Abstract
Glucagon-like peptide 1 (GLP-1) is a cleavage product of the pre-proglucagon gene which is expressed in the α-cells of the pancreas, the L-cells of the intestine, and neurons located in the caudal brainstem and hypothalamus. GLP-1 is of relevance to appetite and weight maintenance because it has actions on the gastrointestinal tract as well as the direct regulation of appetite. It delays gastric emptying and gut motility in humans. In addition, interventricular injections of GLP-1 inhibit food intake, independent of the presence of food in the stomach or gastric emptying. Peripherally administered GLP-1 also affects the central regulation of feeding. It is therefore the synergistic actions of GLP-1 in the gut and brain, acting on both central and peripheral receptors that seem responsible for the effects of the hormone on satiety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Synthesis and secretion of GLP-1
Glucagon-like peptide 1 (GLP-1) is a cleavage product of the pre- proglucagon gene [1] which is expressed in the α-cells of the pancreas, the l-cells of the intestine, and neurons located in the caudal brainstem and hypothalamus [2]. GLP-1 is primarily synthesized and secreted by the L cells of the distal small intestine in response to a nutrient load, although non-nutrient driven secretion has also been reported [3, 4]. GLP-1 is also synthesized by a small population of neurones in the nucleus of the solitary tract (NTS) in the caudal brainstem which project to areas in the hypothalamus and hindbrain that express GLP-1 receptors (GLP-1- R) [5]. The major bioactive species in humans are GLP-1 (7–36) amide and GLP-1 (7–37).
In response to a nutrient load, GLP-1 is secreted in a biphasic fashion: the early response occurs within minutes, and lasts about 30 minutes post prandially while the second phase occurs an hour or so later [6, 7]. Given that the majority of L cells are located in the distal intestines, it is unlikely that direct contact with nutrients is responsible for the first phase of GLP-1 release. In fact, animal studies have shown that the autonomic nervous system, in particular, the vagus nerve, has an important role to play in mediating the early release of GLP-1 following a meal [8]. Administration of atropine, a muscarinic receptor antagonist in humans after an oral glucose load diminishes the magnitude of early GLP-1 release, an effect independent of gastric emptying [9]. More recently, Theodorakis et al. have shown that even though the density of L cells is lower in the duodenum, it is likely sufficient to explain early GLP-1 release [10]. Within the L-cell, the nutrient-sensing pathways that are involved in GLP-1 secretion are differentially sensitive to glucose, protein, fatty acids and bile acids, all of which are potent triggers for GLP-1 release [11]. Apart from GLP-1, other products of posttranslational modification of the proglucagon gene by prohormone convertase may also be important in glucose metabolism and energy balance. For example, oxyntomodulin inhibits gastrointestinal motility and stimulates pancreatic enzyme secretion and intestinal glucose uptake, in addition to having a role in the promotion of satiety [12]. GLP-2 up-regulates intestinal glucose transport, improves intestinal barrier function, and inhibits food intake, gastric emptying, and acid secretion [13, 14].
2 Role of GLP-1 in satiety
Satiation signals, produced by activation of gastric mechanoreceptors when the stomach is distended, are relayed via the vagal nerves to the NTS in the brainstem. The amount of gastric distension due to food intake is partly influenced by the rate of gastric emptying, which in turn affects postprandial glycemic excursions. GLP-1 delays gastric emptying and gut motility in healthy lean and obese subjects and patients with type 2 diabetes [15–17]. GLP-1 also contributes to the change in gastric volume that occurs in anticipation of food ingestion. This phenomenon is known as gastric accommodation and may affect the perception of stomach distention after food ingestion [18].
The role of the vagus nerve in promoting satiety appears dependent on the route of administration of GLP-1 as demonstrated in an experiment on vagotomized rats. Intravenous as opposed to intraperitoneal infusion of GLP-1 does not require an intact vagus to attenuate nutrient intake [19].
