Abstract
Coronary plaque rupture mediating acute ST segment elevation myocardial infarction (STEMI) is associated with a systemic inflammatory response. Whether early temporal changes in inflammatory biomarkers are associated with angiographic and electrocardiographic markers of reperfusion and subsequent clinical outcomes is unclear. In the APEX-AMI biomarker substudy, 376 patients with STEMI had inflammatory biomarkers measured at the time of hospital presentation and 24 h later. The primary outcome was the 90-day composite of death, shock, or heart failure. Secondary reperfusion outcomes were (1) worst least residual ST segment elevation (ST-E: <1 mm, 1 to <2 mm, ≥2 mm) and (2) post-percutaneous coronary intervention (PCI) TIMI flow grade (0/1/2 vs 3) and TIMI myocardial perfusion grade (TMPG 0/1 vs 2/3). The 90-day incidence of death, shock or heart failure was 21.3 % in this cohort. Electrocardiographic reperfusion (worst residual ST-E <1 mm, 1 to <2 mm, ≥2 mm) was associated with differences in 24 h change in N-terminal proB-type natriuretic peptide (NT-proBNP) (1192.8, 1332.5, 1859.0 ng/mL; p = 0.043) and the pro-inflammatory cytokines Interleukin (IL)-6 (14.0, 13.6, 22.1 pg/mL; p = 0.016), IL-12 (−0.5, −0.9, −0.1 pg/mL; p = 0.013), and tumor necrosis factor α (TNFα) (1.0, 0.6, 3.6 pg/mL; p = 0.023). Angiographic reperfusion (TMPG 0/1 vs 2/3) was associated with changes in median NT-proBNP (2649.3, 1382.7 ng/mL; p = 0.002) and IL-6 (28.7, 15.1; p = 0.040). After adjustment for baseline covariates, the 24 h change in the pro-inflammatory cytokine TNFα [hazard ratio (HR) 0.49; 95 % CI 0.26–0.95; p = 0.035] and the anti-inflammatory cytokine IL 10 (HR 1.41; 95 % CI 1.06–1.87; p = 0.018) were independently associated with the primary composite outcome. Successful coronary reperfusion was associated with less systemic inflammatory response and greater temporal inflammatory changes were independently associated with higher 90-day composite of death, shock, or heart failure. These findings provide support for an association between success of reperfusion, an acute STEMI inflammatory response and subsequent clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Successful electrocardiographic and angiographic reperfusion in ST segment elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PCI) are predictors of cardiac morbidity and mortality [1, 2]. N-terminal proB-type natriuretic peptide (NT-proBNP) is a validated and widely used prognostic biomarker that is lower in patients with successful electrocardiographic and angiographic reperfusion [3–7]. STEMI is also associated with changes in pro-inflammatory cytokines (interleukin [IL]-6, IL-1β, IL-12 and Tumor Necrosis Factor α [TNFα]), as well as anti-inflammatory cytokines (IL-1 receptor antagonist [IL-1ra], IL-4, IL-10), and chemokines (inducible protein [IP]-10 and interferon γ [IFNγ]) [8–11]. Studies reporting outcomes associated with many of these investigational inflammatory biomarkers in myocardial infarction are conflicting and cross-study comparisons are difficult given that inflammatory mediators were measured at different points in time including pre-and post-reperfusion. Importantly, it remains unclear whether successful reperfusion or clinical outcomes are associated with temporal changes in inflammatory mediators among STEMI patients. Improving the understanding of the relationship between the inflammatory response, success of coronary reperfusion, and clinical outcomes may improve STEMI prognostication and identify potential therapeutic targets directed towards reperfusion injury.
The Assessment of Pexelizumab in Acute Myocardial Infarction (APEX-AMI) trial biomarker substudy prospectively collected inflammatory biomarker samples at baseline and 24 h to evaluate the effect of a monoclonal antibody, pexelizumab, on the inflammatory response [12, 13]. In this contemporary population of STEMI patients undergoing primary PCI, we evaluated whether early changes (baseline and 24 h) in NT-proBNP, hsCRP, and inflammatory biomarkers are independently associated with (1) 90-day incidence of death, shock or heart failure and (2) angiographic and electrocardiographic markers of reperfusion.
