Abstract
Purpose
The Short Form version of the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-SF) was designed to measure patients’ subjective experience of enjoyment and satisfaction. However, it had not yet been validated for Chinese societies. This paper reports on the validation of the Chinese version of the Q-LES-Q-SF among primary care patients in Taiwan.
Methods
The study included adult patients in primary care clinics. The participants completed the Q-LES-Q-SF, the Patient Health Questionnaire, and the Short Form Health Survey. After that, the trained researchers interviewed the patients using the mood module of the Schedules for Clinical Assessment in Neuropsychiatry and the 17-item Hamilton Rating Scale for Depression. A subsample of participants was reassessed with Q-LES-Q-SF within a 2-week interval.
Results
A total of 1,482 patients completed the Q-LES-Q-SF. The content validity was good, with no significant floor/ceiling effect. The internal consistency of the Q-LES-Q-SF proved to be substantial as well as the test–retest reliability. The factor structure was examined by exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The EFA yielded a 2-factor structure, which was confirmed by a CFA with acceptable fit indices. Known-group validity of the Q-LES-Q-SF was satisfactory in distinguishing patients with and without depression, according to hierarchical regression analyses. Evidence of concurrent validity was provided for the Q-LES-Q-SF, and its two subscales identified significant correlations with other measures.
Conclusion
The Chinese Q-LES-Q-SF was shown to have adequate validity and reliability. It may be a useful tool to measure patients’ quality of life in Chinese societies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In assessing patients’ clinical conditions, there is increasing consensus among clinicians and researchers that in addition to the presence or absence of symptoms, broader dimensions, such as quality of life (QOL), should be included. To meet such a need, a number of different QOL assessment procedures have been developed. Health-related QOL has become an important outcome measure for psychiatric patients and has been intensively investigated as a measure of outcome in clinical trials, adherence with medication, and adaptation to social environments [1–7].
The Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) is a self-report measure with 93 items that assesses QOL from the point of view of the subject [8]. Since 1993, it has been widely used in QOL outcome studies of mentally disabled patients and shown good reliability, validity, and stability in non-psychiatric populations and in patients [8–13]. However, the Q-LES-Q is a lengthy questionnaire that takes between 40 and 45 min to complete. The Short Form of Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-SF) has only 16 items and includes the same content as the general activities section of the longer version. The Q-LES-Q-SF has been also demonstrated to be a highly reliable and valid measure in adults [1, 14–16]. It is increasingly used in psychiatry because it gives emphasize to the subjective perspectives of patients on physical, psychological, and social domains of daily life.
The Q-LES-Q and its short form (Q-LES-Q-SF) have been translated into several languages and validated in populations of different lifestyles and economic backgrounds [8, 13, 14, 17–21]. This instrument is widely in use internationally and should be validated in a Chinese population. To the best of our knowledge, it had not yet been validated for Chinese societies, including Taiwan. In the present study, we document the psychometric properties of the Chinese Q-LES-Q-SF in Taiwan.
Methods
Study setting
The protocol was approved by the institutional review board of the Mackay Memorial Hospital in Taipei, Taiwan. The study was part of a larger investigation of outcomes of service enhancement with case management for major depressive disorder (MDD) in primary care. The study was undertaken in 6 community-based primary clinics and several hospital-based outpatient clinics of the Family Medicine Department in Taipei from September 2007 to December 2008. All adult patients, 18 years or older, who visited the clinics mentioned above and speak Chinese were invited to join the study while they were waiting for their clinical visits.
Study procedure
All participants gave written informed consent after receiving a full description of the study procedures. They were then asked to complete the Chinese version of the Q-LES-Q-SF, the Patient Health Questionnaire 9-item (PHQ-9), and the Short Form Health Survey (SF-12) during or shortly after their visits to see their primary care physicians. After the participants had completed these questionnaires, trained research staff blinded to the results from the questionnaires interviewed the patients using the mood module of the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) and the 17-item of Hamilton Rating Scale for Depression (HAMD-17). A subsample of participants was re-administered the Chinese version of the Q-LES-Q-SF within 2 weeks of the index visit.