Central (interventricular) injections of GLP-1 inhibit food intake, independent of the presence of food in the stomach or gastric emptying [20]. Also, knock down of the preproglucagon gene in the NTS has been shown to result in hyperphagia and weight gain [21]. Mirroring these findings are neuroimaging studies showing that peripherally administered GLP-1 affects brain activity in areas involved in the regulation of feeding [22, 23]. It is therefore the synergistic actions of GLP-1 in the gut and brain, acting on both central and peripheral receptors that seem responsible for the effects of the hormone on satiety (Fig. 1).
The role of GLP-1 in modulating appetite. GLP-1 has effects on central and peripheral receptors. Afferent branches of the vagus relay information from chemoreceptors and mechanoreceptors in the gastrointestinal tract to the nucleus tractus solitarius (NTS). Circulating hormones could theoretically directly stimulate areas outside the blood brain barrier although the role of this pathway is of uncertain significance in normal physiology (−ve denotes an inhibitory effect, while + ve denotes a permissive/enhancing effect) [72,73,74]
However, the mechanisms involved in both these sites are likely distinct. In the NTS, GLP-1 that is produced also acts on local receptors thus creating a local feedback loop [24]. Orexigenic and anorexigenic neurones possess GLP-1 R so that GLP-1 binding promotes satiety [25]. For example mRNA levels of the orexigenic neuropeptide Y/agouti-related peptide (NPY/AgRP) neuron and the anorexigenic proopiomelanocortin (POMC) neuron, both of which have GLP-1 receptors, have been shown to decrease and increase respectively in the presence of central GLP-1 infusions [26]. These findings, however, are not consistent and others have shown that the effect of GLP-1 on satiety is primarily derived from its action on anorexigenic hormones so that when NPY/AgRP neurons are destroyed, the effect of GLP-1 on decreasing satiation persists [27]. In contrast, POMC has been well documented to induce anorexia in a variety of situations. POMC neurons project to the NTS (site of GLP-1 production) and paraventricular nucleus of the hypothalamus (PVN) and may contribute to the forebrain-brainstem signalling circuit modulating appetite [28]. GLP-1 receptors are found in the PVN, arcuate nucleus and ventromedial hypothalamus [29]. The reciprocal connection between the NTS and PVN of the hypothalamus allows integration of these anorexigenic signals and may be modulated by GLP-1 (Fig. 1).
Additionally, intracerebroventricular administration of GLP-1 is able to induce conditioned taste aversion likely due to a simultaneous effect on visceral sensation [30].
Pharmacologic studies in animals have shown that suppression of food intake after peripheral administration of the GLP-1 receptor agonists exendin-4 and liraglutide is mediated by activation of GLP-1R expressed on vagal afferents as well as direct CNS GLP-1R activation, highlighting the importance of the interaction between peripheral and central receptors [31].
3 The contribution of GLP-1 to bariatric surgery
Post-prandial GLP-1 concentrations are increased following Roux-en-Y gastric bypass, an observation that has fuelled interest in investigating the role of GLP-1 in mediating weight loss and remission of metabolic derangements following surgery [32–34]
All forms of bariatric surgery lead to weight loss to a greater or lesser extent. the superiority of RYGB over adjustable gastric band and perhaps sleeve gastrectomy, highlights an important distinction between purely restrictive and restrictive/malabsorptive procedures. Compared to the purely restrictive sleeve gastrectomy, patients with type 2 diabetes who underwent RYGB exhibited greater truncal fat loss and improved beta cell function at 24 months despite comparable diabetes remission at 12 months [35]. There are some important caveats to this –this study can be criticized in terms of the small (−er) numbers restudied and the gender differences between RYGB and SG groups (thereby introducing a confounder in regards to initial body composition) limiting the generalizability of the study [36].
Adjustable gastric banding (AGB) does not trigger an increase GLP-1 secretion. However, when rats which had undergone AGB were treated with a GLP-1 agonist, body weight decreased both while the band was deflated and inflated. Interestingly, band inflation triggered neural activation in areas of the NTS known to be targeted by GLP-1 receptor agonism, offering a potential mechanism for the interaction [37].
