Abstract
Primary brain tumors are associated with an increased risk of pulmonary embolism (PE), particularly in the early post-operative period. The pathophysiological mechanisms of PE are poorly understood. This study aims to describe prospectively extracellular vesicles (EVs) levels and investigate whether or not their variations allow to identify patients at increased risk of post-operative PE. Consecutive meningioma or glioma patients candidate to tumor resection were included in the study if a pulmonary perfusion scan (Q-scan) performed before surgery ruled out PE. EVs derived from platelets (CD41+) or endothelial cells (CD144+), tissue factor-bearing EVs (CD142+) and their procoagulant subtype (annexin V+) were analyzed by flow cytometry before surgery (T0), within 24 h (T1), two (T2) and seven days (T7) after surgery. Q-scan was repeated at T2. Ninety-three patients with meningioma, 59 with glioma and 76 healthy controls were included in the study. CD142+ and annexin V+/CD142+ EVs were increased at T0 in meningioma and glioma patients compared to healthy controls. Twenty-nine meningioma (32%) and 16 glioma patients (27%) developed PE at T2. EVs levels were similar in meningioma patients with or without PE, whereas annexin V+ and annexin V+/CD142+ EVs were significantly higher at T1 and T2 in glioma patients with PE than in those without. Procoagulant EVs, particularly annexin V+/CD142+, increase after surgery and are more prevalent in glioma patients who developed PE after surgery than in those who did not.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Patients with brain tumors have an increased risk of post-surgery pulmonary embolism.
-
Patients undergoing meningioma or glioma resection were included in this single-hospital study.
-
Extracellular vescicles levels increased after surgery in glioma patients.
-
Further investigations are needed to elucidate the prognostic role of extracellular vescicles.
Introduction
Venous thromboembolism affects 1–2% of the general population [1] and approximately 10% of patients with cancer [2]. Risk factors for cancer-associated venous thromboembolism include tumor type, surgery, chemotherapy and the use of central venous catheters [3,4,5]. Patients with brain tumors have an increased risk of venous thromboembolism, up to 30%, during the post-operative period [6,7,8,9,10,11,12]. The molecular and cellular bases of this strong association are poorly understood. Brain tumors promote a hypercoagulable state increasing the production and secretion of the hemostatic proteins with a concomitant altered fibrinolytic function [13, 14]. Moreover, alterations of the vascular architecture observed in tumor progression cause endothelial downregulation of the anticoagulant protein thrombomodulin and the upregulation of tissue factor (TF) [15]. These changes shift the haemostatic balance to a procoagulant phenotype. The transmembrane protein TF is not only the primary activator of the extrinsic coagulation cascade, but also promotes tumor growth, angiogenesis and metastasis [16, 17]. It is highly expressed in normal brain tissue [18, 19], which represents the largest repository of TF in the body. Surgical injuries in the peculiar brain vascular architecture exposes TF in plasma, initiating coagulation [20]. In addition to its expression in the vessel wall, TF is associated with cell-derived vesicles named extracellular vesicles (EVs) [21,22,23]. EVs are vesicles of 0.1–1 µm shed from the cell membranes in response to specific stimuli or apoptosis-inducing cell signaling that may lead to a variety of processes including thrombosis, inflammation and vascular dysfunction. [24,25,26,27] EVs circulate in the blood of normal individuals and are qualitatively and quantitatively altered in many diseases [28]. The increased number of TF-bearing EVs in cancer patients has been correlated with the risk of VTE in various settings [29, 30]. Primary brain tumors are an interesting model of investigation because they are associated with a high incidence of post-operative pulmonary embolism (PE) [31], but also to an increased risk of intracranial bleeding [32]. Hence, the identification of patients at high risk of post-operative PE is of pivotal importance to tailor antithrombotic prophylaxis.
With the aim to describe EVs across patients with primary brain tumors and to investigate whether EVs were able to identify patients at high risk of post-operative PE after resection of brain tumors we conducted a single center prospective study in patients with meningioma or glioma.