Methods
Biomarker substudy and inflammatory markers of interest
The APEX-AMI (NCT00091637) trial design and results were previously reported [12, 14]. Briefly, it was an international, phase III placebo-controlled trial that compared pexelizumab (a humanized monoclonal antibody C5 complement inhibitor) versus placebo among STEMI patients undergoing primary PCI randomized within 6 h of symptom onset. The APEX-AMI biomarker substudy enrolled consenting patients from global angiographic and magnetic resonance imaging centers [13, 15]. This substudy initially planned to measure biomarkers in 4000 patients at the time of randomization and to collect 24 h samples in 1000 patients. The trial concluded earlier than planned for administrative reasons and budget considerations. The biomarker substudy population was enriched with a case–control approach wherein two controls were matched to each patient with a primary study outcome (death, shock, or heart failure) on age (within 2 years), sex, and myocardial infarct location [13]. Substudy participants had blood samples drawn: (1) immediately after randomization prior to study medication administration and PCI and (2) 24 h after randomization. After the blood clotted, samples were centrifuged and the serum was immediately frozen to −20 °C; then to −70 °C as soon as possible. Study samples were shipped on dry ice to the Duke Center for Human Genetics (Durham, NC, USA) for central storage, and then batch analyzed at a central laboratory (Montreal Heart Institute, Montreal, Quebec, Canada) at the end of the study. The results of the biomarkers substudy using samples drawn at the time of randomization were previously published [7].
Cytokines and chemokines were measured with Bio-Plex assays (LUMINEX 200, Luminex Corporation and Bio-Rad Laboratories Inc., Austin, TX). NT-proBNP and hsCRP were measured with electrochemiluminescence immunoassay (Roche Elecsys, Roche Diagnostics, Indianapolis, IN) and particle-enhanced immunonephelometry (Dade BehringNephelometer, Germany), respectively. The biomarkers of interest included NT-proBNP, hsCRP, pro-inflammatory cytokines (IL-1β, IL-6, IL-12, TNFα), anti-inflammatory cytokines (IL-1ra, IL-4 IL-10), chemokines (IP-10, IFNγ), and markers of myonecrosis (creatinine kinase [CK], CK-MB, troponin I, troponin T).
Study patients and core lab reperfusion analyses
All patients within the APEX-AMI biomarker sub-study with at least one pair (baseline and 24 h) of biomarkers of interest were included in the current study. Given no treatment related differences on clinical outcomes were observed with pexelizumab, the randomized treatment arms were pooled for this study.
All electrocardiograms were evaluated in central core labs blinded to treatment assignment and outcomes (Canadian VIGOUR Centre, Edmonton, Canada; Duke Clinical Research Institute, Durham, NC). Electrocardiographic reperfusion was evaluated as the worst least residual ST segment elevation (ST-E) on the 30 min post-PCI electrocardiogram using previously described methodology [2]. All angiograms were independently reviewed in a central lab (Cleveland Clinic, Cleveland, OH) by two blinded, experienced reviewers. Angiographic reperfusion was evaluated with post-PCI Thrombolysis In Myocardial Infarction (TIMI) flow grade and TIMI Myocardial Perfusion Grade (TMPG) according to previously described methodologies [16].
Outcomes
The primary analysis evaluated the association between the relative change in baseline and 24 h paired biomarkers (biomarker at 24 h-biomarker at baseline/biomarker at baseline) and outcomes of interest. We used relative change for the primary outcome to control for baseline biomarker levels as many of the investigational biomarkers included in this study have been associated with infarct size [15, 17, 18]. The primary outcome of interest was the 90-day composite of all-cause death, shock or heart failure (new or worsening). This composite outcome was a pre-specified secondary endpoint of the APEX-AMI trial, and all events were centrally adjudicated by a clinical events committee according to pre-specified criteria. Secondary outcomes were electrocardiographic and angiographic evidence of reperfusion. Electrocardiographic reperfusion was evaluated with worst least residual ST-E: <1 mm, 1 to <2 mm, ≥2 mm. Given small numbers with poor post PCI angiographic reperfusions, post-PCI TIMI flow was grouped as 0/1/2 versus 3 and TMPG was grouped as 0/1 versus 2/3.
Statistical methods
Continuous variables were summarized as median and Inter-quartile ranges and compared with the Wilcox rank-sum test. Categorical variables were summarized as frequency and percentages and compared with the Pearson Chi square test. The median changes in biomarkers between categories of electrocardiographic and angiographic reperfusion were compared with Kruskal–Wallis one-way analysis of variance.