We and other have studied the role of endogenous GLP-1 in glucose metabolism following RYGB using Exendin 9,39, a competitive antagonist of GLP-1 at its cognate receptor [38]. Non-diabetic subjects who were on average 5 years post-RYGB and at a steady weight were administered a mixed meal; glucose fluxes were studied in the presence or absence of Exendin 9,39 infused at a rate of 300 pmol/kg/min. Age and weight-matched control subjects were studied in a similar experimental design. 111In-DTPA labelling of the solid portion of the meal allowed measurement of gastric emptying and orocecal transit with a gamma camera. We found that Exe-9,39 accelerated gastric emptying suggesting that following RYGB surgery, endogenous GLP-1 delays gastrointestinal transit. Measurement of gastric emptying using scintigraphy under the influence of exendin 9,39 in otherwise healthy humans has demonstrated either no effect or accelerated gastric emptying [39, 40].
Although important, the magnitude of the contribution of GLP-1 to weight loss and remission of metabolic abnormalities after bariatric surgery was challenged by Wilson-Perez et al. who studied vertical sleeve gastrectomy in GLP-1 receptor knock-out mice models [41]. These mice, when compared to their wild-type counterparts responded similarly in terms of reduced body weight and body fat, improvements in glucose homeostasis and altered food choice. These intriguing findings may absolve GLP-1 from mediating much of the beneficial outcomes following vertical sleeve gastrectomy but may not necessarily apply to RYGB which also reconfigures anatomy by moving the distal small intestine closer to incoming nutrients from the stomach and bypassing the proximal small intestine.
Whether GLP-1 contributes to the weight loss seen after bariatric surgery remains to be determined.
4 Role of GLP-1 in the gastrointestinal tract
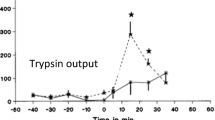
GLP-1 appears to affect gastrointestinal motility through its action on both central and peripheral receptors. The vagus nerve plays an important role in mediating these effects as shown in both animal and human models, perhaps through its action on the circular muscle of the intestines [16, 42–44]. In mouse models, GLP-1 was found to inhibit intestinal motility through the direct interaction and activation of GLP-1R on enteric neurons [44]. When GLP-1 was directly infused into the intracerebroventricular space of rats, gastric emptying was inhibited suggesting an interaction between peripheral and central GLP-1 receptors [45]. In contrast to the upper GI tract, in the colon, GLP-1 serves to accelerate colonic transit an effect that is also likely mediated by the parasympathetic nervous system [46, 47]. In addition, GLP-1 contributes to the ileal brake, an inhibitory feedback loop designed to optimize the digestion and absorption of nutrients [48].
The role of GLP-1 in gastric emptying and accommodation in the fasting and post-prandial state was investigated in a placebo-controlled study by Delgado-Aros et al. [18]. Healthy volunteers were infused GLP-1 and administered an injection of 99mTc-sodium, which is taken up by the gastric wall. Single photon emission computed tomography (SPECT) images of the stomach were taken and processed to produce a 3- dimensional image allowing volume calculations. They demonstrated an increase in volume of the proximal and distal stomach in response to GLP-1 in both the fasting and fed states. These findings have also previously been demonstrated by barostat studies [49]. Delayed gastric emptying was found to be a result of relaxation of the proximal stomach accompanied by an increased tone of the antropyloric region. To compare the effects of GLP-1 and placebo on maximum tolerated volume (MTV, the volume ingested until maximum satiety is reached), the same participants were given a liquid meal and used a visual analog scale to score the presence of symptoms such as bloating, fullness, nausea or pain. No difference in MTV was observed with GLP-1 despite changes in gastric accommodation and emptying. This observation could be explained by its known role on central receptors in the regulation of food intake, independent of its effects on gastrointestinal motility.
The role of the vagal nervous system in mediating the effects of GLP-1 on gastric accommodation was studied by the same group [50]. Two observations suggested an important role for the vagus nerve: 1. Gastric tone is maintained by vagal cholinergic input. 2. Postprandial pancreatic polypeptide release (under vagal control) was blunted in the presence of GLP-1.
