Abstract
Despite the fact that lytic therapy of thromboembolic disorder has been achieved, reocclusion of the damaged vessels and bleeding complication frequently reduce the therapeutic effect. In order to prevent the vessel reocclusion and enhance the therapeutic effect, combining the anticoagulant with the thrombolytic was assumed. Herein, we propose that restraining but locally releasing anticoagulant activity in the vicinity of thrombus is a way to alleviate the bleeding risk. A bifunctional fusion protein, termed as SFH (Staphylokinase (SAK) linked by FXa recognition peptide at N-terminus of Hirudin (HV)), was designed. SFH retained thrombolytic activity but no anticoagulant activity in thrombus-free blood due to the extension of the N-terminus of HV. However, it could locally liberate intact HV and exhibit anticoagulant activity when FXa or fresh thrombus was present. At equimolar dose, both improved antithrombotic and thrombolytic effects of SFH were observed in kappa-carrageenin inducing mouse-tail thrombosis model and rat inferior vena cava thrombosis model, respectively. Moreover, we observed significantly lower bleeding risk in mice and rats treated with SFH than with the mixture of SAK and HV with monitoring TT (P < 0.01), aPTT (P < 0.05) and PT (P < 0.05), and bleeding time (P < 0.05). In conclusion, SFH is a promising bifunctional therapeutic candidate with lower bleeding risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases such as acute myocardial infarction and cerebrovascular diseases such as stroke are prominent causes of morbidity and mortality all over the world [1]. Fibrinolytics and plasminogen activators such as tissue-type plasminogen activator (t-PA), streptokinase (SK) and SAK, are used as potent clinic therapeutics. SAK, especially, is a highly fibrin-selective thrombolytic agent from Staphylococcus aureus. SAK forms a 1:1 stoichiometric complex with the inactive zymogen human plasminogen (hPg) and the complex converts plasminogen to the active serine protease form, plasmin (hPm) [2]. SAK-plasmin complex is rapidly neutralized by α-antiplasmin, whose inhibition rate is reduced by over 100-fold if the lysine-binding sites of plasmin are occupied by fibrin, resulting in an apparent fibrin-selectivity [3]. However, when treated with t-PA or SAK, only approximately 60% of the patients obtain a complete arterial recanalization within 90 min [4–6]. In addition, 10–30% of the patients among this group show reocclusion shortly after clot dissolution, some of whom suffer bleeding complications such as hemorrhagic stroke [7–9]. The reformed secondary clots are usually platelet-rich and show strong resistance to lysis mediated by fibrinolytic agents [10, 11]. One important factor contributing to the formation of reocclusion is the activated thrombin released from the injured site of the vessel and clots that are undergoing lysis [12].
To avoid reocclusion, thrombin inhibitors such as heparin and hirudin have been applied [13–15]. Recombinant hirudin, which has specific and high-affinity binding to thrombin [16], is used to prevent the occurrence of reocclusion and produces a significant reduction in the composite endpoint of death or myocardial infarction compared with heparin [14, 17, 18]. However, the effective anticoagulant activity of hirudin is associated with a frequent occurrence of systemic bleeding [18] and there is no antagonist against hirudin hitherto.
To combine fibrinolytic activity with anticoagulant activity, several chimeric proteins have been created [19–22]. However, when the N-terminus of SAK was linked to the C-terminus of HV, SAK underwent rapid degradation at site Lys10–Lys11 in less than 2 minutes in vivo resulting in no intact fusion protein targeting to thrombus; whereas, the HV domain in the fusion proteins showed no [21] or less [19] anticoagulant activity when the N-terminus of HV was linked to the C-terminus of its partners. Several other studies have also demonstrated that any extension at the N-terminus of HV significantly attenuated or abolished its anticoagulant activities [23, 24].
Activated FX (FXa) is a coagulant factor to convert prothrombin into activated thrombin in the common pathway of coagulation, which specially recognizes primary sequence IEGR and cleaves its C-terminal. It has been widely used to remove tags of recombinant fusion protein with linker peptide IEGR in biochemistry. Recently, linker peptide IEGR also was introduced to construct FXa-dependent fusion proteins to improve anticoagulation [25, 26] or thrombolysis [27, 28]. Generally, the fibrinolytic or anticoagulant was linked with antibodies or fragment to improve the affinity to clot.