The association of the relative change in each of the biomarkers with the 90-day composite outcome was assessed using a Cox proportional hazards model. Modeling assumptions of normality and linearity of the relative change measures were tested and logarithmic transformation was applied to improve the distribution and relationship. Otherwise, the variable was further categorized into discrete groups. Unadjusted and adjusted associations were summarized as hazard ratios (HR) and 95 % confidence intervals (CI). To assess the adjusted association of each biomarker with the outcome of interest, the multivariable model including the set of validated covariates and as parameterized in a previous sub-study of baseline biomarkers was applied [7]. The following factors were included in the model: age, sex, baseline Q wave, hospitalization to randomization time, COPD, diabetes, stroke, systolic blood pressure, diastolic blood pressure, serum creatinine, heart rate, Killip class, baseline total ST segment deviation [7]. To account for potential differences in the likelihood of being included in this paired biomarker subset, inverse probability weighting was used in these models. In an effort to mitigate the potential influence of post-randomization clinical changes on the 24 h change in the investigational biomarker levels we conducted a parallel analysis in which both baseline and post-baseline 24 h dynamic model variables were used as adjustment factors [19]. The adjustment factors in the 24 h based model included age, baseline systolic BP, baseline Killip class, baseline heart rate, creatinine, post-PCI TIMI flow grade, worst lead residual ( ≥2 vs <2 mm), and major cardiac rhythm disturbance. Given no clinical events were observed in the first 24 h in this dataset, no patients were excluded. The data analyses were performed using the SAS (Version 9.4; SAS Institute, Cary, NC).
All patients gave written informed consent to participate in the APEX-AMI trial and its biomarkers sub-study. The protocols were approved by the institutional review board or ethics committee of each participating site.
Results
In the APEX-AMI biomarker sub-study, 376 patients had at least one paired set of biomarker samples and outcome data. A study flow diagram is provided in Online Resource 1. Differences in baseline characteristics and 90-day clinical outcomes between APEX-AMI trial participants with and without baseline and paired biomarkers and those who did not are described in Online Resource 2. Substudy participants with paired biomarkers were older, more frequently women, and more often had a history of hypertension, Killip class >1, higher baseline creatinine, and a left anterior descending artery culprit lesion. Paired biomarker participants were less likely to be a current smoker. The 90-day composite of death, shock, or heart failure was significantly more frequent in the paired biomarker substudy population [n = 80 (21.3 %)] compared with those who were not [n = 506 (9.4 %)].
The median baseline and 24 h biomarker levels and the absolute and relative percent change of all biomarkers of interest are provided in Table 1. Levels of NT-proBNP, hsCRP, markers of myonecrosis, pro-inflammatory biomarkers (IL-1β, IL-6, TNFα), and anti-inflammatory cytokine IL-4 increased at 24 h compared to baseline values. Conversely, pro-inflammatory cytokine IL-2, anti-inflammatory cytokines (IL-1-ra, IL-10) and chemokines (IFNγ and IP-10) were lower at 24 h.
90-day clinical outcomes
The unadjusted and adjusted associations between relative biomarker change and the 90-day composite outcome of death, shock or heart failure are provided in Table 4. After adjustment for baseline covariates the pro-inflammatory cytokine, TNFα (HR 0.49; 95 % CI 0.26–0.95, p = 0.035) and the anti-inflammatory cytokine, IL-10 (HR 1.41; 95 % CI 1.06–1.87; p = 0.018), were independently associated with the primary outcome.
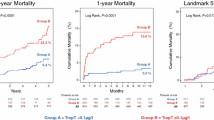
Electrocardiographic and angiographic reperfusion
The median absolute changes between baseline and 24 h biomarker levels stratified by worst residual ST-E are presented in Table 2 and Fig. 1. In this outcome enriched dataset, a majority of patients did not achieve complete electrocardiographic reperfusion (worst residual ST-E <1 mm [n = 103], 1 to <2 mm [n = 145] and ≥2 mm [n = 128]). Worst residual ST- E ≥2 mm was associated with significantly greater levels of NT-proBNP, and pro-inflammatory cytokines IL-6 and TNFα. Compared with those with lesser amounts of residual ST-E worst residual ST- E ≥2 mm was also associated with smaller median IL-12 reductions. All anti-inflammatory cytokines changes were numerically, but not statistically, less with residual ST-E ≥2 mm. CK and troponin I were significantly higher and CK-MB and troponin T also were numerically higher among patients with worst residual ST-E ≥2 mm. Relative changes between baseline and 24 h biomarker levels stratified by worst residual ST-E are provided in Online Resource 3.
