Abstract
Even though there are several reversal strategies available for oral Factor Xa inhibitor associated coagulopathies, 4-factor prothrombin complex concentrate (4F-PCC) is used commonly as the primary reversal agent at many institutions. A dose of 50 units/kg is recommended as safe and effective with growing data suggesting that a lower dosing strategy may be sufficient. This retrospective study included adult patients who received either high-dose (50 units/kg; maximum dose: 5000 units) or low-dose (25 units/kg; maximum dose: 2500 units) 4F-PCC for the emergent reversal of oral Factor Xa inhibitor-related life threatening bleeding. The primary outcome was the attainment of hemostatic effectiveness. Secondary outcomes were rates of thromboembolic events and inpatient mortality. 47 patients were included in the analysis of which 24 patients received high-dose and 23 patients received low-dose 4F-PCC. Overall hemostatic effectiveness was 87.5% in the high-dose group and 91.3% in the low-dose group. Thromboembolic event rate was 8.3% in the high-dose group compared to 4.4% within the low-dose group and inpatient mortality rate was 8.3% in the high-dose group and 4.4% in the low-dose group. Low-dose 4F-PCC (25 units/kg, maximum dose: 2500 units) for the reversal of oral Factor Xa inhibitors is a cost-effective alternative to high-dose 4F-PCC (50 units/kg; maximum dose: 5000 units) and provides effective hemostasis without increased rates of thromboembolic events or inpatient mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
4-Factor prothrombin complex concentrate (4F-PCC) is used commonly as the primary reversal agent for oral Factor Xa inhibitors.
-
Recent literature supports use of lower dosing strategy such as 25 units/kg instead of 50 units/kg of 4F-PCC.
-
The current study evaluates efficacy, safety, and cost-implications of a lower dosing strategy of 25 units/kg of 4F-PCC.
-
Based on the outcomes presented, 25units/kg (max dose: 2500 units) of 4F-PCC is a safe and effective dose for oral Factor Xa inhibitors-related life threatening bleed and is associated with significant cost-saving compared to 50 units/kg. Future, larger studies are required to confirm these findings.
Introduction
Anticoagulation-associated bleeding is one of the most common causes of outpatient drug event-related emergency department (ED) visits resulting in hospital admissions [1]. The most commonly prescribed outpatient anticoagulants are warfarin and oral Factor Xa inhibitors such as rivaroxaban (Xarelto®) and apixaban (Eliquis®). The increasing use of oral Factor Xa inhibitors has coincided with an overall decrease in the use of warfarin due to its many limitations including numerous drug interactions, the need for routine lab monitoring, and the potential for higher bleeding risks compared to oral Factor Xa inhibitors. Additionally, there continue to be increasing guideline endorsements of the use of oral Factor Xa inhibitors in non-valvular atrial fibrillation and venous thromboembolism [2, 3].
As with any anticoagulant, life threatening bleeding is a significant concern directly associated with the use of oral Factor Xa inhibitors and requires timely and effective reversal [4]. Until the introduction of the oral Factor Xa inhibitor-specific antidote andexanet alfa in 2018, 4-factor prothrombin complex concentrate (4F-PCC) and activated PCC (aPCC) were routinely used for the reversal of oral Factor Xa inhibitors. Supporting evidence for the use of 4F-PCC and aPCC came from studies in animal models, healthy volunteers, and case series along with retrospective and prospective studies [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Even though different formulations of PCC were used in these studies, based on the available data and overall benefit seen, PCC was recommended as the reversal agent of choice in the 2017 American College of Cardiology (ACC) guidelines and the 2015 Neurocritical Care guidelines [20, 21]. After the introduction of the FDA approved reversal agent andexanet alfa, 2020 ACC guidelines were updated to recommend andexanet alfa as first line for oral Factor Xa inhibitor reversal and 4F-PCC or aPCC to be used if andexanet alfa is unavailable [22]. In spite of the FDA approval and guideline recommendation, many institutions still continue to use 4F-PCC or aPCC as reversal agents due to significant cost implications of andexanet alfa with the added uncertainty of its benefit compared to PCC alternatives. The uncertainty of its benefits is driven by the limitations of the approval study including but not limited to the open-label, single arm study design and exclusion of patients with severe bleeding [23]. Recently a multi-center, retrospective, observational cohort study evaluating the use of PCCs for the reversal of oral Factor Xa inhibitors related intracranial hemorrhage (ICH) was published which showed that PCCs had a high rate of excellent or good hemostasis (81.8%) along with a low rate of thrombosis (3.8%) [24]. In this study, 77.5% of patients received 4F-PCC at a median initial dose of 43.8 units/kg and the rest of the patients were treated with aPCC at a median initial dose of 26.7 units/kg.