In this report, we hypothesized that reducing anticoagulant concentration or activity in peripheral blood and restricting its activity on the local site of thrombus would be one of the effective strategies to alleviate bleeding risk. To combine fibrinolytic and anticoagulant activities and to better circumvent the dilemma of anticoagulant activity and hemorrhage events, a new fusion protein, SFH, combining SAK with HV2, was designed. An FXa recognition peptide was introduced between SAK and HV2 to regulate the release of the functionally essential N-terminus of HV2 in the vicinity of thrombus, where FXa is present and anticoagulant activity is needed. We combined three features of the pathway of blood coagulation and therapy itself: first, FX is significantly activated in the vicinity of thrombus [29]; second, extension of the N-terminus of HV significantly attenuating its anticoagulant activity [23, 24]; third, excessive anticoagulant activity in peripheral blood is undesired except in the vicinity of the thrombus. Thus, we predicted that the chimeric protein would have three features: (1) bifunction with anticoagulant and fibrinolytic activities, (2) minimal anticoagulant activity at the thrombus-free sites to reduce bleeding risk, and (3) maximal anticoagulant activity at the sites of thrombus to enhance thrombolysis.
To summarize the results, we found that SFH retained fibrinolytic activities that could break down clots, but did not exhibit anticoagulant activity until arriving at the thrombus. Upon reaching the thrombus, the anticoagulant activity locally presented due to the released hirudin by FXa existing only in the thrombus. In animal tests, SFH showed an improved antithrombotic activity with less bleeding risk.
Materials and methods
Host strain and plasmid
E. coli DH5α was used for cloning genes, propagation of plasmid and protein expression. Gene sak was cloned from lysogenic strains of Staphylococcus aureus using PCR and gene hir was synthesized according to the sequence of HV2. Plasmid pBV220 [30] was used as expression vector.
Construction of expression plasmid
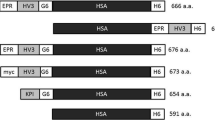
The composition of SFH is shown in Fig. 1. The linker sequence between SAK and HV2 was FXa recognition peptide GSIEGR. The primers used for gene cloning are listed in Table 1. The amplification conditions for sak sequence are as follows: 30 cycles consist of 95°C for 1 min, 55°C for 1 min and 72°C for 1 min with primers 1 and 2. The amplified sak sequence without stop codon was purified, digested with EcoR I and BamH I, and cloned into pBV220 to create plasmid pBV-SAK. Gene sequence of linker peptide was created by PCR amplification at the synthesized primer of hirudin gene sequence (Table 1). The amplification conditions for hir with gene sequence of linker peptide are as follows: 30 cycles consist of 95°C for 30 s, 55°C for 30 s and 72°C for 1 min with primers 3 and 4. The amplified hir with gene sequence of linker peptide was purified, digested with BamH I and Pst I, and cloned into pBV-SAK at downstream of sak to create plasmid pBV-SFH. All clones were verified by DNA sequencing.
Protein expression, isolation and purification
For expression of SFH, the constructed strain was inoculated into LB medium with 50 mg/l Amp and incubated at 30°C for overnight. The overnight culture was amplified at 30°C for 5 h and induced at 42°C for another 5 h. Bacterial cell was collected by centrifugation at 8,000g for 20 min at 4°C.
Protein extraction from cell pellets was performed according to Johnson [31] with 20 mM His–HCl buffer (pH 6.0). In brief, 30 g of cell pellets were frozen at −70°C for 30 min and then thawed by ice/water bath for 30 min. This cycle was repeated 3 times. The pellets were resuspended in 200 ml of 20 mM His–HCl buffer (pH 6.0) and periodically agitated to facilitate completely mixing followed by centrifugation at 10,000g for 30 min at 4°C. The supernatant was applied to Source 15Q column previously equilibrated with 20 mM His–HCl buffer at pH 6.0 and the column were eluted by a 0–1 M NaCl gradient. The active fraction was collected and then applied to Superdex 75 column. The active fraction was applied to Superdex 75 followed by Superdex G-25 to desalt. Protein concentration was determined using the Lowry method [32]. Molecular mass of SFH was determined by reduced SDS-PAGE as well as MALDI-TOF mass spectrometry. Isoelectric point (pI) was determined by capillary electrophoresis. N-terminus sequence was determined by Edman degradation.
Fibrinolytic activity assay
Fibrinolytic activity [33, 34] of SAK and SFH was determined by the proteolytic activity monitored on 5% agar plate containing 1 NIHU/ml of human thrombin (Sigma), 10 μg/ml of human plasminogen (Roche) and 0.8 mg/ml of fibrinogen (Chinese Medical Academy) at pH 7.5. A series of wells of 4 mm diameter were burrowed and 20 μl samples with serial dilutions were added to the wells. The plates were incubated for 4 h at 37°C and the fibrinolytic activities were expressed by the diameter of clear zone around the wells.
Anticoagulant activity assay
Anticoagulant activity in vitro was expressed as antithrombin units (ATU) [35]. Briefly, 10 μl of serially diluted samples were added to 20 μl of thrombin solution (8 NIHU/ml, Sigma) followed by the addition of 50 μl of fibrinogen (5 mg/ml) and clot formation was monitored. The dilution factor that inhibited clot formation was defined as the antithrombin activity of the samples. Data from triple independent experiments were combined and analyzed.