The group studied patients with diabetes and cardiovagal neuropathy in the same experimental design as before. GLP-1 did not influence gastric volume in this group, implying that a vagally-induced mechanism was important for GLP-1’s action on the stomach. However gastric volume response to a meal in these patients was no different when compared to healthy volunteers. This observation illustrates that gastric accommodation after vagotomy recovers with time as has been shown in both animal and human studies.
5 Clinical effects on weight of GLP-based therapy
In response to a meal, GLP-1 delays gastric emptying and increases gastric volumes. GLP-1 enhances insulin secretion and inhibits glucagon-release in a glucose-dependent manner both in normal individuals as well as in patients with type 2 diabetes [51]. In patients with type 2 diabetes, GLP-1 agonist infusion in pharmacologic doses enhanced satiation and promoted weight loss [52]. Hence GLP-1 therapy in humans reduces food intake, appetite and hunger and promotes fullness and satiety with the ultimate result of promoting weight loss.
GLP-1 receptor agonists are currently FDA approved only for the treatment of type 2 diabetes, but clinical trials have consistently shown that they also produce weight loss when compared to controls. A meta-analysis of GLP-1 agonists (twice daily exenatide, daily liraglutide or weekly exenatide) on obese individuals with and without diabetes showed that when compared to controls, treatment groups achieved a greater weight loss (weighted mean difference −2.9 kg, 95 % confidence interval −3.6 to −2.2; 21 trials, 6,411 participants) [53]. Placebo-controlled trials have demonstrated a dose-dependent effect of GLP-1 receptor agonists on weight loss. In patients with type 2 diabetes already on an oral hypoglycemic agent, exenatide 10 μg twice daily produced almost twice the amount of weight loss afforded by the 5 μg twice daily dose, a finding that was subsequently reproduced, though not quite at the same magnitude, by other groups [54, 55,56]. Increasing doses of liraglutide up to 3 mg per day continue to produce incremental weight loss in a group of patients with type 2 diabetes [57]. When exenatide or liraglutide was compared to insulin therapy in patients with similar glycemic control, weight loss with GLP-1 receptor agonist treatment ranged from 1.8 to 4.1 kg, while weight gain with insulin therapy varied between 1.0 and 4.1 kg [44, 58–60]. There was no significant difference in weight loss in patients with type 2 diabetes on maximally tolerated oral hypoglycemic therapy who were either initiated on liraglutide 1.8 mg per day or exenatide 10 μg twice daily [61]. However, liraglutide at a dose of 1.8 mg per day produced greater weight loss when compared to exenatide 2 mg once weekly, in patients with type 2 diabetes on maximum oral hypoglycemic agents over a 26-week period [62]
A randomized placebo-controlled trial of GLP-1 agonist therapy (exenatide) in obese adolescents resulted in modest weight loss, an effect that was equivalent or better than a similar duration of metformin or orlistat therapy in this group of patients [63]. The most commonly reported side effects of nausea and vomiting were similar to that reported in the adult literature and did not result in drop outs from the study.
The weight loss observed with GLP-1 agonist therapy may be associated with reductions in total body fat, in particular visceral and truncal adipose [64, 65].
Also of interest is the successful use of GLP-1 agonists in the treatment of hypothalamic obesity, suggesting that at least in this cohort, GLP-1 analogues were capable of inducing weight loss despite hypothalamic damage [66].
Unlike pure dietary measures, weight loss may be sustained for up to a period of 3 years in the presence of GLP-1 agonist therapy [67, 68]. However, once therapy is discontinued, there is some regain of weight [69]. There seems to be minimal effect of GLP-1 on energy expenditure per se and thus the overall negative energy balance seen with GLP-1 therapy is largely a result of decreased energy intake [70].
