Abstract
Purpose
To describe the prevalence, severity, and risk factors of chemotherapy-induced peripheral neuropathy (CIPN) and its impact on function and quality of life (QOL) among women treated for breast cancer in a large U.S. Community Oncology practice.
Methods
Women previously treated with taxane-based chemotherapy for early-stage breast cancer completed the EORTC QLQ–C30, QLQ–BR23, and QLQ–CIPN20. Subscales are scored 0–100; higher scores indicate greater symptom severity. Pre-specified hypotheses were tested.
Results
126 women with mean age 56.7 years (SD 11.8) were stage I–II (79.4%) or stage III (20.6%) at the time of the survey; 65.1% were White and 27.8% were Black or African American. The mean time since last taxane chemotherapy cycle was 144.9 weeks (SD 112.9). 73.0% reported having CIPN. QLQ–CIPN20 mean scores for the sensory, motor, and autonomic subscales were 18.9 (SD 23.1), 18.6 (SD 18.7), and 17.1 (SD 21.8), respectively. CIPN symptom severity was negatively correlated with global health status/QOL and physical and role functioning (range of r = −0.46 to −0.72). It was not associated with age, body mass index, diabetes, or cumulative taxane dosage, but was greater for Black or African American women (e.g., sensory, p < 0.002). CIPN sensory impairment was marginally greater for patients treated with paclitaxel compared to docetaxel (p < 0.064).
Conclusions
CIPN was prevalent in this community oncology practice and significantly impacts function and QOL. These data highlight the importance of developing methods to mitigate CIPN, and for screening for CIPN particularly among Black or African American women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With advances in cancer diagnosis and treatment there are now an estimated 2.8 million breast cancer survivors in the United States [1]. As a result, greater awareness has been placed on the long-term adverse effects and the impact on quality of life (QOL) of cancer treatment [2]. One such impact is chemotherapy-induced peripheral neuropathy (CIPN), characterized as damage to sensory and motor nerves, which can cause persistent symptoms and limitations in functioning, including numbness, tingling, or pain in the fingers or toes and loss of deep tendon reflexes [3,4,5,6,7]. CIPN is a common side effect of neurotoxic chemotherapy agents, including taxanes (paclitaxel and docetaxel) [8,9,10,11], and significantly affects the QOL of impacted patients [10, 11].
Taxane-induced CIPN is commonly reported in clinical trials and has been observed in 15–60% of patients [10, 12,13,14]. However, the comparison of incidence rates across studies is limited by the use of different grading scales and symptom assessment tools [9, 15, 16]. Further, because the use of patient-reported outcome measures and/or objective assessments result in a higher severity of CIPN as compared to clinician examination, it is thought that CIPN is typically underreported [9, 17,18,19].
Little is known about the incidence, prevalence, and risk factors of CIPN in clinical practice [20], and few studies have examined the impact of CIPN on QOL [11, 21]. Studies of CIPN and QOL among patients with cancer have differed significantly in their assessment methods and study design, including the patient population, chemotherapeutic agent, and number of patients [11]. Thus, additional studies, which include a large number of patients and use validated questionnaires, are needed to elucidate the association of CIPN and QOL and describe risk factors for CIPN.
The objective of this study was to describe the prevalence and pattern of taxane-based CIPN in breast cancer patients receiving care in a large community oncology practice, to identify the effects of CIPN on QOL, and to identify risk factors of CIPN. This study was designed to address gaps in the literature, specifically to assess a large and racially diverse sample of patients receiving care in a community oncology practice, using validated patient-reported outcome instruments of both CIPN and QOL in addition to data abstracted from the medical record regarding treatment and referrals, and to assess patients who range in the number of years past the end of chemotherapy. Based on prior research and clinical experience, we hypothesized CIPN is prevalent among women treated for breast cancer in a community oncology practice [2, 20], CIPN is underreported and under assessed by physicians in clinical practice [9, 17,18,19], and referral and visitation to a neurologist or pain specialist is infrequent [22]. We hypothesized CIPN is likely to have a negative impact on the QOL of affected patients, in particular global health status, physical functioning, and role functioning [11, 21, 23]. Further, we hypothesized CIPN is more likely to be more severe in patients who are older [21], have higher BMI [21], have diabetes [2], are Black or African American [24], have higher stages of breast cancer, are receiving paclitaxel compared to docetaxel [10, 20, 25], are receiving higher cumulative dosage of taxanes [2, 4, 9], have received their last taxane chemotherapy treatment in the last two years [2, 21], and have received a modification in their chemotherapy regimen, such as a dose delay, dose reduction, or treatment discontinuation [20].
