (2017) Worldwide phylogenetic group patterns of Escherichia coli from commensal human and wastewater treatment plant isolates. Front Microbiol 8:2512. https://doi.org/10.3389/fmicb.2017.02512
Toner E, Adalja A, Gronvall GK, Cicero A, Inglesby TV (2015) Antimicrobial resistance is a global health emergency. Health Secur 13:153–155. https://doi.org/10.1089/hs.2014.0088
Tseng M, Sha Q, Rudrik JT, Collins J, Henderson T, Funk JA, Manning SD (2016) Increasing incidence of non-O157 Shiga toxin-producing Escherichia coli (STEC) in Michigan and association with clinical illness. Epidemiol Infect 144:1394–1405. https://doi.org/10.1017/S0950268815002836
Valat C, Haenni M, Saras E, Auvray F, Forest K, Oswald E, Madec JY (2012) CTX-M-15 extended-spectrum β-lactamase in a shiga toxin-producing Escherichia coli isolate of serotype O111:H8. Appl Environ Microbiol 78:8–9. https://doi.org/10.1128/AEM.06997-11
Weisburg WG, Barns SM, Pelletier BA, Lane DJ (1991) 16S ribosomal DNA amplification for phylogenetic study. J Bacteriol 173:697–703. https://doi.org/10.1128/jb.173.2.697-703.1991
Yang QE, Sun J, Li L, Deng H, Liu BT, Fang LX, Liao XP, Liu YH (2015) IncF plasmid diversity in multi-drug resistant Escherichia coli strains from animals in China. Front Microbiol 6:964. https://doi.org/10.3389/fmicb.2015.00964
Acknowledgements
The authors thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for fellowship [Grant No. 88882.180855/2018-01].
Funding
This work was supported by São Paulo Research Foundation—FAPESP [Grant No. 2018/19539-0].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Furlan, J.P.R., Gallo, I.F.L., de Campos, A.C.L.P. et al. Characterization of non-O157 Shiga toxin-producing Escherichia coli (STEC) obtained from feces of sheep in Brazil. World J Microbiol Biotechnol 35, 134 (2019). https://doi.org/10.1007/s11274-019-2712-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11274-019-2712-z