The dosing of 4F-PCC in many of the original studies was 50 units/kg of factor IX, rounded to the nearest available vial size. Recently published studies have shown that 25 units/kg dosing has also provided adequate hemostasis [9,10,11,12,13,14,15,16,17,18,19]. Based on the available evidence, our hospital’s Pharmacy and Therapeutics committee approved a lower dosing strategy of 4F-PCC for oral Factor Xa inhibitor reversal in the management of life-threatening bleeds or emergent surgery. Kcentra® is the preferred 4F-PCC at our institution and the dosing was modified from 50 units/kg (maximum dose: 5000 units) to 25 units/kg (maximum dose: 2500 units). In the new protocol, a repeat dose of 25 units/kg (maximum dose: 2500 units) could be given if satisfactory reversal was not achieved with the initial dose.
Although there have been published studies showing individual outcomes of 25 units/kg and 50 units/kg of 4F-PCC, to the best of our knowledge there have been no studies directly comparing these dosing strategies with regards to safety and efficacy.
Methods
Study population
This is a single-center, retrospective cohort study conducted to compare the efficacy and safety of two different doses of 4F-PCC (Kcentra®) in the reversal of oral Factor Xa inhibitor-related life threatening bleeding—25 units/kg (low-dose group) and 50 units/kg (high-dose group). Patients receiving 4F-PCC were identified by an independent search of all orders for its use in the electronic medical record. This was an unfunded, institutional review board approved analysis conducted at a community hospital with comprehensive stroke center and level 2 trauma designations.
All adult patients (≥ 18 years of age) who received 4F-PCC for oral Factor Xa inhibitor reversal between January 2018 and February 2020 for life-threatening bleeding were included in the study. Life threatening bleeding was defined as ICH, bleeding into a critical site (such as pericardial, retroperitoneal, splenic hemorrhage), or bleeding that causes persistent hemodynamic compromise (ie, systolic blood pressure <90 mmHg or mean arterial pressure <65 mmHg) requiring treatments such as blood-product resuscitation and/or vasopressors.
The patients in the study were pre- and post-guideline change. The high-dose group consisted of patients who received a treatment dose of 50 units/kg (maximum dose: 5000 units) per the institution’s original reversal guidelines. The low-dose group consisted of patients who were treated according to the modified dosing protocol of 25 units/kg (maximum dose: 2500 units). A repeat dose of 25 units/kg (maximum dose: 2500 units) could be given if satisfactory reversal was not achieved with the initial dose. Doses were rounded to the nearest vial size per institutional practice. Patients who received 4F-PCC for indications other than oral Factor Xa inhibitor reversal for life threatening or severe bleeding, patients who received doses other than the 25 or 50 units/kg, patients who were transferred to another facility for further care, and pregnant patients were excluded.
Outcomes
The primary objective was to compare the hemostatic effectiveness between the low-dose group and the high-dose group. The primary efficacy outcome was the percentage of patients with excellent or good hemostasis as defined by the modification of criteria developed by Sarode et al and previously used in other studies [23,24,25,26]. Among patients with ICH, the level of hemostasis achieved was based on the largest hematoma expansion from the baseline CT scan. Excellent hemostasis was attained if the hematoma volume grew by 0–20.0%, good hemostasis if the increase was 20.1–35.0%, and poor hemostasis if the increase was >35.0% compared to baseline. For intraparenchymal hemorrhage, ABC/2 formula was used. For subarachnoid and subdural hemorrhage, the percent increase from maximum thickness of the densest area on the repeat CT was used. These measurements were done manually by a physician and a neurosurgery advanced practice nurse. Among patients with gastrointestinal bleeding (GIB) or other non-visible bleeding, hemostasis was based on the percent decrease in both hemoglobin/hematocrit (Hb/Hct) at 24 h compared with baseline while taking into account blood product usage. Further details of the criteria used are outlined in Table 1.