6 Conclusion
The role of GLP-1 in the modulation of appetite and weight is orchestrated by a complex brain-gut relationship. GLP-1 is primarily secreted by the enteroendocrine cells, but there is additionally a central nervous system source of GLP-1. Activation of GLP-1 receptors present in the CNS and the gut is further modulated by cholinergic signals from the vagus nerve. Through these and other still imprecise mechanisms, GLP-1 in both physiologic and pharmacologic doses promotes satiety, affects mechanistic properties of the GI tract and results in negative energy balance. Additionally, its success in promoting weight loss makes GLP-1 agonist therapy an attractive option in the management of type 2 diabetes. What needs to be balanced against this is the reported association between GLP-1 receptor agonist therapy and pancreatitis, pancreatic hyperplasia and pancreatic neoplasia [71]. Of interest, recent work in a novel transgenic mouse model confirms the presence of GLP-1 receptors in the vasculature of the exocrine pancreas with only sporadic GLP-1 receptors identifiable in the pancreatic ducts [29]. The implication that GLP-1 agonist therapy is directly related to the adverse outcomes observed is still very much up for debate.
7 Future directions
The discovery of GLP-1 has sparked major innovation in the therapy of type 2 diabetes as well as a better understanding of an interaction between the gut and the pancreas to modulate glucose homeostasis as well as appetite and weight. At present GLP-1 receptor agonism has relatively small but significant effects on weight. The reasons for this are still uncertain and efforts are underway to better understand the endogenous factors that dampen GLP-1 signalling. Moreover, compounds that are agonists for GLP-1 and for other receptors important in weight regulation may hold future therapeutic promise.
References
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39.
Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology. 2007;132(6):2131–57.
Dailey MJ et al. Disassociation between preprandial gut peptide release and food-anticipatory activity. Endocrinology. 2012;153:132–42.
Vahl TP et al. Meal-anticipatory glucagon-like peptide-1 secretion in rats. Endocrinology. 2010;151:569–75.
Tang-Christensen M, Vrang N, Larsen PJ. Glucagon-like peptide containing pathways in the regulation of feeding behaviour. Int J Obes Relat Metab Disord. 2001;25 Suppl 5:S42–7.
Elliott RM, Morgan LM, Tredger JA, Deacon S, Wright J. Glucagon-like peptide-1 (7–36) amide and glucose-dependent insulinotropic polypeptide secretion in response to nutrient ingestion in man: acute post-prandial and 24-h secretion patterns. J Endocrinol. 1993;138:159–66.
Hermann C, Goke R, Richter G, Fehmann HC, Arnold R, Goke B. Glucagon-like peptide-1 and glucose-dependent insulin-releasing polypeptide plasma levels in response to nutrients. Digestion. 1995;56:117–26.
Rocca AS, Brubaker PL. Role of the vagus nerve in mediating proximal nutrient-induced glucagon- like peptide-1 secretion. Endocrinology. 1999;140(4):1687–94.
Balks HJ, Holst JJ, Von Zur MA, Brabant G. Rapid oscillations in plasma glucagon-like peptide-1 (GLP-1) in humans: Cholinergic control of GLP-1 secretion via muscarinic receptors. J Clin Endocrinol Metab. 1997;82(3):786–90.
Theodorakis MJ, Carlson O, Michopoulos S, et al. Human duodenal enteroendocrine cells: source of both incretin peptides, GLP-1 and GIP. Am J Physiol Endocrinol Metab. 2006;290:E550–9.
Tolhurst G, Reimann F, Gribble FM. Nutritional regulation of glucagon-like peptide-1 secretion. J Physiol. 2009;587(1):27–32.
Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Oxyntomodulin from distal gut: role in regulation of gastric and pancreatic functions. Dig Dis Sci. 1989;34:1411–9.
Tang-Christensen M, Larsen PJ, Thulesen J, Rømer J, Vrang N. The proglucagon-derived peptide, glucagon-like peptide-2, is a neurotransmitter involved in the regulation of food intake. Nat Med. 2000;6(7):802–7.
Lovshin J, Estall J, Yusta B, Brown TJ, Drucker DJ. Glucagon-like Peptide (GLP)-2 action in the murine central nervous system is enhanced by elimination of GLP-1 receptor signaling. J Biol Chem. 2001;276(24):21489–99.
Nauck MA, Niedereichholz U, Ettler R, et al. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol. 1997;273:E981–8.
