Abstract
Purpose
Peripheral neuropathy (PN) is a common and distressing complication from chemotherapy. Symptoms often, but not always, improve with time. The prevalence of long-term PN symptoms in breast cancer survivors is not well known. We sought to explore PN symptoms and associated risk factors among breast cancer survivors at least 2 years out from diagnosis.
Methods
We performed a cross-sectional retrospective study investigating the prevalence of patient-reported numbness, tingling, and anesthesia symptoms as a surrogate for PN in breast cancer survivors. We included patients with stage 0–III breast cancer who completed a clinical questionnaire at a survivorship visit that occurred 2 or more years after diagnosis. We estimated the prevalence of PN and identified risk factors for PN.
Results
Six hundred and five patients assessed between April 2009 and October 2016 met eligibility for analysis. Median age was 60 years. Median number of years from diagnosis to assessment was 6.3. All patients had surgery and 62% had chemotherapy. Twenty-seven percent reported PN. On univariable analysis, obesity, stage II and III, mastectomy, PN before diagnosis, and receipt of taxane chemotherapy were associated with higher risk of PN (all p < 0.05); older age, exercise, ER-positive disease, and endocrine therapy were associated with lower risk of PN (all p < 0.05). On multivariable analysis, only receipt of docetaxel (OR 2.18, CI 1.22–3.88) or paclitaxel (OR 4.07, CI 2.54–6.50) and reporting PN symptoms before diagnosis (OR 3.28, CI 1.49–7.21) were associated with higher risk of PN. Overall, 17, 20, 31, and 44% reported long-term PN symptoms after no chemotherapy, non-taxane chemotherapy, docetaxel chemotherapy, and paclitaxel chemotherapy, respectively.
Conclusion
Long-term peripheral neuropathy symptoms are reported by a significant minority of breast cancer survivors, particularly following paclitaxel or docetaxel chemotherapy. These study findings can help inform patients and clinicians regarding long-term PN risk following chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy induced peripheral neuropathy (PN) is a common complication in cancer patients with an estimated overall prevalence of 38% [1, 2]. Diagnosing peripheral neuropathy (PN) is challenging; it depends on history, physical examination, and nerve conduction studies as needed with highest accuracy when all are abnormal [3]. Because of the variability in presentation and severity of PN and because defining PN depends on restrictive criteria, the exact prevalence in population is hard to determine. There is significant discrepancy in the literature regarding incidence, severity, and course of chemotherapy induced PN [4].
Patients with early stage breast cancer are commonly exposed to taxanes which have been strongly associated with PN. [4]. Chemotherapy induced PN is an important dose-limiting side effect of taxanes and can start within days and persist for years following treatment [5]. It is mainly sensory neuropathy and presents with paresthesia and pain [5]. The occurrence of PN can be detrimental for quality of life in cancer survivors [6]; it is associated with excess healthcare costs, excess resource utilization, and work loss burden [7]. The prevalence of PN is variable based on time of assessment and the patient population and ranges from 14 to 80% [8,9,10]. In our previous cohort study, numbness/tingling was the second most common complaint in breast cancer survivors at time of survivorship visit (SV) and was reported by 34% of patients [11]. Patients generally accept acute toxicities of curative intent chemotherapy because many of these effects resolve with in the first few years; however, few studies have investigated the long-term prevalence of PN symptoms and their associated burden among breast cancer survivors [12]. In this study, we sought to estimate PN prevalence and identify risk factors for PN in breast cancer survivors at least 2 years out from diagnosis.
Methods
Patients, survivorship care visit and questionnaire
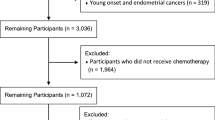
We performed an IRB-approved cross-sectional study of patients who attended a breast cancer survivorship clinic at The Cleveland Clinic. As previously described [11], patient information was extracted from a clinical questionnaire, care plan, and the treatment summary from each participant’s initial visit to the survivorship clinic. Medical records were reviewed. Breast cancer survivors’ data are collected and managed in a database using REDCap™ electronic data capture tools hosted at Cleveland Clinic [13]. All treatment summaries were prepared by a Certified Nurse Practitioner (CNP) at our center and included patient demographic data as well as details of the cancer diagnosis and treatment. Data were available on 1297 patients with stage 0–III breast cancer who had received local therapy with or without systemic therapy and were disease free at the time of their initial SV conducted between March 2009 and December 2016. Patients had their initial SV at various time periods following initial treatment as many patients received initial treatment before it became routine to provide a SV at the time of initial treatment completion. Only patients who were seen 2 or more years out from diagnosis were included in the analysis.
