Abstract
Venous thromboembolism (VTE) is a serious risk after major orthopedic surgery (MOS) including total knee replacement, total hip replacement and hip fracture surgery. This risk can be reduced with several pharmacologic and mechanical prophylactic approaches, and the choice among them depends on their ability to reduce VTE with an acceptable increase in adverse events, especially major bleeding complications. Improvements in medical and surgical care have led to a progressive decrease in the risk of VTE after MOS with an estimated baseline risk with contemporary practice of approximately 4.3 % up to day 39 after surgery. Low-molecular-weight heparin is the most thoroughly studied thromboprophylactic agent following MOS and demonstrates good effectiveness with an acceptable rate of bleeding complications. Warfarin, rivaroxaban, dabigatran, and apixaban have all been studied in large trials in comparison with low-molecular-weight heparin and also show an acceptable benefit: risk ratio. Mechanical approaches including graduated compression stockings, intermittent pneumatic compression and venous foot pump also offer protection against VTE, but there is less evidence is available regarding their effectiveness and risks. Combination therapy consisting of an antithrombotic agent and mechanical device is probably more effective than either alone. The appropriate use of thromboprophylaxis after MOS results in reduced VTE with acceptable bleeding risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing major orthopedic surgery (MOS), including total hip replacement (THR), total knee replacement (TKR) and hip fracture surgery (HFS), are at particular risk of developing post-operative venous thromboembolism (VTE). The number of such procedures is increasing as the population ages, focusing attention on this problem. For example, there are currently over 200,000 THR procedures performed in the United States annually and a similar number of total knee replacements are performed [1]. The problem of post-operative VTE has come to the attention of regulatory agencies that have targeted VTE as a preventable complication and set targets for reduction. Reimbursement may be denied for hospital acquired VTE in the future [2] shifting the financial risk of the cost of caring for patients with these events to providers. The most effective management strategy is primary prophylaxis, and nearly all patients having MOS will receive some form. In recent years there has been an increase in the choices available for prophylaxis as new agents have been introduced and new studies and recommendations made available. The available approaches to prophylaxis and choosing among them will be the topic of this report which will be limited to consideration of major orthopedic surgery (MOS) only. Other orthopedic procedures are also associated with increased risk of thrombosis but will not be considered. The reader is referred to major comprehensive reviews that have recently been published [3, 4].
Balance of thrombosis and bleeding
The goal of thromboprophylaxis is to prevent thromboembolic events that adversely impact patient health including fatal and non-fatal pulmonary embolism (PE) and symptomatic deep vein thrombosis (DVT). The post-thrombotic syndrome may also contribute to morbidity after development of a post-operative DVT, but the data available on the frequency of this complication is sparse and will not be considered here. There is considerable data on acute VTE after MOS, much of which is the result of large randomized controlled trials sponsored by pharmaceutical companies as part of requirements to introduce new anticoagulants with regulatory approval. The primary endpoint in nearly all such studies has been the development of “all venous thromboembolism” which has included asymptomatic DVT identified by mandatory screening using imaging methods including venography or Doppler ultrasound at some time after surgery. In all cases, the great majority of thrombotic endpoints that have been identified in these clinical studies have been asymptomatic DVT, often confined to the calf. The reason for this choice of endpoints is that regulatory agencies in North America and Europe have viewed a reduction in such asymptomatic thrombi as sufficient to warrant approval. This allows studies to be done efficiently with many fewer subjects than would be needed if only symptomatic events were used as endpoints because there is a high ratio of asymptomatic to symptomatic VTE events in such studies.