Measures
The Q-LES-Q-SF is a self-reported questionnaire, with 16 items, derived from the general activities scale of the original 93-item form [8]. It evaluates overall enjoyment and satisfaction with physical health, mood, work, household and leisure activities, social and family relationships, daily functioning, sexual life, economic status, overall well-being and medications. Items are rated on a 5-point scale (“not at all or never” to “frequently or all the time”), with higher scores indicating better enjoyment and satisfaction with life. The scoring of the Q-LES-Q-SF involves summing only the first 14 items to yield a total score. The last two items, about medications and overall life satisfaction, are not included in the total score but are stand-alone items. The total score ranges from 14 to 70 and is usually expressed as a percentage (1–100) of the maximum total score that is achievable, as presented in this study. The original Q-LES-Q-SF was translated into traditional Chinese by a bilingual psychiatrist. The translated version was back-translated into English and modified until the back-translated version was comparable with the original English version. Some patients and experienced psychiatric nurses were invited to review and provide feedback. The Chinese version was then pretested in a small group of psychiatric patients prior this study to test the cultural appropriateness and content validity [22].
The PHQ-9 is a self-administered measure designed for identifying MDD in primary care and non-psychiatric settings. It contains items derived from the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV). The PHQ-9 has been validated in multiple studies conducted in different situations of clinical services and in different cultures. The Chinese version of the PHQ-9 has been validated for the Taiwanese population in primary care [23].
The HAMD-17 is a standardized interview-based assessment examining the frequency and intensity of 17 depressive symptoms. It is one of the most commonly used instruments for rating the overall levels of depression severity in medical studies [24]. The investigator should choose the possible responses to each question by interviewing the patient and by observing his or her symptoms. Each question has between 3 and 5 possible responses that increase in severity. It yields a total score ranging from 0 to 52. Higher values represent greater symptom severity. The reliability and validity of the Chinese version of the HAMD-17 have been demonstrated, showing good inter-rater reliability and internal reliability. Its concurrent validity is excellent while comparing the Global Assessment Scale [25].
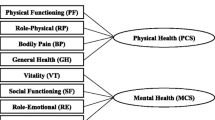
The SF-12 is a shorter version of the SF-36 Health Survey, a generic health-related QOL questionnaire [26]. It is composed of 12 items and provides physical component summary (PCS) and mental component summary (MCS) scores as well as the SF-36. The SF-36 has been validated and used extensively in Taiwan [27].
The SCAN is a set of clinical assessment instruments aimed at assessing, measuring, and also providing possibilities for categorical assessment of psychopathology and behavior associated with the major psychiatric disorders in adult life [28]. It can be used for clinical, research, and training purposes and was developed within the framework of the World Health Organization. The cross-cultural clinical equivalence and reliability of a Chinese version of the SCAN in Taiwan suggested that no between-group differences were found for most individual items, and cross-cultural implementation based on SCAN in Taiwan appears valid [29]. In this study, the mood module of the SCAN was used to identify the patients with MDD in the past one month. Two psychiatric research nurses with 4 years of psychiatric research experience were trained in the administration of SCAN for 6 months. At the end of that period, there was good inter-rater reliability between a research psychiatrist and the research nurses (generalized kappa of 0.88 for the diagnosis of MDD according to DSM-IV criteria).
Statistical analyses
Descriptive statistics were generated and distributions of variables were checked for normality before statistical analyses. Floor and ceiling effects were calculated as the percentages of patients with the lowest or highest scale item (or possible sum score) out of the total number of patients. Floor and ceiling effects were present if more than 15 % of respondents achieved the lowest or highest possible score [30]. Cronbach’s α was used to determine the internal consistency (≧0.70; Cohen) [31]. The intra-class correlation coefficient (ICC) was used to examine test–retest reliability for the two assessments at an interval of 2 weeks.
To analyze the construct structure of the Chinese Q-LES-Q-SF, the sample was randomly split into two halves using the algorithm available in the SPSS: one for exploratory factor analysis (EFA) and one for confirmatory factor analysis (CFA). The EFA was performed with principal component and Varimax rotation. Factors with eigenvalues greater than one were retained, and variables with an absolute loading greater than the amount set in the minimum loading option (>0.4) were selected [32–34]. The CFA was performed to assess the goodness of fit of the factor structure extracted from the EFA. The maximum-likelihood estimation (MLE) method was used to test the covariance matrix to determine how well the model fits the sample data. Traditionally, the chi-square test is applied to assess the goodness of fit for a model. However, the chi-square test is very sensitive to sample size (may reject a model with good fit if sample size is large). In this study, three other indexes, including goodness-of-fit index (GFI), adjusted GFI (AGFI), and the root of the mean square residual (RMR), were chosen to assess the fit of the model [35–37]. Values of GFI greater than 0.9, AGFI greater than 0.8, and RMR less than 0.1 indicate a good fit [37].