FXa releasing free HV2
To cleave SFH and release free HV2, the previously dialyzed FXa (Roche) against TA buffer (50 mM Tris–HCl, 100 mM NaCl, and 1 mM CaCl2, pH 8.0) was used in the following conditions: 0.2U of FXa was mixed with 0.2 mg of SFH in 300 μl TA buffer at 37°C [36]. Twenty microliters of cleaved products at different reaction time were monitored with SDS-PAGE and the anticoagulant activity of 10 μl of reaction products was detected by clot formation.
Antithrombotic activity of SFH in the carrageenin-induced mouse tail thrombosis (MTT) model
To determine antithrombotic activity in vivo, the carrageenin-induced MTT model was employed according to Bekemeier et al. [37, 38] and Hu et al. [39]. To induce thrombosis, 0.2 ml (4 mg/ml) carrageenin (Type I, Sigma) was injected to male inbred Kunming mice (weight between 20–23 g and a group consisting of 10 mice) subcutaneously (s.c.) at a dose of 40 mg/kg body weight. After 1 h of carrageenin injection, SFH, SAK, HV2 and the mixture of SAK with HV2 at equimolar concentration, respectively, were administrated intropeitoneally (i.p.) every 8 h. The frequency and length of tail infarction were recorded at 24, 36, and 48 h after carrageenin injection, respectively. Differences in mouse tail thrombosis frequencies and lengths of between groups were calculated according to χ2-test and t-test, respectively.
Thrombolytic activity of SFH in inferior vena cava (IVC) thrombosis model in the rat
Male Sprague-Dawley rats weighing 240–280 g were randomly divided into 5 treatment groups for saline, SAK, HV2, SFH and SAK plus HV2. The rats were anaesthetized and opened abdomen by a midline incision. IVC thrombosis was performed with IVC ligation below the level of the renal veins [40–42]. Three hours after the ligation, saline with or without drugs (31.5 pmol/kg) was administered through a catheter inserted into the jugular vein.
For determinations of thrombin time (TT), activated partial thromboplastin time (aPTT) and prothrombin time (PT), blood samples were taken through the catheter inserting into the jugular vein at the following time points: prior to ligation, after ligation, and at 30 and 60 min after drug administration, respectively.
After 1 h of drug administration, the animals were re-anaesthetized, the inferior caval veins were longitudinally opened and clots were harvested and weighed.
TT, aPTT and PT in IVC thrombosis model in rats
To measure TT, aPTT and PT, the blood samples were collected into plastic tubes containing 0.11 M trisodium citrate (9:1 of blood to citrate solution) and immediately centrifuged at 10,000g for 5 min. TT, aPTT and PT were measured with a coagulometer and commercially available test kits (Tianjin Institute of Hematology, China). All measurements for every sample were carried out in duplicate according to the guidelines of the manufacturer. Data from 10 animals in each group were expressed as group mean values with the standard error of the mean (SEM). Statistical significance was determined using a one-way analysis of variance (ANOVA). In cases when P < 0.05, pairwise comparisons were made at the same level, applying Bonferroni corrections. Significance was defined at a level of P < 0.05 or P < 0.01.
Bleeding time
Bleeding time was assessed by a tail transection method [43, 44]. Briefly, mice were positioned in a cage that kept the tail steady. After 20 min of drug administration, the mouse tail was transected with a razor blade at approximately 6 mm from its end. The bleeding tail was immediately immersed in saline thermostated at 37°C and the bleeding time was recorded. The end point was defined the arrest of bleeding lasting for more than 30 s.
All animal studies were approved by the Animal Research Ethics Board.
Results
Protein expression and purification
The expressed SFH in bacteria was extracted by repeated freezing and thawing. The supernatant was applied to Source 15Q and followed by Superdex 75 (Fig. 2). HPLC showed the purified product was up to 96% of normalized purity. MALDI-TOF monitored a molecular ion peak at m/z 22,986.1Da for SFH. The isoelectric point (pI) of SFH was 5.45 by capillary electrophoresis. The N-terminus of SFH was SSSFDKGK by Edman degradation.
Fibrinolytic activity of SFH
The clear zone method was employed to monitor the fibrinolytic activities of SFH and SAK at equimolar concentration (Fig. 3). The correlation between activity and sample concentration was expressed by the following equations:
Comparison of fibrinolytic activities of SFH and SAK (A) Fibrinolytic activities of SAK and SFH at different concentration by clear zones method in agar plates (5% agar plate containing 1 NIHU/ml human thrombin, 10 μg/ml human plasminogen and 0.8 mg/ml fibrinogen, pH 8.0. Twenty microliters of samples at different concentration previously diluted were pipetted into 4-mm diameter wells. The plates were incubated for 4 h at 37°C). (B) The specific fibrinolytic activity of SFH is 0.44-fold to that of SAK at equimolar concentration (The diameters of clear zones were plotted over the semi-logarithm of the concentration of step-diluted samples and the equations were regressed. A sak = 2.164 lnC sak + 21.61, (r 2 = 0.9698); A sfh = 2.164 lnC sfh + 19.84, (r 2 = 0.9868))
wherein, A sak and A sfh were activities of SAK and SFH, respectively, expressed as the diameter (mm) of the clear zone; C sak and C sfh were contents of SAK and SFH, respectively, expressed in nanomole.