Patients and methods
Study design
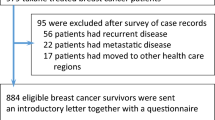
This cross-sectional, observational study employed patient surveys and medical chart review to characterize the prevalence and pattern of CIPN and its impact on QOL among women treated for breast cancer at a community oncology practice. All female patients aged 18–95, with early-stage breast cancer, who had previously received taxane-based chemotherapy, including paclitaxel or docetaxel, and who were a patient at Virginia Oncology Associates, were eligible for inclusion in the study. Patients were recruited at two offices of Virginia Oncology Associates during their scheduled, general follow up appointments, during August 2014. Informed consent was obtained from all patients before inclusion in the study. The study was approved by the Eastern Virginia Medical School Institutional Review Board in Norfolk, Virginia.
Patient demographic and clinical characteristics
Patient demographic and clinical information was abstracted from the participants’ medical records, including age, height, weight, BMI, stage of breast cancer, type of treatment (drug, dosage, and frequency), dose delays, reductions, or discontinuations, other medical conditions or agents known to cause peripheral neuropathy (diabetes, rheumatoid arthritis, multiple sclerosis, etc.), and any treatments or therapies for CIPN. Information about race, ethnicity, experience of CIPN symptoms (yes/no), time of onset of CIPN symptoms, perceived change in CIPN symptoms over time, physician evaluation of CIPN, and referral and visitation to a neurologist or pain specialist was obtained via the questionnaire.
QOL measurements
The European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaires C30 (QLQ–C30) was used to assess health-related QOL [26]. It contains multi- and single-item sub-scales, including five functional scales (physical, role, cognitive, emotional, and social), three symptom scales (fatigue, pain, and nausea and vomiting), a global health status/QOL scale, and six single-item scales (dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties). The EORTC QLQ–BR23 was used to assess breast cancer-related QOL [27]. It contains multi- and single-items sub-scales, including four functional scales (body image, sexual functioning, sexual enjoyment, and future perspective) and four symptom scales and items (systemic therapy side effects, breast symptoms, arm symptoms, and upset by hair loss). Items in both questionnaires have a 7 day recall period, and item responses range from 1 (not at all) to 4 (very much), except for the global health status/QOL items, which range from 1 (very poor) to 7 (excellent). Each sub-scale is scored on a 0–100 scale, where higher scores on the functional scales, global health status/QOL scale, and symptom scales represent a higher level of functioning, better QOL, and more severe symptoms, respectively [28].
CIPN measurements
The EORTC QLQ–CIPN20 was used to assess CIPN [29]. It contains multi- and single-items sub-scales, assessing sensory, motor, and autonomic symptoms and problems, and a single item addressing ability to drive a car. Items have a 7 day recall period, and item responses range from 1 (not at all) to 4 (very much). Each sub-scale is scored on a 0–100 scale, where higher scores indicate more severe symptoms or impairment. A limitation of the EORTC QLQ–CIPN20 is that a cut-point indicating the presence or absence of CIPN is not yet established. Therefore, while the EORTC QLQ–CIPN20 was used to characterize the severity and impact of CIPN, the presence or absence of CIPN was determined by patient-self report via a yes/no survey question; exploratory analyses indicated that responses to this survey item were consistent with much greater severity of scores on the CIPN20 and subsequent survey items about treatment and referrals for CIPN.