Clearly, symptomatic VTE events are of considerable clinical importance as they may cause death, cardiorespiratory compromise and leg symptoms. Further, their treatment with anticoagulants may cause serious bleeding complications by itself. It is, however, less obvious that asymptomatic DVT detected by screening imaging methods are of clinical significance. Such asymptomatic thrombi may later progress and lead to acute symptoms, although most seem to resolve without sequelae. It is possible that some asymptomatic DVT may eventually lead to the development of the post-thrombotic syndrome, although this is not clearly established by the available data. Some view asymptomatic DVT identified by screening is a useful “marker” of the likely development of clinically symptomatic thrombosis, although they are not by themselves significant. The differences in rates of asymptomatic thrombosis identified by screening may be a valuable indicator of the potential thrombosis risk reduction in comparing prophylaxis strategies when used in conjunction with absolute risks of symptomatic thrombosis and bleeding as suggested in the recent ACCP guidelines [5]. This distinction is of more than academic interest, as the benefits of thromboprophylaxis are counterbalanced by its adverse effects. Because anticoagulants are commonly used for thromboprophylaxis, bleeding events are the most common adverse effect. These may be quite serious in the context of MOS and can result in the need for transfusion, reoperation and an increased risk of infection. The proper balance between reducing thrombosis and increasing bleeding risk is difficult to define. Fortunately, fatal PE is very uncommon in contemporary practice. Generally, the need is to consider the relative effects on the patient of reduction in symptomatic, nonfatal PE, symptomatic DVT and major bleeding events.
A critical question is whether the occurrence of VTE or of a major bleeding event has a greater adverse effect on the overall health of a patient, and more research is needed in this area. Recently, the ACCP in its new recommendations has reviewed this topic and judged that most patients would consider the adverse consequences of a symptomatic VTE and a major bleeding complication equally [6]. Asymptomatic DVT identified by screening cannot be included in this judgment, because one cannot balance the abstract value of preventing an asymptomatic DVT against a real, symptomatic bleeding event resulting from anticoagulant thromboprophylaxis.
This balance of thrombosis and bleeding is very important in evaluating the potential benefit of thromboprophylaxis. For example, if the baseline thrombosis rate including asymptomatic DVT is in the range of 20 % and an anticoagulant regimen reduces this by 60 %, then the absolute benefit is a reduction of 12 %. However, anticoagulants always increase bleeding. Consequently, if bleeding were to increase by 2 %, the balance of a 12 % reduction in thrombosis with a 2 % increase in bleeding would appear to strongly favor anticoagulant thromboprophylaxis. However, if we reconsider this scenario using the more relevant symptomatic thrombosis rate, the balance is close. If for example, the symptomatic thrombosis rate is 4 % with the same relative risk reduction of 60 %, then the absolute risk reduction would be 2.4 %. If the increase in bleeding is the same at 2 %, then the balance is close, and decisions about thromboprophylaxis should consider this close balance.
Baseline risks of thromboembolism and bleeding
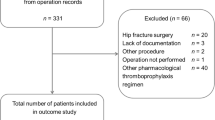
It follows from the above discussion, that critical information for evaluating the benefits of thromboprophylaxis is knowledge of the baseline risks of thrombosis and of bleeding in the absence of any intervention. However, the contemporary baseline risks are difficult to define because thromboprophylaxis has become a standard of care, and large untreated cohorts have not been recently reported. Clinical studies of thromboprophylaxis using untreated or placebo groups were performed prior to the 1990s, and most of our data derives from those studies. However, there have been many changes since that time which render this data difficult to extrapolate to contemporary practice. Such changes include refinements in surgical technique, earlier mobilization after surgery, earlier hospital discharge, improvements in rehabilitation after surgery and changes in demographics. Older studies prior to 1980 often reported a symptomatic rate of VTE between 15 and 30 % with no prophylaxis [7–11]. However, evidence indicates that post-operative VTE after MOS has been decreasing. The recent ACCP report used an approach that analyzed rates of thrombosis over time in groups of patients who received the same LMWH treatment [4]. This is reasonable because comparable LMWH regimens have been used since the 1990s. Evidence suggests that LMWH results in a relative risk reduction of between 50 and 60 %. Using this estimate and the rate of symptomatic VTE reported with LMWH allows an estimation of the contemporary rate of VTE in patients who would not be receiving prophylaxis. This rate is approximately 1.8 % for symptomatic DVT and 1 % for PE in the first 7–14 days after surgery. Estimates of the rate of thrombosis after hospital discharge (extended) suggest a rate of 0.9 % of VTE up to day 39 for a total rate of symptomatic VTE of 4.3 % (Fig. 1).