To verify concurrent validity, the Pearson’s correlation coefficient was used to analyze the correlation between the Q-LES-Q-SF and the other instruments. The SF-12 was used for concurrent validity because it has been used extensively for QOL studies of a wide range of disease, including depression [38–40]. We also investigated the association of the Q-LES-Q-SF with measures of depression (i.e., PHQ-9 and HAMD-17) to establish that scores of Q-LES-Q-SF are higher when people have lower scores on depression scale. Confirmation of these properties enables the Q-LES-Q-SF to be used with confidence in outcome studies of depression. We considered a correlation of <0.3 to be small, 0.3–0.5 moderate, and ≧0.5 large [31].
Known-group validity refers to whether an instrument can differentiate between groups of patients whose health status differs, in this case patients with versus without MDD, diagnosed by SCAN interview. We expected participants without MDD to have better QOL than participants with MDD, using the Mann–Whitney U test. Given the sample was collected from a primary care setting, the information regarding the presence or absence of physical complaints was a possible covariate. Hierarchical regression analyses (stepwise method) were performed to test the hypothesized associations between MDD and QOL, with the Q-LESQ-SF as the dependent variable. All sociodemographic variables were introduced at a first step, followed by two clinical variables of depression (with vs. without MDD) and physical problems (with vs. without physical complaints) on a second step to examine its unique association with QOL accounting for all other variables.
The CFA analyses were performed with AMOS 18.0. All the other analyses were conducted using the SPSS 18.0. All analyses employed a significance level of 0.05. A Bonferroni correction was applied to adjust the significance level of multiple comparisons.
Results
Demographics
Study participants consisted of 1,482 subjects including 614 male (41.43 %) and 868 female (58.57 %), with a mean age of 54.65 years (SD 18.64). Of the 1482 subjects who completed the Chinese version of the Q-LES-Q-SF, 1,100 (74.22 %) received the SCAN diagnostic interviews by mental health professionals. Of the 1,100 who were interviewed with SCAN, 29 subjects (2.64 %) were diagnosed as having MDD in the past one month. Table 1 shows basic demographic and clinical characteristics. As shown in Table 2, the average raw score on the Q-LES-Q-SF was 47.93 (SD 6.15), or 68.47 % of the total score of 70. The mean raw score of each item and raw total score of Q-LES-Q-SF are also reported in Table 2. Distributions of scores for each item were normal, with skewness and kurtosis within acceptable limits [35]. No floor effect was observed. Ceiling values were less than 12.1 %.
Reliability
The internal consistency of the Q-LES-Q-SF, as measured by Cronbach’s α coefficient, was found to be substantial (α = 0.87). No items showed significantly lower item-total correlation compared to the other items. The test–retest reliability was high (ICC = 0.75) using data from the 199 participants who were re-administered the Q-LES-Q-SF 2 weeks after the first administration.
Validity
EFA was first performed on a random 50 % of the total sample. Bartlett’s test of sphericity was statistically significant (P < 0.001), and the Kaiser–Meyer–Olkin value was 0.90. The inspection of scree plot (Fig. 1) showed two factors in the analysis. Factor 1 consisted of 10 items (items 2-11) representing “psychosocial dimension” with eigenvalue of 5.24, accounting for 37.41 % of variance. Factor 2 consisted of 4 items (items 1, 12, 13, and 14) representing “physical dimension” with eigenvalue of 1.27, accounting for 9.07 % of variance. All the factor-pattern coefficients were above 0.40, indicating that all the items were salient (Table 3).
The CFA was used to determine the goodness of fit of the previously identified two-factor model. The results of CFA for the model showed that χ2 = 415.18, df = 76, P < 0.001, GFI = 0.93, AGFI = 0.90, and RMR = 0.03. The values of GFI, AGFI, and RMR were considered as acceptable [35–37]. The factor loadings for each of the 14 items ranged from 0.67 to 1.46, and all of the factor loadings were significant at P < 0.05. Thus, the two-factor model was confirmed by a CFA.