Methods
Patients
Consecutive adult patients candidate to surgical resection of a primary brain tumor (newly diagnosed or relapsed) from February 2012 to July 2016 at the hospital pre-admission visit were eligible for this prospective study. Inclusion criteria were age > 18 years, patients with meningioma or glioma candidate to surgical resection, availability of a negative pulmonary perfusion scan (Q-scan) within 20 days before surgery. Patients with a positive pulmonary Q-scan before surgery or without a post-operative Q-scan were excluded from the study. Demographic data and a detailed medical history were collected by a trained physician through a standardized questionnaire. Tumor location was classified as skull base or convexity-falx for meningioma and as superficial or deep-seated for glioma. The final diagnosis of tumor type was made on tumor histology on post-operative specimens. WHO grade was adjudicated by an expert pathologist. A second Q-scan was performed 2 days (T2) after surgical tumor resection. A positive Q-scan led to diagnosis of lobar, segmental or sub segmental PE. As standard of care, patients did not receive antithrombotic pharmacological prophylaxis in the first 48 h after surgery, but all of them received mechanical antithrombotic prophylaxis with compression stockings.
A population of healthy controls was selected to compare laboratory parameters. They were partners or friends of patients referred to the Thrombosis Center in the same period of the study for a thrombophilia work-up, with no personal history of thrombosis and without an overt cancer.
All patients and controls gave informed consent to participate to the study which was approved by the Hospital Ethical Committee (Milano Area 2, approval number n 253/12).
Blood sampling, EVs preparation and labelling
Blood samples were obtained before surgery (T0), within 24 h (T1), 2 days (T2) and 7 days (T7) after surgery in patients with meningioma and glioma, and only once in healthy controls. Venous blood was drawn with a 21 gauge needle into 0.109 M sodium citrate vacutainer tubes (BD Biosciences, San Jose, USA) and processed within 2 h.
Platelet free plasma was prepared by double centrifugation (2 × 15 min at 2500 g) at room temperature, as recommended [33, 34]. Aliquots of plasma were immediately frozen and stored at -80 °C until use. Samples were analyzed after thawing at 37 °C. For each analysis 25 µl of freshly thawed platelet free plasma were incubated with a cocktail of properly titrated conjugated monoclonal antibodies, comprising: anti-annexin V (Beckman Coulter, Miami, Fl, USA) which binds phosphatidylserine, anti-CD41-FITC as platelet marker, anti-CD142-PE as TF expressing EVs marker and anti-CD144-PerCp-Cy5.5 as endothelial marker. All monoclonal antibodies were from BD Biosciences. Samples were incubated for 30 min at room temperature in the dark in Hepes buffer (10 mM Hepes, 140 mM NaCl, 4.5 KC, pH 7.4) in the presence of 15 mM CaCl2 and the reaction was stopped with 500 µl of annexin V binding buffer. To prevent coagulation, the calcium-rich buffer contained hirudin (Stago) at a final concentration of 1 AUT/ml in the detection reaction. All the solutions were filtered with a 0.22 µm strainer to limit background noise. Flow-Count fluorospheres (Beckman Coulter) were added to each sample to express EVs counts as absolute numbers.
Flow cytometric analysis
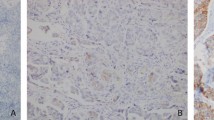
Since the polystyrene beads has a higher refractive index than lipid microvescicles of comparable size, a mix of FITC-fluorescent beads of 0.15, 0.2, 0.24 and 0.5 µm in diameter (Megamix-Plus SSC beads; BioCytex, Marseille, France), covering the major part of the theoretical EVs size range (0.1 to 1 µm), were used to set the threshold in order to determine the SSC vs FSC EVs [35]. Isotype controls were used to determine non-specific binding and autofluorescence within each sample as indicated in the supplemental materials (Figure S1). The following EVs populations were identified: annexin V + EVs expressing phosphatidylserine ( V +), CD142 + EVs expressing TF (CD142+), CD41 + platelet-derived EVs (EVs CD41+) and CD144 + endothelial cell-derived EVs (EVs CD144+). The co-expression of phosphatidylserine with the others surface markers allows to further distinguish some subpopulations of EVs procoagulant compartment: procoagulant-platelet-EVs: V+/CD41+; procoagulant TF-bearing EVs: V+/CD142+) and procoagulant endothelial EVs: V+/CD144+). The gating strategy is shown in the supplemental materials (Figure S1). EVs counts were expressed as absolute numbers (n/μl) and percentages (%). Flow-cytometry acquisition was performed at low flow rate and events were recorded after 10 s from the beginning of the acquisition, to allow sheath flux stabilization. Both acquisition and analysis were performed on a FACSCanto II flow cytometer equipped by FACSDiva software version 6.2 (BD Biosciences).