Angiographic markers of reperfusion and their association with absolute changes in biomarkers levels are provided in Table 3. Median NT-proBNP levels were higher among patients with both poor post-PCI TIMI flow and TMPG. IL-6 was higher in participants with TMPG 0/1. All other pro-inflammatory cytokines, and hsCRP were numerically higher among patients without successful angiographic reperfusion. Markers of myonecrosis were numerically higher among patients without successful reperfusion. Boxplots of 24 h changes in NT-proBNP and IL-6 levels are displayed in Fig. 2 and median absolute changes by angiographic markers of reperfusion are provided in Online Resource 4.
Discussion
In this international dataset of STEMI patients undergoing primary PCI in whom serial measured inflammatory biomarkers were acquired, two novel finding emerged. First, successful coronary artery reperfusion by electrocardiographic measures was associated in time with changes in NT-proBNP and multiple pro-inflammatory cytokines (IL-6, IL-12, TNFα) but not with anti-inflammatory cytokines or chemokines evaluated in this study. Additionally, post-PCI TMPG was associated with temporal changes in NT-proBNP and IL-6. Second, the temporal relative changes in the pro-inflammatory cytokine TNFα and the anti-inflammatory cytokine IL-10 were independently associated with the 90-day composite of death, shock, or heart failure.
The pro-and anti-inflammatory cytokine responses to myocardial infarction have been well described, but the in vivo response to coronary reperfusion has remained less clear [20–22]. We observed that NT-proBNP and the pro-inflammatory cytokines IL-6, IL-12, and TNFα absolute changes were associated with electrocardiographic reperfusion and NT-proBNP was associated with post-PCI TMPG. IL-6 and TNFα are not normally expressed in healthy myocardium and synthesis has been shown to be upregulated in infarcted, peri-infarct and non-infarcted tissue zones following myocardial infarction, while IL-12 is expressed in atherosclerotic plaques [9, 23–25]. Recognizing that IL-6 and TNFα are proposed mediators of post-infarction cardiac remodeling and that IL-12 may accelerate further cardiac atherosclerosis, our findings may have implications for future efforts aimed at understanding the pathophysiologic link between reperfusion, the systemic inflammatory response, and both post-infarction heart failure and re-infarction [9, 26]. Although a causal effect cannot be inferred from the present analysis, our results suggest that myocardial reperfusion may be associated with important mediators of the temporal inflammatory response.
There are conflicting published associations between inflammatory cytokines, chemokines and outcomes after acute coronary syndromes [7, 27, 28]. We observed that a 24 h increase in the pro-inflammatory cytokine TNFα was associated with less 90-day death, shock or heart failure while a non-significant trend was observed with the anti-inflammatory cytokine IL-4 and chemokine IFNγ. Given inflammatory markers are correlated with myocardial infarct size, this analysis controlled for biomarker levels at the time of presentation and evaluated temporal changes in inflammatory biomarkers [29, 30]. IL-4 is known to attenuate the post-infarction pro-inflammatory of IL-1 and IL-6 response. This is first study to report an association between temporal changes in these inflammatory markers and clinical outcomes [30]. IL-10, an anti-inflammatory cytokine that is expressed in ischemic and reperfused myocardium, is thought to have a protective effect by inhibiting the production of pro-inflammatory cytokines (IL-1α, IL-1β, IL-6 < IL-8, IL-12, TNFα) and metalloproteinases [31–33]. The observed positive association between temporal changes in IL-10 and 90-day clinical outcomes should be carefully interpreted in the context of studies that have reported that the ratio of pro:anti-inflammatory cytokines (and not absolute levels) are predictive of clinical events [34–36]. However, this inverse association with TNFα is both unexpected and potentially novel. TNFα mediates the pro-inflammatory effects through IL-6 release by vascular smooth muscle cells, which leads to increased leukocyte recruitment, platelet aggregation, apoptosis and cardiac remodeling [8, 9, 37]. This suggests that a temporal increase in TNFα should be associated with adverse clinical outcomes; however, other pre-clinical studies have suggested potential myocardial protective effects. TNFα expression has been found in both the peri-infarct and non-infarcted zone of the heart, suggesting a possible role in myocardial repair. Consistent with this hypothesis, double TNFα receptor knockout mice have increased myocardial apoptosis [32, 38, 39]. Although the pro-inflammatory TNFα has well reported deleterious physiologic effects, the in vivo effects of this inflammatory cytokine are incompletely understood and based on our results, we hypothesize that TNFα may have a net cardioprotective effect.