Using Eqs. 1 and 2, the specific activity of SFH was calculated as 0.44-fold to that of SAK. It revealed that the extension at C-terminus of SAK significantly reduced the fibrinolytic activity of SAK.
SFH was separated into SAK and HV2 and recovered fibrinolytic and antithrombin activities by FXa in vitro
To validate the action of cleavage of SFH by FXa, cleaved products were monitored by both SDS-PAGE (Fig. 4A) and antithrombin activity (Fig. 4B). Within 5 min after FXa addition in vitro, SFH was rapidly cleaved into two fragments: SAK with linker peptide and free HV2. The released SAK fragment was clearly observed with an apparent molecular weight of about 16 kDa and its content increased along with the reaction time (Fig. 4A). However, the HV2 fragment irregularly migrated with a 24 kDa instead of 7 kDa, which overlapped with SFH in the used gel. The similar behavior of unusual electrophoretic mobility was also observed in other studies [20, 21]. We speculated that the rich acidic groups of hirudin decelerated its mobility.
Time course of SFH cleaved by FXa and released hirudin with anticoagulant activity in vitro (Cleavage condition: 0.2U FXa mixed with 0.2 mg SFH in 300 μl TA buffer (50 mM Tris–HCl, 100 mM NaCl, and 1 mM CaCl2, pH 8.0)). (A) SDS-PAGE showed SFH was cleaved to free SAK and HV2 fragments by FXa in vitro. (16.5% reduced SDS-PAGE. Lane 1 to 6, SFH was cleaved for 0, 5, 10, 30, 60, 180 min, respectively; lane 7, SAK; lane 8, HV2; lane 9, protein marker). (B) Cleaved SFH products presented anticoagulant activity by releasing free hirudin. (Ten microliters of reaction product was used for activity assay. Anticoagulant activities of reaction products were indicated as the final dilution folds that inhibited clot formation and specific activities were indicated as a ratio of activity to total protein content, ATU/mole protein. Relative special activities of cleaved products were the ratio compared on equimolar special activity of HV2)
To further monitor the cleavage of SFH by FXa, the antithrombin activity of SFH was detected. No antithrombin activity of intact SFH was detected without FXa (Fig. 4B). However, in the presence of FXa, free hirudin was liberated and its anticoagulant activity was recovered from SFH by FXa cleavage. In comparison to the special activity, about 25% anticoagulant activity was released from SFH by 0.2U FXa within 3 h in vitro.
An improved antithrombotic activity of SFH in carrageenin-induced MTT model
In the carrageenin-induced MTT model, both infarction frequency and mean length of mouse tail thrombus were determined. The infarction frequency in SFH group was significantly lower than that in both SAK and saline groups at equimolar dose (Table 2). Furthermore, the mean length of mice tail thrombus in SFH group was remarkably less than that in both SAK and saline groups (P < 0.05, Fig. 5A). In MTT model, SAK showed an apparent antithrombotic activity because of its fibrinolytic activity, whereas SFH showed a significantly improved antithrombotic activity in comparison with SAK. This enhanced antithrombotic activity of SFH suggested that it derived not only from fibrinolytic activity of SAK domain, but also from the native anticoagulant activity of HV2 liberated from SFH under catalysis of FXa during the evolvement of infarction. Otherwise, the intact SFH could not show such a high antithrombotic activity based on its fibrinolytic activity in vitro (Fig. 3). To further confirm the antithrombotic activity of SFH, an additional experiment (n = 6) was performed with a dose of SFH (50 nmole/kg), which showed an equivalent antithrombotic effect to that of SAK alone (155 nmole/kg).
SFH showed an improved antithrombotic and thrombolytic activities compared with SAK, HV2, mixture of free SAK plus free HV2 (SAK+HV2) at equimolar concentration in vivo (A) Improved antithrombotic activities of SFH compared with its free components in MTT model. Tail infarction length was determined after 48 h of thrombus induction by k-carrageenin in mice. The mean length of mouse tail thrombus in the fusion protein group was remarkably less than those in SAK and control groups (P < 0.05). (B) An improved thrombolytic function of SFH evaluated in IVC thrombosis model in the rats (n = 10). A significant reduction in thrombus size was observed for SFH group compared with SAK (P < 0.01), HV2 (P < 0.01) and saline alone (P < 0.01), respectively. No significant difference was observed for SFH from the combination of SAK with HV2 (P > 0.5)
An improved thrombolytic activity of SFH in IVC thrombosis model in rats
The clot sizes of drug administration groups were significantly smaller than that of the saline control group. The clot size (0.87 ± 1.78 mg) of the SFH group, in particular, markedly reduced in comparison with the SAK (5.67 ± 2.67 mg, P < 0.01), HV2 (5.77 ± 2.36 mg, P < 0.01) and saline (9.96 ± 4.03 mg, P < 0.01) groups, respectively (Fig. 5B). Moreover, a significantly improved thrombolytic activity of SFH equal to that of the combination of SAK with HV2 was observed (Fig. 5B), although no anticoagulant activity of intact SFH was observed in absence of FXa or clot in vitro (Fig. 4B). This improved thrombolytic activity in the rat model is consistent with the improved antithrombotic activity observed in the MTT model above (Table 2 and Fig. 5A).