Secondary objectives were to compare the rates of thromboembolic events and inpatient mortality between both groups. Thromboembolic events were defined as deep vein thrombosis (DVT), pulmonary embolism (PE), ischemic stroke, or myocardial infarction (MI) that occurred during admission or up to 30 days after the administration of 4F-PCC based on available documentation from repeat visits per EMR. Inpatient mortality was defined to include patients with documented inpatient death during their admission. Hospice was excluded from the definition of inpatient mortality due to the inability of the study investigators to follow the outcomes of patients that were discharged to outpatient settings. Differences in the cost of 4F-PCC, length of stay, and discharge disposition were also evaluated with the allocation of hospice as a disposition category in order to identify possible differences between both groups.
Statistical analysis
Demographics are presented with means and standard deviations (SD) or medians and interquartile ranges (IQR) as applicable for continuous variables, and as proportions and absolute numbers for categorical variables. Descriptive analysis was used to present outcomes within the dosing groups. Analyses were completed using SAS statistical package (release 9.4; SAS Institute Inc, Cary, NC).
Results
Baseline characteristics
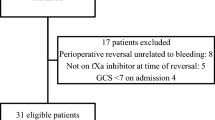
A total of 121 patients were screened and 47 were eligible for inclusion (Fig. 1). 24 patients were included in the high-dose group and 23 patients in the low-dose group (Table 2). Patients were similar in age [81 years (IQR: 72–86) high-dose; 82 years (IQR: 73–88) low-dose] and sex (45.8% female high-dose; 56.5% female low-dose) between the high and low dose groups. The most common anticoagulant reversed was apixaban (66.7% high-dose; 82.6% low-dose). The majority of patients received 4F-PCC for ICH (70.8% high-dose; 73.9% low-dose). There was a higher median ICH volume in the high-dose group compared to low-dose group. Glasgow coma scale (GCS) was only documented in about half of the ICH patients in both groups and there was no difference between the groups. Additional hemostatic agents administered included desmopressin and vitamin K.
Hemostatic effectiveness, thrombotic events, and inpatient mortality
Table 3 shows the rates of primary and secondary outcomes among both high- and low-dose groups. Percentage of patients that met criteria for excellent or good overall hemostasis was higher in the low-dose group compared to high-dose (87.5% high-dose, 91.3% low-dose). Thromboembolic events and inpatient mortality were lower in the low-dose group (8.3% high-dose, 4.4% low-dose for both data points). Length of stay was similar between both groups (6 days high-dose, 5 days low-dose). More patients in the low-dose group had a discharge disposition of home or hospice, while a higher proportion of patients in the high-dose group needed admission to a skilled nursing facility. With regards to hemostasis, three patients in the high-dose group and two patients in the low-dose group experienced worsening bleeds after the administration of 4F-PCC. None of the patients with worsening bleed received a second dose of 4F-PCC. Thromboembolic events occurred in two patients in the high-dose group and one patient in the low-dose group. One patient in the high-dose group suffered from both a DVT and PE 15 days after the administration of 4F-PCC and the second patient suffered from a DVT 3 days after 4F-PCC. Among patients who received low-dose, one patient suffered from a DVT within 2 days of 4F-PCC administration.
Table 4 shows the proportion of patients with hemostatic effectiveness stratified by bleed type and Table 5 lists the blood product usage within both groups before and after treatment with 4F-PCC. Among patients with ICH, good or excellent hemostasis was achieved in 88.2% of patients in the high-dose group and 100.0% of patients in the low-dose group. Hemostasis within the GI bleed group was sub-optimal in the low-dose group compared to high-dose (80% high-dose, 33.3% low-dose). Patients with non-ICH, non-GI bleed had 100.0% hemostatic efficacy in both groups. Two patients in the high-dose group with ICH had poor hemostasis with > 35% increase in hematoma volume on the repeat CT scan. One patient with a GI bleed in the high-dose group had poor hemostasis as evidenced by the need for more than 2 units of blood products after the initial treatment with 4F-PCC and blood products. Two patients with GI bleed within the low-dose group had poor hemostasis since they met the criteria of > 20% reduction in Hb/Hct from baseline. One of these patients had no obvious bleeding after 4F-PCC at the time of direct visualization during esophagogastroduodenoscopy (EGD) despite the Hb drop. The other patient needed interventional radiology (IR) embolization to control the bleed. None of the patients with worsening bleeds experienced an inpatient death and were discharged to home or a skilled nursing facility in stable condition.
