Abstract
Venous thromboembolism (VTE) is a life-threatening medical disorder worldwide. A great deal of evidence suggests that prevalence of VTE varies significantly among ethnic populations, with consistently lower incidence found in Asians. While the distribution of genetic risk factors may vary among races, genetic risk factors can play a major role among individuals with different genetic backgrounds. Two clinically evaluated low-frequency genetic mutations that predispose to VTE—the factor V Leiden mutation and prothrombin G20210A mutation—are found predominantly in Caucasians, and virtually never in Asians. The findings of a recent genetic study of VTE in northeast Asians, which greatly advanced our knowledge in this area, indicate that the most frequent genetic risk factors for VTE in northeast Asians can be attributed to a dysfunction of the protein C anticoagulant system. Several low-frequency genetic mutations, PROS1 p.Lys196Glu in Japanese and PROC p.Arg189Trp and p.Lys193del in Chinese, are significantly associated with increased risk for VTE, with odds ratio more than 2 through the reduced protein C anticoagulant activity. Construction of a multifactorial model based on the genetic risk factors in the protein C anticoagulant system could facilitate genetic counseling for VTE risk in these populations. The influence of prevalent genetic mutations on the risk of VTE should be further investigated in Asian countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE), a multifactorial disorder consisting of deep venous thrombosis (DVT) and pulmonary embolism (PE), represents a major thrombotic medical disorder worldwide. Despite acknowledged problems with different criteria and misclassification in determining VTE, there is strong evidence that the prevalence of VTE varies significantly among different ethnic/racial populations. Among the few studies with sufficiently diverse ethnic population samples to make direct comparisons [1–4] (Table 1), the most notable findings were from epidemiological studies based on ethnically diverse populations in California [1.3.4]. They suggested that the annual incidence of idiopathic DVT in persons over 18 years is higher among African Americans (29 per 100,000 individuals per year) than among Caucasians (23 per 100,000 individuals per year), is significantly lower among Hispanic populations (14 per 100,000 individuals per year), and is strikingly lower among Asian-Pacific Islanders (6 per 100,000 individuals per year) [1]. Population-based epidemiological studies of VTE are relatively rare in Asians. Recently, Sakuma et al. [5] reported the annual estimated incidence of PE and DVT in Japanese to be 6.19 and 11.55 patients per 100,000 individuals per year, respectively. Lee et al. [6] analyzed the incidence of symptomatic VTE in almost the entire population of Taiwan. The incidence of PE and DVT among Taiwanese adults was 4.8 and 16.5 per 100,000, respectively, which is lower than among Caucasians and African-Americans, and similar to that of other Asians. Nevertheless, prevalence of PE and DVT in Asia may be increasing with improvements in diagnosis and access to healthcare [7].
VTE is recognized to be a multifactorial, complex disorder, which results from an interaction between environmental, clinical, and genetic risk factors. While racial differences in the incidence of VTE have been well established, interactive risk factors also vary by race [8]. Generally accepted environmental and clinical risk factors for VTE—such as obesity and access to complex surgery and cancer treatments—as well as prevalence of VTE risk factors such as human immunodeficiency virus and the sickle cell trait, are likely to emerge as important mediators of the racial difference in VTE [7]. Data from studies in Asian patients indicate a lower incidence of symptomatic VTE complicating trauma, immobilization, surgery, and/or use of thalidomide [7]. In addition to these well-established risk factors for VTE, it is conceivable that genetic risk factors may vary and play a major role in the different distribution of VTE among people from different genetic backgrounds [8].
The involvement of genetic factors in increased risk for VTE was confirmed in family-based studies in Caucasians, where genetics were thought to account for up to 60 % of risk [9]. Well-established genetic risks for VTE include increased pro-coagulant activities and hereditary deficiencies of natural anticoagulants. Two well-known and clinically evaluated genetic mutations associated with VTE are factor V Leiden mutation (factor V p.Arg506Gln mutation) and prothrombin G20210A mutation, which are found predominantly in populations with European ancestry, and are virtually non-existent in Asians without European admixture [8]. The relatively lower incidence of VTE in Asians compared to Caucasians may partly be due to the lower prevalence of these predisposing genetic factors.
Recently, in northeast Asian populations, where VTE incidence appears low, the most represented genetic risk factors are congenital deficiency of natural anticoagulants, especially genetic deficiency concerning the dysfunction of the protein C anticoagulant system [10]. The purpose of this review is to discuss the prevalence of this deficiency in Asians, and to evaluate the influence of genetic mutations in the protein C anticoagulant system on the risk of VTE in these populations. In this review, the A of the ATG initiator Met codon is denoted as nucleotide +1, and the initial Met residue is denoted as amino acid +1 [11].