Schematic of estimated incidence rates for LMWH and no prophylaxis for major orthopedic surgery. Reproduced with permission from the American College of Chest Physicians [4]
Baseline bleeding rates are somewhat easier to estimate as data can be derived from recent clinical trials considering those patients randomized to receive only mechanical means of prophylaxis that should have little or no effect on hemostasis. Considering all such data, the ACCP review [4] has identified median rate of bleeding was 1.5 %, a rate which is consistent with a recent systematic review that estimated the baseline bleeding rate at between 1 and 2 % [3]. It is reasonable to conclude that bleeding rates in studies using anticoagulant prophylaxis that are above 1.5 % are due to the anticoagulant intervention.
One approach to optimizing thromboprophylaxis would be to perform an initial evaluation of both thrombosis and bleeding risks as the basis of choosing prophylaxis so that patients at the highest risk of thrombosis receive the most effective regimen that may be associated with an increased bleeding risk. In contrast, those at a high bleeding risk might not receive an anticoagulant. An example of this approach is a guideline from the AAOS that divides patients according to thrombosis and bleeding risk and provides different recommendations for prophylaxis depending on risk group [12]. This strategy could be an ideal approach to the problem, but there is little substantial data to support such risk stratification. Various patient-specific characteristics such as prior VTE, Charlson comorbidity index, body mass index, age and the presence of cardiovascular disease have been shown to be associated with increased risk in MOS (see Table 1) [13–16]. However, the relative risk associated with these factors is typically small or modest and must be considered in relation to the very large risk attendant on the surgical procedure alone. Indeed, there are no studies that have successfully demonstrated the value of risk stratification in choosing prophylaxis after MOS. Therefore, judging thrombosis risk in patients having MOS based on patient characteristics cannot be recommended generally. However, a particular patient with a combination of such risk factors such as prior VTE, advanced age and high BMI could be considered to be at particularly high risk.
There may be greater value in judging bleeding risk, although the data is also limited in this area. Typically, patients with a clinically important bleeding risk such as significant thrombocytopenia do not choose to have elective MOS. They may, however, need HFS. In such cases, the risk of bleeding would be increased and would influence the choice of prophylaxis so that a regimen such as mechanical prophylaxis would be advisable. Procedure-specific issues may also indicate an increased bleeding risk. For example, if there is excessive bleeding during the operative procedure with hemostasis that is difficult to achieve or if bleeding continues post-operatively, then anticoagulant thromboprophylaxis is likely to add risk and mechanical devices may be a better choice (see Table 1).
Thromboprophylaxis compared with no treatment or placebo
Studies comparing various thromboprophylaxis regimens with no treatment or with placebo are typically decades old and have been thoroughly reviewed [3, 4]. All of the following provide reduction in risk of thrombosis compared to no treatment based on studies with a direct comparison: warfarin, unfractionated heparin, LMWH, fondaparinux, aspirin, graduated compression stockings, and intermittent pneumatic compression or venous foot pump (Table 2). Approved drug doses are shown in Table 3. The strength of the data is variable because of the quality of these studies and the number of patients included. The 95 % confidence intervals for the relative risks are often large and extend beyond 1. In the case of aspirin there is only one large study to evaluate [17]. Similarly, one small study constitutes the data available comparing fondaparinux with no prophylaxis and that was only for extended treatment after hospital discharge [18]. In evaluating mechanical devices, it is notable that there is considerable variation in the design of these devices and that compliance with their use is a large problem. This must be considered in evaluating the data. The comparison of these various agents versus no treatment or placebo is of considerable academic interest but of little practical value as standard practice in contemporary treatment is to offer some manner of thromboprophylaxis. It is of greater interest to make a comparison among these various approaches so that the best method can be selected for prophylaxis. This, again, has been extensively reviewed in the ACCP [4] and NICE recommendations [3].
