Abstract
Direct oral factor Xa (FXa) inhibitors are widely used for anticoagulation but a targeted antidote is not available. Four-factor prothrombin complex concentrate (4FPCC) has been shown in observational studies to support hemostasis in most patients with major bleeding related to FXa inhibitors with an acceptable rate of thromboembolic events. However, the effectiveness of 4FPCC for reversal of FXa inhibitors prior to emergency surgery or invasive procedures is unclear. A retrospective chart review was performed in patients that received 4FPCC at Hamilton General Hospital from 2015 to 2017. The primary effectiveness outcome was based on the comment of the surgeon on the adequacy of the hemostasis. If no such comment was documented, the case was discussed with a surgeon specialized in the type of surgery/procedure performed to obtain their best opinion. The principal safety outcome was thromboembolic events including venous thromboembolism, ischemic stroke, systemic embolism or myocardial infarction during 7 days after surgery. A total of 247 patients that had received 4FPCC were initially screened and 21 were on a FXa inhibitor and had emergency surgery/procedure. The mean age was 74 ± 11 years, and 14 (66.7%) were males. Hemostasis was rated as good in most patients (18 of 21, 85.7%). There were no thromboembolic events. The all-cause mortality rate was 28.6%; 2/3 of these patients had an intracranial hemorrhage. Hemostasis was rated as good in most patients with no thromboembolic events observed. Prospective studies assessing the safety and effectiveness of 4FPCC for this indication are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Four direct oral anticoagulants (apixaban, dabigatran, edoxaban, and rivaroxaban) have been shown in clinical trials to be as effective as warfarin for prevention of stroke in patients with atrial fibrillation and treatment and prevention of venous thromboembolism (VTE) and associated with less major bleeding [1, 2]. Dabigatran is a direct thrombin inhibitor and the rest are direct factor Xa (FXa) inhibitors.
Compared with warfarin, direct oral anticoagulants (DOACs) have fewer drug interactions, do not require frequent laboratory monitoring, and are given at fixed doses. However, despite having these positive attributes, dabigatran is the only DOAC with an approved targeted antidote, idarucizumab [3]. An antidote for direct FXa inhibitors is not available but andexanet alpha is currently under investigation and the interim results of a phase III trial in patients with major bleeding have been published [4].
Four-factor prothrombin complex concentrate (4FPCC) successfully reversed the anticoagulant effects of direct FXa inhibitors in healthy volunteers and animal studies [5,6,7,8]. In addition, 4FPCC has been shown in observational studies to achieve hemostasis in most patients with major bleeding related to direct FXa inhibitors and seemed to have a low rate of thromboembolic complications [9, 10]. However, there are no studies on the use of 4FPCC for reversal of direct FXa inhibitors prior to emergency surgeries or invasive procedures.
We reviewed consecutive cases in our hospital to determine the effectiveness of 4FPCC for direct FXa inhibitor reversal in achieving adequate hemostasis during emergency surgery or an invasive procedure and the incidence of thromboembolic events related to 4FPCC administration.
Materials and methods
Inclusion and exclusion criteria
A retrospective chart review was performed in patients that received 4FPCC at Hamilton General Hospital from January 2015 to December 2017. This was based on information from Transfusion Medicine on all patients for whom 4FPCC had been issued. Patients were included if they had received 4FPCC ≤ 24 h prior to emergency surgery or invasive procedure while on treatment with apixaban, edoxaban, or rivaroxaban. Patients were excluded if (1) 4FPCC was used for reversal of anticoagulant effects of warfarin or for the management of coagulopathy, or (2) 4FPCC was administered to reverse direct FXa-related bleeding during or after a procedure. We obtained approval from the Hamilton Integrated Research Ethics Board without the need for informed consent.