The present findings have implications for future biomarker research among patients with STEMI. The significant association between successful coronary reperfusion and temporal changes in inflammatory biomarker levels suggests that the timing of biomarker sampling relative to reperfusion is an important methodical consideration. We hypothesize that differences in biomarker sample timing may, in part, explain some the conflicting associations between post-infarction inflammatory biomarker levels and clinical outcomes reported in the literature. We also acknowledge that the biomarkers that were significantly associated with reperfusion were not significantly associated with clinical outcomes and the timing of biomarker sampling was remote form the 90-day clinical outcomes, thus precluding causal inferences. The modest sample size may have limited the ability to detect important associations and further study in a larger dataset is required. Finally, the significant associations between changes in inflammatory biomarkers and clinical outcomes suggest that some serial evaluation of some biomarkers may contribute incremental information to dynamic clinical prediction models that have been shown to improve risk discrimination [19, 40].
Limitations and strengths
The study included a modest sample size and it may be underpowered to detect clinically important associations; however, this is the largest known dataset of paired inflammatory biomarkers in STEMI patients undergoing reperfusion. The APEX-AMI paired biomarker substudy enrolled a high risk subset of STEMI patients, thus the results may not be generalizable to all STEMI patients. Since multiple biomarkers (and their associations) were evaluated without adjustment for multiple comparisons, statistically significant findings should be considered hypothesis generating. The 24 h markers of myonecrosis were not routinely recorded; thus, peak markers were used in the paired analyses. The present data are a subset of a biomarker substudy, given the small sample size we did not explore if previously published findings were consistent in this subset population [7]. Lastly, the study pooled treatment arms of the APEX-AMI study. Pexelizumab had neither an effect on clinical outcomes nor any of the study biomarkers with except IL-6 (24-levels were attenuated by pexelizumab treatment) [41].
Conclusions
In an international study population with centrally adjudicated outcomes, we observed that temporal changes in the pro-inflammatory cytokines IL-6, IL-12, and TNFα levels were associated with electrocardiographic evidence of reperfusion and temporal changes in IL-6 was associated with angiographic reperfusion. The composite of death, shock, or heart failure was independently and negatively associated with the 24 h change in the pro-inflammatory cytokine TNFα and positively associated with the anti-inflammatory cytokine IL-10. These findings provide potential clinical insights into the potential associations between reperfusion success and the inflammatory response in STEMI, with potential implications for post-infarction cardiac remodeling. Future research is required to elucidate whether reperfusion modulation of the systemic inflammatory response is causally linked to post-STEMI outcomes.
References
Morishima I, Sone T, Okumura K et al (2000) Angiographic no-reflow phenomenon as a predictor of adverse long-term outcome in patients treated with percutaneous transluminal coronary angioplasty for first acute myocardial infarction. J Am Coll Cardiol 36(4):1202–1209
Buller CE, Fu Y, Mahaffey KW et al (2008) ST segment recovery and outcome after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation 118(13):1335–1346
Grabowski M, Filipiak KJ, Malek LA et al (2007) Admission B-type natriuretic peptide assessment improves early risk stratification by Killip classes and TIMI risk score in patients with acute ST elevation myocardial infarction treated with primary angioplasty. Int J Cardiol 115(3):386–390
Ezekowitz JA, Theroux P, Chang W et al (2006) N-terminal pro-brain natriuretic peptide and the timing, extent and mortality in ST elevation myocardial infarction. Can J Cardiol 22(5):393–397