The use of aspirin for prophylaxis in MOS has been quite controversial. It was studied as in several small studies using varying doses in the 1970s and 1980s. The results are difficult to interpret. Because of the attractiveness of aspirin as a potentially useful agent, it was studied in a single large multicenter, randomized, placebo controlled trial in the 1990s entitled the pulmonary embolism prevention trial (PEP) [17]. In that trial, a dose of 160 mg of aspirin or placebo was given for 35 days, and the endpoint was the rate of development of symptomatic thrombotic events. The study included 17,444 patients who primarily had hip fracture surgery, but there was also a group that had THR (Table 4). It showed a 28 % reduction in the risk of symptomatic DVT in the aspirin group, and there was also a suggestion of a decrease in mortality with 17 VTE associated deaths in the aspirin group compared with 45 in the placebo group. There was a trend toward more nonfatal myocardial infarctions in the aspirin-treated group. The study has been criticized because of difficulty with presentation of the results and changes in sample size after initiation [19]. Also, the study included primarily HFS patients with fewer that had THR or TKR. Considering the THR or TKR patients alone, the results were non-significant. However, the study had significant strengths including excellent randomization, blinding of patients and caregivers, and blinded adjudication. Additionally, follow up was excellent. Overall, the results may be interpreted to show that aspirin reduces VTE after MOS including HFS and THR. However, the relative risk reduction that is reported (28 % in DVT) is considerably less than that with anticoagulant agents or with mechanical devices, and aspirin cannot be recommended alone as a single agent for thromboprophylaxis in patients having MOS. Consideration may be given to combining aspirin with a mechanical approach, but there is insufficient data to recommend this at this time.
Comparison of approaches to thromboprophylaxis
An analysis of the results of a large number of clinical studies forms the basis of choosing among the several prophylactic approaches, and this topic has been reviewed [3, 4]. Despite the large number of studies addressing thromboprophylaxis in MOS, there remains difficulty in interpreting the results as a guide to choice of therapy. There are several reasons for this problem. For example, the studies have been conducted over 40 years, and techniques of surgery and patterns of care have changed and patient demographics have also altered. Often the primary endpoint for studies was all VTE including asymptomatic cases identified by screening imaging tests. In most studies asymptomatic DVT dominated the endpoint numbers, and the number of symptomatic events was typically small. Considering that symptomatic events are the most important endpoint clinically, this reduces the precision of estimates of efficacy. Bleeding has been typically the primary endpoint for safety, but bleeding definitions in various studies have been different, and categories have been defined to include fatal, major bleeding, minor bleeding, clinically relevant non-major bleeding and trivial bleeding and bleeding requiring reoperation. The lack of a comparable definition of bleeding endpoints across studies makes comparison difficult, particularly in judging the balance of thrombosis and bleeding events.
The largest amount of data from clinical trials is available for LMWH which was introduced in the 1990s and has recently represented the comparator against which large clinical trials using newer anticoagulants were conducted. Several different LMWH preparations have been evaluated and used in different dosing schedules. Discussion of these variations is beyond the scope of this report, and the data is generally comparable across this class of agents. LMWH was compared with low-dose unfractionated heparin in many studies of both general surgery and orthopedic surgery. Together they include over 23,000 patients with approximately 2,300 having MOS and suggest that LMWH is superior to unfractionated heparin with fewer PE (RR 0.78; CI 0.49–1.24) and DVT (0.80; CI 0.73–0.88) and also less major bleeding (RR 0.91; CI 0.75–1.09) [4]. This benefit is small, but more apparent when asymptomatic events are considered in the efficacy analysis. Several trials compared LMWH to vitamin K antagonists in THR and TKR showing significantly less asymptomatic DVT with LMWH, but there were also fewer symptomatic VTE events. Early after surgery, LMWH appears to be associated with an increase in bleeding complications compared with vitamin K antagonists [4], possibly because vitamin K antagonists have a delayed anticoagulant effect after initial administration. However, with longer use, they appear to have more serious bleeding events.