Statistical analyses
Pre-specified hypotheses were tested using appropriate bivariate statistical tests, including independent sample t tests, Chi-square tests, Pearson’s correlation, and linear regression. The EORTC subscale scores are continuous, and although the scores were not normally distributed, parametric tests are appropriate [30]. The minimally important differences (MID) for QOL scores were calculated as described by Norman et al., in which a difference of at least one half a standard deviation can be interpreted as a clinically important between-group difference [31]. All statistical tests were considered significant if p < 0.05. Analyses were conducted using Stata, version 13 (Stata Corp., Plano, TX).
Results
Patient demographic and clinical characteristics
One hundred and twenty-six female, breast cancer patients enrolled in the study had a mean age 56.7 years (standard deviation (SD) 11.8) and were stage I–II (79.4%) or stage III (20.6%) at the time of the survey (Table 1). Eighty-two (65.1%) patients were White, and 35 (27.8%) patients were Black or African American. Fifty-eight (46.0%) patients received paclitaxel, while 72 (57.1%) received docetaxel with mean weeks since last taxane chemotherapy (first date of the last cycle) 144.9 weeks (SD 112.9). Furthermore, 34 (27.0%) patients reported a modification of chemotherapy regimens such as a dose delay, dose reduction, or treatment discontinuation.
Twenty-five (19.8%) patients had diabetes (Table 1). Among other disorders potentially including symptoms of peripheral neuropathy, 13 (10.3%) patients had rheumatoid arthritis. Nine (7.1%) patients received metformin, an agent reported to cause peripheral neuropathy [32]. Due to these small percentages, sub-group analysis of patients with rheumatoid arthritis and of patients who received metformin were not conducted.
Prevalence and pattern of CIPN
Ninety-two (73.0%) women reported having CIPN, among whom 44 (47.8%) had received paclitaxel, 45 (48.9%) had received docetaxel, and 3 (3.3%) had received paclitaxel and docetaxel (Table 2), and the mean number of weeks since last taxane chemotherapy was 131.4 (SD 98.6) (n = 91; one patient as outlier [>364 weeks]) (Table 1). Fifty (54.0%) women reported having CIPN evaluated by a physician, 14/92 (15.2%) were referred to a neurologist, and 11/92 (12.0%) visited a neurologist (Table 2). QLQ–CIPN20 mean scores for the sensory, motor, and autonomic subscales were 18.9 (SD 23.1), 18.6 (SD 18.7), and 17.1 (SD 21.8), respectively (Table 3). The between-group minimally important difference in QLQ–CIPN20 subscale scores, estimated as one half the standard deviation of the sample mean score, would therefore be approximately 10 points. Forty-six (36.5%) patients reported that symptoms had improved, 16 (12.7%) patients reported that symptoms were the same, and 16 (12.7%) patients reported that symptoms had gotten worse, since the time of symptom onset (Table 2).
Among women with CIPN (n = 92), the average time to the first occurrence of CIPN was 3.8 weeks (SD 3.0) (n = 72; 20 patients reported time to first occurrence unknown). The average cumulative taxane dosage threshold for occurrence of CIPN was 301.0 mg/m2 (SD 175.4) (n = 70; for two patients an accurate taxane dosage could not be determined).
Health-related quality of life and functioning
The mean score of EORTC QLQ–C30 global health status/QOL was 77.0 (SD 20.3), physical function was 85.7 (SD 17.1), role functioning was 86.5 (SD 22.7), and pain was 22.9 (SD 26.8). The mean scores of QLQ–BR23 subscales measuring systemic therapy side effects and arm symptoms were 25.7 (SD 21.4) and 22.0 (SD 24.9), respectively. All subscales scores are reported in Table 3.
