Abstract
Venous thromboembolism (VTE) is a common complication in cancer patients and anticoagulation (AC) remains the standard of care for treatment. Inferior vena cava (IVC) filters may also used to reduce the risk of pulmonary embolism, either alone or in addition to AC. Although widely used, data are limited on the safety and efficacy of IVC filters in cancer patients. We performed a retrospective review of outcomes after IVC filter insertion in a database of 1270 consecutive patients with cancer-associated pulmonary embolism (PE) at our institution between 2008 and 2009. Outcomes measured included rate of all recurrent VTE, recurrent PE, and overall survival within 12 months. 317 (25%) of the 1270 patients with PE had IVC filters placed within 30 days of the index PE event or prior to the index PE in the setting of prior DVT. Patients with IVC filters had markedly lower overall survival (7.3 months) than the non-IVC filter patients (13.2 months). Filter patients also had a lower rate of AC use at time of initial PE. There was a trend towards higher recurrent VTE in patients with IVC filters (11.9%) compared to non-filter patients (7.7%), but this was not significant (p = 0.086). The risk of recurrent PE was similar between the IVC filter cohort (3.5%) and non-filter group (3.5%, p = 0.99). Cancer patients receiving IVC filters had a similar risk of recurrent PE, but a trend towards more overall recurrent VTE. The filter patients had poorer overall survival, which may reflect a poorer cancer prognosis, and had greater contraindication to AC; therefore these patients likely had a higher inherent risk for recurrent VTE. A prospective study would be helpful for further clarification on the partial reduction in the recurrent PE risk by IVC filter placement in cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) is a frequent complication in cancer patients, with a four- to seven-fold higher risk of VTE compared to patients without cancer [1]. Active cancer is associated with nearly 20% of newly diagnosed VTE in the community setting [2]. The mainstay of treatment for VTE is anticoagulation (AC). Over several decades, inferior vena cava (IVC) filters have been increasingly utilized as mechanical thromboprophylaxis to reduce the risk of PE, either in the setting of contraindications to AC or in conjunction with AC [3, 4]. Studies examining IVC filters alone [5] or in addition to AC [6, 7] in primarily non-cancer populations have demonstrated a decreased risk for recurrent pulmonary emboli (PE), and an increased risk of deep vein thrombosis (DVT) in the population receiving filters.
Whether IVC filters play a causal role in recurrent VTE or their use reflects a higher VTE risk patient population is not understood. Studies examining IVC filter use in cancer populations are lacking. In this study, we address IVC filter use in patients with cancer-associated PE (active measurable cancer and/or undergoing treatment for cancer) within our institution. Key relevant outcomes were rates of all recurrent VTE, recurrent PE, and overall survival (OS) in the presence or absence of an IVC filter and AC.
Methods
Study design and participants
This is a retrospective, single institution study, which was approved by our Institutional Review Board. The study population comprised all adult patients (≥ 18 years of age) diagnosed with a radiographically-confirmed PE at Memorial Sloan Kettering Cancer Center (MSKCC) from 2008 to 2009 (N = 1270). 554 (44%) of PE were asymptomatic and 716 (56%) were symptomatic. All PE cases were initially identified by billing code, followed by manual review of the electronic medical record by two study physicians. Similarly, baseline patient characteristics, use of AC, and outcomes of recurrent VTE and date of death were identified by review of the electronic medical record by two study physicians. For patients with a new VTE event, we determined whether patients were on AC on the date of diagnosis of the recurrent event. Interruptions in anticoagulation during the study period could not otherwise be reliably captured. Analysis was at 12-months of follow-up or earlier endpoint for patients without 12 months of follow-up. In these cases, the date of last available relevant records was used as date of censoring.
Statistical analysis
Statistical analyses were performed using R version 3.2.2 (cran.r-project.org). Patient characteristics are presented as median and range for continuous variables, and frequency and percentage for categorical variables. Wilcoxon rank sum test and Chi-squared test were used to compare patient characteristics in those with and without IVC filter placement. The cumulative incidence for recurrent DVT/PE was calculated from date of index PE diagnosis to date of recurrent DVT/PE detection radiographically, death, or last follow up. Deaths without recurrent DVT/PE were considered a competing event. Patients alive without any new VTE event were censored at last follow-up. Gray’s k-test was used in analyzing the relationship between recurrent DVT/PE and IVC filter placement. OS was calculated from date of index PE diagnosis to date of death or last follow up. Log-rank test was used to compare OS between cohorts that did or did not receive IVC filters. Multivariate modeling was performed using Fine and Gray regression and Cox proportional hazard model to adjust for other clinical variables in analyses for recurrent VTE and for OS, respectively. Fisher’s exact test was employed to compare the use of AC at time of recurrent VTE in patients with and without IVC filters.