More recent studies have compared LMWH with fondaparinux, rivaroxaban, apixaban, and dabigatran. These studies all used imaging tests to screen patients for asymptomatic DVT, and total VTE, including asymptomatic events was the primary efficacy endpoint in these studies. Symptomatic events were reported, but there were generally few, and this reduces the precision for clinical endpoints in these study programs. LMWH was compared to fondaparinux for prevention of VTE following THR, TKR, and HFS in several randomized controlled trials [18, 20–22]. The combined data shows that fondaparinux was superior to LWMH in reducing asymptomatic DVT, but differences in symptomatic VTE were non-significant. Bleeding events were more common with fondaparinux.
Three new oral anticoagulants have been tested as thromboprophylactic agents in MOS including rivaroxaban, apixaban, and dabigatran. All were evaluated in randomized, controlled trials in THR and TKR (but not HFS) using enoxaparin as the comparator in all studies. Rivaroxaban, a factor Xa inhibitor, was evaluated for thromboprophylaxis in a program of MOS that included over 10,000 patients which compared a regimen of 10 mg daily starting 6–8 h after surgery and continued once daily compared with standard regimens of enoxaparin [23–26]. Combining the results of these studies, the use of rivaroxaban led to an approximate 59 % reduction in symptomatic DVT (RR 0.41; 95 % CI 0.20–0.83) with a nonsignificant effect on PE. Asymptomatic DVT was significantly less in patients with rivaroxaban. There was a nonsignificant trend toward more bleeding with rivaroxaban, but the overall rates were low in part because the trial design excluded surgical site bleeding from this endpoint category.
Apixaban is another Xa inhibitor that has been evaluated in large randomized, controlled trials for thromboprophylaxis in MOS including THR and TKR but not HFS. This program included over 11,000 subjects who received either enoxaparin in standard regimens or apixaban 2.5 mg twice daily starting 12–24 h after surgery [27–30]. The use of apixaban was associated with a reduction in symptomatic DVT (RR 0.41; 95 % CI 0.18–0.95) with no statistically significant effect on the occurrence of PE. There was a significant reduction in asymptomatic DVT in patients receiving apixaban. Major bleeding and bleeding requiring reoperation were uncommon and similar in both the enoxaparin and apixaban groups in these studies.
Dabigatran, another new oral anticoagulant, differs in being a thrombin inhibitor and also a prodrug that is activated after oral administration. The registration trials in MOS included over 10,000 subjects having either THR or TKR, and the comparator in all studies was enoxaparin given in standard regimens [31–34]. Dabigatran was administered in doses of either 150 or 220 mg daily with the first dose given approximately 4 h postoperatively with a reduction in the dose of 50 % for this initial dose. The overall results show that dabigatran was similar to enoxaparin in the occurrence of symptomatic DVT, PE and bleeding events with non-significant differences in rates in all categories of endpoints.
These new oral anticoagulants offer expanded choices for thromboprophylaxis in THR and TKR, but it is important to note that none has been evaluated in large studies with HFS. Important advantages include oral administration, with both dabigatran and rivaroxaban administered once daily and apixaban twice daily. This facilitates the continuation of thromboprophylaxis after hospital discharge which is necessary in nearly all patients. The choice among these agents will be guided by regulatory approvals, analysis of the trial results, local practice patterns and expense. At this time all 3 agents are approved in the European Union for prophylaxis after THR and TKR, whereas both dabigatran and rivaroxaban are approved for these indications in Canada, but only rivaroxaban is approved in the United States.