Mega JL, Morrow DA, De Lemos JA et al (2004) B-type natriuretic peptide at presentation and prognosis in patients with ST segment elevation myocardial infarction: an entire-TIMI-23 substudy. J Am Coll Cardiol 44(2):335–339
Damman P, Beijk MAM, Kuijt WJ et al (2011) Multiple biomarkers at admission significantly improve the prediction of mortality in patients undergoing primary percutaneous coronary intervention for acute ST segment elevation myocardial infarction. J Am Coll Cardiol 57(1):29–36
van Diepen S, Newby LK, Lopes RD et al (2013) Prognostic relevance of baseline pro- and anti-inflammatory markers in STEMI: an APEX AMI substudy. Int J Cardiol 168(3):2127–2133
Alam SE, Nasser SS, Fernainy KE, Habib AA, Badr KF (2004) Cytokine imbalance in acute coronary syndrome. Curr Opin Pharmacol 4(2):166–170
Nian M, Lee P, Khaper N, Liu P (2004) Inflammatory cytokines and postmyocardial infarction remodeling. Circ Res 94(12):1543–1553
Herskowitz A, Choi S, Ansari AA, Wesselingh S (1995) Cytokine mRNA expression in postischemic/reperfused myocardium. Am J Pathol 146(2):419–428
Smith DA, Irving SD, Sheldon J, Cole D, Kaski JC (2001) Serum levels of the antiinflammatory cytokine interleukin-10 are decreased in patients with unstable angina. Circulation 104(7):746–749
The Apex-AMI Investigators (2007) Pexelizumab for acute ST-elevation myocardial infarction in patients undergoing primary percutaneous coronary intervention. JAMA 297(1):43–51
Mahaffey KW, Reist CJ, Fu Y et al (2008) Integrating ancillary studies in a large clinical trial: the design and rationale of the APEX library. Contemp Clini Trials 29(6):887–895
Armstrong PW, Adams PX, Al-Khalidi HR et al (2005) Assessment of pexelizumab in acute myocardial infarction (APEX AMI): a multicenter, randomized, double-blind, parallel-group, placebo-controlled study of pexelizumab in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Am Heart J 149(3):402–407
van Diepen S, Roe M, Lopes R et al (2012) Baseline NT-proBNP and biomarkers of inflammation and necrosis in patients with ST segment elevation myocardial infarction: insights from the APEX-AMI trial. J Thromb Thrombolysis 34(1):106–113
Brener SJ, Moliterno DJ, Aylward PE et al (2008) Reperfusion after primary angioplasty for ST-elevation myocardial infarction: predictors of success and relationship to clinical outcomes in the APEX-AMI Angiographic Study. Eur Heart J 29(9):1127–1135
Koten K, Hirohata S, Miyoshi T et al (2008) Serum interferon-gamma-inducible protein 10 level was increased in myocardial infarction patients, and negatively correlated with infarct size. Clin Biochem 41(1–2):30–37
Patti G, Mega S, Pasceri V et al (2005) Interleukin-1 receptor antagonist levels correlate with extent of myocardial loss in patients with acute myocardial infarction. Clin Cardiol 28(4):193–196
Westerhout CM, Pieper KS, James SK et al (2013) Dynamic modeling of 90-day mortality in ST elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Am Heart J 165(3):354–362
Biasucci LM, Liuzzo G, Fantuzzi G et al (1999) Increasing levels of interleukin (IL)-1Ra and IL-6 during the first two days of hospitalization in unstable angina are associated with increased risk of in-hospital coronary events. Circulation 99(16):2079–2084
Heeschen C, Dimmeler S, Hamm CW et al (2003) Serum level of the antiinflammatory cytokine interleukin-10 is an important prognostic determinant in patients with acute coronary syndromes. Circulation 107(16):2109–2114
Lee KW, Lip GYH, Tayebjee M, Foster W, Blann AD (2005) Circulating endothelial cells, von Willebrand factor, interleukin-6, and prognosis in patients with acute coronary syndromes. Blood 105(2):526–532
Deten A, Volz HC, Briest W, Zimmer H-G (2002) Cardiac cytokine expression is upregulated in the acute phase after myocardial infarction experimental studies in rats. Cardiovasc Res 55(2):329–340
Irwin MW, Mak S, Mann DL et al (1999) Tissue expression and immunolocalization of tumor necrosis factor-α in postinfarction dysfunctional myocardium. Circulation 99(11):1492–1498
Uyemura K, Demer LL, Castle SC et al (1996) Cross-regulatory roles of interleukin (IL)-12 and IL-10 in atherosclerosis. J Clin Invest 97(9):2130–2138
Hauer AD, Uyttenhove C, de Vos P et al (2005) Blockade of interleukin-12 function by protein vaccination attenuates atherosclerosis. Circulation 112(7):1054–1062