Statistical analysis
Means and standard deviations or medians and inter-quartile ranges were used to describe continuous variables. Counts and percentages were used for categorical variables. Patients with PE were compared to those without in meningioma and glioma patients. The Q-scans at T2 that did not allow certain diagnosis of PE were considered negative in the main analysis. Non-parametric Mann–Whitney U test was used to compare means between groups for non-normally distributed data and paired sample t-test was used to determine differences between repeated measures (T0, T1, T2, T7). Cut-off values for high levels of EVs were set arbitrarily at the 75th percentile of EVs distribution values among patients without PE. All analyses were performed with the statistical software SPSS (release 25.0, IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, USA).
Results
One hundred and seventy-two patients were screened for the study and 152 patients met the inclusion criteria. Five patients missed the pre-operative Q-scan, 2 patients missed the post-operative Q-scan and in one patient surgery was not performed. Twelve patients (7.9%) were excluded for a positive Q-scan at baseline. Hence, 93 patients with meningioma (of whom 12 relapsed patients) and 59 with glioma (all newly diagnosed) were finally evaluated. Table 1 shows the general characteristics of the two groups of patients. The vast majority of meningioma patients had WHO grade 1 histology, 73% located at the convexity and 27% at the skull base. More than half of glioma patients had WHO grade 4, 64% deep seated and 36% superficial (located at less than 1 cm from the surface of the cortex). Radical resection was achieved in 96% of patients.
Q-scan was positive at T2 in 29 meningioma patients (31%) and in 16 glioma patients (27%). All PE were asymptomatic, 26 segmental and 19 subsegmental, 26 (58%) multiple. Meningioma patients with PE were younger, whereas glioma patients were older than those without, and no difference in terms of sex, body mass index, hemoglobin, platelet count, white blood cell count and histology was observed (Table 2). Among 16 glioma patients with PE, 15 (94%) had WHO grade 4 and the remaining one had WHO grade 3 histology.
Three patients (3%) with meningioma and 5 (8%) with glioma had bleeding complications after tumor resection, all requiring surgical attention.
Seventy-six healthy controls were evaluated to establish the EVs reference values. In both meningioma and glioma patients at T0 numbers of CD142+ and V+/CD142+ were higher (p-value < 0.01) while CD144 + and V+/CD144+ were lower than in healthy controls (p value < 0.01), the mean values of meningioma, glioma and healthy controls for each EVs population are shown in Table 3. No difference was observed between meningioma and glioma EVs levels at baseline. When EVs levels of patients with or without PE were compared, there was no differences in meningioma patients but glioma patients with PE showed increased levels of V+ at T1 (p = 0.027) and CD142+ at T2 (p = 0.015) and T7 (p = 0.05) (Fig. 1). The representative plots of flow cytometry in glioma patients are shown in the supplemental Figure S2. Considering mean values of the percentage of co-stained EVs, representing the procoagulant subset, on the total EVs of the same subtype (EVs%) among patients with or without PE, we found no differences in meningioma patients, but at T1 in glioma patients (52% vs 34%, p = 0.037). The prevalence of high levels of EVs was similar among meningioma patients with or without PE. At T0 the prevalence of high levels of CD142+, V+/CD142+ and V+/CD144+ was higher (46% vs 25%) in patients with PE than in those without. These subsets of EVs showed a further increased prevalence at T1. The prevalence of high levels of EVs in patients with PE decreased at T2 for all EVs subsets, except for V+ and CD142+. The sensitivity of high levels of EVs to detect PE also in glioma patients remained low, and the best positive predictive value was 40% for high levels of V + /CD142 + EVs at T1.