Patients were referred for a SV per the clinical practice of their oncologist. Initial treatment was defined as definitive surgery and any chemotherapy and/or radiotherapy. Patients might be on long-term hormonal therapy or targeted therapy at time of the SV.
At the SV, patients completed a questionnaire addressing current state of health, ongoing health issues, and health habits. Patients were asked about past and current symptoms including numbness, tingling, and loss of sensation. The questionnaire was built mainly for clinical assessment and follow-up. The CNP provided guidance in filling out the questionnaire as needed. The SVs were conducted using ASCO guidelines for SV [14]. The treatment summary and survivorship care plan were documented using a modified Journey Forward template [15] and copies were provided to the patient and appropriate members of the medical team.
From 1297 potential patients, 692 were excluded; 689 whose SV was less than 2 years after diagnosis and 3 whose specific treatment regimen could not be determined. Analysis is based on the remaining 605 patients who were diagnosed between January 1991 and September 2014 with SV between April 2009 and October 2016.
Statistical analysis
Continuous variables were summarized as the mean, standard deviation, median, and range and categorical variables were summarized as frequency counts and percentages. Logistic regression analysis was used to identify univariable risk factors for PN. Stepwise logistic regression analysis with a variable entry criterion of p ≤ 0.10 and a variable retention criterion of p ≤ 0.05 was used to identify multivariable risk factors. The multivariable model was confirmed with bootstrap analysis. Logistic regression results are summarized as the odds ratio (OR) and 95% confidence interval (CI). The multivariable model was used to calculate the probability of PN for combinations of variables in the model. Analyses were done using SAS Software (SAS Institute, Inc., Cary, NC, USA). All tests were two-sided, and p ≤ 0.05 was used to indicate statistical significance.
Variables assessed as potential risk factors included years from diagnosis to SV, age; BMI (<18.5 underweight and 18.5–24.9 normal weight vs. 25–25.9 overweight vs. ≥30 obese), breast cancer side, estrogen receptor status, progesterone receptor status, stage, type of surgery, type of chemotherapy received (none, non-taxane, docetaxel, or paclitaxel) radiotherapy, endocrine therapy, exercise (none, yes/started after cancer diagnosis, yes/started before cancer diagnosis), smoking history (current, former, never), alcohol consumption (yes vs. no, and 0 vs. 1–3 vs. >3 drinks/week), diabetes mellitus, and thyroid disease. Chemotherapy regimens were classified as: paclitaxel-containing regimens: doxorubicin and cyclophosphamide (AC) followed by paclitaxel (q3, q2, or weekly paclitaxel), AC followed by taxane/trastuzumab, paclitaxel/trastuzumab; docetaxel-containing regimens: AC followed by docetaxel, a combination of docetaxel and cyclophosphamide (TC), a combination of docetaxel carboplatin and trastuzumab (TCH), TC + trastuzumab, TCH+pertuzumab, or a combination of docetaxel, doxorubicin and cyclophosphamide (TAC) and non-taxane regimens: AC, a combination of cyclophosphamide, methotrexate, and 5-fluororuacil (CMF), a combination of methotrexate and 5-fluororuacil (MF), a combination of cyclophosphamide, doxorubicin and 5-fluororuacil (CAF), or a combination of 5-fluororuacil, epirubicin, and cyclophosphamide (FEC)).
Results
Patient characteristics and neuropathy rates
Table 1 describes patient and breast cancer characteristics and frequency of PN reporting among different groups. The mean and median age of patients at time of SV was 59 (SD 11) years and 60 (range 31–93) years, respectively. The mean and median time from diagnosis to SV was 7.2 (SD 3.3) years and 6.3 (range 2–20.7), respectively.
One hundred sixty-two patients in our cohort reported PN symptoms at the time of the SV (26.8%), the point prevalence of PN throughout the years of follow-up ranged between 15% and 30%, approximately. The prevalence of PN symptoms in patients who were less than 6 years from therapy was 29.7% compared to 24.7% in patients who were at least 6 years out from therapy. Twenty-nine (4.8%) reported having PN symptoms before their breast cancer diagnosis.