Schirra J, Wank U, Arnold R, Goke B, Katschinski M. Effects of glucagon-like peptide-1 (7–36) amide on motility and sensation of the proximal stomach in humans. Gut. 2002;50:341–8.
Meier JJ, Gallwitz B, Salmen S, et al. Normalization of glucose concentrations and deceleration of gastric emptying after solid meals during intravenous glucagon-like peptide 1 in patients with type 2 diabetes. J Clin Endocrinol Metab. 2003;88:2719–25.
Delgado-Aros S, Doe-Young K, Burton DD, Thomforde GM, et al. Effect of GLP-1 on gastric volume, emptying, maximum volume ingested, and postprandial symptoms in humans. Am J Physiol Gastrointest Liver Physiol. 2002;282:G424–31.
Ruttimann EB et al. Intrameal hepatic portal and intraperitoneal infusions of glucagon-like peptide-1 reduce spontaneous meal size in the rat via different mechanisms. Endocrinology. 2009;150:1174–81.
Turton MD, O’Shea D, Gunn I, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379:69–72.
Barrera JG et al. Hyperphagia and increased fat accumulation in two models of chronic CNS glucagon-like peptide-1 loss of function. J Neurosci. 2011;31:3904–13.
Chaudhri OB, Parkinson JR, Kuo YT, et al. Differential hypothalamic neuronal activation following peripheral injection of GLP-1 and oxyntomodulin in mice detected by manganese-enhanced magnetic resonance imaging. Biochem Biophys Res Commun. 2006;350:298–306.
Min DK, Tuor UI, Koopmans HS, Chelikani PK. Changes in differential functional magnetic resonance signals in the rodent brain elicited by mixed-nutrient or protein-enriched meals. Gastroenterology. 2011;141:1832–41.
Dailey M.J., Moran T. H. Glucagon-like peptide 1 and appetite. Trends in Endocrinology and Metabolism. 2013; 24 (2).
Larsen PJ et al. Central administration of glucagon-like peptide-1 activates hypothalamic neuroendocrine neurons in the rat. Endocrinology. 1997;138:4445–55.
Seo S. Acute effects of glucagon-like peptide-1 on hypothalamic neuropeptide and AMP activated kinase expression in fasted rats. Endocr J. 2008;55:867–74.
Bugarith K et al. Basomedial hypothalamic injections of neuropeptide Y conjugated to saporin selectively disrupt hypothalamic controls of food intake. Endocrinology. 2005;146:1179–91.
Blevins JE, Baskin DG. Hypothalamic-brainstem circuits controlling eating. Forum Nutr. 2010;63:133–40.
Richards P, Parker HE, Adriaenssens AE, et al. (2013) Identification and characterisation of glucagon-like peptide-1 receptor expressing cells using a new transgenic mouse model. Diabetes; Publish Ahead of Print, published online December 2, 2013.
Kinzig KP et al. The diverse roles of specific GLP-1 receptors in the control of food intake and the response to visceral illness. J Neurosci. 2002;22:10470–6.
Dailey MJ, Moran T. H. Glucagon-like peptide 1 and appetite. Trends in Endocrinology and Metabolism. 2013;24 (2).
Kellum JM, Kuemmerle JF, O’Dorisio TM. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg. 1990;211:763–70.
Laferrère B, Teixeira JMJ. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008;93:2479–85.
le Roux CW, Aylwin SJ, Batterham RL. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243:108–14.
Kashyap SR, Bhatt DL, Wolski K. Metabolic effects of bariatric surgery in patients with moderate obesity and type 2 diabetes: analysis of a randomized control trial comparing surgery with intensive medical treatment. Diabetes Care. 2013;36:2175–82.
Gagner M. Sleeve gastrectomy: an ideal choice for T2DM. Nat Rev Endocrinol. 2013;9:623.
Habegger KM, Kirchner H, Yi CX, Heppner KM, et al. GLP-1R agonism enhances adjustable gastric banding in diet-induced obese rats. Diabetes Care. 2013;62(9):3261–7.