Treatment cost
Based on the average wholesale price (AWP) of 4F-PCC (Kcentra®), the median cost of treatment was $6765 in the high-dose group and $3663 in the low-dose group leading to a cost saving of $3102 per patient. This is in stark contrast to the cost of andexanet alfa (Andexxa®). Per package insert, a low-dose regimen (total dose 880 mg) should be used for patients on apixaban ≤ 5 mg or rivaroxaban ≤ 10 mg if taken within 8 h and a high-dose regimen (total dose 1760 mg) should be used for patients on apixaban > 5 mg or rivaroxaban > 10 mg or an unknown dose taken within 8 h or at an unknown time [23, 27]. At an AWP of $5335 per 200 mg this leads to a total cost of $23,474 for the-low dose regimen and $46,948 for the high-dose regimen.
Discussion
This study compared 50 units/kg (high-dose) 4F-PCC with 25 units/kg (low-dose) 4F-PCC in the emergent reversal of oral Factor Xa inhibitors and found an overall hemostatic effectiveness rate of 87.5% in the high-dose group and 91.3% in the low-dose group.
While 4F-PCC remains “off-label” for the reversal of oral Factor Xa inhibitors, previously reported data show it to be an effective reversal agent. Santibanez et al performed a retrospective study of 4F-PCC administration in a diverse subset of patients (e.g., oral Factor Xa inhibitors and warfarin reversals, LVAD explants to heart transplants, massive transfusions, etc.) and found that hemostatic effectiveness was attained with greatest incidence among oral Factor Xa inhibitors patients at 78.9% using their institutional dosing of 25 units/kg [19]. As this dose was lower than the recommended dosing put forth by consensus guidelines, the authors concluded that a lower dose may be reasonable for this patient population.
Majeed et al conducted a prospective cohort study assessing the use of 4F-PCC in the management of rivaroxaban- or apixaban-associated major bleeding and found that the use of a median 4F-PCC dose of 27 units/kg (2000 units) resulted in 69.1% hemostatic effectiveness [12]. An observational multicenter cohort study conducted by Schulman et al also assessed the use of 4F-PCC at a mean dose of 26 units/kg (2077 units) for the reversal of rivaroxaban- or apixaban- associated major bleeding and found that good hemostasis was attained in 65% of patients and moderate hemostasis was attained in 20% of patients. They found that 8% of patients experienced a thromboembolic event within 1–22 days of receiving 4F-PCC [11]. A retrospective study by Berger et al using low-dose 4F-PCC for oral Factor Xa inhibitor-associated intracranial hemorrhage showed a 94.7% hemostasis with a 9% of risk of thromboembolism [17] .
Our study is a real-world descriptive analysis of 4F-PCC practices at a community hospital. The rates of hemostatic effectiveness and thromboembolic complications in this study are comparable to other studies evaluating the use of 4F-PCC for oral Factor Xa inhibitor reversal. The hemostasis rates in those studies ranged from 68 to 95% and the thrombotic events ranged from 0 to 13% [11,12,13,14,15,16,17,18,19]. The mortality rates reported in previous studies ranged from 16 to 32% which is higher than the inpatient mortality rates reported in this study. These differences may be attributable to the ways in which each study defines mortality. The presence of a comparator group in our study supports the independent correlations of hemostatic effectiveness, thromboembolic, and mortality rates with 4F-PCC administration.
Limitations of this study include the retrospective nature of this single-center study, the pre-post institutional protocol design, and the small sample size necessitating further studies with larger sample sizes to confirm these hypothesis generating findings. Since all data were extracted from electronic medical record, the information is limited to what was available to the investigators through chart review thus precluding inclusion of any clinically relevant information if the patient sought care at a different institution post-discharge. We also did not analyze or compare other baseline medical conditions that could have contributed to the outcomes of these patients. Even though majority of the patients had reported their last apixaban or rivaroxaban dose to be within 24 h of presentation and while checking anti-Factor Xa levels is not a standard at many institutions, inability to confirm the presence of anticoagulant is a limitation. Also, only a small proportion of patients were on rivaroxaban and no patients were on edoxaban limiting the generalizability of our study to those specific groups. Additionally, median ICH volume was higher in the high-dose group, raising the possibility that ICH patients in the high-dose group were sicker at baseline. This may explain the lower percentage of hemostatic effectiveness attained within the high-dose ICH subgroup compared to the low-dose ICH subgroup. It is also possible that low-dose of 4F-PCC may not be appropriate for patients with higher volume bleeds. This study also had a small proportion of ICH patients undergoing neurosurgery thus limiting the extrapolation of the results to that population. Baseline GCS was not documented in all patients with ICH, which is another limitation with this study.