Discussion
PE after neurosurgery is a frightening complication because of the bleeding risk associated with anticoagulant treatment, even at prophylactic doses [32]. This study was aimed to describe different subtypes EVs in a population of patients with primary brain tumor and to detect a possible promising biomarker that may help clinicians to identify patients at increased risk of post-operative PE. We confirm our[31] and others[36] previous observations that surgery for meningioma or glioma is an important risk factor for PE, that occurs in one third of patients in the early post-operative period. We observed that the higher the grade of glioma, the higher the probability to develop PE, with all but one event occurred in WHO grade IV tumors. The prospective design and the exclusion of patients with a positive Q-scan before surgery, make us confident that PE events were surgery-related. Patients with both meningioma and glioma had higher baseline circulating V+/CD142+ than healthy individuals. Among patients who developed PE after tumor resection, high levels of EVs were more prevalent in glioma than in meningioma patients. In the former, particularly procoagulant EVs expressing phosphatidylserine and other surface markers as TF, one of the main blood coagulation activators, are prevalent. Phosphatidylserine is one of the activator of TF that, interacting with FVII, initiates the extrinsic coagulation pathway [37]. Also procoagulant EVs derived from endothelial cells were increased before and after glioma resection. One may speculate that the vascular damage caused by tumor resection triggers the release of EVs from both the tumor and the vascular wall. However, our data support this hypothesis only for malignant tumors as gliomas.
Circulating EVs are increased in various diseases associated with thrombotic complications such as diabetes, inflammation, vascular diseases and cancer [28]. High baseline levels of EVs in glioma patients have been associated with a fourfold increased risk of VTE in a 7-month follow-up period, with two thirds of events occurred in the first post-operative week. However, the absence of a pre-operative objective investigation to rule out a pre-existing event makes these results uncertain [38]. Moreover, high baseline EVs levels have also been associated with early tumor recurrence and short survival in newly diagnosed glioma patients [37, 39, 40].
Although strengths of our study are the prospective design, the large number of patients included and the requirement of a negative pre-operative Q-scan, some limitations need to be discussed. First, we did not discriminate the origin of the TF-bearing EVs with cell of origin specific markers; V+/CD142+ can originate from tumor cells, activated leucocytes or platelets. Second, the low refractive index of EVs and the inability to identify EVs smaller than 500 nm on the adopted flow cytometer,caused difficulties in distinguishing them. This may have led to an underestimation of V+/CD142+ levels and a consequent low sensitivity of high levels of EVs to predict the risk of PE. Third, the short observational period did not allow us to assess the impact of EVs levels or post-operative PE on patients survival, as already demonstrated for such other vascular biomarkers as circulating endothelial cells [37]. Fourth, despite the incidence of PE was similar in glioma and meningioma patients, in the latter we did not find an association between high EVs levels and the disease, and other biomarkers remain to be investigated. Whether the risk of PE is associated with high EVs levels at least in malignant tumors remains to be confirmed, as well as the validity of EVs as a predictive biomarkers of PE. We speculate that other mechanisms, possibly non EVs-mediated could be involved, but the answer to this question is beyond the scope of the present work. Regarding the role of WBC-derived EVs it is of note that CD142 + EVs are mainly of WBC origin, and in glioma patients with PE are high.
In conclusion, high levels of EVs at the first post-operative day were more prevalent in glioma than in meningioma patients, particularly in those who developed PE.. Further investigations are needed to elucidate the prognostic role of EVs.