Correlates of CIPN
Independent sample t tests indicated those who reported having symptoms of CIPN had significantly higher EORTC QLQ–CIPN20 mean scores for the sensory scale (24.6 vs. 3.5, p < 0.001), motor scale (22.9 vs. 7.0, p < 0.001), and autonomic scale (20.3 vs. 8.3, p < 0.006). Further, referral to a neurologist for CIPN, visiting a neurologist for CIPN, and patient-reported symptoms of CIPN were significantly associated (p < 0.05; per Chi-square tests) with patient-reported CIPN status. The mean CIPN20 sensory and motor subscale scores were higher for patients referred to a neurologist for CIPN (sensory: 43.9 vs. 21.2, p < 0.001; motor: 43.2 vs. 19.2, p < 0.001) and for patients who visited a neurologist for CIPN (sensory: 41.4 vs. 22.4, p < 0.014; motor: 43.7 vs. 20.0, p < 0.001), per independent sample t tests (Table 4).
Bivariate linear regression models indicated that the average decline in CIPN20 sensory scale scores by years since treatment was −3.1 per year (p < 0.005), and for the motor scale was −2.1 per year (p < 0.022), indicating scores were higher (worse) for women who completed treatment more recently.
CIPN motor impairment was marginally greater for patients with higher stages of breast cancer, specifically, stage III versus stages I and II (group means by stage: 13.7 vs. 18.7 vs. 22.9; bivariate linear regression beta coefficient = 4.6, p < 0.083). CIPN sensory impairment was marginally greater for patients treated with paclitaxel compared to docetaxel (23.3 vs. 15.6, independent samples t test p < 0.064), and patient-reported CIPN (yes/no) was marginally more common in patients receiving paclitaxel only than docetaxel only (81.5 vs. 66.1%) (χ 2 = 3.57, p < 0.059).
CIPN sensory, motor, and autonomic impairment was greater for Black or African American patients versus White patients (sensory: 28.6 vs. 14.4, p < 0.002; motor: 25.0 vs. 15.6, p < 0.012; autonomic: 24.3 vs. 13.4, p < 0.014; per independent sample t tests) (Fig. 1), as was patient-reported CIPN (yes/no) (82.9 vs. 67.1%). Post hoc analyses indicated these clinically meaningful differences in symptom severity by race persisted when the analysis was limited to patients who reported having CIPN (n = 84) (sensory: 33.6 vs. 20.1, p < 0.014; motor: 29.7 vs. 19.5, p < 0.019; autonomic: 27.6 vs. 16.7, p < 0.042). Further, we included covariates in linear regression models of race onto CIPN symptom severity. The models indicated that the differences in CIPN symptom severity by race were not modified when controlling for clinical and treatment characteristics, including age, diabetes, BMI, stage, time since last treatment, taxane type, cumulative taxane dosage, or presence of dose modification in linear regression models (one covariate per model; covariates were non-significant and did not impact the effect of race). The impact of time since last treatment persisted independent of race (sensory scale: difference by race beta coefficient = 13.4, p < 0.003, and difference per year beta coefficient = −3.25, p < 0.003).
These observed statistically significant differences, described above, were also large enough to be clinically significant, i.e., were greater than 10. No associations were found between EORTC QLQ–CIPN20 subscales and age, BMI, diabetes, cumulative taxane dosage, paclitaxel treatment course, type of taxane therapy, and modifications in chemotherapy regimen, and no associations were found between patient-reported CIPN status and cumulative taxane dosage or modification of chemotherapy regimen.
Association between CIPN and QOL
It was hypothesized that CIPN symptom severity has a negative influence on the QOL of affected patients, in particular global health status, and physical and role functioning. The EORTC QLQ–C30 global health status/QOL subscale, physical functioning subscale, and role functioning subscales, each had moderate to strongly negative associations with the CIPN20 sensory, motor, and autonomic subscales (range of Pearson correlation coefficients: r = −0.46 to r = −0.72).