Protein C anticoagulant system
Natural anticoagulation in healthy individuals is primarily achieved through the actions of the anticoagulant systems, which include antithrombin, tissue factor pathway inhibitor, protein C, and protein S. Antithrombin plays a major role through the inhibition of thrombin and factor Xa. Tissue factor pathway inhibitor performs its physiological and pathological roles through the inhibition of factor Xa and factor VIIa-tissue factor complex. Unlike these protease inhibitors, the inactive serine-protease zymogen, protein C, must first be activated by thombomodulin (TM)-bound thrombin on the endothelial surface, with the help of the endothelial cell protein C receptor (EPCR); this produces activated protein C (APC) that then proteolytically inactivates factors Va and VIIIa in the presence of protein S. Protein S also stimulates factor Xa inhibition by tissue factor pathway inhibitor, resulting in the down-regulation of the extrinsic coagulation pathway. Thus, the protein C anticoagulant system, consisting of protein C, protein S, TM, and EPCR, regulates the balance between procoagulant and anticoagulant activities. Thrombus formation occurs when this balance is disturbed.
Deficiency of natural anticoagulants and prevalence in Asians
Deficiencies of proteins C and S result in the dysfunction of the protein C anticoagulant system. Hereditary protein C deficiency is usually inherited as an autosomal dominant trait. It is associated with an increased risk of VTE, and is thus considered hereditary thrombophilia. Protein C deficiency is classified into type I (low plasma concentration of both functional and immunological protein C) and type II (low concentration of functional protein C with normal antigen concentration). The inheritance pattern of protein S deficiency is usually autosomal-dominant. Protein S deficiency is classified as type I (quantitative deficiency of both activity and antigen concentration), type II (qualitative deficiency characterized by decreased activity with normal antigen concentration), or type III (normal concentration of total protein S and low concentration of free protein S).
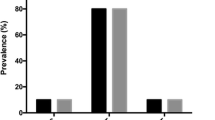
The frequency of deficiencies of protein C, protein S, and antithrombin in VTE patients of Western ethnicity was reported to be 1.4–8.6, 1.4–7.5, and 0.5–4.9 %, respectively [12]. Compared with Caucasians, deficiencies of protein C and protein S in Asians were higher in both the general population and in VTE patients [13–23]. As shown in Table 2, the most prevalent deficiencies in Asian VTE patients were protein S deficiency, followed by protein C deficiency. A report from Hong Kong claimed that as many as 42 % of Chinese VTE patients have reduced activity of the protein C anticoagulant system [13]. In the Taiwanese population, about 50 % of VTE patients showed reduced activity of protein C and protein S [24]. In the Japanese population, the frequency of mutations of the protein C gene was almost three times higher than in Caucasian patients, and protein S deficiency was approximately 5–10 times more prevalent in Japanese VTE patients [20]. These studies suggested that Asian individuals have thrombophilias that differ from those of Caucasians, with a high likelihood of thrombophilia being due to an abnormality of protein C or protein S. They also indicate that there may be an overall higher prevalence of abnormality in protein C or protein S in Asian populations in general, and that a higher occurrence of this class of genetic risk factors may be expected in patients with VTE from the same genetic background [8].
Genetic mutations in the protein C anticoagulant system with VTE in Asians
Recently, several genetic mutations that are associated with a reduction of protein C anticoagulant activity and increased risk for VTE have been confirmed in the protein C anticoagulant system in Japanese and Chinese populations. While differences in VTE by race due to genetic predisposition will probably always be present, understanding the racially specific genetic risk factors for VTE can provide important information about etiological mechanisms, as well as novel therapeutic targets.
PROS1 p.Lys196Glu as a genetic risk of VTE in Japanese
Approximately 8–47 % of Japanese and Chinese individuals who develop VTE have reduced activities of protein S (Table 2). At present, more than 200 mutations have been described in the protein S gene (PROS1), and large deletions/duplications can also be identified as causes of protein S deficiency [25, 26]. The most common PROS1 mutation is a p.Lys196Glu mutation (rs121918474, c.586A>G, protein S Tokushima, p.Lys155Glu in the mature protein numbering), which accounts for 9–30 % of protein S molecule abnormalities in people of Japanese decent [10, 20, 27–29].
An abnormal protein S molecule with the p.Lys196Glu mutation was identified in thrombophilic Japanese patients almost simultaneously by two independent groups in 1993 [30, 31]. It is a missense mutation that causes Lys196 to be replaced by Glu, formerly known as protein S Tokushima. This mutation is present in the second EGF-like domain of the protein S molecule. The allele frequency is approximately 0.9 % in the Japanese population, which means that 1 out of 55 Japanese carries the mutation as a heterozygote [29, 32, 33]. The frequency is much higher, approximately 6–10 % among DVT patients (Table 3) [20, 28, 32]. While homozygotes for this mutation have been identified in VTE patients, with a prevalence of one homozygote out of approximately 85 patients [20, 32], they have thus far not been identified in the general population [29]. The protein S p.Lys196Glu mutation can also be found in VTE patients with congenital protein C deficiency, thereby facilitating the development of VTE [34], and is frequently seen in VTE patients who are pregnant [35]. So far, 3 independent case–control studies, all performed in Japan, have reached the conclusion that the protein S p.Lys196Glu mutation is a risk factor for VTE, with odds ratio between 3.74 and 8.56 [20, 28, 32] (Table 3).