Shah M, Law JH, Micheletto F, et al. Contribution of endogenous glucagon-like peptide-1 to glucose metabolism after Roux-en-Y gastric bypass. Diabetes. 2014;63:1–10.
Deane AM, Nguyen NQ, Stevens JE. Endogenous glucagon-like peptide-1 slows gastric emptying in healthy subjects, attenuating postprandial glycemia. J Clin Endocrinol Metab. 2010;95:215–21.
Nicolaus M, Brödl J, Linke R, Woerle H-J, Göke B, Schirra J. Endogenous GLP-1 regulates postprandial glycemia in humans: relative contributions of insulin, glucagon, and gastric emptying. J Clin Endocrinol Metab. 2011;96:229–36.
Wilson-Perez HE, Chambers AP, Ryan KK, Li B, Sandoval DA, et al. Vertical sleeve gastrectomy is effective in two genetic mouse models of glucagon-like peptide 1 receptor deficiency. Diabetes. 2013;62(7):2380–5.
Nea I. Glucagon-like peptide-1 inhibits gastric emptying via vagal afferent-mediated central mechanisms. Am J Physiol Rev. 1997;273:G920–7.
Aea W. Glucagon-like peptide-1 inhibits gastropancreatic function by inhibiting central parasympathetic outflow. Am J Physiol. 1998;275:G984–92.
Aea A. Peripheral motor action of glucagon-like peptide-1 through enteric neuronal receptors. Neurogastroenterol Motil. 2010;22:664–e203.
Mea T-C. Central administration of GLP-1-(7–36) amide inhibits food and water intake in rats. Am J Physiol. 1996;271:R848–56.
Gulpinar MA. Glucagon-like peptide (GLP-1) is involved in the central modulation of fecal output in rats. Am J Physiol Gastrointest Liver Physiol. 2000;278:924–9.
Ayachi SE. Contraction induced by glicentin on smooth muscle cells from the human colon is abolished by exendin (9–39). Neurogastroenterol Motil. 2005;17:302–9.
Yoder SM. Stimulation of incretin secretion by dietary lipid: is it dose dependent? Am J Physiol Gastrointest Liver Physiol. 2009;297:299–305.
Wank U, Schirra J, Arnold R, Goke B, Katschinki M. Effects of GLP-1 on proximal gastric motor and sensory function in human. Gastroenterology. 1998;114:A1190.
Delgado-Aros S, Vella A, Camilleri M, et al. Effects of glucagon-like peptide-1 and feeding on gastric volumes in diabetes mellitus with cardio-vagal dysfunction. Neurogastroenterol Motil. 2003;15:435–43.
Holst JJ, Toft-Nielsen MB, Orskov C, Nauck M, Willms B. On the effects of glucagon-like peptide-1 on blood glucose regulation in normal and diabetic subjects. Ann N Y Acad Sci. 1996;805:729–36.
Zander M, Madsbad S, Madsen JL, Holst JJ. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and beta-cell function in type 2 diabetes: a arallel-group study. Lancet. 2002;359:824–30.
Vilsboll T, Christensen M, Junker AE FKK, Gluud LL. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:7771.
Buse JB, Henry RR, Han J, Kim DD, MS F, Baron AD. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care. 2004;27:2628–35.
DeFronzo RA, Ratner RE, Han J, et al. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care. 2005;28:1092–100.
Moretto TJ, Milton DR RT, Macconell LA, Okerson T, AM W, Brodows RG. Efficacy and tolerability of exenatide monotherapy over 24 weeks in antidiabetic drug-naive patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel group study. Clin Ther. 2008;30:1448–60.
Astrup A, Rossner S, Van GL, et al. Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet. 2009;374:1606–16.
Bergenstal R, Lewin A, Bailey T, Chang D, Gylvin T, Roberts V. Efficacy and safety of biphasic insulin aspart 70/30 versus exenatide in subjects with type 2 diabetes failing to achieve glycemic control with metformin and a sulfonylurea. Curr Med Res Opin. 2009;25:65–75.