Results
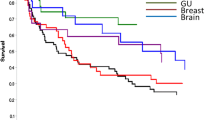
1270 patients were diagnosed with a PE during the study period. Patients had diverse primary tumors with most common types including lung (N = 246, 19.4%), colorectal (N = 139, 10.9%), gynecologic (N = 130, 10.2%), and breast (N = 103, 8.1%). Of this cohort, 1030 patients (81.1%) had a metastatic solid tumor, 85 (6.7%) had a hematologic malignancy, 46 (3.6%) had primary central nervous system (CNS) tumors, and 109 (8.6%) had localized solid tumors (excluding CNS tumors). Cancer status was ascertained at the time of the index PE. Median age at index PE was 64.1 years (range 18.3–93.4), and 53% of patients were female. Anatomic locations of the index PE included saddle (N = 33, 2.6%), main (N = 187, 14.7%), lobar (N = 197, 15.5%), segmental (N = 583, 45.9%), subsegmental (N = 224, 17.6%), and unspecified (N = 46, 3.6%). 96% of patients were placed on therapeutic AC within 7 days of PE diagnosis.
Deaths and recurrent VTE were recorded for 12 months following the index PE diagnosis. Follow-up information was available for at least 12 months or reaching a primary endpoint for all but 21 patients (1.7%). The majority of patients (96%) were placed on therapeutic AC at time of diagnosis of PE (within 7 days of PE diagnosis). For patients with a new VTE event, we determined whether patients were on AC on the date of recurrent event but otherwise interruptions in AC during the study period could not be reliably captured. Recurrent VTE was defined as a new PE in a new radiographically identified vascular distribution, such as in a new lobe, or in a more proximal distribution than index PE and/or any new, symptomatic proximal deep vein thrombosis. Recurrent VTE were recorded for 1 year following initial PE diagnosis. For this analysis, a new isolated calf thrombosis, venous catheter-associated thrombosis, upper extremity thrombosis, superficial vein thrombosis, or visceral thrombosis were not considered a recurrent VTE event.
Of the 1270 PE cohort, 25% (N = 317) had IVC filters placed either within 30 days following the index PE event (N = 274), or prior to the index PE in the setting of prior DVT (N = 43). The indications stated for IVC filter placement included contraindication to AC (39%), pre-operative (16%), AC failure (16%), poor cardiopulmonary reserve (6%) or indication unclear (23%).
Comparison of baseline characteristics for the 317 patients with IVC filters to the 953 patients that did not receive IVC filters (Table 1) revealed several significant differences. Patients who received IVC filters were more likely to have proximal emboli within the pulmonary arterial system (saddle embolism and main pulmonary artery) (p < 0.001), and more likely to have a primary CNS tumor (overall comparison by disease: p = 0.002). Patients receiving IVC filters were less likely to be on therapeutic AC at time of index PE when compared to patients without filters (86 vs. 99%, respectively, p < 0.001).
Composite 12-month rate of all recurrent VTE was non-significantly higher with IVC filters (11.9%) than patients without filters (7.7%), (p = 0.086, Table 1). Risk of recurrent PE was similar between the IVC filter cohort (3.5%) and non-IVC filter cohort (3.5%), (p = 0.99). The incidence of recurrent DVT was significantly higher in the IVC filter group, 8.2 vs. 4.2% (p = 0.03) (Table 1). As we were unable to account for all subsequent interruptions in AC, we explored the use of AC in the patients who experienced a recurrent VTE at time of the recurrent event. Of the patients with recurrent VTE, fewer patients (62%) with IVC filters had been on therapeutic AC at the time of the recurrent event, compared to 74% of those without IVC filters, though this was not statistically significant (p = 0.27 by Fisher’s exact test). All patients were on Low Molecular Weight Heparin (enoxaparin, dalteparin, or tinzaparin), or fondaparinux. No patients with recurrent VTE were anticoagulated with warfarin. There were 51 recurrent PE. The majority of the recurrent PE were located in a new anatomical location compared to the index PE (42, 82.4%); however, 9 (17.6%) were considered to be possible propagation of the index PE based on a more proximal location within the same pulmonary artery (all nine in patients without IVC filters).
Given the presence of other clinical variables that may influence rate of recurrent VTE, a multivariate analysis was performed, adjusting for age, sex, index PE location (main/saddle vs. other), use of therapeutic AC at time of index PE diagnosis, and disease type (Table 2). Following multivariate analysis, there was a trend toward recurrent DVT in patients with IVC filters though this did not reach statistical significance (p = 0.087).
