Abstract
The present study was conducted to study the antibiotic resistance pattern among nontyphoidal Salmonella isolated from human, animal and meat. A total of 37 Salmonella strains isolated from clinical cases (human and animal) and meat during 2008–2009 belonging to 12 serovars were screened for their antimicrobial resistance pattern using 25 antimicrobial agents falling under 12 different antibiotic classes. All the Salmonella isolates tested showed multiple drug resistance varying from 5.40% to 100% with 16 of the 25 antibiotics tested. None of the isolates were sensitive to erythromycin and metronidazole. Resistance was also observed against clindamycin (94.59%), ampicillin (86.49%), co-trimoxazole (48.65%), colistin (45.94%), nalidixic acid (35.10%), amoxyclave (18.90%), cephalexin, meropenem, tobramycin, nitrofurantoin, tetracycline, amoxicillin (8.10% each), sparfloxacin and streptomycin (5.40% each). Isolates from clinical cases of animals were resistant to as many as 16 antibiotics, whereas isolates from human clinical cases and meat were resistant to 9 and 14 antibiotics, respectively. Overall, 19 resistotypes were recorded. Analysis of multiple antibiotic resistance index (MARI) indicated that clinical isolates from animals had higher MARI (0.25) as compared to isolates from food (0.22) and human (0.21). Among the different serotypes studied for antibiogram, Paratyhi B isolates, showed resistance to three to 13 antibiotics, whereas Typhimurium strains were resistant to four to seven antibiotics. Widespread multidrug resistance among the isolates from human, animal and meat was observed. Some of the uncommon serotypes exhibited higher resistance rate. Considerable changes in the resistance pattern were also noted. An interesting finding was the reemergence of sensitivity to some of the old antibiotics (chloromphenicol, tetracycline).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salmonella infection is one of the main zoonotic diseases worldwide (Vo et al., 2010). Salmonellosis in humans can manifest in a number of disease syndromes including enteric fever (typhoid-like disease) and nontyphoidal form. Enteric fever is an endemic disease in the tropic and subtropic regions and has become a major health problem in developing countries (Okon, 2010). The most common clinical manifestation of nontyphoidal salmonellosis is that of acute gastroenteritis with a short and self-limiting clinical course. However, severe sequelae, such as bacteremia or meningitis, may develop in an approximately 5–10% of individuals infected with nontyphoid Salmonella (Su and Chiu, 2007)
Salmonella infections are also common in different species of animals. Host specific Salmonella serotypes such as Choleraesuis, Abortusequi, Gallinarum commonly produces systemic diseases and are characterized by low morbidity and high mortality. Gastrointestinal symptoms are predominant with generalist serotypes and are often characterized by high morbidity but low mortality (Hoelzer et al., 2011). Almost all cold-blooded and warm-blooded animals serve as natural host for Salmonella spp.
The most common serovars that cause infection in humans and food animals belong to subspecies enterica. Of the 2,610 serovars recorded so far (Guibourdenche et al., 2010), over 2,300 serovars were identified within subspecies I. However, only a small fraction of the thousands of described subspecies I serovars frequently cause disease in humans and domestic animals. Incidence of disease caused by different serovars varies over time and evolution is further punctuated by the emergence of epidemic and multidrug resistant variants (Stevens et al., 2009). There are also occasional reports of occurrence of uncommon serotypes from clinical cases (Antony et al., 2009; Kulkarni et al., 2009).
Of increasing concern is the worldwide emergence of multidrug resistant phenotypes among Salmonella serotypes (Sirichote et al., 2010), in particular S. Typhimurium, which express resistance to ampicillin, chloramphenicol, streptomycin, sulfamethoxazole and tetracycline (ACSSuT) (Hall, 2010). There are many reasons for the spread of multidrug resistance. A major concern is the use of antibiotics in food animals (Nikaido, 2009). An estimate in the United States suggests that 111,583.72 MT of antibiotics are given to animals each year as growth promoters at subtherapeutic amounts in their feed compared to 1,366.77 MT consumed by humans (White et al., 2001).
Nontyphoidal human Salmonella diarrhea does not warrant antimicrobial therapy; however, there are occasions when the infections can lead to life-threatening systemic infections that require effective chemotherapy (Vila et al., 2006). In developing countries like India, easy availability of a wide range of drugs coupled with inadequate health services result in increased proportions of drugs used as self-medication compared to prescribed drugs resulting in impending health problems and antimicrobial resistance. Problems caused by the increasing antimicrobial resistance of Salmonella include not only difficulties in antimicrobial therapy but also the apparent predilection of the organism to cause serious diseases. The possible emergence and spread of Salmonella strains resistant to antibiotics commonly used as treatment are concerns, because these infections can be invasive and difficult to treat by the drugs of choice for invasive Salmonella disease (Paterson, 2006). Monitoring drug resistance pattern is important to decide the therapeutic regime to be adopted against individual cases, and to devise a comprehensive chemoprophylactic and chemotherapeutic drug schedule on herd basis within a geographical area (Murugkar et al., 2004). MDR is also a concern in tropical regions, where there may be variation in resistance pattern compared to other parts of the world (Vila et al., 2006).