Based on the grouping of items resulting from CFA, two subscales of the Q-LES-Q-SF were created by summing the raw values of the items attributed to each factor. As shown in Table 4, the concurrent validity of the Q-LES-Q-SF (the whole scale and two subscales) versus other scales was examined. Correlations between the SF-12 subscales with the overall Q-LES-Q-SF were moderate (r range 0.35–0.38, all Ps < 0.001); correlations between two clinical measures (PHQ-9 and HAMD-17) with the Q-LES-Q-SF (total and two subscales) were also moderate, but negative (r range −0.37–−0.49, all Ps < 0.001). As expected, the physical subscale of the Q-LES-Q-SF had a moderate correlation with PCS-12 (r = 0.39) and the psychosocial subscale of the Q-LES-Q-SF had a moderate correlation with the MCS-12 (r = 0.37), whereas the physical subscale of the Q-LES-Q-SF had a small correlation with the MCS-12 (r = 0.28) and the psychosocial subscale of the Q-LES-Q-SF also had a small correlation with PCS-12 (r = 0.27). These results confirmed the concurrent validity of the Chinese version of the Q-LES-Q-SF.
Table 2 shows the mean raw scores of each item and total scale of Q-LES-Q-SF among depressed and non-depressed patients. As shown in Table 2, the Mann–Whitney U tests revealed significant differences between subjects with versus without a MDD across all of the individual items and the whole scale measured by the Q-LES-Q-SF. Depressed patients displayed significantly poorer scores of the Q-LES-Q-SF than those without depression. Simple linear regression revealed that both variables of MDD and presence of physical complaints were significant predictors of the Q-LES-Q-SF. Hierarchical multiple regression strategies (stepwise method) were used to determine the predictors of Q-LES-Q-SF scores. As shown in Table 5, QOL was found to be significantly associated with education, marital status, and socioeconomic status in Model 1. In Model 2, the significant association with these sociodemographic variables was unchanged, and QOL also showed significant associations with two clinical variables, MDD and physical complaints. MDD remained in the model as the strongest predictor for QOL. The adjusted R 2 for Model 2 was bigger than the R 2 for Model 1, and the change in R 2 was also significant.
Discussion
This is the first study to validate the Chinese version of the Q-LES-Q-SF. We demonstrate that the Chinese version of the Q-LES-Q-SF is a reliable and valid measure of quality of life using data from a large sample of Taiwanese primary care patients in the present study. Most of validity and reliability analysis of data generated in this study was conducted according to parameters described in similar studies developed by other investigators.
Internal consistency data revealed a high reliability evidenced by internal consistency Cronbach’s α (0.87) for the Chinese Q-LES-Q-SF. The internal consistency reliability coefficients of the short form or the general activities scale of the Q-LES-Q, an equivalent to the short form, are also high in many versions including the original English version [8] and other language versions used in various countries (range from 0.9 to 0.95) [14, 17].
As is the case with the original version [8] and many other versions [7, 14, 18, 41], the Chinese Q-LES-Q-SF has been demonstrated to have high test–retest reliability in the 2-week interval. The analysis demonstrates that it is appropriate for individual comparisons, implying its stability in repeated assessments.
The EFA for the Chinese Q-LES-Q-SF yielded a 2-factor structure (psychosocial and physical dimensions). The 2 factors accounted for 46.47 % of the variance, which appears to be sufficient, although not ideal. Factor 1 consisted of 10 items (items 2–11), including satisfaction of mood, work, household activities, social relationships, family relationships, leisure time activities, ability to function in daily life, sexual drive, interest, and/or performance, economic status, and living/housing situation, so we conceptualized factor 1 as psychosocial dimension of the Chinese Q-LES-Q-SF. Factor 2 was composed of 4 items (items 1, 12–14) covering physical health, ability to get around physically, vision in terms of ability to do work/hobbies, and overall sense of well-being; thus, we conceptualized factor 2 as physical dimension of the Chinese Q-LES-Q-SF. Furthermore, a subsequent CFA indicated that the data sufficiently fit the 2-factor model [36]. To the best of our knowledge, the factor structure of the Q-LES-Q-SF has not been reported earlier in adult population. Inconsistent with a previous study [41], it revealed that an exploratory principal component factor analysis of pediatric version of the Short Form of the Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q) indicated that a single factor accounted for 37 % of the variance and all of the items had their highest loading on the first factor. PQ-LES-Q has 15 items and is almost alike to Q-LES-Q-SF except lack of an item of satisfaction of medication. The sample that included outpatient children (6–11 years old) and adolescents (12–17 years old) with MDD in the previous study differs much from that of the present study. The difference of patients’ age and diagnosis may influence the result of factor analysis much. Our study, therefore, provides some new and important information.