A genotype–phenotype study of the general Japanese population showed that individuals heterozygous for the mutant Glu-allele had a 16 % mean reduction in plasma protein S anticoagulant activity compared to wild-type individuals [27]. A patient with DVT who is a homozygote of protein S p.Lys196Glu mutation showed 35 % protein S anticoagulant activity and 37 % specific anticoagulant activity (activity/amount of protein S) [20]. In vitro studies using the recombinant proteins have shown that mutant protein S with Glu196 had impaired APC cofactor function [36]. Plasma protein S activities in carriers of the p.Lys196Glu mutation showed reduced activity as described, but antigen levels were within normal limits [27, 30, 31].
The protein S p.Lys196Glu mutation is race-specific; so far this mutation has not been identified in any population other than Japanese. Chinese and Koreans populations, despite being geographically and genetically close to Japanese, did not carry this mutation [37]. Thus, the protein S p.Lys196Glu mutation must be a recent occurrence and fixed within the Japanese population.
PROC p.Arg189Trp and p.Lys193del as genetic risks of VTE in Chinese
At least 161 different protein C gene (PROC) mutations have been reported, and most of them are missense mutations. The predominant genetic defects in the PROC gene may be different for different races. Recently, the p.Arg189Trp mutation of protein C (rs146922325, c.565C>T, p.Arg147Trp in the mature protein numbering) was reported by two independent studies to be not only the most frequent variant for protein C deficiency but also a significant risk factor for VTE in Chinese populations [38, 39]. This missense mutation was initially described in an American patient with symptomatic protein C deficiency [40], and was later reported in an asymptomatic individual [41]. Although a rare mutation in Western populations, the p.Arg189Trp mutation was present in approximately 0.9 % of the general Chinese population (Table 3) [38, 39]. The heterozygous state of the p.Arg189Trp mutation is associated with decreased plasma functional activity and a relatively normal protein C antigen level, indicating type II protein C deficiency. This mutation was identified in almost half of the probands with hereditary protein C deficiency [38, 39]. First-degree relatives bearing this variant had an 8.8-fold increased risk of VTE [39]. Two independent population-based case–control studies showed the odds ratio of VTE in carriers of the variant ranged from 5 to 7 (Table 3) [38, 39]. The p.Arg189Trp mutation is located at the C-terminal region of the light chain adjacent to the EGF-2 like domain, and may impair the interaction of protein C with other molecules suggesting that Arg189 may constitute an exosite for the binding of factor Va and/or the thrombin–thrombomodulin complex. Further functional studies are needed to elucidate the deleterious effect of this mutation on the activation of protein C and the inactivation of factor Va by APC. Data on the prevalence of this mutation and the thrombotic risk associated with it in other populations (especially other Asian populations) are still quite limited, and should be further evaluated.
Recently, using coagulation screening tests, resequencing, and a case–control study, Tang et al. revealed that the PROC p.Lys193del mutation (rs199469469, c.574_576del, p.Lys151del in the mature protein numbering) was associated with both decreased protein C anticoagulant activity and an increased risk of VTE in Chinese, with an odds ratio of 2.7 (Table 3) [23]. The nomenclature of one amino acid deletion in this case is somewhat complicated, as positions 192 and 193 of protein C are both Lys and one of the Lys residues is deleted in this case. We call the mutation the “p.Lys193del” according to the recommendation of the Human Genome Variation Society [11]. This variant was first described in three Japanese patients who suffered from protein C deficiency [42]. In other studies on protein C and protein S deficiencies in Japanese individuals, this mutation was identified in 2 of 85 VTE patients, as well as in 1 of 30 healthy individuals in one study [20], and in 4 of 173 VTE patients in another [34]. Despite being identified as a rare genetic mutation in Japanese, the contribution of the variant to the risk for VTE was not further evaluated in the general Japanese population. Another recent study found that the prevalence of p.Lys193del mutation was 2.36 % in the general Chinese population [23]. It was identified in 68 of 1,003 VTE patients (6.78 %) and in 25 of 1,031 healthy individuals (2.42 %), therefore, it conferred an increased risk of VTE with an adjusted odds ratio of 2.7 (Table 3) [23]. Patients with the p.Lys193del mutation showed lower anticoagulant activity of protein C, but relatively normal amidolytic activity compared to the wild-type carriers [23, 34, 42]. The anticoagulant activity of the recombinant mutant protein C showed about 40 % of the wild-type, consistent with the value of plasma from the homozygous patient [23]. Although this mutation has been reported previously in Japanese populations, further studies are needed to evaluate its prevalence in other Asians, and to determine whether this polymorphism is a risk factor for VTE in other Asian populations.