Discussion
This study assessed patient-reported CIPN and QOL using validated instruments, in a racially diverse sample of patients receiving care at a community oncology practice, many of whom were at least several years past the end of chemotherapy. Many of the findings of this study are consistent with the results of prior research, although comparison across studies of CIPN is limited by differences in study population, treatment regimens, and assessment tools [3, 7, 10, 11, 16]. A large study of Danish women receiving docetaxel and other agents for early-stage breast cancer (N = 1725) found 34% had CIPN of grade 2–4 [33]. In this study sample, 73.1% of women self-reported symptoms of CIPN, specifically 81.5% of women treated with paclitaxel only and 66.1% of women treated with docetaxel only. These estimates are higher than the Danish study in part because they include CIPN of the severity that would be classified as grade 1. In addition, this study found patient-reported CIPN status was significantly associated with taxane type, providing further evidence that the neurotoxicity of paclitaxel is greater than docetaxel.
Among women reporting CIPN, only about half (54.0%) recalled having an evaluation by a physician; however, self-reports of clinical care can be of limited reliability. A small percentage (15.2%) of women who reported CIPN were referred to a neurologist, and the severity of symptoms indicated by the EORTC QLQ–CIPN20 was substantially higher than those who were not referred. In addition, Alberti et al. addressed the perception and assessment of CIPN between healthcare providers and patients [34]. They compared three clinical assessments to the EORTC QLQ–CIPN20. They found that differences between clinical assessments and patients’ perceptions’ most likely occurred among those with intermediate levels of CIPN severity. Therefore, they provide further evidence for a more comprehensive assessment of CIPN using both clinical and patient-reported outcomes measures.
CIPN symptom severity was negatively correlated with global health status/QOL and physical and role functioning (range of r = −0.46 to −0.72) as measured by the EORTC QLQ–C30. A review by Mols et al. of studies examining the association of CIPN with QOL found that in 8 of 11 studies CIPN was associated with a lower QOL, although the studies differed in their assessment methods and patient populations (diagnoses, treatments, and time since diagnosis) [11]. To the best of our knowledge, only one previous study has examined the relationship between CIPN and QOL in women with breast cancer using the EORTC QLQ–C30, QLQ–BR23, and QLQ–CIPN20; in a sample of 82 Korean women, Kim et al. found significant moderate correlations between CIPN and QOL (range r = −0.37 to 0.65) [23].
In a review of multiple studies, Hausheer et al. found patients experienced more severe symptoms with cumulative docetaxel doses over 400 mg/m2 [9]. Further, a large randomized trial comparing docetaxel and paclitaxel for treatment of metastatic breast cancer identified the mean cumulative dose to onset of clinically graded CIPN as 371 mg/m2 for docetaxel and 715 mg/m2 for paclitaxel [35]. In this study, cumulative taxane dosage was not associated with CIPN symptom severity, however the relationship may have been attenuated by gradual decrease in symptom severity in the time since the end of treatment.
Mild symptoms of CIPN are known to improve or resolve within several months after the discontinuation of chemotherapy; however, symptoms may persist longer in patients who develop more severe neuropathy [6, 36, 37]. In this study, the time since last taxane chemotherapy was associated with lower symptom severity, and 46 (50.5%) reported symptoms had improved.
Taxane-induced CIPN has been found to result in sensory nerve dysfunction more often than motor dysfunction [6, 7, 9, 22]. In this study, there was no significant difference in the mean scores of the sensory and motor subscales.
CIPN was more prevalent and symptom severity was greater in women who self-identified as Black or African American compared to White women, and these differences were not explained by the array of clinical or treatment characteristics measured in this study. A genome-wide association study reported by Schneider et al. found that a genetic variant (rs3125923) which may impact neuronal development and “genetically determined African-American race” via principal component analysis were significant predictors of taxane-induced peripheral neuropathy [24].