Baseline characteristics
Patient demographics and clinical and laboratory data were collected. The demographics included patient’s age, sex, body weight and renal function. Clinical characteristics were the use of additional anti-thrombotic agents including aspirin and/or clopidogrel; and the type of surgical or invasive procedure performed. The following parameters related to treatments were collected: type (apixaban or rivaroxaban), dose, indication, and the timing of the last dose of DOAC; the dose of 4FPCC and the time elapsed from administration of 4FPCC to the start of surgery; the use of other hemostatic products such as cryoprecipitate, platelets, tranexamic acid, activated PCC, or recombinant factor VIIa. The use of other blood products including fresh frozen plasma (FFP) and red blood cells (RBCs) was also recorded. The laboratory parameters reviewed were baseline hemoglobin level prior to surgery, the first hemoglobin level after the surgery, and the lowest hemoglobin level; the baseline creatinine; and the closest international normalized ratio (INR) and anti-FXa level, if available, prior to surgery. We calculated the drop in hemoglobin during surgery as the difference between the last hemoglobin before and the first hemoglobin after surgery, with correction for transfusions, assuming that each unit of RBC had increased the hemoglobin by 10 g/L. The creatinine clearance was calculated using the Cockcroft–Gault formula.
Primary and secondary outcomes
The primary effectiveness outcome was based on the comment by the surgeon if hemostasis was good/not good or that there was no bleeding complication/was a bleeding complication. If no such comment was documented, results of hemoglobin values, the estimated blood loss (EBL), and the operating report were discussed with a surgeon specialized in the type of surgery/procedure performed to obtain their opinion. Secondary effectiveness outcomes were transfusions of RBC after 4FPCC, the corrected drop in hemoglobin peri-operatively, and EBL after surgery. The principal safety outcome was the incidence of thromboembolic complications including VTE, ischemic stroke, systemic embolism, or myocardial infarction during 7 days after surgery. Secondary safety outcome was all-cause 30-day mortality.
Statistical analysis
Results are presented with mean and standard deviation for variables with a normal distribution and with median and interquartile range (IQR) for skewed distributions.
Results
Baseline characteristics
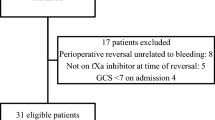
A total of 247 patients that had received 4FPCC were initially screened and 21 patients were included in the analysis. The remaining patients were excluded as 4FPCC was used for reversal of anticoagulant effects of warfarin or for the management of coagulopathy (n = 223), or 4FPCC was administered to reverse direct FXa-related bleeding during or after a procedure (n = 3). The baseline characteristics of the patients are listed in Table 1. The surgical characteristics for each patient including the type of surgery, the surgeon’s comment, transfusion of RBCs pre- and post surgery, as well the time from the last dose of apixaban or rivaroxaban to the administration of 4FPCC are listed in Table 2.
Hemostatic treatment
The hemostatic management given prior to the start of the surgeries or procedures is outlined in Table 3. 4FPCC was administered at a mean total dose of 2167 ± 428 units and a mean dose of 26 ± 7 units/kg. 16 (76.2%) received 2000 units of 4FPCC, 4 (19%) had 3000 units, and 1 (4.8%) had 1500 units, which was Octaplex® (Octapharma, Lachen, Switzerland) in all patients. The reason for the use of different 4FPCC doses was based on an empiric decision on a case-by-case situation. The median (IQR) time from 4FPCC administration to the start of surgery was 1 h (1–3). None of the patients received a second dose of 4FPCC. 8 (38%) also received other hemostatic agents prior to the start of the surgery/procedure; cryoprecipitate alone (n = 1), platelets and cryoprecipitate (n = 2), platelets alone (n = 1), platelets and tranexamic acid (n = 2), and tranexamic acid alone (n = 2). Of the five patients (23.8%) who received platelets, three had one adult dose of platelets, one received two adult doses of platelets, and one received three adult doses of platelets. In addition, of the five patients who received platelets, two were on an anti-platelet medication (one was on Aspirin and the other was on Plavix). None of the patients received activated PCC or recombinant factor VIIa. The median (IQR) time from 4FPCC administration to the re-start of anticoagulation in 12 patients was 6 days (2–10). The timing of the re-start of anticoagulation after 4FPCC administration was unknown in two patients and anticoagulation was never re-started in six patients who died during the 30-day follow-up. In addition, one patient was on prophylactic anticoagulation after a total hip replacement procedure prior to requiring an emergency appendectomy, therefore anticoagulation was discontinued after the latter surgery.