Some other PROC mutations were also reported in VTE patients from Asia [39, 40, 43–45]. Both protein C p.Arg211Trp and p.Met406Ile (p.Arg169Trp and p.Met364Ile in the mature protein numbering), which are related to type I protein C deficiency, were first reported in Japanese patients with VTE [43, 44]. Protein C p.Arg211Trp is a recurrent mutation occurring at a CpG mutation hotspot at the thrombin cleavage site in the heavy chain; it has also been described in Caucasian patients with VTE. It was reported to account for about 10 % of PROC mutations in Japanese [45]. In contrast, p.Met406Ile, which occurs at a non-CpG site of the serine protease domain, has been described exclusively in Japan, accounting for ~8 % of PROC mutations in Japanese VTE patients [45]. In resequencing the PROC gene in probands of protein C deficiency, 8 novel coding sequence mutations contributed to 7 amino acid exchanges; 3 evidently detrimental novel null mutations were also supposed to contribute to the development of VTE in Chinese [39].
THBD mutations as VTE risk in Asians
Thrombomodulin (TM encoded by THBD), another critical component of the protein C anticoagulant system, is a transmembrane glycoprotein of 557 amino acids, and is expressed mainly on the endothelial cells. TM binds thrombin and alters its substrate specificity. The resulting TM–thrombin complex efficiently catalyzes protein C activation. The intron-less human THBD gene is 3.6 kb in length. Based on the important anticoagulant role of TM, mutations within THBD could predispose individuals to VTE. In addition, THBD mutations may affect the plasma-soluble TM level. Several studies have focused on the influence of genetic polymorphisms in THBD on soluble TM level and VTE. One study conducted in the USA found mutations—including c.127G>A (p.Ala43Thr), c.1418C>T (p.Ala473Val), c.1752C deletion, and c.3645A>G—were not associated with VTE [46]. An association study of the Japanese population that included 2,247 individuals showed that c.2729A>C in tight linkage disequilibrium with c.1418C>T (p.Ala473Val) was associated with the soluble TM level [47]. This mutation also showed a marginal association with VTE, but only in males (Table 3).
A recent large study of the Chinese population showed an association of the soluble TM levels with c.−151G>T in THBD (Table 3) [48]. Furthermore, this genetic mutation increased risk of VTE. The study enrolled 1,304 individuals with VTE and 1,334 age- and sex-matched controls. By resequencing and genotyping of the THBD gene, the study showed that c.−151G>T in THBD could cause a predisposition to VTE, with a 2.8-fold increased risk of developing VTE in the population and a 3.42-fold increased risk of VTE in the family [48]. The prevalence of this variant in the Chinese population was 0.97 %, indicating an allele frequency of 0.49 %. Compared with the wild-type allele, the c.−151G>T mutation significantly reduced the reporter gene-expression level in cultured cells [48].
In addition, rare nonsynonymous mutations, p.Ser190Trp, p.Ser212Ter, p.Leu220Ter, and p.Asp126Tyr in THBD were also identified in 108 thrombophilic individuals with VTE [48]. The prevalence and relative risk of VTE with these mutations in other populations, especially in Asians, will require further evaluation.
The extensive resequencing studies on THBD in VTE patients revealed yet another aspect of the THBD mutations, that is, a possible link between the nonsynonymous mutations and atypical hemolytic uremic syndrome (aHUS), a type of microangiopathy characterized by uncontrolled complement activation. One of the causative genes for aHUS is THBD [49]. In vitro, TM binds to C3b and complement factor H and negatively regulates the complement by accelerating complement factor I-mediated inactivation of C3b. The TM mutations were less effective than wild-type TM in enhancing factor I-mediated inactivation of C3b. Thus, some missense mutations of TM are characterized as causative for the development of aHUS [49]. A missense mutation, p.Asp486Tyr, in the Ser/Thr rich domain of TM, which has been identified in both VTE patients and controls [46–48], was characterized as a causative mutation for aHUS. Missense mutations in the lectin-like domain of TM are also reportedly causative for aHUS. Thus, nonsynonymous mutations in THBD would affect not only VTE but also aHUS to a certain degree.
PROCR mutations as VTE risk in Asians
On the pathway of the protein C anticoagulant system, protein C is activated on the endothelial surface by the membrane-bound TM–thrombin complex. Protein C activation is enhanced approximately 20-fold when protein C binds to the endothelial protein C receptor (EPCR) encoded by PROCR. EPCR also serves as a cellular binding site for factor VII and factor VIIa. A soluble form of this receptor (sEPCR) in plasma inhibits both APC activity and protein C activation by competing for protein C with membrane-bound EPCR. These findings suggest an important role for EPCR in VTE.