Mechanical approaches
Several mechanical approaches to thromboprophylaxis have been evaluated in MOS, and they act primarily by increasing venous blood flow. Broadly, these approaches can be divided into graduated compression stockings, pneumatic compression devices and the venous foot pump. They have the considerable advantage of not increasing bleeding after surgery, and this makes their use attractive. A major disadvantage is compliance, as all devices must be properly applied and need to be removed for events such as a washing and ambulation. Patients may also remove these devices because of discomfort, and their use after hospital discharge is problematic. Compliance is a particular problem with devices that require an external power source, but new portable and battery powered power devices that can be used after hospital discharge have been introduced, and these represent a promising technical improvement.
Several clinical studies have been reported using these mechanical devices for prophylaxis after MOS, but they have serious limitations. First, there are several different devices with varying properties that have been tested, and it is unclear whether they are all comparable. Overall, the studies are smaller than contemporary trials with anticoagulants. Further, blinding is not practical with these studies introducing the possibility of bias in ascertainment of endpoints. Few studies have been reported evaluating graduated compression stockings. However, a recent meta-analysis considering the available studies in both orthopedic and non-orthopedic surgery showed that GCS had a non-significant effect on PE (RR 0.63; CI 0.32–1.25) but reduced overall VTE including asymptomatic DVT (RR 0.51; CI 0.36–0.73)[4]. Although the data supporting their use is fairly small, they are frequently used in combination with an antithrombotic agent.
Pneumatic compression devices have been compared with anticoagulant thromboprophylaxis in MOS patients in studies using either warfarin or LMWH as the comparator [35–39] and these have been analyzed [4]. Overall, the rates of symptomatic DVT and PE appear to be somewhat greater in patients receiving prophylaxis with compression devices, but the small size of the trials limits confidence in the results. Fewer bleeding events are reported as might be expected, but these studies were non-blinded raising the possibility of bias in judging bleeding events.
Graduated compression stockings or pneumatic devices may also be used in combination with an antithrombotic agent. For example, recent trials evaluated a combination of the portable pneumatic compression device in combination with aspirin compared to LMWH in patients having THR and TKR [40, 41]. The occurrence of VTE was comparable in the treatment groups with fewer bleeding complications in those receiving aspirin and compression. Overall, however, the numbers are small, limiting confidence in these conclusions. A Cochrane review and ACCP analysis [42] have been performed of the reported studies using combination therapy, and these found that the combination appears to reduce asymptomatic DVT significantly, but the overall data is quite limited with imprecision in the results, an important problem with study design that limit confidence in the conclusions.
Summary
The skillful use of thromboprophylaxis after MOS will result in a decrease in VTE with acceptable adverse effects. The goal is to optimize therapy to minimize the occurrence of both VTE and bleeding events. New agents have been introduced that must be considered in choosing a prophylactic approach, and they offer the advantage of oral administration without monitoring which is particularly suitable for post discharge administration. Mechanical approaches to thromboprophylaxis and especially a combination therapy using both mechanical devices and an antithrombotic agent offer new opportunities to optimize thromboprophylaxis, and more studies are needed in this area.