Ridker PM, Rifai N, Pfeffer M, Sacks F, Lepage S, Braunwald E (2000) Elevation of tumor necrosis factor-alpha and increased risk of recurrent coronary events after myocardial infarction. Circulation 101(18):2149–2153
Valgimigli M, Ceconi C, Malagutti P et al (2005) Tumor necrosis factor-alpha receptor 1 is a major predictor of mortality and new-onset heart failure in patients with acute myocardial infarction: the cytokine-activation and long-term prognosis in myocardial infarction (C-ALPHA) study. Circulation 111(7):863–870
Puhakka M, Magga J, Hietakorpi S et al (2003) Interleukin-6 and tumor necrosis factor alpha in relation to myocardial infarct size and collagen formation. J Cardiac Fail 9(4):325–332
Szkodzinski J, Hudzik B, Osuch M et al (2011) Serum concentrations of interleukin-4 and interferon-gamma in relation to severe left ventricular dysfunction in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart Vessels 26(4):399–407
Frangogiannis NG, Mendoza LH, Lindsey ML et al (2000) IL-10 is induced in the reperfused myocardium and may modulate the reaction to injury. J Immunol 165(5):2798–2808
Frangogiannis NG, Smith CW, Entman ML (2002) The inflammatory response in myocardial infarction. Cardiovasc Res 53(1):31–47
Lacraz S, Nicod LP, Chicheportiche R, Welgus HG, Dayer JM (1995) IL-10 inhibits metalloproteinase and stimulates TIMP-1 production in human mononuclear phagocytes. J Clin Invest 96(5):2304–2310
Chalikias GK, Tziakas DN, Kaski JC et al (2005) Interleukin-18: interleukin-10 ratio and in-hospital adverse events in patients with acute coronary syndrome. Atherosclerosis 182(1):135–143
Kilic T, Ural D, Ural E et al (2006) Relation between proinflammatory to anti-inflammatory cytokine ratios and long-term prognosis in patients with non-ST elevation acute coronary syndrome. Heart 92(8):1041–1046
Waehre T, Halvorsen B, Damas JK et al (2002) Inflammatory imbalance between IL-10 and TNFalpha in unstable angina potential plaque stabilizing effects of IL-10. Eur J Clin Invest 32(11):803–810
Woods A, Brull DJ, Humphries SE, Montgomery HE (2000) Genetics of inflammation and risk of coronary artery disease: the central role of interleukin-6. Eur Heart J 21(19):1574–1583
Jacobs M, Staufenberger S, Gergs U et al (1999) Tumor necrosis factor-alpha at acute myocardial infarction in rats and effects on cardiac fibroblasts. J Mol Cell Cardiol 31(11):1949–1959
Kurrelmeyer KM, Michael LH, Baumgarten G et al (2000) Endogenous tumor necrosis factor protects the adult cardiac myocyte against ischemic-induced apoptosis in a murine model of acute myocardial infarction. Proc Natl Acad Sci USA 97(10):5456–5461
Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286(14):1754–1758
Martel C, Granger CB, Ghitescu M et al (2012) Pexelizumab fails to inhibit assembly of the terminal complement complex in patients with ST elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am Heart J 164(1):43–51
Acknowledgments
We would like thank Dr. Cynthia M. Westerhout for her academic review and Ms. Lisa Soulard for copy-editing this manuscript.
Funding
The APEX-AMI trial, from which this work was derived, was supported by a research grant jointly funded from Procter & Gamble (Cincinnati, OH, USA) and Alexion Pharmaceuticals (Cheshire, CT, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sean van Diepen, Wendimagegn G. Alemayehu, Yinggan Zheng: The authors declare they have no conflicts of interest; L. Kristin Newby, Christopher B. Granger: disclosures are publically available at https://www.dcri.org/about-us/conflict-of-interest; Kenneth W. Mahaffey: disclosure is publicly available at https://med.stanford.edu/profiles/kenneth-mahaffey?tab=research-and-scholarship; Paul W. Armstrong: disclosure is publically available at http://www.vigour.ualberta.ca/About/RelationshipsWithIndustry.aspx; Pierre Theroux has received a grant from the trial sponsor to lead all the Bio-Plex assays (LUMINEX 200).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
van Diepen, S., Alemayehu, W.G., Zheng, Y. et al. Temporal changes in biomarkers and their relationships to reperfusion and to clinical outcomes among patients with ST segment elevation myocardial infarction. J Thromb Thrombolysis 42, 376–385 (2016). https://doi.org/10.1007/s11239-016-1390-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1390-z