Several studies have reported that the PROCR p.Ser219Gly mutation (rs867186, c.655A>G) present within the membrane-spanning region reduced plasma sEPCR levels to 56–87 % [50]. Significantly higher levels of factor VII, factor VIIa, and downstream markers of activated coagulation in the extrinsic pathway (factor IX activation peptide, factor X activation peptide), and prothrombin F1 + 2 were also identified in Gly carriers, compared to Ser/Ser [51]. Evidence for the association between the p.Ser219Gly mutation and VTE is conflicting in ethnically diverse populations. A recent meta-analysis in 4,821 VTE patients and 6,070 controls found a significant association of this mutation with VTE [50]. Under an additive genetic model, the odds of VTE increased by a factor of 1.22 for every additional copy of the G allele in all ethnic populations, suggesting a moderate effect for VTE. The reported frequency of the G allele in northeast Asians is approximately 10 % [52, 53]. Thus far, only two independent, small-scale studies of Chinese populations have reported a significant association between the p.Ser219Gly mutation and VTE in Asian populations (Table 3) [52, 53]. Further studies restricted to idiopathic VTE patients in Asian might facilitate the positive association of this variant.
Perspectives
The genetic mutations in the protein C anticoagulant system (PROS1 p.Lys196Glu, PROC p.Arg189Trp, PROC p.Lys193del, and THBD c.−151G>T) associated with risk of VTE in Asians are all classified into low-frequency variations with allele frequencies of less than 5 %. Three genetic mutations in the protein C anticoagulant system (PROC p.Arg189Trp, PROC p.Lys193del, and THBD c.−151G>T) were detected concurrently in the Chinese population, with a respective frequency of 0.90, 2.40, and 0.97 %, and a respective odds ratio for VTE of 6.06, 2.84, and 2.80. Their estimated population-attributable risks were therefore calculated to be 4.67, 4.14, and 1.48 %, respectively [48]. Taken together, about 10 % of VTE events in the general Chinese population could be explained by these mild to moderate thrombophilic risk factors. Hence, as we have described [29], these low-frequency genetic variations could play an important role in the development of VTE. The risk loci may act in concert with each mutation adding or detracting a small amount from the phenotype; the environment also interacts with the genotype to produce the final phenotype [8].
Recent genome-wide association studies have found additional genetic polymorphisms that are potentially related to VTE risk, but most have been detected predominately in European-ancestry populations [54, 55]. Genome-wide association studies do serve an important role in identifying new loci of interest, as well as confirming previously suggested loci for VTE. However, their main potential is for identifying common mutations (>5 %) with relatively lower risk (odds ratio <1.5). The candidate gene resequencing in the protein C anticoagulant system or the exome sequencing would facilitate the discovering of low-frequency variations with high risk for VTE in Asians. An accumulating body of evidence strongly suggests that genetic studies should be carried out in ethnically diverse populations, and that studies of common variations, as well as low-frequency variations, are warranted [29].
As VTE is a complex disease with genetic factors accounting for part of the risk, a multifactorial non-Mendelian inheritance model that includes the influence of genetic and environmental factors should be proposed for genetic counseling of VTE risk. Recently, a multiple single-nucleotide polymorphism test based on 31 VTE-associated polymorphisms or the 5 most strongly associated polymorphisms was found to improve risk prediction of first venous thrombosis in Caucasians [56]. Future studies should consider the construction of a multifactorial model based on the genetic risk factors in the protein C anticoagulant system, which is specific for Asian populations.
In summary, the genetic mutations leading to dysfunction of the protein C anticoagulant system could be a major risk factor for VTE in northeast Asian populations, especially in Japanese and Chinese. Conditions where the pro-coagulant activity surpasses the anticoagulant activity, including the protein C anticoagulant system, could trigger the development of thrombosis in individuals with risk genetic variants. Genetic analysis for VTE is highly restricted in Japanese and Chinese populations, and other Asian populations are not yet well studied. Even in geographically close populations, such as Japanese and Chinese, low-frequency mutations are not evenly distributed. The PROS1 p.Lys196Glu mutation, for example, is exclusively identified in Japanese populations. Whether dysfunction of the protein C anticoagulant system occurs in other Asian countries is an important unresolved issue of the thrombophilia study among Asians, and an international survey is warranted to disclose it.