SFH did not prolong TT, aPTT or PT of peripheral blood
Basically, the interruption of the coagulation pathway accounts for bleeding risk. Based on the hypothesis that reducing hirudin concentration or activity in peripheral blood and restricting its activity on the site of the thrombus would be one of the effective strategies to alleviate bleeding risk, TT, aPTT and PT of peripheral blood were employed to monitor bleeding risk.
There was no difference in TT, aPTT and PT values in all five groups before drug administration. At 30 and 60 min after drug administration (31.5 nmole/kg), TT, aPTT and PT in the SFH group did not prolong in comparison with those in other drug-administration groups or controls before drug administration (Fig. 6). However, at both 30 and 60 min after drug administration, significantly prolonged TT (P < 0.01, Fig. 6A), aPTT (P < 0.05, Fig. 6B) and PT (P < 0.05, Fig. 6C) were observed in groups receiving equimolar HV2 and SAK+HV2 compared with both other groups (saline, SAK, and SFH groups) and controls before drug administration. It indicated that SFH did not show antithrombin activity at the thrombus-free site in peripheral blood and did not impose bleeding/hemorrhage risk.
SFH did not increase TT, aPTT or PT. SFH group did not increase (A) TT, (B) aPTT or (C) PT compared with both before drug administration and saline control groups at 30 and 60 min after drug administration (31.5 nmole/kg). Whereas, a significant prolongs of TT (P < 0.01), aPTT (P < 0.05) and PT (P < 0.05) were observed in groups receiving HV2 and SAK+HV2 compared with both before drug administration and other groups (SFH, SAK and saline groups)
Less bleeding time of SFH than the mixture of SAK with HV2 in the tail transection model
The bleeding times at 20 min after drug treatment were measured in tail-transected mice receiving 200 nmole/kg of each drug. The bleeding time (299 ± 148 s, 1.9-fold increase compared with saline group (157 ± 61 s)) in mice treated with SFH was significantly less prolonged than half in mice receiving equimolar SAK (531 ± 229 s) and the mixture of SAK plus HV2 (646 ± 159 s) (3.4- and 4.1-fold, compared with the saline group; P < 0.01 and 0.01, respectively; Fig. 7).
Discussion
Anticoagulant agents such as heparin and hirudin are proposed to be used to avoid reocclusion [14, 15, 45]. Hirudin as a combinative anticoagulant agent has several advantages: first, thrombin bound to fibrin or fibrin degradation product is resistant to inhibition by the heparin–antithrombin complex, but susceptible to inactivation by hirudin [46]; second, animals treated with t-PA and concomitant hirudin experienced less reocclusion than those with t-PA and heparin or aspirin [47]; third, hirudin exhibited excellent activity of inhibiting thrombin-mediated platelet aggregation [47] and seemed to displace FXa from its complex with the components of prothrombinase complex [48]. Thus, to combine thrombolysis with anticoagulation to reduce the occurrence of reocclusion and bleeding complication, SAK and HV2 were chosen in this study.
To circumvent the bifunctional activity and the dilemma between anticoagulant activity and hemorrhage event, we introduced FXa recognition site to the novel bifunctional fusion protein because an FXa is an essential activated factor for blood coagulation. Intact SFH showed no activity at the thrombus-free sites without FXa. As SFH arrived at the clot site, hirudin was locally released and its anticoagulant activity was present where this activity was needed in vivo. SFH retained fibrinolytic activity of SAK, which is consistent with the previous reports [21, 22]. However, we also found that SFH showed less than half of fibrinolytic activity at the equimolar concentration to that of SAK in vitro (Fig. 3). This apparent decrease of fibrinolytic activity SFH in vitro might result from the link with hirudin, but the fibrinolytic activity in vivo did not decrease (Table 2, Fig. 5).
Our results demonstrated that FXa began to cleave SFH rapidly within 5 min, but did not completely cleave it in vitro within 3 h. The dynamics of the cleavage reaction is closely related not only to the cleaved protein, but also to the reaction condition and the special activity of FXa itself in vitro. Previous studies reported that the reaction rate of FXa to prothrombin in vivo should be increased at least 19,000-fold at the site of thrombus compared with that in vitro [49, 50]. Therefore, the activity of FXa to SFH in vivo should be much higher than that in vitro and SFH should be much more easily cleaved to release the full fibrinolytic and anticoagulant activities in the vicinity of the thrombus in vivo than in vitro. Actually, two animal experiments above supported this hypothesis.