Risk factors for PN
Table 2 summarizes univariable and multivariable risk factors for PN. Several factors were associated with increased reporting of PN on univariable analysis, including: obesity, PN reporting before diagnosis, stage II and III disease, mastectomy surgery, and receiving taxane regimens (all p < 0.05). On the other hand, older age, exercise, ER-positive disease, and endocrine therapy were associated with lower risk of PN (all p < 0.05). Only type of chemotherapy and PN symptoms prior to breast cancer diagnosis remained prognostic for PN on multivariable analysis; docetaxel- and paclitaxel-containing regimens had a higher risk of PN relative to no chemotherapy (OR 2.18 and 4.07, respectively), as did patients who reported PN symptoms before diagnosis (OR 3.28). No difference was observed in PN prevalence among patients who received every 2–3-week paclitaxel scheduling (49/118: 41.5%) compared with PN prevalence among those who had received predominantly weekly paclitaxel regimens (24/48: 50%) (p = 0.32). In patients who reported no PN symptoms before diagnosis, the probability of reporting PN was 15% in the absence of chemotherapy, 19% following a non-taxane regimen, 28% following a docetaxel-containing regimen, and 43% following a paclitaxel-containing regimen. In contrast, the respective probabilities were 37, 44, 57, and 71% among patients who reported PN symptoms before diagnosis.
Discussion
This study investigated the long-term prevalence of PN in breast cancer survivors attending a survivorship clinic. The prevalence of short-term PN in breast cancer survivors has been investigated in several studies [8,9,10]; however there is little information about the long-term course of chemotherapy associated PN [9, 12, 16, 17] (Table 3). In a meta-analysis evaluating the prevalence of PN in 4179 patients receiving chemotherapy of any type for a variety of different cancers, Seretny et al. [18] found that PN was reported in 68% at one month, 60% at 3 months, 30% at 6 months or more after chemotherapy; it was concluded that PN symptoms decrease with time. In a prospective cohort of 50 breast cancer survivors receiving taxane chemotherapy, formal assessments of neurotoxicity demonstrated improvement at 12 months post therapy compared to within two weeks of treatment completion [9]. These studies indicate that that PN symptoms improve within the first year after treatment. Our study showed that, however, PN symptoms are present for years following diagnosis, particularly among those who received paclitaxel or docetaxel chemotherapy, with estimated point prevalence about 15–20% 9 years from diagnosis. Bao et al. [12] observed in 296 breast cancer survivors who had received taxane chemotherapy that 58% of patients reported PN symptoms at a mean of 6.3 ± 3 years post diagnosis, however, the study included patients who were still within their first 2 years from treatment. In our study, the prevalence of long-term PN was 27% overall at a mean of 6.3 ± 3.3 years post diagnosis and as high as 44% among those who had received paclitaxel chemotherapy. Symptoms of numbness and tingling may be due to conditions other than chemotherapy and, in fact, some patients reported having these symptoms even prior to their cancer diagnosis. Excluding patients who reported having PN symptoms prior to their cancer diagnosis, PN rates were 28–43% with docetaxel or paclitaxel chemotherapy compared with 15-19% following no chemotherapy or non-taxane chemotherapy.
It is also worth noting that some patients who do not experience PN symptoms immediately after therapy may develop symptoms after months or years; this phenomenon is termed coasting [17, 19]. In a study of 790 breast cancer survivors who received docetaxel and did not experience immediate PN symptoms, PN developed as a late complication in 79 patients after 1–3 years [17]. This indicates that long-term follow-up is essential for understanding the risk of neuropathy in this population.
There is a significant variability in reported prevalence of short-term and long-term PN in cancer survivors in literature [4]. PN symptoms may be affected by patient demographics, comorbidities, genetics, type of chemotherapy used, and the timing of assessments [20]. In addition to that, there is a lack of a universally accepted defining tool for chemotherapy induced PN and the diagnostic criteria are not universally applicable or fully validated [4]. Adding further to the complexity, there is significant discrepancy between patient-reported symptoms of PN and health care provider assessments using different tools, leading to inconsistent and sometimes conflicting interpretation of patient-reported symptoms [21] Similar to our study, most studies have assessed PN by symptoms without physical examination or nerve conduction studies [12, 16, 17].