Russell-Jones D, Vaag A, Schmitz O, et al. Liraglutide vs insulin glargine and placebo in combination with metformin and sulfonylurea therapy in type 2 diabetes mellitus (LEAD-5 met + SU): a randomised controlled trial. Diabetologia. 2009;52:2046–55.
Gallwitz B, Bohmer M, Segiet T, et al. Exenatide twice daily versus premixed insulin aspart 70/30 in metformin-treated patients with type 2 diabetes: a randomized 26-week study on glycemic control and hypoglycemia. Diabetes Care. 2011;34:604–6.
Buse JB, Rosenstock J, Sesti G, et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet. 2009;374(9683):39–47.
Buse JB, Nauck M, Forst T. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet. 2013;381:117–24.
Kelly A, Rudser KD, Nathan BM, Fox CK, et al. The effect of glucagon-like peptide-1 receptor agonist therapy on body mass index in adolescents with severe obesity. JAMA Pediatr. 2013;167(4):355–60.
Bunck MC, Diamant M, Eliasson B, et al. Exenatide affects circulating cardiovascular risk biomarkers independently of changes in body composition. Diabetes Care. 2010;33:1734–7.
Jendle J, Nauck MA, Matthews DR, Frid A, Hermansen K, et al. Weight loss with liraglutide, a once-daily human glucagon-like peptide-1 analogue for type 2 diabetes treatment as monotherapy or added to metformin, is primarily as a result of a reduction in fat tissue. Diabetes Obes Metab. 2009;11:1163–72.
Zoicas F, Droste M, Mayr B, Buchfelder M, Schofl C, et al. GLP-1 analogues as a new treatment option for hypothalamic obesity in adults: report of nine cases. Eur J Endocrinol. 2013;168(5):699–706.
Garber A, Henry RR RR, Hale P, CT C, Bode B. Liraglutide, a once-daily human glucagon-like peptide 1 analogue, provides sustained improvements in glycaemic control and weight for 2 years as monotherapy compared with glimepiride in patients with type 2 diabetes. Diabetes Obes Metab. 2011;13:348–56.
Macconell L, Pencek R, Li Y, Maggs D, Porter L. Exenatide once weekly: sustained improvement in glycemic control and cardiometabolic measures through 3 years. Diabetes Metab Syndr Obes. 2013;6:31–41.
Bunck MC, Corner A, Eiasson B, et al. Effects of exenatide on measures of beta-cell function after 3years in metformin-treated patients with type 2 diabetes. Diabetes Care. 2011;34:2041–7.
van Bloemendaal L, Ten Kulve JS, la Fleur SE, Ijzerman RG, Diamant M. Effects of GLP-1 on appetite and body weight: focus on the central nervous system. J Endocrinol. 2013 (Dec 9. [Epub ahead of print]).
Butler AE, Campbell-Thompson M, Gurlo T, Dawson DW, Atkinson M, Butler PC. Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes. 2013;62:2595–604.
Kral JG. Vagal nerve function in obesity: therapeutic implications. World J Surg. 2009;33:1995–2006.
Hoyda TD, Smoth PM, Ferguson AV. Gastrointestinal hormone actions in the central regulation of energy metabolism: potential sensory roles for the circumventricular organs. Int J Obes. 2009;33:S16–21.
Thorens B, Larsen P. Gut-derived signaling molecules and vagal afferents in the control of glucose and energy homeostasis. Curr Opin Clin Nutr Metab Care. 2004;7:471–8.
Acknowledgments
The authors acknowledge the support of the Mayo Clinic General Clinical Research Center (DK TR000135). Dr. Vella is supported by DK78646 and by DK82396.
Conflict of interest
Dr. Vella has received research grants from Merck and Daiichi-Sankyo. He is an investigator in multicenter studies sponsored by Novartis and GI dynamics, respectively. He has consulted for XOMA, Sanofi-Aventis, Novartis and Bristol-Myers Squibb. Dr. Shah has no relevant disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, M., Vella, A. Effects of GLP-1 on appetite and weight. Rev Endocr Metab Disord 15, 181–187 (2014). https://doi.org/10.1007/s11154-014-9289-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-014-9289-5