The antithrombotic effect of HV2 alone was better than SAK alone and SAK group showed a higher infarction frequency in MTT model (Table 2 and Fig. 5A). These results are consistent with previous reports on the difference between fibrinolytic and anticoagulant agents such as streptokinase and heparin [38, 51]. Therefore, the MTT infarction model is more suitable for evaluation of anticoagulants than fibrinolytics. It is equally well suited for investigating whether FXa cleaved SFH and liberated the anticoagulant activity of hirudin.
In both MTT and IVC thrombosis models, we observed that SFH performed better than SAK and HV2 alone (Fig. 5). Besides the bifunctional activity, a significantly lower bleeding risk in mice receiving SFH than in mice receiving the mixture of free SAK and HV2 was observed not only through monitoring TT (P < 0.01), aPTT (P < 0.05) and PT (P < 0.05), but also in bleeding time in the vessel-injured animal model. In fact, aPTT and TT better reflect the bleeding risk triggered by anticoagulants, while the tail transection bleeding time reflects the bleeding risk triggered by both fibrinolytics and anticoagulants. That is why a less variant aPTT and TT in mice receiving SAK while a less variant bleeding time in mice receiving HV2 is shown in Figs. 6 and 7. Comparing the bleeding time in mice receiving SFH with those in mice receiving SAK, HV2 (329 ± 153 s) and the mixture of SAK plus HV2, the remaining fibrinolytic activity of SFH mostly accounted for the prolonged bleeding time in mice receiving SFH. This lower bleeding risk of SFH is not only because of N-terminal extension of HV2, but also because of the reduced fibrinolytic activity of intact SFH.
It should be noted that, according to design idea of SFH, the man-made vessel-injured model amplified the monitored bleeding risk of SFH because the artificial bleeding synchronously triggered the coagulation pathway and resulted in the liberation of free HV2 and its anticoagulant activity. So, the actual bleeding risk might be less than the result monitored by bleeding time at the cut site but much closer to the results monitored by aPTT and TT without a man-made wound.
In summary, the newly designed SFH is a promising candidate for effective and safe clinical thrombosis therapy. The potential therapeutic use of SFH resides in its three features: first, an improved antithrombotic and fibrinolytic bifunction; second, no anticoagulant activity at thrombus-free sites and locally recovered its maximal anticoagulant activity at the site of thrombus where it is needed; and third, based on the second, SFH significantly reduced the side effects of systemic bleeding risk in animal models. Further investigation is under way to determine possible clinical application.
References
Anderson RN, Smith BL (2003) Deaths: leading causes for 2001. National Vital Statistics Reports 52:1–12
Collen D (1998) Staphylokinase: a potent, uniquely fibrin-selective thrombolytic agent. Nat Med 4:279–284
Lijnen HR, Van Hoef B, Matsuo O, Collen D (1992) On the molecular interactions between plasminogen-staphylokinase, alpha 2-antiplasmin and fibrin. Biochim Biophys Acta 1118:144–148
Ohman EM, Harrington RA, Cannon CP, Agnelli G, Cairns JA, Kennedy JW (2001) Intravenous thrombolysis in acute myocardial infarction. Chest 119:253S–277S
Vanderschueren S, Barrios L, Kerdsinchai P, Van den Heuvel P, Hermans L, Vrolix M, De Man F, Benit E, Muyldermans L, Collen D et al (1995) A randomized trial of recombinant staphylokinase versus alteplase for coronary artery patency in acute myocardial infarction. The STAR Trial Group. Circulation 92:2044–2049
Investigaors TGa (1993) The effects of tissue plasminogen activator, streptokinase, or both on coronary–artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators. N Engl J Med 329:1615–1622
Hennekens CH, O’Donnell CJ, Ridker PM, Marder VJ (1995) Current issues concerning thrombolytic therapy for acute myocardial infarction. J Am Coll Cardiol 25:18S–22S
Tsikouris JP, Tsikouris AP (2001) A review of available fibrin-specific thrombolytic agents used in acute myocardial infarction. Pharmacotherapy 21:207–217
Vanderschueren S, Stockx L, Wilms G, Lacroix H, Verhaeghe R, Vermylen J, Collen D (1995) Thrombolytic therapy of peripheral arterial occlusion with recombinant staphylokinase. Circulation 92:2050–2057
Eccleston D, Topol EJ (1995) Inhibitors of platelet glycoprotein IIb/IIIa as augmenters of thrombolysis. Coron Artery Dis 6:947–955