Median OS for IVC filter patients was 7.2 vs. 13.2 months in non-IVC filter patients, (p < 0.001 by log-rank testing). On multivariate analysis, presence of IVC filter (HR 1.26 [CI 1.09–1.47], p = 0.002), was significantly associated with poorer OS (data not shown). Sex, anatomy of initial PE, and administration of therapeutic AC at time of initial PE were not associated with OS. Median time from IVC filter placement to death was 3.6 months (range 0.07–88.4 months) with 62 IVC filters placed within 1 month before death (14%).
Discussion
IVC filter placement has become a widely used tool for the prevention of PE, but the relative benefits and risks remain unclear, particularly in cancer patients. The objective of filter placement is to reduce the risk of PE in patients with a temporary or ongoing contraindication to AC, or who are at particularly high risk of a PE for other reasons.
Few randomized studies have been conducted to evaluate the risk to benefit ratio of IVC filters, and no prospective studies have been conducted specifically in cancer populations. The role for IVC filter placement in the setting of a new PE diagnosis has recently been examined in a randomized study, The Prévention du Risque d’Embolie Pulmonaire par Interruption Cave 2 (PREPIC2) Study [8]. PREPIC2 examined the effect of retrievable IVC filters in addition to anticoagulation in patients with a severe PE in presence of a lower extremity DVT. They concluded that the addition of an IVC filter to AC did not reduce the risk of recurrent, symptomatic PE at 3 months time, and therefore routine IVC filters should not be recommended in patients who can be treated with AC [8]. PREPIC2 was in a primarily non-cancer population as only 62 of the 399 patients in the study had active cancer [8]. Two recent reports retrospectively reported complications from IVC filters in cancer patients, however, these reports did not compare the outcomes of patients with and without IVC filters [9, 10].
In our current study of cancer patients with a diagnosed PE, IVC filters were placed in 25% of the patients. Interpretation of the key findings must be considered in the context that the choice of IVC filter was at the judgment and discretion of the managing physicians and the populations with and without IVC filter were not matched. The patients receiving IVC filters were of poorer overall status, as reflected by the difference in overall survival: OS 7.2 months in the IVC filter patients vs. 13.2 months in non-filter patients. Patients with CNS tumors were more likely to have IVC filters placed, which may be related to an increased perceived risk of intracranial hemorrhage [11,12,13]. Patients with larger PEs including saddle and main PEs were more likely to undergo IVC filter placement as well, perhaps because a relative indication for IVC filter per the Society for Interventional Radiology guidelines is a “massive PE treated with thrombectomy/thrombolysis [14].” The IVC filter patients also were more likely to have a contraindication to AC at the time of index PE and at time of filter placement. We observed that patients receiving IVC filters had a trend towards a higher rate of all recurrent VTE, although not statistically significant. The trend towards increased recurrent VTE event rate observed in patients receiving filters may relate to increased DVT risk from more advanced cancer and inability to anticoagulate.
Further, of the recurrent VTE events, fewer were PE in the IVC filter cohort (29%) vs. the non-filter cohort (45%). This is interpreted as a potential reduction in embolization rates with the use of IVC filters, though filters did not provide complete protection from recurrent PE in our study. A putative partial protective effect of IVC filter on PE rates may have been counterbalanced by a higher VTE risk associated with poorer performance status, more significant acute illnesses/hospitalizations, and resulting immobilization in those receiving the IVC filter. Future research is warranted to evaluate the partial risk reduction of an existing DVT becoming a clinically detected PE with IVC filter placement.
Patients with more advanced disease may also undergo more imaging studies in both outpatient and inpatient settings. It is plausible that this could create a detection bias in which patients with IVC filters undergo more imaging, and thus more DVT or PE events were detected.
Barginear and colleagues retrospectively reviewed outcomes of 206 consecutive cancer patients with VTE, and also found that the need for IVC filter predicted marked reduced survival, similar to our observation [15]. Multivariate survival analysis did not demonstrate that performance status or type of thrombus were confounders [15]. Ho et al. analyzed IVC filter use in a large series of cancer patients with acute VTE, noting that IVC filters were placed in 2747 (19.6%) of 14,000 cancer patients, with filter usage varying significantly based upon type of hospital and primary tumor type [16]. Our series demonstrated a slightly higher rate of IVC filter placement (25%) reflective of institutional variation in practice and patient population.