Effectiveness of 4FPCC
The primary and secondary outcomes are listed in Table 4. The median (IQR) hemoglobin values were 125 g/L (109–130), 111 g/L (102–119), and 87 g/L (78–101), prior to operation, first hemoglobin after the operation, and the lowest hemoglobin value, respectively. The median (IQR) change in hemoglobin, the corrected change in hemoglobin, and EBL after surgery were − 15 g/L (− 21 to − 3), − 21 g/L (− 36 to − 10), and 200 mL (200–625, n = 8), respectively. Three patients (14.3%) received RBC transfusions after surgery: one patient received 6 units, one received 2 units, and one received 1 unit of RBC. The latter two patients received the RBC transfusions 2 days after surgery. Hemostasis was rated as good in most patients (18 of 21, 85.7%). A 61-year old male had a corrected change in hemoglobin of − 62 g/L. This patient underwent laparotomy for repair of penetrating stab wounds resulting in lacerations of epigastric vessels, small bowel, and liver. The surgeon’s comment was that “active bleeding from stab wounds was controlled by the end of surgery and that surgical hemostasis was adequate”. Two additional cases with excessive blood loss were due to surgical technical failure. A 90-year old male had a repair of type 1A aortic endoleak. The EBL after surgery was 2.5 L. Since there was no comment available on the adequacy of hemostasis during surgery, the case was discussed with the surgeon who performed the initial surgery to obtain their best opinion. The surgeon’s comment was that “this was absolutely a surgical bleed, the stent did not seal the aorta. As a result, there was a hole remaining. This was not a failure of 4FPCC”. In addition, a 61-year old male had an endovascular embolization, extensive coiling for a superior mesenteric artery (SMA) bleeding by interventional radiology (IR). However, he died of progressive intra-abdominal bleeding and compartment syndrome after a failed IR-guided coiling of an arterial active bleeding from a branch of the SMA.
Safety of 4FPCC
There were no thromboembolic complications. An 80-year old female who was on rivaroxaban for a left leg proximal DVT diagnosed 10 days prior to having a laminectomy was found to have persistence of her old DVT on compression ultrasound 2 days after her surgery. A 61-year old male who was on apixaban for a history of unprovoked PE 2 years prior to having a laparotomy was reported to have suspected segmental PE 2 days after his surgery. However, the computerized tomography scan was discussed with an experienced radiologist, who concluded that the filling defect seen was likely an artifact and not a PE.
Six patients (28.6%) died during the hospital stay 1–17 days after the surgery; four had intracranial hemorrhage (ICH) with poor prognosis prior to having a twist drill and decompression, one had hydrocephalus and died as a result of progressive brain herniation, and one died of progressive intra-abdominal bleeding and compartment syndrome.
Discussion
This is the first report that has examined the effectiveness and safety of 4FPCC for reversal of direct FXa inhibitors prior to emergency surgery or invasive procedure. Hemostasis was assessed as normal in most patients with no thromboembolic events observed.
Majority of the patients in our study received 4FPCC at a low dose of 2000 units, which corresponds to about 25 units/kg for an 80 kg person. Of the six patients who had an ICH, only one had a dose of 3000 units. The likely reason for the use of a fixed dose of 2000 units is the presence of a hospital protocol suggesting the use of this regimen for the reversal of direct FXa inhibitor-related major bleeding [11]. This dose of 4FPCC was shown to reverse the rivaroxaban anticoagulant activity in an ex-vivo study [5] and has been shown in two observational studies to achieve hemostasis in most patients with major bleeding related to direct FXa inhibitors [10, 11]. Consensus algorithms recommend a dose of 50 units/kg for reversal of FXa inhibitor-related major bleeding [12, 13]. However, there is no recommended dose available for reversal of urgent surgery. It is unclear if a higher dose such as 50 units/kg could have improved the outcomes, especially in patients presenting with an ICH. Future studies comparing a low dose (for example 25 units/kg) with 50 units/kg are needed.