Yasuda T, Gold HK, Yaoita H, Leinbach RC, Guerrero JL, Jang IK, Holt R, Fallon JT, Collen D (1990) Comparative effects of aspirin, a synthetic thrombin inhibitor and a monoclonal antiplatelet glycoprotein IIb/IIIa antibody on coronary artery reperfusion, reocclusion and bleeding with recombinant tissue-type plasminogen activator in a canine preparation. J Am Coll Cardiol 16:714–722
Rapold HJ (1990) Promotion of thrombin activity by thrombolytic therapy without simultaneous anticoagulation. Lancet 335:481–482
Gruber A, Harker LA, Hanson SR, Kelly AB, Griffin JH (1991) Antithrombotic effects of combining activated protein C and urokinase in nonhuman primates. Circulation 84:2454–2462
Zeymer U, von Essen R, Tebbe U, Niederer W, Maurer W, Vogt A, Neuhaus KL (1995) Frequency of “optimal anticoagulation” for acute myocardial infarction after thrombolysis with front-loaded recombinant tissue-type plasminogen activator and conjunctive therapy with recombinant hirudin (HBW 023). ALKK Study Group. Am J Cardiol 76:997–1001
Yao SK, McNatt J, Anderson HV, Eidt J, Cui KX, Golino P, Glas-Greenwalt P, Maraganore J, Buja LM, Willerson JT (1992) Thrombin inhibition enhances tissue-type plasminogen activator-induced thrombolysis, delays reocclusion. Am J Physiol 262:H374–H379
Markwardt F (1991) Hirudin and derivatives as anticoagulant agents. Thromb Haemost 66:141–152
Metz BK, White HD, Granger CB, Simes RJ, Armstrong PW, Hirsh J, Fuster V, MacAulay CM, Califf RM, Topol EJ (1998) Randomized comparison of direct thrombin inhibition versus heparin in conjunction with fibrinolytic therapy for acute myocardial infarction: results from the GUSTO-IIb trial. Global use of strategies to open occluded coronary arteries in acute coronary syndromes (GUSTO-IIb) investigators. J Am Coll Cardiol 31:1493–1498
Weitz JI, Buller HR (2002) Direct thrombin inhibitors in acute coronary syndromes: present and future. Circulation 105:1004–1011
Lijnen HR, Wnendt S, Schneider J, Janocha E, Van Hoef B, Collen D, Steffens GJ (1995) Functional properties of a recombinant chimeric protein with combined thrombin inhibitory and plasminogen-activating potential. Eur J Biochem 234:350–357
Wirsching F, Luge C, Schwienhorst A (2002) Modular design of a novel chimeric protein with combined thrombin inhibitory activity and plasminogen-activating potential. Mol Genet Metab 75:250–259
Szarka SJ, Sihota EG, Habibi HR, Wong S (1999) Staphylokinase as a plasminogen activator component in recombinant fusion proteins. Appl Environ Microbiol 65:506–513
Icke C, Schlott B, Ohlenschlager O, Hartmann M, Guhrs KH, Glusa E (2002) Fusion proteins with anticoagulant and fibrinolytic properties: functional studies and structural considerations. Mol Pharmacol 62:203–209
Wallace A, Dennis S, Hofsteenge J, Stone SR (1989) Contribution of the N-terminal region of hirudin to its interaction with thrombin. Biochemistry 28:10079–10084
Fortkamp E, Rieger M, Heisterberg-Moutses G, Schweitzer S, Sommer R (1986) Cloning and expression in Escherichia coli of a synthetic DNA for hirudin, the blood coagulation inhibitor in the leech. Dna 5:511–517
Peter K, Graeber J, Kipriyanov S, Zewe-Welschof M, Runge MS, Kubler W, Little M, Bode C (2000) Construction and functional evaluation of a single-chain antibody fusion protein with fibrin targeting and thrombin inhibition after activation by factor Xa. Circulation 101:1158–1164
Peter K, Gupta A, Nordt T, Bauer S, Runge MS, Bode C (2003) Construction and in vitro testing of a novel fab-hirudin-based fusion protein that targets fibrin and inhibits thrombin in a factor Xa-dependent manner. J Cardiovasc Pharmacol 42:237–244
Lian Q, Szarka SJ, Ng KK, Wong SL (2003) Engineering of a staphylokinase-based fibrinolytic agent with antithrombotic activity and targeting capability toward thrombin-rich fibrin and plasma clots. J Biol Chem 278:26677–26686
Szemraj J, Walkowiak B, Kawecka I, Janiszewska G, Buczko W, Bartkowiak J, Chabielska E (2005) A new recombinant thrombolytic and antithrombotic agent with higher fibrin affinity—a staphylokinase variant. I. In vitro study. J Thromb Haemost 3:2156–2165
Kaiser B (2002) Factor Xa–a promising target for drug development. Cell Mol Life Sci 59:189–192
Zhang ZQ, Yao LH, Hou YD (1990) Construction and application of a high-level expression vector containing PRPL promotor. Bingdu Xuebao 6:111–115