References
American Academy of Orthopaedic Surgeons. Total hip replacement. American Academy of Orthopaedic Surgeons Website. http://orthoinfo.aaos.org/topic.dfm?topic=a00377. Accessed 12 Dec 2012
Department of Health & Human Services. Centers for Medicare & Medicaid Services. Medicare Fact Sheet. Proposals for improving quality of care during inpatients stays in acute care hospitals in the fiscal year 2011 notice of proposed rulemaking. April 19, 2010. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/downloads/FSQ09_IPLTCH11_NPRM041910.pdf. Accessed 12 Dec 2012
Hill J, Treasure T, National Clinical Guideline Centre for Acute and Chronic Conditions (2010) Reducing the risk of venous thromboembolism in patients admitted to hospital: summary of NICE guidance. BMJ 340:c95
Falck-Ytter Y, Francis C, Johanson NA, Curley C, Dahl OE, Schulman S, Ortel TL, Pauker SG, Colwell CW (2012) Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 suppl):e326S–e350S. doi:10.1378/chest.11-2298
Guyatt GH, Eikelboom JW, Gould MK et al (2012) Approach to outcome measurement in the prevention of thrombosis in surgical and medical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141(2 Suppl):e185S–e194s
Maclean S, Mulla S, Akl EA, Jankowski M, Vandvik PE, Ebrahim S, McLeod S, Bhatnagar N, Guatt GH, American College of Chest Physicians (2012) Patient values and preferences in decision making for antithrombotic therapy: a systematic review: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e1S–e23S. doi:10.1378/chest.11-2290
Sevit S, Gallagher NG (1959) Prevention of venous thrombosis and pulmonary embolism in injured patients. A trial of anticoagulant prophylaxis with phenindione in middle-aged and elderly patients with fractured necks of femur. Lancet 2(7110):981–989
Galasko CS, Edwards DH, Fearn CB, Barber HM (1976) The value of low dosage heparin for the prophylaxis of thromboembolism in patients with transcervical and intertrochanteric femoral fractures. Acta Orthop Scand 47(3):276–282
Sautter RD, Koch EL, Myers WO et al (1983) Aspirin-sulfinpyrazone in prophylaxis of deep venous thrombosis in total hip replacement. JAMA 250(19):2649–2654
Borgstroem S, Greitz T, Van Der Linden W, Molin J, Rudics I (1965) Anticoagulant prophylaxis of venous thrombosis in clinical patients with fractured neck of the femur; a controlled clinical trial using venous phlebography. Acta Chir Scand 129:500–508
Eskeland G, Solheim K, Skjörten F (1966) Anticoagulant prophylaxis, thromboembolism and mortality in elderly patients with hip fractures. A controlled clinical trial. Acta Chir Scand 131(1):16–29
American Academy of Orthopedic Surgeons (US) (2007) American Academy of Orthopedic Surgeons Clinical Guidelines on prevention of symptomatic pulmonary embolism in patients undergoing total hip or knee arthroplasty, p 63. http://www.aaos.org/Research/guidelines/PE_guideline.pdf. Accessed 12 Dec 2012
White RH, Zhou H, Romano PS (2003) Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost 90(3):446–455
White RH, Gettner S, Newman JM, Trauner KB, Romano PS (2000) Predictors of rehospitalization for symptomatic venous thromboembolism after total hip arthroplasty. N Engl J Med 343(24):1758–1764
Pedersen AB, Sorensen HT, Mehnert F, Overgaard S, Johnsen SP (2010) Risk factors for venous thromboembolism in patients undergoing total hip replacement and receiving routine thromboprophylaxis. J Bone Joint Surg Am 92(12):2156–2164
Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL (2003) Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology 99(3):552–560 discussion 5A
Pulmonary Embolism Prevention (PEP) Trial Collaborative Group (2000) Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: pulmonary embolism prevention (PEP) trial. Lancet 355(9212):1295–1302
Lassen MR, Bauer KA, Eriksson BI, Turpie AG, European Pentasaccharide Elective Surgery Study (EPHESUS) Steering Committee (2002) Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery; a randomised double-blind comparison. Lancet 359(9319):1715–1720
Cohen A, Quinlan D (2000) Correspondence PEP trial. Lancet 356(9225):250–251
Turpie AG, Bauer KA, Eriksson BI, Lassen MR, PENTATHALON 2000 Study Steering Committee (2002) Post-operative fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet 359(9319):1721–1726
Bauer KA, Eriksson BI, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Major Knee Surgery Study (2001) Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med 345(18):1305–1310