Although information on typhoidal Salmonella is widely studied in medical literature, data specifically describing the antibiogram among clinical isolates of nontyphoidal Salmonella of human and animal in India is scarce. We describe the prevalence of multidrug resistance among the clinical and meat isolates of Salmonella.
Material and methods
Salmonella isolates
Salmonella isolates (37) isolated during 2008–2009, belonging to 12 serovars (Paratyphi B var java, Typhimurium, Enteritidis, Isangi, Virchow, Heidelberg, Berta, Tshiongwe, Saintpaul, Bsilla, Labadi and rough type) were included in the study (Table 1). Twenty-seven of the isolates were isolated in our previous study from human and animal clinical cases and ten isolates were obtained from stocks at the National SalmoneIlla Centre (Vet), Indian Veterinary Research Institute, Izatnagar, repository. All isolates were confirmed through biochemical and serological methods (Agarwal et al., 2003; Farmer, 1995) and maintained on nutrient agar slopes until tested. A reference E. coli K12 strain (E-382), sensitive to all antimicrobials, was used as control.
Antimicrobial sensitivity assay
All the Salmonella isolates were examined for their antimicrobial drugs susceptibility/resistance pattern in triplicate on Mueller Hinton agar No. 4 (Himedia, Mumbai, India) by disc diffusion technique using 25 different antimicrobial agents belonging to 12 different classes. The antibiotics used were as follows, aminoglycosides (streptomycin 10 μg, gentamicin 10 μg, tobramycin 5 μg), polymyxinn (colistin 10 μg), cephalosporins (cephalexin 30 μg, cefotaxime 30 μg), imidazoles (metronidazole 5 μg), quinolones (nalidixic acid 30 μg, ciprofloxacin, levofloxacin 5 μg, sparofloxacin 5 μg, moxifloxacin 5 μg, norfloxacin 10 μg, ofloxacin 5 μg), macrolides (erythromycin 15 μg), carbapenem (imipenem 10 μg, meropenem 10 μg), penicillins (amoxicillin 30 μg, amoxyclave 10 μg, ampicillin 10 μg), tetracyclines (tetracycline 30 μg), lincosamides (clindamycin 2 μg), sulphonamides (co-trimoxazole 25 μg) and others (chloramphenicol 10 μg, nitrofurantoin 30 μg).
Based on zone of inhibition, isolates were classified as sensitive or resistant according to manufacturer's (Himedia, Mumbai, India) instructions. Data of isolates were computerized and analyzed with Statistical Package for Social Science (SPSS) software (version 10.0) (SPSS, Inc.) for determining relatedness among isolates.
Multiple antibiotic resistance index (MARI) for each resistance pattern was calculated by employing following formula:
Results
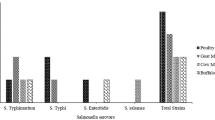
All the Salmonella strains tested in the study were shown to be multiple drug resistant. Resistance rate varied from 5.40% to 100%, with as many as 16 of the 25 antibiotics tested showing some degree of resistance. Majority of the isolates (54%) were resistant to <5 antibiotics and reaming isolates (46%) were resistant to >6 drugs. Four of the isolates were resistant to as many as 10–15 antibiotics. All the isolates were resistant to erythromycin and metronidazole. Other antibiotics that show resistance were clindamycin (94.59%), ampicillin (86.49%), co-trimoxazole (48.65%), colistin (45.94%), nalidixic acid (35.10%), amoxyclave (18.90%), cephalexin, meropenem, tobramycin, nitrofurantoin, tetracycline, amoxicillin (8.10% each), sparfloxacin and streptomycin (5.40% each). Nine antimicrobials (cefotaxime, ciprofloxacin, chloramphenicol, norfloxacin, impenem, oflaxacin, moxifloxacin, levofloxacin, and gentamicin) were the most effective antimicrobials showing 100% efficacies (Table 2).
Isolates from animal clinical cases showed resistance to as many as 16 antibiotics in comparison to isolates from human clinical cases and meat, which were resistant to 9 and 14 antibiotics, respectively. Only animal clinical isolates recorded some resistance against nitrofuranatoin and streptomycin, whereas some isolates of both animal clinical and meat origins were resistant to tobramycin, sparfloxacin, tetracycline and amoxicillin.