References
White RH, Zhou H, Romano PS (1998) Incidence of idiopathic deep venous thrombosis and secondary thromboembolism among ethnic groups in California. Ann Intern Med 128(9):737–740
Klatsky AL, Armstrong MA, Poggi J (2000) Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am J Cardiol 85(11):1334–1337
White RH, Zhou H, Murin S, Harvey D (2005) Effect of ethnicity and gender on the incidence of venous thromboembolism in a diverse population in California in 1996. Thromb Haemost 93(2):298–305
White RH, Keenan CR (2009) Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res 123(Suppl 4):S11–S17
Sakuma M, Nakamura M, Yamada N, Ota S, Shirato K, Nakano T, Ito M, Kobayashi T (2009) Venous thromboembolism: deep vein thrombosis with pulmonary embolism, deep vein thrombosis alone, and pulmonary embolism alone. Circ J 73(2):305–309
Lee CH, Cheng CL, Lin LJ, Tsai LM, Yang YH (2011) Epidemiology and predictors of short-term mortality in symptomatic venous thromboembolism. Circ J 75(8):1998–2004
Zakai NA, McClure LA (2011) Racial differences in venous thromboembolism. J Thromb Haemost 9(10):1877–1882
Margaglione M, Grandone E (2011) Population genetics of venous thromboembolism. A narrative review. Thromb Haemost 105(2):221–231
Souto JC, Almasy L, Borrell M, Blanco-Vaca F, Mateo J, Soria JM, Coll I, Felices R, Stone W, Fontcuberta J, Blangero J (2000) Genetic susceptibility to thrombosis and its relationship to physiological risk factors: the GAIT study. Genetic analysis of idiopathic thrombophilia. Am J Hum Genet 67(6):1452–1459
Hamasaki N, Kuma H, Tsuda H (2013) Activated protein C anticoagulant system dysfunction and thrombophilia in Asia. Ann Lab Med 33(1):8–13
den Dunnen JT, Antonarakis SE (2000) Mutation nomenclature extensions and suggestions to describe complex mutations: a discussion. Hum Mut 15(1):7–12
De Stefano V, Finazzi G, Mannucci PM (1996) Inherited thrombophilia: pathogenesis, clinical syndromes, and management. Blood 87(9):3531–3544
Liu HW, Kwong YL, Bourke C, Lam CK, Lie AK, Wei D, Chan LC (1994) High incidence of thrombophilia detected in Chinese patients with venous thrombosis. Thromb Haemost 71(4):416–419
Shen MC, Lin JS, Tsay W (2000) Protein C and protein S deficiencies are the most important risk factors associated with thrombosis in Chinese venous thrombophilic patients in Taiwan. Thromb Res 99(5):447–452
Ho CH, Chau WK, Hsu HC, Gau JP, Yu TJ (2000) Causes of venous thrombosis in fifty Chinese patients. Am J Hematol 63(2):74–78
Suehisa E, Nomura T, Kawasaki T, Kanakura Y (2001) Frequency of natural coagulation inhibitor (antithrombin III, protein C and protein S) deficiencies in Japanese patients with spontaneous deep vein thrombosis. Blood Coagul Fibrinolysis 12(2):95–99
Chen TY, Su WC, Tsao CJ (2003) Incidence of thrombophilia detected in southern Taiwanese patients with venous thrombosis. Ann Hematol 82(2):114–117
Sakata T, Okamoto A, Mannami T, Tomoike H, Miyata T (2004) Prevalence of protein S deficiency in the Japanese general population: the Suita study. J Thromb Haemost 2(6):1012–1013
Sakata T, Okamoto A, Mannami T, Matsuo H, Miyata T (2004) Protein C and antithrombin deficiency are important risk factors for deep vein thrombosis in Japanese. J Thromb Haemost 2(3):528–530
Kinoshita S, Iida H, Inoue S, Watanabe K, Kurihara M, Wada Y, Tsuda H, Kang D, Hamasaki N (2005) Protein S and protein C gene mutations in Japanese deep vein thrombosis patients. Clin Biochem 38(10):908–915
Angchaisuksiri P, Atichartakarn V, Aryurachai K, Archararit N, Rachakom B, Atamasirikul K, Tiraganjana A (2007) Risk factors of venous thromboembolism in Thai patients. Int J Hematol 86(5):397–402
Zhu T, Ding Q, Bai X, Wang X, Kaguelidou F, Alberti C, Wei X, Hua B, Yang R, Wang X, Wang Z, Ruan C, Schlegel N, Zhao Y (2011) Normal ranges and genetic variants of antithrombin, protein C and protein S in the general Chinese population. Results of the chinese hemostasis investigation on natural anticoagulants study I group. Haematologica 96(7):1033–1040
Tang L, Lu X, Yu JM, Wang QY, Yang R, Guo T, Mei H, Hu Y (2012) PROC c.574_576del polymorphism: a common genetic risk factor for venous thrombosis in the Chinese population. J Thromb Haemost 10(10):2019–2026