Regarding concurrent validity, correlations between the Chinese Q-LES-Q-SF and both the PCS and MCS of SF-12 health survey are positive significantly, which demonstrate that these questionnaires are congruent with each other regarding patients’ well-being. Higher scores on both dimensions of SF-12 are associated with higher satisfaction of QOL measured by the Chinese Q-LES-Q-SF, which result is consistent with previous studies. A previous study [19] implies that improvements in Q-LES-Q scores are associated with improvements in overall mental health and vitality measured by the SF-36. The subscales of Q-LES-Q-SF are significantly correlated with the PCS and MCS; there are, however, validation subscales that show stronger associations with corresponding domains. This may be depicting the complex and interrelated nature of health-related QOL.
The anticipated association between poorer QOL and depression was confirmed by “dimensional” and “categorical” assessments. The Chinese version of the Q-LES-Q-SF and its two subscales presented significant negative Pearson’s correlation scores with both scales measuring severity of depression, PHQ-9, and the HAMD-17. The more depressed patients reported lower enjoyment and satisfaction of QOL. Similarly, the results of other previous studies show that Q-LES-Q scores are associated negatively with severity of depressive symptoms [9, 13, 19, 20]. Regarding the known-group validity, individuals with MDD had significant lower scores in the total scale and each item of the Chinese Q-LES-Q-SF, using either t test (data not shown) or the Mann–Whitney’s U test. Using the hierarchical multiple regression strategies to control for the sociodemographic variables and physical complaints, MDD remained the strongest predictor for the Q-LES-Q-SF. The Chinese Q-LES-Q-SF was thus proved to have good capacity to discriminate depressed and non-depressed patients in the sample. This is in line with the other quality of life studies on MDD [1, 18]. It should also be noted that one-month prevalence rate of MDD was low (2.64 %) in our study, with the figure being much lower than those reported in the literature [42]. However, the finding of a low prevalence of MDD in this study is similar to that in the previous national epidemiological studies in Taiwan [43, 44]. In a national epidemiological study using representative samples between 2003 and 2005 in Taiwan, a low prevalence rate of MDD was reported, with 12-month and lifetime prevalence being 0.6 % and 1.2 %, respectively [43]. We speculated that the cultural factors may be responsible for this difference.
Implications
The strengths of this study include the use of a validated criterion standard administered by trained researchers blinded to the results of the tested instrument to avoid interview bias, and the recruitment of a large number of patients from both community-based and hospital-based primary care clinics to provide sample diversity. The sample size in this study was much larger than some previous studies of psychometric properties of full version or short form of Q-LES-Q [10, 14, 16, 18, 20, 21].
The experience of enjoyment and satisfaction is an important aspect of life. In clinical assessments, if we only measure the severity of symptoms and impairments of psychosocial functioning, we would ignore this important aspect of life. The Q-LES-Q-SF is a short questionnaire that is easy to use in many clinical settings and it only takes just a little time to complete. The present study has provided the parameters of validity and reliability of the Chinese version of the Q-LES-Q-SF. We consider the findings robust and trustworthy with this large sample size containing 1,482 primary care patients. Given its high validity and ease of administration for primary care patients, the Q-LES-Q-SF can be used widely in clinical services. Busy primary care medical staff would find this questionnaire to be a useful and simple tool that can be applied routinely in measuring and monitoring patients’ QOL.