There were 19 resistotypes recorded in the study (Table 3). Among the 19 resistotypes, ACdClEMtNa and ACdEMt were the most commonly expressed by six isolates each. Four isolates each demonstrated CdEMtNa and ACdCoEMt resistotypes.
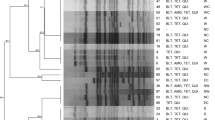
Hierarchical cluster analysis revealed two distinct clusters, A and B (Fig. 1). Cluster A represented 14 of 17 resistotypes and could be subdivided into three subclusters. In cluster A1, most of the isolates were of cow (5) and meat origin. One isolates each from buffalo and human were also part of this subcluster. A2 subcluster consisted mostly of isolates from cow (8) and human (3) along with meat (2) and buffalo (1) isolates. Subcluster A3 represented three isolates each from human and cow and one isolate each from goat and meat. Interestingly, all the three isolates in cluster B were from buffalo (two diarrhea and one beef).
Multiple antibiotic resistance index (MARI) analysis (Table 4) indicated that animal clinical isolates had higher index (0.25) in comparison to food (0.22) and human (0.20) isolates (Table 3). Among the different clinical cases, the isolate from goat abortion case (0.4) had the highest index followed by isolates from buffalo calf diarrhea (0.38), human diarrhea (0.26), cow calf diarrhea (0.21), human pyrexia (0.21) and cow pyrexia (0.2) cases. Isolates from cow wound and human UTI recorded somewhat lower indices. MARI among the food isolates ranged from 0.16 to 0.56.
Among the different serotypes (Table 5) studied for antibiogram, two uncommon serotypes, namely, Labadi and Saintpaul recorded the highest resistance. S. Virchow was another serotype (isolated from buffalo meat) that was resistant to 14 antibiotics. MARI for other serotypes ranged from 0.16 to 0.24. Most serotypes, including Typhimurium were resistant to ampicillin, erythromycin, clindamycin and metronidazole. All S. Paratyphi B Java isolates were resistant to clindamycin and erythromycin, besides metronidazole. Twelve of 14 (85.71%) isolates were also resistant to ampicillin and five (35.71%) were resistant to nalidixic acid. Notably, none of the S. Typhimurium isolates expressed ACSSuT type resistance.
Discussion
An increasing rate of antimicrobial resistance in Salmonella has been reported in many developing and developed countries (Ashtiani et al., 2009) and resistance to combinations of several classes of antimicrobials has led to the emergence of MultiDrug Resistant (MDR) strains (White et al., 2001). In this study, all the Salmonella strains were found to be MDR. Higher frequency of resistance is presumably due to extensive use of antimicrobial agents in human and veterinary medicine (Kikuvi et al., 2010).
All the isolates in this study were resistant to erythromycin and metronidazole. Erythromycin is an old antibiotic belonging to class macrolides that has been used to prevent infections caused by Gram − ve enteric pathogens. Salmonella seems to have acquired resistance against this drug as evident from several studies, where almost 100% resistance have been reported from different parts of world (Harakeh et al., 2005; Khan et al., 2005; Cardoso et al., 2006; Ekwenye and Kazi, 2007; Maripandi and Al-Salamah, 2010). Cell surface hydrophobicity and the presence of active efflux could contribute to the resistance of S. enterica to the antibacterial agents (Braoudaki and Hilton, 2005).
High frequency resistance was also found against clindamycin of lincosamide class (94.59%). The lincosamide is functionally similar but structurally different to macrolide group of antibiotics that all bind to the 50 S ribosomal subunit (Tenson et al., 2003) and a number of genes confer resistance to more than class of antibiotics. Resistance to this drug has been recorded in several studies from different regions (Harakeh et al., 2005; Ekwenye and Kazi, 2007; Maripandi and Al-Salamah, 2010).
Metronidazole, a nitroimidazole derivative, is active against mizroaerophilic and anaerobic bacteria; although it has been reported that facultative anaerobic bacteria such as E. coli may respond to metronidazole, at least under strict anaerobic conditions (Hof et al., 1986). The drug is often used in combination with other antibiotics for treatment of diarrhea, where protozoon infection or deep sited infections such as abscesses is suspected (Randhawa et al., 2006; Hung et al., 2007). All the 37 isolates of Salmonella including the ones isolated from wound infections were found to be resistant against this antibiotic. Hence, use of metronidazole in the treatment of infections due to Salmonella is to be avoided.