The percentage of hemostatic efficacy for reversal of GI bleed within the low-dose strategy could be considered sub-optimal at 33.3%. The sample size of patients with GI bleed was very small in this study. There were only three patients with GI bleed in the low-dose group and two patients were categorized as achieving poor hemostasis. Out of the two, one patient had attained hemostasis per EGD report but did have a drop in hemoglobin. The second patient needed IR embolization to control bleed. No repeat doses of 4F-PCC were given to any patients with worsening bleeds in the low-dose group despite the modified institutional reversal guideline allowing for one more dose in worsening bleeds. This may have been either due to lack of familiarity with the repeat dosing strategy or due to perceived futility with further treatment.
This real-world experience comparing 25 units/kg to 50 units/kg of 4F-PCC for oral Factor Xa inhibitor reversal suggests that the administration of 25 units/kg is a safe and cost-effective alternative to 50 units/kg of 4F-PCC, with median cost savings per patient of $3102. Further studies are needed to confirm these findings.
Conclusion
Institutions have varying approaches for the reversal of oral Factor Xa inhibitor related bleeding. Presented here is an experience with two different dosing strategies of 4F-PCC for oral Factor Xa inhibitor reversal. Patients who received the 25 units/kg dosing of 4F-PCC for oral Factor Xa inhibitor reversal had good hemostasis without compromising safety making it a more cost-effective alternative to the 50 units/kg dosing of 4F-PCC.
References
Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS (2016) US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA 316(20):2115–2125. https://doi.org/10.1001/jama.2016.16201
Kearon C, Akl EA, Ornelas J et al (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report [published correction appears in Chest. 2016 Oct; 150(4):988]. Chest 149(2):315–352. https://doi.org/10.1016/j.chest.2015.11.026
January CT, Wann LS, Calkins H et al (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons [published correction appears in Circulation. 2019 Aug 6;140(6):e285]. Circulation 140(2):e125–e151. https://doi.org/10.1161/CIR.0000000000000665
Skaistis J, Tagami T (2015) Risk of fatal bleeding in episodes of major bleeding with new oral anticoagulants and vitamin K antagonists: a systematic review and meta-analysis. PLoS ONE 10(9):e0137444. https://doi.org/10.1371/journal.pone.0137444
Herzog E, Kaspereit F, Krege W et al (2015) Four-factor prothrombin complex concentrate reverses apixaban-associated bleeding in a rabbit model of acute hemorrhage. J Thromb Haemost 13(12):2220–2226. https://doi.org/10.1111/jth.13165
Barco S, Whitney Cheung Y, Coppens M, Hutten BA, Meijers JC, Middeldorp S (2016) In vivo reversal of the anticoagulant effect of rivaroxaban with four-factor prothrombin complex concentrate. Br J Haematol 172(2):255–261. https://doi.org/10.1111/bjh.13821
Nagakari K, Emmi M, Iba T (2017) Prothrombin time tests for the monitoring of direct oral anticoagulants and their evaluation as indicators of the reversal effect. Clin Appl Thromb Hemost 23(6):677–684. https://doi.org/10.1177/1076029616638506
Grandhi R, Newman WC, Zhang X et al (2015) Administration of 4-Factor prothrombin complex concentrate as an antidote for intracranial bleeding in patients taking direct Factor Xa inhibitors. World Neurosurg 84(6):1956–1961. https://doi.org/10.1016/j.wneu.2015.08.042
Schenk B, Goerke S, Beer R, Helbok R, Fries D, Bachler M (2018) Four-factor prothrombin complex concentrate improves thrombin generation and prothrombin time in patients with bleeding complications related to rivaroxaban: a single-center pilot trial. Thromb J 16:1. https://doi.org/10.1186/s12959-017-0158-9
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M (2011) Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation 124(14):1573–1579. https://doi.org/10.1161/CIRCULATIONAHA.111.029017