The results of our study are similar to previous studies that examined the safety and effectiveness of 4FPCC for emergency reversal of warfarin anticoagulation [14, 15]. A prospective study of 43 patients requiring emergency reversal of warfarin anticoagulation, in which 26 had interventional procedures and 17 had an acute bleeding, reported that hemostatic efficacy was rated as very good or satisfactory in most of the patients (42 of 43; 98%) [14]. One patient (2%) with a history of metastatic cancer had a suspected fatal PE; this was possibly related to 4FPCC administration [14]. Another prospective study of 61 patients requiring urgent reversal of warfarin anticoagulation, in which 48 had interventional procedures and 13 had acute bleeding, found that the efficacy of 4FPCC was “excellent” in the majority of the patients (60 of 61; 98%). Two patients (3%) had a thromboembolic event. The authors concluded that the thromboembolic complication rate was low and that these events could have occurred without 4FPCC administration [15]. In addition, similar to our study, Idarucizumab was effective in reversing the anticoagulant effect of dabigatran and achieving normal hemostasis in the majority of patients (184 of 202; 93.4%) who had urgent surgery in the Reversal Effects of Idarucizumab on Active Dabigatran (REVERSE-AD) study [4]. However, the rate of thromboembolic events was 7.4%, which is higher compared with our study. This might due to differences in sample size and baseline characteristics.
The mortality rate was 28.6% in our study, which is higher than the rates of 7% [14] and 3% [15] reported in previous reports of 4FPCC use for emergency reversal of warfarin anticoagulation and 18.9% in the REVERSE-AD study [4]. However, 2/3 of the patients that died in our study had an ICH with poor prognosis prior to the neurosurgical intervention. This can be compared with one patient [14] and none of the patients [15] in the warfarin reversal cohorts and 17 patients in the REVERSE-AD study [4] experiencing ICH. Anticoagulant-related ICH is known to have a high mortality rate [16].
Our study has limitations. First, this is a retrospective study and there could have been a selection bias for using 4FPCC with the exclusion of severe cases. Second, the exact timing of the last dose of the FXa inhibitor was more than 24 h for three patients and missing for eight of the patients. The timing of the last dose of apixaban or rivaroxaban was patient self-reported; therefore it is possible that this was misremembered (for example in those presenting with an ICH). In addition, we did not have plasma levels of rivaroxaban or apixaban prior to the start of the surgery. Given the short half-life of apixaban (12 h) [17] and rivaroxaban (5–13 h) [18, 19], it is possible that the anticoagulant effect was already low prior to the administration of 4FPCC in some of the patients. An anti-Xa assay is a useful test to perform in directing therapeutic interventions as normal anti-Xa activity likely excludes clinically relevant direct FXa levels [20]. Third, we did not have a control group to enable us to assess the true effect of the addition of 4FPCC to conservative management. Nonetheless, our study is the first report that has addressed the use of 4FPCC in reversing the anticoagulant effect of direct FXa inhibitors prior to emergency surgery or invasive procedure.
Conclusions
We found that hemostasis was normal in most patients with no thromboembolic complications observed. Our results are however limited by the absence of a control group and the lack of information on the plasma levels of the direct FXa inhibitors. Therefore, prospective studies assessing the safety and effectiveness of 4FPCC for this indication are needed.
References
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomized trials. Lancet 383:955–962
Kakkos SK, Kirkilesis GI, Tsolakis IA (2014) Editor’s Choice - efficacy and safety of the new oral anticoagulants dabigatran, rivaroxaban, apixaban, and edoxaban in the treatment and secondary prevention of venous thromboembolism: a systematic review and meta-analysis of phase III trials. Eur J Vasc Endovasc Surg 48(5):565–575
Pollack CV Jr, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, Dubiel R, Huisman MV, Hylek EM, Kam CW, Kamphuisen PW, Kreuzer J, Levy JH, Royle G, Sellke FW, Stangier J, Steiner T, Verhamme P, Wang B, Young L, Weitz JI (2017) Idarucizumab for dabigatran reversal – full cohort analysis. N Engl J Med 377(5):431–441