High resistance to ampicillin (86.49%) was also recorded in this study. The result was corroborative to the finding of Yu et al. (2011). Therefore, ampicillin should be used with caution for the treatment of Salmonella. This resistance is associated with the presence of ß-lactamases (Cabrera et al., 2004).
Quinolones are broad-spectrum antimicrobial drugs used to treat many clinical infections including salmonellosis. It is used mainly in elderly or immunocompromised patients, but these drugs are also used for treating patients with enteric fever, invasive disease, or long-term salmonellae carriage. Of the seven quinolones (nalidixic acid, ciprofloxacin, levofloxacin, sparofloxacin, moxifloxacin, norfloxacin and ofloxacin) tested in this study, significant resistance was observed only against nalidixic acid (35.10%) and only one isolate showed resistance against sparofloxacin (5.40%). It has been observed that high-level quinolone resistance is uncommon, but reduced susceptibility is increasing (Hopkins et al., 2008). Resistance to nalidixic acid was similar to the ones reported in Vietnam (Vo et al., 2010). However, higher resistance (90% to 96%) to nalidixic acid has been reported from India (Lakshmi et al., 2006), Bhutan (Dahal, 2007) and France (Cailhol et al., 2005). Salmonella resistance to quinolones is usually a consequence of a single point mutation in QRDR of the gyrA gene that encodes the A subunit of DNA gyrase (Threlfall et al., 2002). However, full resistance to quinolones is achieved only when double or more mutations are present concurrently (Su and Chiu, 2007). It appears that isolates tested in this study underwent single mutation only because of which they were resistant to nalidixic acid but not to other antibiotics such as norfloxacin, ciprofloxacin and ofloxacin. Later antibiotics are the drugs of choice for the treatment of invasive human Salmonella infections. Conjugal transfer ability of nalidixic acid resistance determinants posses significant threats through the lateral gene transfer of nalidixic acid resistance determinants to commensal or pathogen bacteria of the human gastrointestinal tract.
Cephalosporins are among the most diverse classes of antibiotics, which are grouped into “generations” by their antimicrobial properties. Each generation has a a broader spectrum of activity than the one before. Third generation cephalosporins are considered drugs of choice for treatment of persons with nontyphoidal Salmonella infections that require chemotherapy or when quinolones are contraindicated (Egorova et al., 2008). However, lately, there has been rise of resistance against cephalosporins among several Salmonella serotypes (Su and Chiu, 2007). In this study, cephalexin and cefotaxime belonging to this group were included. Only two of 37 isolates showed resistance to cephalexin, and all isolates were sensitive to cefotaxime (a third generation cephalosporin). Low levels of resistance to cefotaxime might be attributed to either less use of this third generation cephalosporin in animals and human beings or probably due to its comparatively high cost compared to broad spectrum and cheaper quinolones (Prescot and Baggot, 1993).
All the isolates were found to be sensitive to imipenem and only two isolates were resistant to meropenem of carbapenem group tested in this study. The carbapenems are a class of β-lactam antibiotics with broad spectrum activity and are stable to hydrolysis by extended-spectrum β-lactamase (ESBL)-producing isolates (Sorbera et al., 2002). Though the use of carbapenems is not recommended, they are likely to have a role in the final stage of treatment of quinolone-resistant and ESBL-producing multidrug-resistant salmonellae (Capoor et al., 2009).
Lower resistance to tetracycline was also recorded in this study. Only four isolates, one each from goat and meat and two from buffaloes, were found resistant to this antibiotic. It is surprising because usually high level of resistance has been recorded among Salmonella isolates (Cardoso et al., 2006; Ekwenye and Kazi, 2007; Maripandi and Al-Salamah, 2010). In the United States, resistance to tetracycline increased from 9% in 1980 to 24% in 1990. The changing trend may have been due to ban on the use of tetracycline as a growth enhancer in food producing animals and decrease in its use as a therapeutic agent.
Of the three antibiotics of aminoglycosides group tested in this study, a low degree of resistance was recorded with streptomycin and tobramycin, whereas gentamicin was completely sensitive. Low rate of resistance has also been recorded in European (Threlfall et al., 2003) and African (Cardoso et al., 2006) countries. However, a high rate of resistance against aminoglcosides was recorded among Vietnamese isolates (Vo et al., 2010). Resistance to aminoglycoside antibiotics is often mediated by enzymes that modify those drugs by acetylation, adenylation, or phosphorylation. The corresponding genes are often part of plasmids or transposons (Onyango et al., 2009).