References
Fowkes FJI, Price JF, Fowkes FGR (2003) Incidence of diagnosed deep vein thrombosis in the general population: systematic review. Eur J Vasc Endovasc Surg 25:1–5
Khorana AA, Francis CW (2018) Risk prediction of cancer-associated thrombosis: appraising the first decade and developing the future. Thromb Res 164:S70–S76
Sheth RA, Niekamp A, Quencer KB, Shamoun F, Knuttinen MG, Naidu S, Oklu R (2017) Thrombosis in cancer patients: etiology, incidence, and management. Cardiovasc Diagn Ther 7:S178–S185
Petterson TM, Marks RS, Ashrani AA, Bailey KR, Heit JA (2015) Risk of site-specific cancer in incident venous thromboembolism: a population-based study. Thromb Res 135:472–478
Baumann Kreuziger L, Jaffray J, Carrier M (2017) Epidemiology, diagnosis, prevention and treatment of catheter-related thrombosis in children and adults. Thromb Res 157:64–71
Walsh DC, Kakkar AK (2001) Thromboembolism in brain tumors. Curr Opin Pulm Med 7:326–331
Magnus N, D’Asti E, Garnier D, Meehan B, Rak J (2013) Brain neoplasms and coagulation. Semin Thromb Hemost 39:881–895
Gerber DE, Grossman SA, Streiff MB (2006) Management of venous thromboembolism in patients with primary and metastatic brain tumors. J Clin Oncol 24:1310–1318
Perry JR (2012) Thromboembolic disease in patients with high-grade glioma. Neuro-Oncology 14:73–80
Jenkins EO, Schiff D, Mackman N, Key NS (2010) Venous thromboembolism in malignant gliomas. J Thromb Haemost 8:221–227
Hoefnagel D, Kwee LE, Van Putten EHP, Kros JM, Dirven CMF, Dammers R (2014) The incidence of postoperative thromboembolic complications following surgical resection of intracranial meningioma. A retrospective study of a large single center patient cohort. Clin Neurol Neurosurg 123:150–4
Rinaldo L, Brown DA, Bhargav AG, Rusheen AE, Naylor RM, Gilder HE, Monie DD, Youssef SJ, Parney IF (2020) Venous thromboembolic events in patients undergoing craniotomy for tumor resection: incidence, predictors, and review of literature. J Neurosurg 132:10–21
Sawaya R, Ramo OJ, Glas-Greenwalt P, Wu SZ (1991) Plasma fibrinolytic profile in patients with brain tumors. Thromb Haemost 65:15–19
Cote DJ, Smith TR (2016) Venous thromboembolism in brain tumor patients. J Clin Neurosci 25:13–18
Moore KL, Andreoli SP, Esmon NL, Bang NU (1987) Endotoxin enhances tissue factor and suppresses thrombomodulin expression of human vascular endothelium in vitro. J Clin Invest 79:124–130
Grover SP, Mackman N (2018) Tissue factor: an essential mediator of hemostasis and trigger of thrombosis. Arterioscler Thromb Vasc Biol 38:709–725
Van Den Berg YW, Osanto S, Reitsma PH, Versteeg HH (2012) The relationship between tissue factor and cancer progression: insights from bench and bedside. Blood 119:924–932
Eddleston M, De La Torre JC, Oldstone MBA, Loskutoff DJ, Edgington TS, Mackman N (1993) Astrocytes are the primary source of tissue factor in the murine central nervous system: a role for astrocytes in cerebral hemostasis. J Clin Invest 92:349–358
Drake TA, Morissey JH, Edgington TS (1989) Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am J Pathol 134:1087–97
Del Zoppo GJ, Izawa Y, Hawkins BT (2013) Hemostasis and alterations of the central nervous system. Semin Thromb Hemost 39:856–875
Key NS (2010) Analysis of tissue factor positive microparticles. Thromb Res 125:1–9
Hron G, Kollars M, Weber H, Sagaster V, Quehenberger P, Eichinger S, Kyrle PA, Weltermann A (2007) Tissue factor-positive microparticles: cellular origin and association with coagulation activation in patients with colorectal cancer. Thromb Haemost 97:119–123
Tawil N, Bassawon R, Rak J (2019) Oncogenes and clotting factors: the emerging role of tumor cell genome and epigenome in cancer-associated thrombosis. Semin Thromb Hemost 45:373–384
Falanga A, Russo L, Milesi V, Vignoli A (2017) Mechanisms and risk factors of thrombosis in cancer. Crit Rev Oncol Hematol 118:79–83
Lacroix R, Dubois C, Leroyer AS, Sabatier F, Dignat-George F (2013) Revisited role of microparticles in arterial and venous thrombosis. J Thromb Haemost 11:24–35