Shen MC, Lin JS, Tsay W (1997) High prevalence of antithrombin III, protein C and protein S deficiency, but no factor V Leiden mutation in venous thrombophilic Chinese patients in Taiwan. Thromb Res 87(4):377–385
Gandrille S, Borgel D, Sala N, Espinosa-Parrilla Y, Simmonds R, Rezende S, Lind B, Mannhalter C, Pabinger I, Reitsma PH, Formstone C, Cooper DN, Saito H, Suzuki K, Bernardi F, Aiach M (2000) Protein S deficiency: a database of mutations—summary of the first update. Thromb Haemost 84(5):918
Yin T, Takeshita S, Sato Y, Sakata T, Shin Y, Honda S, Kawasaki T, Tsuji H, Kojima T, Madoiwa S, Sakata Y, Murata M, Ikeda Y, Miyata T (2007) A large deletion of the PROS1 gene in a deep vein thrombosis patient with protein S deficiency. Thromb Haemost 98(4):783–789
Kimura R, Sakata T, Kokubo Y, Okamoto A, Okayama A, Tomoike H, Miyata T (2006) Plasma protein S activity correlates with protein S genotype but is not sensitive to identify K196E mutant carriers. J Thromb Haemost 4(9):2010–2013
Ikejiri M, Wada H, Sakamoto Y, Ito N, Nishioka J, Nakatani K, Tsuji A, Yamada N, Nakamura M, Ito M, Nobori T (2010) The association of protein S Tokushima-K196E with a risk of deep vein thrombosis. Int J Hematol 92(2):302–305
Miyata T, Hamasaki N, Wada H, Kojima T (2012) More on: racial differences in venous thromboembolism. J Thromb Haemost 10(2):319–320
Yamazaki T, Sugiura I, Matsushita T, Kojima T, Kagami K, Takamatsu J, Saito H (1993) A phenotypically neutral dimorphism of protein S: the substitution of Lys155 by Glu in the second EGF domain predicted by an A to G base exchange in the gene. Thromb Res 70(5):395–403
Shigekiyo T, Uno Y, Kawauchi S, Saito S, Hondo H, Nishioka J, Hayashi T, Suzuki K (1993) Protein S Tokushima: an abnormal protein S found in a Japanese family with thrombosis. Thromb Haemost 70(2):244–246
Kimura R, Honda S, Kawasaki T, Tsuji H, Madoiwa S, Sakata Y, Kojima T, Murata M, Nishigami K, Chiku M, Hayashi T, Kokubo Y, Okayama A, Tomoike H, Ikeda Y, Miyata T (2006) Protein S-K196E mutation as a genetic risk factor for deep vein thrombosis in Japanese patients. Blood 107(4):1737–1738
Miyata T, Kimura R, Kokubo Y, Sakata T (2006) Genetic risk factors for deep vein thrombosis among Japanese: importance of protein S K196E mutation. Int J Hematol 83(3):217–223
Miyata T, Sato Y, Ishikawa J, Okada H, Takeshita S, Sakata T, Kokame K, Kimura R, Honda S, Kawasaki T, Suehisa E, Tsuji H, Madoiwa S, Sakata Y, Kojima T, Murata M, Ikeda Y (2009) Prevalence of genetic mutations in protein S, protein C and antithrombin genes in Japanese patients with deep vein thrombosis. Thromb Res 124(1):14–18
Neki R, Fujita T, Kokame K, Nakanishi I, Waguri M, Imayoshi Y, Suehara N, Ikeda T, Miyata T (2011) Genetic analysis of patients with deep vein thrombosis during pregnancy and postpartum. Int J Hematol 94(2):150–155
Hayashi T, Nishioka J, Suzuki K (1995) Molecular mechanism of the dysfunction of protein S(Tokushima) (Lys155→Glu) for the regulation of the blood coagulation system. Biochim Biophys Acta 1272(3):159–167
Liu W, Yin T, Okuda H, Harada KH, Li Y, Xu B, Yang J, Wang H, Fan X, Koizumi A, Miyata T (2013) Protein S K196E mutation, a genetic risk factor for venous thromboembolism, is limited to Japanese. Thromb Res 132(2):314–315
Tsay W, Shen MC (2004) R147W mutation of PROC gene is common in venous thrombotic patients in Taiwanese Chinese. Am J Hematol 76(1):8–13
Tang L, Guo T, Yang R, Mei H, Wang H, Lu X, Yu J, Wang Q, Hu Y (2012) Genetic background analysis of protein C deficiency demonstrates a recurrent mutation associated with venous thrombosis in Chinese population. PLoS ONE 7(4):e35773
Tsay W, Greengard JS, Montgomery RR, McPherson RA, Fucci JC, Koerper MA, Coughlin J, Griffin JH (1993) Genetic mutations in ten unrelated American patients with symptomatic type 1 protein C deficiency. Blood Coagul Fibrinolysis 4(5):791–796
Tait RC, Walker ID, Reitsma PH, Islam SI, McCall F, Poort SR, Conkie JA, Bertina RM (1995) Prevalence of protein C deficiency in the healthy population. Thromb Haemost 73(1):87–93
Miyata T, Sakata T, Yasumuro Y, Okamura T, Katsumi A, Saito H, Abe T, Shirahata A, Sakai M, Kato H (1998) Genetic analysis of protein C deficiency in nineteen Japanese families: five recurrent defects can explain half of the deficiencies. Thromb Res 92(4):181–187