The Salmonella isolates in India have been reported to be 80% to 100% sensitive to chloramphenicol (Mandal et al., 2004; Kumar, 2009)). The present study also showed 100% sensitivity to chloramphenicol. This reemergence of chloramphenicol sensitivity could be attributed to the limited use of the antimicrobial during the last decade in India and in other countries (Shukla and Khan, 2004; Achla et al., 2005; Mohanty et al., 2006; Ekwenye and Kazi, 2007). However, a report by Khan et al. (2005) from Bangladesh showed less sensitivity of Salmonella isolates to chloramphenicol.
Also, in this study, most serotypes were resistant to four to seven antibiotics. Multiple drug resistance against higher number of drugs has been reported in India (Prakash et al., 2005). Emergences of multiple drug resistant Salmonella strains have often been alleged to be responsible for frequently occurring outbreaks and hyperendemicity of salmonellosis in India.
Since the late 1990s, multidrug-resistant S. Paratyphi B dT + has been increasingly isolated from infected persons in different parts of the world. Two types of resistance patterns have been recognized. One type, which is resistant to streptomycin, spectinomycin, trimethoprim, and sulfonamides, is predominantly associated with poultry and poultry products in Germany and the Netherlands. The second type, with resistance to ampicillin, chloramphenicol, streptomycin, spectinomycin, sulfonamides and tetracycline, have been isolated from human cases of gastroenteritis in Canada, the United Kingdom, France and Australia (Levings et al., 2006). Although spectinomycin was not tested in this study, none of isolates demonstrated the above-mentioned two resistant clones. All S. Paratyphi B Java isolates were resistant to clindamycin and erythromycin, besides metronidazole.
Interestingly, none of the S. Typhimurium strains showed ACSSuT resistance pattern, which has been recognized the world over as a major resistance type among S. Typhimurium (Hall, 2010). Thus, it appears that resistance pattern among different serotypes is different among Indian isolates, which may be due to prevalent selection pressure in this region. The study also revealed that animal isolates were more resistant to different antibiotics than meat and human isolates. This indicates that animals act as primary host for the development of antibiotic resistance.
Buffalo farming is a major contributor to the agriculture and livestock industry in many Asian countries through the production of good quality milk, meat and farmyard manure. India largely depends on buffalo for its milk production. Due to ban over cow slaughter in most part of India, buffalo is also used for meat purpose. There are only occasional reports on the occurrence of Salmonella and its antibiotic pattern in buffaloes (Agarwal et al., 1999; Maharjan et al., 2006; Boonmar et al., 2008) and to the best of our knowledge, there is hardly any study dealing with association of Salmonella with clinical infections in this animal. In the present study, antibiogram of four Salmonella isolates belonging to two serotypes viz., Paratyphi B var Java (3) and Saintpaul (1) from buffalo calf diarrhea, revealed them to be multidrug resistant. One isolate was resistant to 15 antibiotics and another to 13 antibiotics, whereas the other two were resistant to four and six antibiotics, respectively. The MARI was 0.38 next only to that of one isolate from a goat abortion case. Cluster analysis also revealed that three of the four isolates formed a single cluster indicating the same clonal lineage. Another cluster had isolates from diverse sources (human, cow, meat, etc.), which indicates that Salmonella probably circulates in different animals and humans; and empirical drug use resulting in emergence of resistant strains in one host might be responsible for similar resistance in other hosts, where the concerned drug is not used. In a contemporary study, isolates from beef (buffalo) had maximum MARI (0.491) in comparison to isolates from other food sources (Kumar, 2009). In another study, S. Stockholm strain isolated from buffalo was found to be resistant to seven drugs (Agarwal et al., 1999). Thus, it appears that buffaloes are acting as melting pot for the emergence of multidrug resistance among Salmonella isolates in India. However, a study in Laos indicated that five buffalo isolates were susceptible to the ten antimicrobials tested (Boonmar et al., 2008). This high sensitivity to most antimicrobial agents in that study was attributed to the unpopularity of using antimicrobial agents as feed additives. Whereas in India, where buffalo is a major dairy and meat animal, the use of antibiotics is quite rampant, which may be a predisposing factor.
The study has provided valuable information in understanding the epidemiology of Salmonella in this part of the world. The development of antimicrobial resistance in Salmonella constitutes a public health risk, as it may potentially affect the efficacy of drug treatment in humans. Therefore, the levels of antibacterial resistance found in this study emphasize that antibiotics must be used judiciously, based on previous resistance tests. The study also revealed changing multidrug resistance pattern and emergence of sensitivity to older drugs. The role of animals in the spread of antibiotic resistance is emphasized. One interesting observation was the higher resistance among buffalo isolates, which calls for a detailed study on the role of buffalo in Salmonella epidemiology. Some of the uncommon serotypes also showed higher resistance, which is a matter of great concern. Legislation to enforce a more prudent use of antibiotics in both human and veterinary medicine should be implemented by the authorities.