Limitations of this study include that rates of CIPN evaluation and referral reflect rates from a single medical oncology practice with two sites. While the study aimed to enroll all eligible patients who were receiving care during a 1 month period, the sample is limited to patients who were willing and able to participate in a survey study. Although only a small percentage of patients reported other disorders potentially including symptoms of peripheral neuropathy, the relationship between taxane treatment and EORTC QLQ–CIPN20 scores may have been confounded by these factors. In addition, because the number of Black or African American women in the study (n = 35) was not larger, the exploratory analyses to identify potential confounders of the relationship between race and CIPN was likely underpowered. Further, although the study highlights the prevalence of CIPN and its impact on QOL, it is potentially limited by the lack of clinician assessment of CIPN conducted at the same time as the patient-reported outcomes assessment.
Patient reports of CIPN (yes/no) were highly consistent with the symptom severity captured by the QLQ–CIPN20 (e.g., sensory scale: 24.6 vs. 3.5, p < 0.001). However, identifying cut-points for the categorization of symptom severity as none/negligible, mild, moderate, and severe, would greatly assist the interpretation of findings in future research. Hausheer et al. discuss the substantial limitations of quantitative sensory testing, electrophysiologic measurement, and clinician grading scales as reliable and responsive measurement tools, and assert that patient-based questionnaires are highly suitable for identifying CIPN in the clinical context [9].
This study had several key strengths. Patient-reported QOL and CIPN were assessed using validated instruments, and the analyses evaluated a priori hypotheses based on scientific literature and clinical experience. The patient population was 27.8% Black or African American, which allowed us to examine racial differences in CIPN. The patient population also included a mean of 131.4 (SD 98.6) weeks since last taxane chemotherapy treatment, providing a unique opportunity to evaluate CIPN by time since treatment of up to seven years. This study was also able to examine the association of chemotherapy dosage and number of cycles received with CIPN.
The importance of addressing CIPN has increased with the rise in the number of breast cancer survivors, because it is a persistent condition that is associated with QOL. Further investigations of the risk factors of CIPN, including regimen, dose, schedule of the neurotoxic chemotherapy, genetic markers, medical conditions and medications, are needed to better predict the incidence and severity of this chronic treatment toxicity.
Conclusion
CIPN was prevalent in this community oncology practice patient population even among patients who were many years post-treatment and it was associated with impaired function and quality of life. These data provide further evidence for the risk factors of CIPN, including taxane type and cumulative taxane dosage, and for those most at risk of CIPN, in particular Black or African American women. These findings highlight the need for increased screening and the importance of developing therapies for the mitigation of CIPN, in order to enhance the long-term function and QOL of patients with breast cancer.
References
American Cancer Society. (2014). What are the key statistics about breast cancer? Learn about cancer. Retrieved October 12, 2014 from http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics.
Park, S. B., Goldstein, D., Krishnan, A. V., Lin, C., Friedlander, M. L., Cassidy, J., et al. (2013). Chemotherapy-induced peripheral neurotoxicity: A critical analysis. CA: A Cancer Journal for Clinicians, 63(6), 419–436.
Bakitas, M. A. (2007). Background noise: The experience of chemotherapy-induced peripheral neuropathy. Nursing Research, 56(5), 323–331.
Forsyth, P., Balmaceda, C., Peterson, K., Seidman, A. D., Brasher, P., & DeAngelis, L. M. (1997). Prospective study of paclitaxel-induced peripheral neuropathy with quantitative sensory testing. Journal of Neuro-oncology, 35, 47–53.
Hilkens, P. H., & van den Bent, M. J. (1997). Chemotherapy-induced peripheral neuropathy. Journal of the Peripheral Nervous System, 2, 350–361.
Rowinsky, E. K., Chaudry, V., Cornblath, D. R., & Donehower, R. C. (1993). Neurotoxicity of taxol. Journal of the National Cancer Institute, 15, 107–115.
Lipton, R. B., Apfel, S. C., Dutcher, J. P., Rosenberg, R., Kaplan, J., Berger, A., et al. (1989). Taxol produces a predominantly sensory neuropathy. Neurology, 39, 368–373.
Paice, J. A. (2009). Clinical challenges: Chemotherapy-induced peripheral neuropathy. Seminars in Oncology Nursing, 25, S8–S19.