Matsuda M, Sugo T, Sakata Y, Murayama H, Mimuro J, Tanabe S, Yoshitake S (1988) A thrombotic state due to an abnormal protein C. N Engl J Med 319(19):1265–1268
Miyata T, Zheng YZ, Sakata T, Tsushima N, Kato H (1994) Three missense mutations in the protein C heavy chain causing type I and type II protein C deficiency. Thromb Haemost 71(1):32–37
Sakata T, Kario K, Katayama Y, Matsuyama T, Kato H, Miyata T (2000) Studies on congenital protein C deficiency in Japanese: prevalence, genetic analysis, and relevance to the onset of arterial occlusive diseases. Semin Thromb Haemost 26(1):11–16
Heit JA, Petterson TM, Owen WG, Burke JP, DE Andrade M, Melton LJ 3rd (2005) Thrombomodulin gene polymorphisms or haplotypes as potential risk factors for venous thromboembolism: a population-based case–control study. J Thromb Haemost 3(4):710–717
Sugiyama S, Hirota H, Kimura R, Kokubo Y, Kawasaki T, Suehisa E, Okayama A, Tomoike H, Hayashi T, Nishigami K, Kawase I, Miyata T (2007) Haplotype of thrombomodulin gene associated with plasma thrombomodulin level and deep vein thrombosis in the Japanese population. Thromb Res 119(1):35–43
Tang L, Wang HF, Lu X, Jian XR, Jin B, Zheng H, Li YQ, Wang QY, Wu TC, Guo H, Liu H, Guo T, Yu JM, Yang R, Yang Y, Hu Y (2013) Common genetic risk factors for venous thrombosis in the Chinese population. Am J Hum Genet 92(2):177–187
Delvaeye M, Noris M, De Vriese A, Esmon CT, Esmon NL, Ferrell G, Del-Favero J, Plaisance S, Claes B, Lambrechts D, Zoja C, Remuzzi G, Conway EM (2009) Thrombomodulin mutations in atypical hemolytic-uremic syndrome. New Engl J Med 361(4):345–357
Dennis J, Johnson CY, Adediran AS, de Andrade M, Heit JA, Morange PE, Tregouet DA, Gagnon F (2012) The endothelial protein C receptor (PROCR) Ser219Gly variant and risk of common thrombotic disorders: a HuGE review and meta-analysis of evidence from observational studies. Blood 119(10):2392–2400
Ireland HA, Cooper JA, Drenos F, Acharya J, Mitchell JP, Bauer KA, Morrissey JH, Esnouf MP, Humphries SE (2009) FVII, FVIIa, and downstream markers of extrinsic pathway activation differ by EPCR Ser219Gly variant in healthy men. Arterioscler Thromb Vasc Biol 29(11):1968–1974
Chen XD, Tian L, Li M, Jin W, Zhang HK, Zheng CF (2011) Relationship between endothelial cell protein C receptor gene 6936A/G polymorphisms and deep venous thrombosis. Chin Med J (Engl) 124(1):72–75
Yin G, Jin X, Ming H, Zheng X, Zhang D (2012) Endothelial cell protein C receptor gene 6936A/G polymorphism is associated with venous thromboembolism. Exp Ther Med 3(6):989–992
Bezemer ID, Bare LA, Doggen CJ, Arellano AR, Tong C, Rowland CM, Catanese J, Young BA, Reitsma PH, Devlin JJ, Rosendaal FR (2008) Gene variants associated with deep vein thrombosis. JAMA 299(11):1306–1314
Tregouet DA, Heath S, Saut N, Biron-Andreani C, Schved JF, Pernod G, Galan P, Drouet L, Zelenika D, Juhan-Vague I, Alessi MC, Tiret L, Lathrop M, Emmerich J, Morange PE (2009) Common susceptibility alleles are unlikely to contribute as strongly as the FV and ABO loci to VTE risk: results from a GWAS approach. Blood 113(21):5298–5303
de Haan HG, Bezemer ID, Doggen CJ, Le Cessie S, Reitsma PH, Arellano AR, Tong CH, Devlin JJ, Bare LA, Rosendaal FR, Vossen CY (2012) Multiple SNP testing improves risk prediction of first venous thrombosis. Blood 120(3):656–663
Acknowledgments
This work was supported in part by grants-in-aid from the Ministry of Health, Labour, and Welfare of Japan; the Ministry of Education, Culture, Sports, Science, and Technology of Japan; the Japan Society for the Promotion of Science, and by grants from the Clinical Research Supportive Fund, General Hospital of Chinese People’s Liberation Army (No. 2012FC-TSYS-3042).
Conflict of interest
The authors have no relevant disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yin, T., Miyata, T. Dysfunction of protein C anticoagulant system, main genetic risk factor for venous thromboembolism in Northeast Asians. J Thromb Thrombolysis 37, 56–65 (2014). https://doi.org/10.1007/s11239-013-1005-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-013-1005-x