References
Achla, P., Grover, S.S., Bhatia, R. and Khare, S., 2005. Sensitivity index of antimicrobial agents as a simple solution for multidrug resistance in Salmonella Typhi. Indian Journal of Medical Research, 121, 185–193.
Agarwal, R.K., Bhilegaonkar, K.N., Singh, D.K., Kumar, Ashok and Rathore, R.S., 2003. Laboratory manual for the isolation and identification of foodborne pathogen. (Indian Veterinary Research Institute, Bareilly).
Agarwal, R.K., Kapoor, K.N., Verma, J.C. and Bachhil, V.N., Singh, B.R., Kumar, A., Sachan, N., Singh, D.K. and Malik, S.V.S., 1999. First report and some properties of Salmonella Stockholm in India, Indian Journal of Comparative Microbiology Immunology and Infectious Diseases, 20, 50–52.
Antony, B., Scaria, B., Dias, M. and Pinto, H., 2009. Salmonella wien from gastroenteritis cases encountered in Mangalore, India: A report of 10 cases and review of the literature. Indian Journal of Medical Science, 63, 195–197.
Ashtiani, M.T., Monajemzadeh, M., Kashi, L., 2009. Trends in antimicrobial resistance of fecal Shigella and Salmonella isolates in Tehran, Iran. Indian Journal of Pathology and Microbiology, 52, 52–55.
Boonmar, S., Markvichitr, K., Chaunchom, S., Chanda, C., Bangtrakulnonth, A., Pornrunangwong, S., Yamamoto, S., Suzuki, D., Kozawa, K., Kimura, H. and Morita Y., (2008). Salmonella prevalence in slaughtered buffaloes and pigs and antimicrobial susceptibility of isolates in Vientiane, Lao People's Democratic Republic. Journal of Veterinary Medical Science, 70, 1345–1348.
Braoudaki, M. and Hilton, A.C., 2005. Mechanisms of resistance in Salmonella enterica adapted to erythromycin, benzalkonium chloride and triclosan. International Journal of Antimicrobial Agents, 25, 31–37.
Cabrera, R., Ruiz, J., Marco, F., Oliveira, I., Arroyo, M., Aladueña, A., Usera, M.A., De Anta, M.T.J., Gascón, J. and Vila, J., 2004. Mechanism of resistance to several antimicrobial agents in Salmonella clinical isolates causing traveler's diarrhea. Antimicrobial Agents and Chemotherapy, 48, 3934–3939.
Cailhol, J., Lailler, R., Bouvet, P., Vieille, S.L., Gauchard, F., Sanders, P. and Brisabois, A., 2005. Trends in antimicrobial resistance phenotypes in non-typhoid Salmonellae from human and poultry origins in France. Epidemiology and Infection, 134, 171–178.
Capoor, M.R., Nair, D., Posti, J., Singhal, S., Deb, M., Aggarwal, P. and Pillai, P., 2009. Minimum inhibitory concentration of carbapenems and tigecycline against Salmonella spp. Journal of Medical Microbiology, 58, 337–341.
Cardoso, M.O., Ribeiro, A.R., dos Santos, L.R., Pilotto, F., Moraes, H.L.S., Salle, C. T.P., Rocha, S.L. Silveira and Nascimento, V.P., 2006. Antibiotic resistance in Salmonella Enteritidis isolated from broiler carcasses. Brazilian Journal of Microbiology, 37, 368–371.
Dahal, N., 2007. Prevalence and antimicrobial resistance of Salmonella in imported chicken carcasses in Bhutan, (Unpublished MSc Thesis, Chiang mai university and Freie universität, Berlin).
Ekwenye, U.N. and Kazi, E., 2007. Investigation of plasmid DNA and antibiotic resistance in some pathogenic organisms. African Journal of Biotechnology, 6, 877–880.
Egorova, S., Timinouni, M., Demartin, M., Granier, S.A., Whichard, J.M. Sangal, V., Fabre, L., Delauné, A., Pardos, M., Millemann, Y., Espié, E., Achtman, M., Grimont, P.A.D. and Weill, F., 2008. Ceftriaxone-resistant Salmonella enterica serotype Newport, France. Emerging Infectious Disease, 14, 954–957.
Farmer, J.J. III., 1995. Enterobacteriaceae: introduction and identification. In: Murray, P.R., Baron, E.J., Pfaller, M.A., Tenover, F.C., Yolken, R.H. (eds), Manual of clinical microbiology, (American Society for Microbiology Press. Washington DC) 438–449.