Limitations
The present study has some limitations. First, our patients were recruited from primary care clinics of northern Taiwan; hence, the results may differ to some extent in other clinical settings or other regions with different ethnic backgrounds or cultures. Moreover, we excluded participants who were younger than the age of 18 years. There might be a bias when this self-report measure is used in surveying people under the age of 18. However, mental disorders are common among adolescents in Taiwan [45]; thus, it is important to meet the identified need to assess the status of QOL and changes in QOL with treatment in this group. The original author of Q-LES-Q developed PQ-LES-Q to aid in the assessment of an important aspect of life experience in children and adolescents (6–17 years old) [41]. It was proved to have good reliability and validity [41]. In the future, it will be necessary to develop the Chinese version of the PQ-LES-Q for patients under 18 years old. Second, we did not estimate the concurrent validity with respect to the “original” version of the Q-LES-Q because the study was administered as part of a large-scale interventional outcome study for MDD in primary care. Considering that one of the most important ways to validate the short form of an instrument is based upon the estimate of concurrent validity with respect to the “original” version of the instrument, it would be informative to examine the relationship of the Q-LES-Q-SF with the “original” version of the Q-LES-Q. Another significant limitation is that patients’ comorbid chronic medical disorders were not accounted for in the present analyses. It is certainly possible that poor QOL in patients with MDD is more strongly related to coexisting chronic physical disorders, and multiple disorders could have an additive effect on QOL. Future research should incorporate chronic medical disorders and examine this effect. Finally, our study is a cross-sectional design. Further longitudinal studies are needed to establish its sensitivity to change.
Conclusion
This study showed that the original English version of the Q-LES-Q-SF can be successfully adapted to Chinese with satisfactory psychometric properties of validity and reliability among Chinese primary care patients in Taiwan. Importantly, the Chinese version of the Q-LES-Q-SF was well accepted by patients and primary care physicians as it has the advantage of being a time-saving and brief instrument. If it can be well integrated into primary care services, it may be a useful adjunct in the daily practice of clinicians to heighten their awareness to this important aspect of patients’ life.
Abbreviations
- HAMD-17:
-
17-item of Hamilton Rating Scale for Depression
- MDD:
-
Major depressive disorder
- MCS:
-
Mental component score
- PCS:
-
Physical component score
- PHQ-9:
-
Patient Health Questionnaire 9-item
- PQ-LES-Q:
-
Pediatric version of the Short Form of the Quality of Life Enjoyment and Satisfaction Questionnaire
- QOL:
-
Quality of life
- Q-LES-Q:
-
Quality of Life Enjoyment and Satisfaction Questionnaire
- Q-LES-Q-SF:
-
Short Form of Quality of Life Enjoyment and Satisfaction Questionnaire
- SCAN:
-
Schedules for Clinical Assessment in Neuropsychiatry
- SF-12:
-
Short Form Health Survey
References
Rapaport, M. H., Clary, C., Fayyad, R., & Endicott, J. (2005). Quality-of-life impairment in depressive and anxiety disorders. American Journal of Psychiatry, 162(6), 1171–1178. doi:10.1176/appi.ajp.162.6.1171.
Lehman, A. F. (1983). The well-being of chronic mental patients. Archives of General Psychiatry, 40(4), 369–373.
Lehman, A. F. (1996). Measures of quality of life among persons with severe and persistent mental disorders. Social Psychiatry and Psychiatric Epidemiology, 31(2), 78–88.
Voruganti, L., Heslegrave, R., Awad, A. G., & Seeman, M. V. (1998). Quality of life measurement in schizophrenia: Reconciling the quest for subjectivity with the question of reliability. Psychological Medicine, 28(1), 165–172.
Ritsner, M., & Kurs, R. (2002). Impact of antipsychotic agents and their side effects on the quality of life in schizophrenia. Expert Review of Pharmacoeconomics and Outcomes Research, 2(4), 347–356. doi:10.1586/14737167.2.4.347.
Ritsner, M., & Kurs, R. (2003). Quality of life outcomes in mental illness: Schizophrenia, mood and anxiety disorders. Expert Review Pharmacoeconomics and Outcomes Research, 3(2), 189–199. doi:10.1586/14737167.3.2.189.
Ritsner, M., Kurs, R., Gibel, A., Ratner, Y., & Endicott, J. (2005). Validity of an abbreviated Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-18) for schizophrenia, schizoaffective, and mood disorder patients. Quality of Life Research, 14(7), 1693–1703. doi:10.1007/s11136-005-2816-9.
Endicott, J., Nee, J., Harrison, W., & Blumenthal, R. (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: A new measure. Psychopharmacology Bulletin, 29(2), 321–326.
Michalak, E. E., Murray, G., Levitt, A. J., Levitan, R. D., Enns, M. W., Morehouse, R., et al. (2007). Quality of life as an outcome indicator in patients with seasonal affective disorder: Results from the Can-SAD study. Psychological Medicine, 37(5), 727–736. doi:10.1017/S0033291706009378.