In our study, exposure to taxane regimens was significantly associated with increased reporting of PN symptoms in breast cancer survivors. While the literature is contradictory regarding whether paclitaxel or docetaxel is more neurotoxic [20], we observed that long-term PN symptoms were reported more frequently in patients who received paclitaxel (44%) compared to people who received docetaxel-containing regimens (31%). Other studies demonstrated that age and obesity are risk factors for persistent PN symptoms in breast cancer survivors, [12, 17]. In our study, obese patients were two times more likely to report PN compared to underweight and normal weight patients (OR 1.93, CI 1.23–3.04, p = 0.004); however this effect was not observed on multivariable analysis. In addition, the prevalence of PN symptoms in our study did not vary by time from treatment beyond 2 years (OR 0.98, 95% CI 0.93–1.04, p = 0.60). Despite that alcohol and diabetes are important risk factors for PN, we did not observe an association in this study. On univariable analysis, patients who had hormone receptor positive disease, those who received hormonal therapy, and those with lower disease stage reported less PN; these are all factors that might be associated with a lower likelihood of receiving chemotherapy. Additionally, patients who reported regular exercise also reported less PN symptoms, a finding warranting further investigation.
There are several limitations to this study. The cross-sectional design assesses PN symptoms at one-point in time for each subject and cannot determine the evolution of symptoms over time. We estimated PN prevalence using symptoms as a surrogate which is not optimal and we were unable to assess the severity and distribution of PN symptoms in patients, the impact of those symptoms on quality of life, or therapies used to manage the symptoms. Furthermore, it is possible that patient risk factors for neuropathy may have influenced chemotherapy choice in this non-randomized population. Another limitation is that the data were derived from a single tertiary hospital and patients analyzed were those who were referred and agreed to attend the survivorship clinic subjecting the information to potential selection bias. Reassuringly, the median age of 59 years for patients in this study is similar to median age of 60 years for early stage breast cancer patients seen at our institution from 2010 to 2015. The stage breakdown for early stage patients during this timeframe at our institution was 19% stage 0, 44% stage I, 27% stage II and 10% stage III; this distribution is similar to the study population with the exception that stage 0 appears to be under-represented in the study population.
In conclusion, persistent PN symptoms in breast cancer survivors are common even years out from initial treatment. Exposure to taxane-including regimens and reporting PN before diagnosis were risk factors for long-term PN symptoms using multivariable analysis. The lack of universally accepted and practical methods to diagnose PN remains an obstacle to better estimate the prevalence of PN. Long-term prospective cohort studies are needed to determine natural course and associated risk factors as well as attenuating factors for PN in breast cancer survivors. Moreover, interventional studies are needed to explore therapeutic options to reduce the long-term burden of PN in breast cancer survivors.
References
Cavaletti G, Zanna C (2002) Current status and future prospects for the treatment of chemotherapy-induced peripheral neurotoxicity. Eur J Cancer 38(14):1832–1837
Balayssac D, Ferrier J, Descoeur J, Ling B, Pezet D, Eschalier A, Authier N (2011) Chemotherapy-induced peripheral neuropathies: from clinical relevance to preclinical evidence. Expert Opin Drug Saf 10(3):407–417
England JD, Gronseth GS, Franklin G, Miller RG, Asbury AK, Carter GT, Cohen JA, Fisher MA, Howard JF, Kinsella LJ, Latov N, Lewis RA, Low PA, Sumner AJ (2005) Distal symmetric polyneuropathy: a definition for clinical research: report of the American Academy of Neurology, the American Association of Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology 64(2):199–207. doi:10.1212/01.wnl.0000149522.32823.ea
Cavaletti G, Marmiroli P (2015) Chemotherapy-induced peripheral neurotoxicity. Curr Opin Neurol 28(5):500–507
Pachman DR, Barton DL, Swetz KM, Loprinzi CL (2012) Troublesome symptoms in cancer survivors: fatigue, insomnia, neuropathy, and pain. J Clin Oncol 30(30):3687–3696. doi:10.1200/jco.2012.41.7238