Guibourdenche, M., Roggentin, P., Mikoleit, M., Fields, P.I., Bockemu¨ J., Grimont, P. A.D. Weill, F-Xavier., 2010. Supplement 2003e2007 (No. 47) to the White-Kauffmann-Le Minor scheme. Research in Microbiology, 161, 26–29.
Hall, R.M. 2010. Salmonella genomic islands and antibiotic resistance in Salmonella enterica. Future Microbiology, 5, 1525–1538.
Harakeh, S., Yassine, H., Gharios, M., Barbour, E., Hajjar, S., El-fadel, M., Toufeili, I. and Tannous, R., 2005. Isolation, molecular characterization and antimicrobial resistance patterns of Salmonella and Escherichia coli isolates from meat-based fast food in Lebanon. Science of the Total Environment, 341, 33–44.
Hoelzer, K., Moreno Switt, A.I. and Wiedmann M., 2011. Animal contact as a source of human non-typhoidal salmonellosis. Veterinary Research, 42, 34.
Hof, H., Stroder, J., Buisson, J and Royer, R., 1986. Effect of different nitroheterocyclic compounds on aerobic, microaerophilic, and anaerobic bacteria. Antimicrobial Agents and Chemotherapy, 30, 679–683.
Hopkins, K.L., Day, M. and Threlfall, E.J., 2008. Plasmid-mediated quinolone resistance in Salmonella enterica, United Kingdom. Emerging Infectious Diseases, 14, 340–342.
Hung, P.H., Chiu, Y.L. and Hsueh, P.R., 2007. Gas-forming splenic abscess due to Salmonella enterica serotype Enteritidis in a chronically hemodialyzed patient. Journal of Microbiology, Immunology and Infection, 40, 276–278.
Kikuvi, G.M., Ombui, J.N. and Mitema, E.S., 2010. Serotypes and antimicrobial resistance profiles of Salmonella isolates from pigs at slaughter in Kenya. Journal of Infections in Developing Countries, 4, 243–248.
Khan, M.F.R., Rahman, M.B., Khan, M.S.R. and Nazir, M.N.H., 2005. Antibiogram and plasmid profile analysis of isolated poultry Salmonella of Bangladesh. Pakistan Journal of Biological Sciences, 8, 1614–1619.
Kulkarni, R.D., Ajantha, G.S, Shubhada, C. and Jain P., 2009. Isolation of Salmonella enterica serotype Isangi from a suspected case of enteric encephalopathy. Indian Journal of Medical Microbiology, 27, 65–66.
Kumar, K., 2009. PCR based detection of zoonotic Salmonella from foods. (Unpublished PhD Thesis, Hemwati Nandan Bahuguna Garhwal Central University, Srinagar, Uttrakhand, India).
Lakshmi, V., Ashok, R., Susmita, J. and Shailaja, V.V., 2006. Changing trends in the antibiograms of Salmonella isolates at a tertiary care hospital in Hyderabad. Indian Journal of Medical Microbiology, 24, 45–48.
Levings, R.S., Lightfoot, D., Hall, R.M. and Djordjevic, S.P., 2006. Aquariums as reservoirs for multidrug-resistant Salmonella Paratyphi B, Emerging Infectious Diseases, 12, 507–510.
Maharjan, M., Joshi, V., Joshi, D.D. and Manandhar, P., 2006. Prevalence of Salmonella species in various raw meat samples of a local market in Kathmandu. Annals of the New York Academy of Science, 1081, 249–256.
Mandal, S., Mandal, M.D. and Pal, N.K., 2004. Reduced minimum inhibitory concentration of chloramphenicol for Salmonella enterica serovar Typhi. Indian Journal of Medical Sciences, 58, 16–23.
Maripandi, A. and Al-Salamah, A.A., 2010. Multiple-antibiotic resistance and plasmid profiles of Salmonella Enteritidis isolated from retail chicken meats. American Journal of Food Technology, 5, 260–268.
Mohanty, S., Renuka, K., Sood, S., Das, B.K. and Kapil, A., 2006, Antibiogram pattern and seasonality of Salmonella serotypes in a north Indian tertiary care hospital. Epidemiology and Infection, 134, 961–966.
Murugkar, H.V., Rahman, H., Kumar, A. and Bhattacharyya, D., 2004. Isolation, phage typing and antibiogram of Salmonella from man and animals in northeastern India. Indian Journal of Medical Research, 122, 237–242.
Nikaido, H., 2009. Multidrug resistance in bacteria. Annual Review of Biochemistry, 78, 119–146.