Hausheer, F. H., Schilsky, R. L., Bain, S., Berghorn, E. J., & Lieberman, F. (2006). Diagnosis, management, and evaluation of chemotherapy-induced peripheral neuropathy. Seminars in Oncology, 33(1), 15–49.
Argyriou, A. A., Kyritsis, A. P., Makatsoris, T., & Kalofonos, H. P. (2014). Chemotherapy-induced peripheral neuropathy in adults: A comprehensive update of the literature. Cancer Management and Research, 6, 135–147.
Mols, F., Beijers, T., Vreugdenhil, G., & van de Poll-Franse, L. (2014). Chemotherapy-induced peripheral neuropathy and its association with quality of life: A systematic review. Supportive Care in Cancer, 22(8), 2261–2269.
Hilkins, P. H., Verweij, J., Stoter, G., Vecht, C. J., van Putten, W. L., & van den Bent, M. J. (1996). Peripheral neurotoxicity induced by docetaxel. Neurology, 46, 104–108.
Taxol [package insert]. (2003). Princeton, NJ: Bristol-Myers Squibb.
Wampler, M. A., Miaskowski, C., Hamel, K., Byl, N., Rugo, H., & Topp, K. S. (2006). The modified total neuropathy score: A clinically feasible and valid measure of taxane-induced peripheral neuropathy in women with breast cancer. The Journal of Supportive Oncology, 4(8), W9–W16.
Postma, T. J., Heimans, J. J., Muller, M. J., Ossenkoppele, G. J., Vermorken, J. B., & Aaronson, N. K. (1998). Pitfalls in grading severity of chemotherapy-induced peripheral neuropathy. Annals of Oncology, 9, 739–744.
Cavaletti, G., Frigeni, B., Lanzani, F., Mattavelli, L., Susani, E., Alberti, P., et al. (2010). Chemotherapy-induced peripheral neurotoxicity assessment: A critical revision of the currently available tools. European Journal of Cancer, 46, 479–494.
Shimozuma, K., Ohashi, Y., Takeuchi, A., Aranishi, T., Morita, S., Kuroi, K., et al. (2009). Feasibility and validity of the Patient Neurotoxicity Questionnaire during taxane chemotherapy in a phase III randomized trial in patients with breast cancer: N-SAS BC 02. Supportive Care in Cancer, 17, 1483–1491.
Kuroi, K., Shimozuma, K., Ohashi, Y., Takeuchi, A., Aranishi, T., Morita, S., et al. (2008). A questionnaire survey of physicians’ perspectives regarding the assessment of chemotherapy-induced peripheral neuropathy in patients with breast cancer. Japanese Journal of Clinical Oncology, 38, 748–754.
Basch, E., Iasonos, A., McDonough, T., Barz, A., Culkin, A., & Kris, M. G. (2006). Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: Results of a questionnaire-based study. The Lancet Oncology, 7(11), 903–909.
Speck, R. M., Sammel, M. D., Farrar, J. T., Hennessy, S., Mao, J. J., Stineman, M. G., et al. (2013). Impact of chemotherapy-induced peripheral neuropathy on treatment delivery in nonmetastatic breast cancer. Journal of Oncology Practice, 9(5), e234–e240.
Mols, F., Beijers, T., Lemmens, V., van den Hurk, C. J., Vreugdenhil, G., & van de Poll-Franse, L. V. (2013). Chemotherapy-induced neuropathy and its association with quality of like among 2- to 11-year colorectal cancer survivors: Results from the population-based PROFILES registry. Journal of Clinical Oncology, 31(21), 2699–2707.
Stubblefield, M. D., Burstein, H. J., Burton, A. W., Custodio, C. M., Deng, G. E., Ho, M., et al. (2009). NCCN task force report: Management of neuropathy in cancer. Journal of the National Comprehensive Cancer Network, 7(suppl 5), S-1–S-26.