Johnson BH, Hecht MH (1994) Recombinant proteins can be isolated from E. coli cells by repeated cycles of freezing and thawing. Biotechnology (N Y) 12:1357–1360
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Saksela O (1981) Radial caseinolysis in agarose: a simple method for detection of plasminogen activator in the presence of inhibitory substances and serum. Anal Biochem 111:276–282
Schlott B, Hartmann M, Guhrs KH, Birch-Hirschfeid E, Pohl HD, Vanderschueren S, Van de Werf F, Michoel A, Collen D, Behnke D (1994) High yield production and purification of recombinant staphylokinase for thrombolytic therapy. Biotechnology (N Y) 12:185–189
Jutisz M, Martinoli G, Tertrin C (1962) Microdetermination of an anti-thrombic activity: hirudin Bull Soc Chim Biol (Paris) 44:461–469
Ohashi H, Katsuta-Enomoto Y, Yasufuku K, Okada K, Yano M (1991) Synthesis of human big endothelin-1 by sequence-specific proteolysis of a fusion protein in Escherichia coli. J Biochem (Tokyo) 110:628–634
Bekemeier H, Giessler AJ (1987) Thrombosis induction by different carrageenans in rats and mice. Naturwissenschaften 74:345–346
Bekemeier H, Hirschelmann R, Giessler AJ (1985) Carrageenin-induced thrombosis in rats and mice: a model for testing antithrombotic substances? Agents Actions 16:446–451
Hu SJ, Tian QL, Pei QY et al (1993) A new model for animal thrombosis in vivo. Chinese J Hematol 14:541–542
Elg M, Borjesson I, Carlsson S (2003) Three vehicle formulations for melagatran, a direct thrombin inhibitor, evaluated in a vena cava thrombosis model in the rat. Biopharm Drug Dispos 24:251–257
Millet J, Theveniaux J, Pascal M (1987) A new experimental model of venous thrombosis in rats involving partial stasis and slight endothelium alterations. Thromb Res 45:123–133
Monreal M, Silveira P, Monreal L, Monasterio J, Angles AM, Lafoz E, Lorente L (1991) Comparative study on the antithrombotic efficacy of four low-molecular-weight heparins in three different models of experimental venous thrombosis. Haemostasis 21:91–97
Dejana E, Villa S, de Gaetano G (1982) Bleeding time in rats: a comparison of different experimental conditions. Thromb Haemost 48:108–111
Momi S, Nasimi M, Colucci M, Nenci GG, Gresele P (2001) Low molecular weight heparins prevent thrombin-induced thrombo-embolism in mice despite low anti-thrombin activity. Evidence that the inhibition of feed-back activation of thrombin generation confers safety advantages over direct thrombin inhibition. Haematologica 86:297–302
Eisenberg PR (1991) Importance of modulating balance of procoagulant and fibrinolytic activity to success of antithrombotic therapy. Circulation 84:2601–2603
Weitz JI, Leslie B, Hudoba M (1998) Thrombin binds to soluble fibrin degradation products where it is protected from inhibition by heparin-antithrombin but susceptible to inactivation by antithrombin-independent inhibitors. Circulation 97:544–552
Badimon L, Badimon JJ, Lassila R, Heras M, Chesebro JH, Fuster V (1991) Thrombin regulation of platelet interaction with damaged vessel wall and isolated collagen type I at arterial flow conditions in a porcine model: effects of hirudins, heparin, and calcium chelation. Blood 78:423–434
Pizzo SV, Friedberg RC, Sze P, Winant R, Hudson D, Lazar JM, Johnson PH (1990) Recombinant hirudin displaces human factor Xa from its endothelial binding sites. Thromb Res 57:803–806
Betz A, Wong PW, Sinha U (1999) Inhibition of factor Xa by a peptidyl-alpha-ketothiazole involves two steps. Evidence for a stabilizing conformational change. Biochemistry 38:14582–14591
Suttie JW, Geweke LO, Martin SL, Willingham AK (1980) Vitamin K epoxidase: dependence of epoxidase activity on substrates of the vitamin K-dependent carboxylation reaction. FEBS Lett 109:267–270
Bekemeier H, Hirschelmann R, Giessler AJ (1984) Carrageenin-induced thrombosis in the rat and mouse as a test model of substances influencing thrombosis. Biomed Biochim Acta 43:S347–S350
Acknowledgments
The authors thank Professors Zhonghua Jiang, Yuanmin Li, Zhongxiong Tang and Lizhen Yuan for their fruitful advice and discussions. This work was supported by China Postdoctoral Science Foundation, 2002032086.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Shi, B., Yu, A., Liu, Y. et al. Locally activity-released bifunctional fusion protein enhances antithrombosis and alleviates bleeding risk. J Thromb Thrombolysis 24, 283–292 (2007). https://doi.org/10.1007/s11239-007-0036-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-007-0036-6