Onyango, M.D., Ghebremedhin, B., Waindi, E.N., Kakai, R., Rabsch, W., Tietze, E., König, W. and König, B., 2009. Phenotypic and genotypic analysis of clinical isolates Salmonella serovar Typhimurium in western Kenya. Journal of Infections in Developing countries, 3, 685–694.
Paterson, D.L., 2006. Resistance in Gram-negative bacteria. Enterobacteriaceae, American Journal of Medicine. 119, S20-S28.
Prakash, B., Krishnappa, G., Muniyappa L. and Kumar, B.S., 2005. Epidemiological characterization of avian Salmonella enterica serovar infections in India, International Journal of Poultry Science, 4, 388–395.
Prescot, J.F. and Baggot, J.D., 1993. Fluoroquinolones, In: J. F. Prescot and J. D. Baggot (eds), Antimicrobial therapy. In: Veterinary Medicine. 2nd Edn. (Iowa State University Press. Ames) 252–261.
Sirichote, P., Bangtrakulnonth, A., Tianmanee, K., Unahalekhaka, A., Oulai, A., Chittaphithakchai, P., Kheowrod, W., Hendriksen, R.S., 2010. Serotypes and antimicrobial resistance of Salmonella enterica spp in central Thailand, 2001–2006. Southeast Asian Journal of Tropical Medicine and Public Health. 41, 1405–1415.
Shukla, I. and Khan, J.A., 2004. Re-emergence of chloranicol sensitive Salmonella enterica serotype Typhi - a preliminary report. Bionotes, 6, 50.mphe
Sorbera, L.A., Del Fresno, N., Castaner, R.M. and Rabasseda, X., 2002. Faropenem daloxate. Drugs of the Future, 27, 223–233.
Su, L-H. and Chiu, C-H., 2007. Salmonella: Clinical importance and evolution of nomenclature. Chang Gung Medicine Journal, 30, 210–219.
Stevens, M.P., Humphrey, T.J. and Maskell, D.J., 2009. Molecular insights into farm animal and zoonotic Salmonella infections. Philosophical Transactions of the Royal Society B. 364, 2709–2723.
Tenson, T., Lovmar, M. and Ehrenberg, M., 2003 The Mechanism of action of macrolides, lincosamides and streptogramin B reveals the nascent peptide exit path in the ribosome. Journal of Molecular Biology, 330, 1005–1014.
Threlfall, E.J., Clifton-Hadley, F.A., Ridley, A.M., Davies, R.H., 2002. Comparison of gyrA mutations, cyclohexane cesistance, and the presence of class I Integrons in Salmonella enterica from farm animals in England and Wales. Journal of Clinical Microbiology, 40, 1481–1486.
Threlfall, E.J., Fisher, I.S.T., Berghold, C., Gerner-Smidt, P., Tschape, H., Cormican, M., Luzzi, I., Schnieder, F., Wannet, W., Machado, J. and Edwards G., 2003. Antimicrobial drug resistance in isolates of Salmonella enterica from cases of salmonellosis in humans in Europe in 2000: results of international multi-centre surveillance. Eurosurveillance, 8, 41– 45
Vila, J., Gascdn, J., Abdalla, S., Gomez, ]., Moveno, A., Covachlin, M. and Jimenez de Anta, M.T., 2006, Antimicrobial Resistance of Nontyphoidal Salmonella Isolates in Traveler's Diarrhea, Journal of Travel Medicine, 2, 45–47.
Vo, A.T., van Duijkeren, E., Gaastra, W. and Fluit, A.C., 2010. Antimicrobial resistance, class 1 integrons, and genomic island 1 in Salmonella isolates from Vietnam. PLoS One, 5, e9440.
White, D.G., Zhao, S. and Sudler, R., 2001. The isolation of antibiotic resistant Salmonella from retail ground meats. New England Journal of Medicine, 345, 1147–1154.
Yu, F., Chen, Q., Yu, X., Li, Q., Ding, B., Yang, L., Chen, C., Qin, Z., Parsons, C., Zhang, X., Huang, J., Luo, Y., Wang, L. and Pan J., 2011. High prevalence of extended-spectrum beta lactamases among Salmonella enterica Typhimurium isolates from pediatric patients with diarrhea in China. PLoS One, 6, e16801.
Acknowledgement
The authors thank the Director, Indian Veterinary Research Institute, Izatnagar, Bareilly, India for providing facilities to carry out this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, S., Agarwal, R.K., Tiwari, S.C. et al. Antibiotic resistance pattern among the Salmonella isolated from human, animal and meat in India. Trop Anim Health Prod 44, 665–674 (2012). https://doi.org/10.1007/s11250-011-9953-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11250-011-9953-7