Schulman S, Gross PL, Ritchie B et al (2018) Prothrombin complex concentrate for major bleeding on Factor Xa inhibitors: a prospective cohort study [published correction appears in Thromb Haemost 2018 Dec; 118(12): 2188]. Thromb Haemost 118(5):842–851. https://doi.org/10.1055/s-0038-1636541
Majeed A, Ågren A, Holmström M et al (2017) Management of rivaroxaban- or apixaban-associated major bleeding with prothrombin complex concentrates: a cohort study. Blood 130(15):1706–1712. https://doi.org/10.1182/blood-2017-05-782060
Dager WE, Roberts AJ, Nishijima DK (2019) Effect of low and moderate dose FEIBA to reverse major bleeding in patients on direct oral anticoagulants. Thromb Res 173:71–76. https://doi.org/10.1016/j.thromres.2018.11.009
Engelbart JM, Zepeski A, Galet C, Policeni B, Skeete DA, Faine BA (2019) Safety and effectiveness of factor eight inhibitor bypassing activity for direct oral anticoagulant-related hemorrhage reversal. Am J Emerg Med 37(2):214–219. https://doi.org/10.1016/j.ajem.2018.05.023
Mao G, King L, Young S, Kaplan R (2017) Factor eight inhibitor bypassing agent (FEIBA) for reversal of target-specific oral anticoagulants in life-threatening intracranial bleeding. J Emerg Med 52(5):731–737. https://doi.org/10.1016/j.jemermed.2016.11.011
Piran S, Gabriel C, Schulman S (2018) Prothrombin complex concentrate for reversal of direct Factor Xa inhibitors prior to emergency surgery or invasive procedure: a retrospective study. J Thromb Thrombolysis 45(4):486–495. https://doi.org/10.1007/s11239-018-1645-y
Berger K, Santibañez M, Lin L, Lesch CA (2019) A low-dose 4F-PCC protocol for DOAC-associated intracranial hemorrhage [published online ahead of print, 2019 Apr 14]. J Intensive Care Med 35(11):1203–1208. https://doi.org/10.1177/0885066619840992
Reynolds TR, Gilbert BW, Hall KM (2020) Utilization of 4-Factor prothrombin complex concentrate for reversal of oral Factor Xa inhibitor-associated acute major bleeding: a case series. J Pharm Pract. https://doi.org/10.1177/089719002090701226
Santibanez M, Lesch CA, Lin L, Berger K (2018) Tolerability and effectiveness of 4-factor prothrombin complex concentrate (4F-PCC) for warfarin and non-warfarin reversals. J Crit Care 48:183–190. https://doi.org/10.1016/j.jcrc.2018.08.031
Tomaselli GF, Mahaffey KW, Cuker A et al (2017) 2017 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American College of Cardiology task force on expert consensus decision pathways. J Am Coll Cardiol 70(24):3042–3067. https://doi.org/10.1016/j.jacc.2017.09.1085
Frontera JA, Lewin JJ 3rd, Rabinstein AA et al (2016) Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care 24(1):6–46. https://doi.org/10.1007/s12028-015-0222-x
Tomaselli GF, Kenneth W et al (2020) 2020 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants. J Am Coll Cardiol 76(5):594–622. https://doi.org/10.1016/j.jacc.2020.04.053
Connolly SJ, Crowther M, Eikelboom JW et al (2019) Full study report of andexanet alfa for bleeding associated with Factor Xa inhibitors. N Engl J Med 380:1326–1335. https://doi.org/10.1056/NEJMoa1814051
Panos N, Cook A, John S et al (2020) Factor Xa inhibitor-related intracranial hemorrhage results from a multicenter, observational cohort receiving prothrombin complex concentrates. Circulation 141:1681–1689. https://doi.org/10.1161/CIRCULATIONAHA.120.045769
Sarode R, Milling TJ Jr, Refaai MA et al (2013) Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation 128:1234–1243. https://doi.org/10.1161/CIRCULATIONAHA.113.002283
Brekelmans M, Abdoellakhan R, Scheres L et al (2018) Clinical outcome of patients with a vitamin K antagonist-associated bleeding treated with prothrombin complex concentrate. Res Pract Thromb Haemost. 2(1):77–84. https://doi.org/10.1002/rth2.12055
ANDEXXA [package insert] (2018) Portola Pharmaceuticals, Inc, South San Francisco
Acknowledgements
Mital Desai, Susan Ontanon.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hormese, M., Littler, A., Doane, B. et al. Comparison of high- and low-dose 4-factor prothrombin complex concentrate for the emergent reversal of oral Factor Xa inhibitors. J Thromb Thrombolysis 52, 828–835 (2021). https://doi.org/10.1007/s11239-021-02412-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02412-8