Barginear and colleagues also performed a small, randomized study of cancer patients with VTE (N = 64) to compare fondaparinux vs .fondaparinux plus IVC filter and did not find any differences in recurrent VTE, resolution of index VTE, or survival between groups, though comparisons were limited by small numbers [17]. There are insufficient randomized, prospective data in oncology populations addressing the utility of IVC filters, and considering the nature of complexity and heterogeneity of cancer-associated thrombosis, it is unlikely to be available in the foreseeable future.
Limitations to our study include the retrospective, non-randomized nature of this study, although patients who underwent filter placement compared to those who did not were reasonably similar demographically. For other differences such as PE location, cancer type, we accounted for these differences using multivariate modeling. We adjusted for use of AC at time of PE diagnosis, but we unable to adjust for subsequent interruptions in AC in our multivariate models. Of note, the risk for VTE was adjusted for baseline characteristics (such as PE location, cancer type) but not for clinical complications that may have occurred during the follow-up (surgery, infections, immobilization, chemotherapeutic agent used or radiotherapy).
In patients where a contraindication to AC is no longer present, consideration should be made to remove IVC filters as IVC filtration is no longer indicated. Further prospective research is required to establish safety and efficacy of IVC filters in cancer patients.
References
Blom JW, Doggen CJ, Osanto S, Rosendaal FR (2005) Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 293(6):715–722
Heit JA, O’Fallon WM, Petterson TM, Lohse CM, Silverstein MD, Mohr DN et al (2002) Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 162(11):1245–1248
Stein PD, Matta F, Hull RD (2011) Increasing use of vena cava filters for prevention of pulmonary embolism. Am J Med 124(7):655–661
Duszak R Jr, Parker L, Levin DC, Rao VM (2011) Placement and removal of inferior vena cava filters: national trends in the medicare population. J Am Coll Radiol 8(7):483–489
Muriel A, Jimenez D, Aujesky D, Bertoletti L, Decousus H, Laporte S et al (2014) Survival effects of inferior vena cava filter in patients with acute symptomatic venous thromboembolism and a significant bleeding risk. J Am Coll Cardiol 63(16):1675–1683
PREPIC Study Group (2005) Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 112(3):416–422
Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P et al (1998) A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prevention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med 338(7):409–415
Mismetti P, Laporte S, Pellerin O, Ennezat PV, Couturaud F, Elias A et al (2015) Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA 313(16):1627–1635
Wallace MJ, Jean JL, Gupta S, Eapen GA, Johnson MM, Ahrar K et al (2004) Use of inferior vena caval filters and survival in patients with malignancy. Cancer 101(8):1902–1907
Mikhail S, Hannan L, Pishvaian MJ, Kessler C (2015) Retrievable inferior vena cava filters in patients with cancer are safe but are they beneficial? Med Oncol 32(6):622
Norden AD, Bartolomeo J, Tanaka S, Drappatz J, Ciampa AS, Doherty LM et al (2012) Safety of concurrent bevacizumab therapy and anticoagulation in glioma patients. J Neurooncol 106(1):121–125
Yust-Katz S, Mandel JJ, Wu J, Yuan Y, Webre C, Pawar TA et al (2015) Venous thromboembolism (VTE) and glioblastoma. J Neurooncol 124(1):87–94
Weinstock MJ, Uhlmann EJ, Zwicker JI (2016) Intracranial hemorrhage in cancer patients treated with anticoagulation. Thromb Res 140(Suppl 1):S60–S65
Kaufman JA, Kinney TB, Streiff MB, Sing RF, Proctor MC, Becker D et al (2006) Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 17(3):449–459
Barginear MF, Lesser M, Akerman ML, Strakhan M, Shapira I, Bradley T et al (2009) Need for inferior vena cava filters in cancer patients: a surrogate marker for poor outcome. Clin Appl Thromb/Hemost 15(3):263–269
Ho G, Brunson A, White R, Wun T (2015) Vena cava filter use in cancer patients with acute venous thromboembolism in California. Thromb Res 135(5):809–815
Barginear MF, Gralla RJ, Bradley TP, Ali SS, Shapira I, Greben C et al (2012) Investigating the benefit of adding a vena cava filter to anticoagulation with fondaparinux sodium in patients with cancer and venous thromboembolism in a prospective randomized clinical trial. Support Care Cancer 20(11):2865–2872
Funding
This research was funded in part through the NIH/NCI, Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Coombs, C., Kuk, D., Devlin, S. et al. Outcomes after inferior vena cava filter placement in cancer patients diagnosed with pulmonary embolism: risk for recurrent venous thromboembolism. J Thromb Thrombolysis 44, 489–493 (2017). https://doi.org/10.1007/s11239-017-1557-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1557-2