Zarà M, Guidetti GF, Camera M, Canobbio I, Amadio P, Torti M, Tremoli E, Barbieri SS (2019) Biology and role of extracellular vesicles (EVs) in the pathogenesis of thrombosis. Int J Mol Sci 20:2840
Kalluri R, LeBleu VS (2020) The biology, function, and biomedical applications of exosomes. Science (-80) 367:6977
Enjeti AK, Lincz LF, Seldon M (2008) Microparticles in health and disease. Semin Thromb Hemost 34:683–691
Geddings JE, Mackman N (2013) Tumor-derived tissue factor-positive microparticles and venous thrombosis in cancer patients. Blood 122:1873–1880
Gardiner C, Harrison P, Belting M, Böing A, Campello E, Carter BS, Collier ME, Coumans F, Ettelaie C, Van Es N, Hochberg FH, Mackman N, Rennert RC, Thaler J, Rak J, Nieuwland R (2015) Extracellular vesicles, tissue factor, cancer and thrombosis—discussion themes of the ISEV 2014 educational day. J Extracell Vesicles 4:1–14
Carrabba G, Riva M, Conte V, Di Cristofori A, Caroli M, Locatelli M, Castellani M, Bucciarelli P, Artoni A, Stocchetti N, Martinelli I, Rampini P (2018) Risk of post-operative venous thromboembolism in patients with meningioma. J Neurooncol 138:401–406
Algattas H, Damania D, DeAndrea-Lazarus I, Kimmell KT, Marko NF, Walter KA, Vates GE, Jahromi BS (2018) Systematic review of safety and cost-effectiveness of venous thromboembolism prophylaxis strategies in patients undergoing craniotomy for brain tumor. Neurosurgery 82:142–154
Poncelet P, Robert S, Bailly N, Garnache-Ottou F, Bouriche T, Devalet B, Segatchian JH, Saas P, Mullier F (2015) Tips and tricks for flow cytometry-based analysis and counting of microparticles. Transfus Apher Sci 53:110–126
Artoni A, Merati G, Padovan L, Scalambrino E, Chantarangkul V, Tripodi A (2012) Residual platelets are the main determinants of microparticles count in frozen-thawed plasma. Thromb Res 130:561–562
Chandler WL, Yeung W, Tait JF (2011) A new microparticle size calibration standard for use in measuring smaller microparticles using a new flow cytometer. J Thromb Haemost 9:1216–1224
Koopmans RJ, Cannegieter SC, Koot RW, Vleggeert-Lankamp CLA. Nadroparin plus compression stockings versus nadroparin alone for prevention of venous thromboembolism in cerebellopontine angle tumour excisions: a cohort study. Thromb Haemost 2020; .
Reynés G, Vila V, Fleitas T, Reganon E, Font de Mora J, Jordá M, Martínez-Sales V (2013) Circulating endothelial cells and procoagulant microparticles in patients with glioblastoma: prognostic value. PLoS ONE 8:4–8
Sartori MT, Della Puppa A, Ballin A, Saggiorato G, Bernardi D, Padoan A, Scienza R, D’Avella D, Cella G (2011) Prothrombotic state in glioblastoma multiforme: an evaluation of the procoagulant activity of circulating microparticles. J Neurooncol 104:225–231
Sartori MT, Della Puppa A, Ballin A, Campello E, Radu CM, Saggiorato G, d’Avella D, Scienza R, Cella G, Simioni P (2013) Circulating microparticles of glial origin and tissue factor bearing in high-grade glioma: a potential prothrombotic role. Thromb Haemost 110:378–385
Evans SM, Putt M, Yang XY, Lustig RA, Martinez-Lage M, Williams D, Desai A, Wolf R, Brem S, Koch CJ (2016) Initial evidence that blood-borne microvesicles are biomarkers for recurrence and survival in newly diagnosed glioblastoma patients. J Neurooncol 127:391–400
Funding
The authors disclosed receipt of the following financial support for the research: this work was supported by the Italian Ministry of Health [grant number RF-GR- 2011–02347854].
Author information
Authors and Affiliations
Contributions
All the authors read, revised and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the Authors has conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Passamonti, S.M., Artoni, A., Carrabba, G. et al. Plasma levels of extracellular vesicles and the risk of post-operative pulmonary embolism in patients with primary brain tumors: a prospective study. J Thromb Thrombolysis 52, 224–231 (2021). https://doi.org/10.1007/s11239-021-02441-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02441-3