Kim, H. Y., Kang, J. H., Song, C. E., & Youn, H. J. (2013). Chemotherapy-induced peripheral neuropathy and quality of life in breast cancer patients. Asian Oncology Nursing, 13(4), 222–230.
Schneider, B. P., Li, L., Radovich, M., Shen, F., Miller, K. D., Flockhart, D. A., et al. (2015). Genome-wide association studies for taxane-induced peripheral neuropathy in ECOG-5103 and ECOG-1199. Clinical Cancer Research, 21(22), 5082–5091.
Candelario, N., Wongrakpanich, S., & Morginstin, M. S. (2015). Predictors of chemotherapy-induced peripheral neuropathy among breast cancer patients treated with taxanes. Journal of Clinical Oncology, 33(suppl 28S), 90.
Aaronson, N. K., Ahmadzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85, 365–376.
Sprangers, M. A., Groenvold, M., Arraras, J. I., Franklin, J., te Velde, A., Muller, M., et al. (1996). The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. Journal of Clinical Oncology, 14(10), 2756–2768.
Fayers, P. M., Aaronson, N. K., Bjordal, K., Groenvold, M., Curran, D., & Bottomley, A. (2001). The EORTC QLQ-C30 Scoring Manual (3rd ed.). Brussles: European Organisation for Research and Treatment of Cancer.
Postma, T. J., Aaronson, N. K., Heimans, J. J., Muller, M. J., Hildebrand, J. G., Delattre, J. Y., et al. (2005). The development of an EORTC quality of life questionnaire to assess chemotherapy-induced peripheral neuropathy: The QLQ-CIPN20. European Journal of Cancer, 41(8), 1135–1139.
Lumley, T., Diehr, P., Emerson, S., & Chen, L. (2002). The importance of the normality assumption in large public health data sets. Annual Review of Public Health, 23, 151–169.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41(5), 582–592.
Bell, D. S. (2010). Metformin-induced vitamin B12 deficiency presenting as a peripheral neuropathy. Southern Medical Journal, 103(3), 265–267.
Eckhoff, L., Knoop, A. S., Jensen, M. B., Ejlertsen, B., & Ewertz, M. (2013). Risk of docetaxel-induced peripheral neuropathy among 1,725 Danish patients with early stage breast cancer. Breast Cancer Research and Treatment, 142(1), 109–118.
Alberti, P., Rossi, E., Cornblath, D. R., Merkies, I. S., Postma, T. J., Frigeni, B., et al. (2014). Physician-assessed and patient-reported outcome measures in chemotherapy-induced sensory peripheral neurotoxicity: Two sides of the same coin. Annals of Oncology, 25(1), 257–264.
Jones, S. E., Erban, J., Overmoyer, B., Budd, G. T., Hutchins, L., Lower, E., et al. (2005). Randomized phase III study of docetaxel compared with paclitaxel in metastatic breast cancer. Journal of Clinical Oncology, 22, 5542–5551.
Argyriou, A. A., Polychronopoulos, P., Iconomou, G., Koutras, A., Kalofonos, H. P., & Chroni, E. (2005). Paclitaxel plus carboplatin-induced peripheral neuropathy. A prospective clinical and electrophysiological study in patients suffering from solid malignancies. Journal of Neurology, 252(12), 1459–1464.
Hershman, D. L., Weimer, L. H., Wang, A., Kranwinkel, G., Brafman, L., Fuentes, D., et al. (2011). Association between patient reported outcomes and quantitative sensory tests for measuring long-term neurotoxicity in breast cancer survivors treated with adjuvant paclitaxel chemotherapy. Breast Cancer Research and Treatment, 125(3), 767–774.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Statement of Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Simon, N.B., Danso, M.A., Alberico, T.A. et al. The prevalence and pattern of chemotherapy-induced peripheral neuropathy among women with breast cancer receiving care in a large community oncology practice. Qual Life Res 26, 2763–2772 (2017). https://doi.org/10.1007/s11136-017-1635-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1635-0