Schechter, D., Endicott, J., & Nee, J. (2007). Quality of life of ‘normal’ controls: Association with lifetime history of mental illness. Psychiatry Research, 152(1), 45–54. doi:10.1016/j.psychres.2006.09.008.
Seidman, S. N., & Rabkin, J. G. (1998). Testosterone replacement therapy for hypogonadal men with SSRI-refractory depression. Journal of Affective Disorders, 48(2–3), 157–161.
Pohl, R. B., Wolkow, R. M., & Clary, C. M. (1998). Sertraline in the treatment of panic disorder: A double-blind multicenter trial. American Journal of Psychiatry, 155(9), 1189–1195.
Goracci, A., Martinucci, M., Scalcione, U., Fagiolini, A., & Castrogiovanni, P. (2005). Quality of life and subthreshold affective symptoms. Quality of Life Research, 14(3), 905–909.
Stevanovic, D. (2011). Quality of Life Enjoyment and Satisfaction Questionnaire-short form for quality of life assessments in clinical practice: A psychometric study. Journal of Psychiatric and Mental Health Nursing, 18(8), 744–750. doi:10.1111/j.1365-2850.2011.01735.x.
Revicki, D. A., Brandenburg, N., Matza, L., Hornbrook, M. C., & Feeny, D. (2008). Health-related quality of life and utilities in primary-care patients with generalized anxiety disorder. Quality of Life Research, 17(10), 1285–1294. doi:10.1007/s11136-008-9406-6.
Mick, E., Faraone, S. V., Spencer, T., Zhang, H. F., & Biederman, J. (2008). Assessing the validity of the Quality of Life Enjoyment and Satisfaction Questionnaire Short Form in adults with ADHD. Journal of Attention Disorder, 11(4), 504–509. doi:10.1177/1087054707308468.
Müllerová, H., Libigerová, E., & Prouzová, M. (2001). Cross-cultural transfer and validation of the Quality of Life Enjoyment and Satisfaction Questionnaire in the population of depressed patients. PSYCHIATRIE-PRAHA, 5, 80–87.
Rossi, A., Rucci, P., Mauri, M., Maina, G., Pieraccini, F., Pallanti, S., et al. (2005). Validity and reliability of the Italian version of the Quality of Life, Enjoyment and Satisfaction Questionnaire. Quality of Life Research, 14(10), 2323–2328. doi:10.1007/s11136-005-7387-2.
Hope, M. L., Page, A. C., & Hooke, G. R. (2009). The value of adding the Quality of Life Enjoyment and Satisfaction Questionnaire to outcome assessments of psychiatric inpatients with mood and affective disorders. Quality of Life Research, 18(5), 647–655. doi:10.1007/s11136-009-9478-y.
Ritsner, M., Kurs, R., Kostizky, H., Ponizovsky, A., & Modai, I. (2002). Subjective quality of life in severely mentally ill patients: A comparison of two instruments. Quality of Life Research, 11(6), 553–561.
Zubaran, C., Foresti, K., Thorell, M. R., Franceschini, P. R., & Homero, W. (2009). Portuguese version of the Quality of Life Enjoyment and Satisfaction Questionnaire: A validation study. Revista Panamericana de Salud Publica, 25(5), 443–448.
Fayers, P. M., & Machin, D. (2007). Quality of life: The assessment, analysis and interpretation of patient-reported outcomes (2nd ed.). Chichester: Wiley.
Liu, S. I., Yeh, Z. T., Huang, H. C., Sun, F. J., Tjung, J. J., Hwang, L. C., et al. (2011). Validation of Patient Health Questionnaire for depression screening among primary care patients in Taiwan. Comprehensive Psychiatry, 52(1), 96–101. doi:10.1016/j.comppsych.2010.04.013.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56–62.
Zheng, Y. P., Zhao, J. P., Phillips, M., Liu, J. B., Cai, M. F., Sun, S. Q., et al. (1988). Validity and reliability of the Chinese Hamilton depression rating scale. British Journal of Psychiatry, 152, 660–664.