Eriksson HI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study (2001) Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med 345(18):1298–1304
Kakkar AK, Brenner B, Dahl OE et al (2008) Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet 372(9632):31–39
Eriksson BI, Borris LC, Friedman RJ et al (2008) Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med 358(26):2765–2775
Lassen MR, Ageno W, Borris LC et al (2008) Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med 358(26):2776–2786
Turpie AG, Lassen MR, Davidson BL et al (2009) Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet 373(9676):1673–1680
Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM, ADVANCE-3 Investigators (2010) Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med 363(26):2487–2498
Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P, ADVANCE-2 Investigators (2010) Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): a randomised double-blind trial. Lancet 375(9717):807–815
Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Portman RJ (2009) Apixaban or enoxaparin for thromboprophylaxis after knee replacement [published correction appears in N Engl J Med. 2009;36(18):1814]. N Engl J Med 361(6):594–604
Lassen MR, Davidson BL, Gallus A, Pineo G, Ansell J, Deitchman D (2007) The efficacy and safety of apixaban, an oral, direct factor Xa inhibitor, as thromboprophylaxis in patients following total knee replacement. J Thromb Haemost 5(12):2368–2375
Eriksson BI, Dahl OE, Huo MH et al (2011) Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE-NOVATE II*). A randomised, double-blind, non-inferiority trial. Thromb Haemost 105(4):721–729
Eriksson BI, Dahl OE, Rosencher N et al (2007) Dabigatran etexilate versus enoxaparin for total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 370(9591):949–956
Ginsberg JS, Davidson BL, Comp PC et al (2009) Oral thrombin inhibitor dabigatran etexilate vs. North American enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery. J Arthroplasty 24(1):1–9
Eriksson BI, Dahl OE, Rosencher N et al (2007) Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE-MODEL randomized trial. J Thromb Haemost 5(11):2178–2185
Chin PL, Amin MS, Yang KY, Yeo SJ, Lo NN (2009) Thromboembolic prophylaxis for total knee arthroplasty in Asian patients: a randomised controlled trial. J Orthop Surg (Hong Kong) 17(1):1–5
Pitto RP, Hamer H, Heiss-Dunlop W, Kuehle J (2004) Mechanical prophylaxis of deep-vein thrombosis after total hip-replacement, a randomised clinical trial. J Bone Joint Surg Br 86(5):639–642
Stone MH, Limb D, Campbell P, Stead D, Culleton G (1996) A comparison of intermittent calf compression and enoxaparin for thromboprophylaxis in total hip replacement. A pilot study. Int Orthop 20(6):367–369
Warwick D, Harrison J, Glew D, Michelmore A, Peters TH, Donovan J (1998) Comparison of the use of a foot pump with the use of low-molecular-weight heparin for the prevention of deep-vein thrombosis after total hip replacement. A prospective randomized trial. J Bone Joint Surg Am 80(8):1158–1166
Blanchard J, Meuwly JY, Leyvraz PF et al (1999) Prevention of deep-vein thrombosis after total knee replacement. Randomised comparison between a low-molecular-weight heparin (nadroparin) and mechanical prophylaxis with a foot-pump system. J Bone Joint Surg Br 81(4):654–659
Colwell CW Jr, Froimson MI, Mont MA et al (2010) Thrombosis prevention after total hip arthroplasty: a prospective, randomized trial comparing a mobile compression device with low-molecular-weight heparin. J Bone Joint Surg Am 92(3):527–535
Gelfer Y, Tavor H, Oron A, Peer A, Halperin N, Robinson D (2006) Deep vein thrombosis prevention in joint arthroplasties: continuous enhanced circulation therapy vs. low-molecular-weight heparin. J Arthroplasty 21(2):206–214
Kakkos SK, Caprini JA, Geroulakos G, Nicolaides AN, Stansby GP, Reddy DJ (2008) Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism in high-risk patients. Cochrane Database Syst Rev (4):CD005258
Conflict of interest
Dr. Francis received compensation from Eisai for participation on a Steering Committee.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Francis, C.W. Prevention of VTE in patients having major orthopedic surgery. J Thromb Thrombolysis 35, 359–367 (2013). https://doi.org/10.1007/s11239-013-0889-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-013-0889-9