Mols F, Beijers T, Vreugdenhil G, van de Poll-Franse L (2014) Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer 22(8):2261–2269
Pike CT, Birnbaum HG, Muehlenbein CE, Pohl GM, Natale RB (2012) Healthcare costs and workloss burden of patients with chemotherapy-associated peripheral neuropathy in breast, ovarian, head and neck, and nonsmall cell lung cancer. Chemother Res Pract 2012:913848. doi:10.1155/2012/913848
Jud SM, Hatko R, Maihofner C, Bani MR, Schrauder MG, Lux MP, Beckmann MW, Bani G, Eder I, Fasching PA, Loehberg CR, Rauh C, Hein A (2014) Comprehensive visualization of paresthesia in breast cancer survivors. Arch Gynecol Obstet 290(1):135–141. doi:10.1007/s00404-014-3164-1
Hershman DL, Weimer LH, Wang A, Kranwinkel G, Brafman L, Fuentes D, Awad D, Crew KD (2011) Association between patient reported outcomes and quantitative sensory tests for measuring long-term neurotoxicity in breast cancer survivors treated with adjuvant paclitaxel chemotherapy. Breast Cancer Res Treat 125(3):767–774. doi:10.1007/s10549-010-1278-0
Tanabe Y, Hashimoto K, Shimizu C, Hirakawa A, Harano K, Yunokawa M, Yonemori K, Katsumata N, Tamura K, Ando M, Kinoshita T, Fujiwara Y (2013) Paclitaxel-induced peripheral neuropathy in patients receiving adjuvant chemotherapy for breast cancer. Int J Clin Oncol 18(1):132–138. doi:10.1007/s10147-011-0352-x
Mustafa Ali M, Moeller M, Rybicki L, Moore HC (2017) Prevalence and correlates of patient-reported symptoms and comorbidities in breast cancer survivors at a tertiary center. J Cancer Survivorship. doi:10.1007/s11764-017-0612-5
Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ (2016) Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159(2):327–333. doi:10.1007/s10549-016-3939-0
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Mayer DK, Nekhlyudov L, Snyder CF, Merrill JK, Wollins DS, Shulman LN (2014) American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. J Oncol Pract Am Soc Clin Oncol 10(6):345–351. doi:10.1200/jop.2014.001321
Hausman J, Ganz PA, Sellers TP, Rosenquist J (2011) Journey forward: the new face of cancer survivorship care. J Oncol Pract Am Soc Clin Oncol 7(3 Suppl):e50s–56s. doi:10.1200/jop.2011.000306
Andersen KG, Jensen MB, Kehlet H, Gartner R, Eckhoff L, Kroman N (2012) Persistent pain, sensory disturbances and functional impairment after adjuvant chemotherapy for breast cancer: cyclophosphamide, epirubicin and fluorouracil compared with docetaxel+epirubicin and cyclophosphamide. Acta Oncol 51(8):1036–1044. doi:10.3109/0284186x.2012.692884
Eckhoff L, Knoop A, Jensen MB, Ewertz M (2015) Persistence of docetaxel-induced neuropathy and impact on quality of life among breast cancer survivors. Eur J Cancer 51(3):292–300. doi:10.1016/j.ejca.2014.11.024
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M (2014) Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain 155(12):2461–2470. doi:10.1016/j.pain.2014.09.020
Osmani K, Vignes S, Aissi M, Wade F, Milani P, Levy BI, Kubis N (2012) Taxane-induced peripheral neuropathy has good long-term prognosis: a 1- to 13-year evaluation. J Neurol 259(9):1936–1943. doi:10.1007/s00415-012-6442-5
Kerckhove N, Collin A, Condé S, Chaleteix C, Pezet D, Balayssac D (2017) Long-term effects, pathophysiological mechanisms, and risk factors of chemotherapy-induced peripheral neuropathies: a comprehensive literature review. Front Pharmacol. doi:10.3389/fphar.2017.00086
Alberti P, Rossi E, Cornblath DR, Merkies IS, Postma TJ, Frigeni B, Bruna J, Velasco R, Argyriou AA, Kalofonos HP, Psimaras D, Ricard D, Pace A, Galie E, Briani C, Dalla Torre C, Faber CG, Lalisang RI, Boogerd W, Brandsma D, Koeppen S, Hense J, Storey D, Kerrigan S, Schenone A, Fabbri S, Valsecchi MG, Cavaletti G (2014) Physician-assessed and patient-reported outcome measures in chemotherapy-induced sensory peripheral neurotoxicity: two sides of the same coin. Ann Oncol 25(1):257–264
Funding
No funding received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that there is no conflict of interest.
Ethical approval
All procedures performed in studies were in accordance with the ethical standards of the Cleveland Clinic institutional review board and the national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Previous presentation
Study results were published online for 2017 ASCO Annual Meeting.
Rights and permissions
About this article
Cite this article
Mustafa Ali, M., Moeller, M., Rybicki, L. et al. Long-term peripheral neuropathy symptoms in breast cancer survivors. Breast Cancer Res Treat 166, 519–526 (2017). https://doi.org/10.1007/s10549-017-4437-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4437-8