Ware, J. E, Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Fuh, J. L., Wang, S. J., Lu, S. R., Juang, K. D., & Lee, S. J. (2000). Psychometric evaluation of a Chinese (Taiwanese) version of the SF-36 health survey amongst middle-aged women from a rural community. Quality of Life Research, 9(6), 675–683.
Wing, J. K., Babor, T., Brugha, T., Burke, J., Cooper, J. E., Giel, R., et al. (1990). SCAN. Schedules for clinical assessment in neuropsychiatry. Archives of General Psychiatry, 47(6), 589–593.
Cheng, A. T., Tien, A. Y., Chang, C. J., Brugha, T. S., Cooper, J. E., Lee, C. S., et al. (2001). Cross-cultural implementation of a Chinese version of the schedules for clinical assessment in neuropsychiatry (SCAN) in Taiwan. British Journal of Psychiatry, 178, 567–572.
McHorney, C. A., & Tarlov, A. R. (1995). Individual-patient monitoring in clinical practice: are available health status surveys adequate? Quality of Life Research, 4(4), 293–307.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: L. Erlbaum Associates.
Thompson, B. (2004). Exploratory and confirmatory factor analysis: Understanding concepts and applications. Washington, DC: American Psychological Association.
Gorsuch, R. (1983). Factor Analysis (2nd ed.). Mahawah: Lawrence Erlbaum Associates.
Tabachnick, B., & Fidell, L. (1996). Using Multivariate Statistics (3rd ed.). New York: Harper Collins.
Hair, J. F., Anderson, R. E., Tatham, R. L., & Black, W. C. (1998). Multivariate Data Analysis (5th ed.). Upper Saddle River, NJ: Prentice-Hall.
Cohen, S., & Williamson, G. (1988). Perceived stress in a probability sample of the United States. The Social Psychology of Health: Charemont Symposium on Applied Social Psychology, Newbury Park, CA: Sage.
Nixon, S., & Parsons, O. (1989). Cloninger’s tridimensional theory of personality: Construct validity in a sample of college students. Personality and Individual Differences, 10, 1261–1267.
Lim, L. L., & Fisher, J. D. (1999). Use of the 12-item short-form (SF-12) Health Survey in an Australian heart and stroke population. Quality of Life Research, 8(1–2), 1–8.
Amir, M., Lewin-Epstein, N., Becker, G., & Buskila, D. (2002). Psychometric properties of the SF-12 (Hebrew version) in a primary care population in Israel. Medical Care, 40(10), 918–928. doi:10.1097/01.mlr.0000027359.33761.fa.
Sugar, C. A., Sturm, R., Lee, T. T., Sherbourne, C. D., Olshen, R. A., Wells, K. B., et al. (1998). Empirically defined health states for depression from the SF-12. Health Services Research, 33(4 Pt 1), 911–928.
Endicott, J., Nee, J., Yang, R., & Wohlberg, C. (2006). Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q): Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 45(4), 401–407. doi:10.1097/01.chi.0000198590.38325.81.
O’Connor, E. A., Whitlock, E. P., Beil, T. L., & Gaynes, B. N. (2009). Screening for depression in adult patients in primary care settings: A systematic evidence review. Annals of Internal Medicine, 151(11), 793–803. doi:10.1059/0003-4819-151-11-200912010-00007.
Liao, S. C., Chen, W. J., Lee, M. B., Lung, F. W., Lai, T. J., Liu, C. Y., et al. (2012). Low prevalence of major depressive disorder in Taiwanese adults: Possible explanations and implications. Psychological Medicine, 42(6), 1227–1237. doi:10.1017/S0033291711002364.
Hwu, H. G., Yeh, E. K., & Chang, L. Y. (1989). Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatrica Scandinavica, 79(2), 136–147.
Gau, S. S. F., Chong, M. Y., Chen, T. H. H., & Cheng, A. T. A. (2005). A 3-year panel study of mental disorders among adolescents in Taiwan. American Journal of Psychiatry, 162(7), 1344–1350. doi:10.1176/appi.ajp.162.7.1344.
Acknowledgments
This study was supported by a grant from the National Health Research Institute, Republic of China (NHRI-EX97-9706PI). We thank all participants for their participation in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, YT., Liu, SI., Huang, HC. et al. Validity and reliability of the Chinese version of the Short Form of Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-SF). Qual Life Res 23, 907–916 (2014). https://doi.org/10.1007/s11136-013-0528-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-013-0528-0