Connolly SJ, Milling TJ Jr, Eikelboom JW, Gibson CM, Curnutte JT, Gold A, Bronson MD, Lu G, Conley PB, Verhamme P, Schmidt J, Middeldorp S, Cohen AT, Beyer-Westendorf J, Albaladejo P, Lopez-Sendon J, Goodman S, Leeds J, Wiens BL, Siegal DM, Zotova E, Meeks B, Nakamya J, Lim WT, Crowther M (2016) ANNEXA-4 investigators. Andexanet alfa for acute major bleeding associated with factor Xa inhibitors. N Engl J Med 375(12):1131–1141
Marlu R, Hodaj E, Paris A, Albaladejo P, Crackowski JL, Pernod G (2012) Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost 108(2):217
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M (2011) Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation 124(14):1573–1579
Levi M, Moore KT, Castillejos CF, Kubitza D, Berkowitz SD, Goldhaber SZ, Raghoebar M, Patel MR, Weitz JI, Levy JH (2014) Comparison of three-factor and four-factor prothrombin complex concentrates regarding reversal of the anticoagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost 12(9):1428–1436
Zahir H, Brown KS, Vandell AG, Desai M, Maa JF, Dishy V, Lomeli B, Feussner A, Feng W, He L, Grosso MA, Lanz HJ, Antman EM (2015) Edoxaban effects on bleeding following punch biopsy and reversal by a 4-factor prothrombin complex concentrate. Circulation 131(1):82–90
Grandhi R, Newman WC, Zhang X, Harrison G, Moran C, Okonkwo DO, Ducruet AF (2015) Administration of 4-factor prothrombin complex concentrate as an antidote for intracranial bleeding in patients taking direct factor Xa inhibitors. World Neurosurg 84(6):1956–1961
Majeed A, Ågren A, Holmström M, Bruzelius M, Chaireti R, Odeberg J, Hempel EL, Magnusson M, Frisk T, Schulman S (2017) Management of rivaroxaban- or apixaban-associated major bleeding with prothrombin complex concentrates: a cohort study. Blood 130(15):1706–1712
Schulman S, Gross PL, Ritchie B, Nahirniak S, Lin Y, Lieberman L, Carrier M, Crowther MA, Ghosh I, Lazo-Langner A, Zondag M (2018) Prothrombin complex concentrate for major bleeding on factor Xa inhibitors: a prospective cohort study. Accepted in Thromb Haemost
Frontera JA, Lewin JJ 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, del Zoppo GJ, Kumar MA, Peerschke EI, Stiefel MF, Teitelbaum JS, Wartenberg KE, Zerfoss CL (2016) Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care 24(1):6–46
Tomaselli GF, Mahaffey KW, Cuker A, Dobesh PP, Doherty JU, Eikelboom JW, Florido R, Hucker W, Mehran R, Messé SR, Pollack CV Jr, Rodriguez F, Sarode R, Siegal D, Wiggins BS (2017) 2017 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American College of Cardiology Task Force on expert consensus decision pathways. J Am Coll Cardiol 70(24):3042–3067
Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H (2008) Beriplex P/N Anticoagulation Reversal Study Group. Prothrombin complex concentrate (Beriplex P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost 6(4):622–631
Altorjay Á, Szabó É, Boda Z, Kramer L, Ngo LY, Engl W, Firth CL, Ahlstrom ER, Gelmont DM, Pabinger I (2015) An international, multicenter, prospective study of a prothrombin complex, Prothromplex Total complex®, in anticoagulant reversal. Thromb Res 135(3):485–491
Majeed A, Kim YK, Roberts RS, Holmström M, Schulman S (2010) Optimal timing of resumption of warfarin after intracranial hemorrhage. Stroke 41(12):2860–2866
Frost C, Wang J, Nepal S, Schuster A, Barrett YC, Mosqueda-Garcia R, Reeves RA, LaCreta F (2013) Apixaban, an oral, direct factor Xa inhibitor: single dose safety, pharmacokinetics, pharmacodynamics and food effect in healthy subjects. Br J Clin Pharmacol 75(2):476–487
Kubitza D, Becka M, Wensing G, Voith B, Zuehlsdorf M (2005) Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939—an oral, direct Factor Xa inhibitor—after multiple dosing in healthy male subjects. Eur J Clin Pharmacol 61(12):873–880
Kubitza D, Becka M, Roth A, Mueck W (2008) Dose-escalation study of the pharmacokinetics and pharmacodynamics of rivaroxaban in healthy elderly subjects. Curr Med Res Opin 24(10):2757–2765
Cuker A, Siegal D (2015) Monitoring and reversal of direct oral anticoagulants. Hematol Am Soc Hematol Educ Program 2015:117–124
Funding
SP was a recipient of a CanVECTOR thrombosis fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Schulman has received a research grant from Octapharma for a previous study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Piran, S., Gabriel, C. & Schulman, S. Prothrombin complex concentrate for reversal of direct factor Xa inhibitors prior to emergency surgery or invasive procedure: a retrospective study. J Thromb Thrombolysis 45, 486–495 (2018). https://doi.org/10.1007/s11239-018-1645-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-018-1645-y