Abstract
Purpose
In the domain of mental health outcomes, increasing interest has been shown in complementing traditional symptom measures with measures of a patient’s quality of life. The objective of this study was to evaluate the value of including the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) in the routine assessment battery used at a psychiatric hospital.
Methods
The sample consisted of 1,276 consecutive inpatients treated at a private psychiatric hospital over a two-year period. Admission and discharge data were collected for the Q-LES-Q, the mental health subscales of the Medical Outcomes Short Form Questionnaire (SF-36), the Depression Anxiety Stress Scales, and the Health of the Nation Outcome Scale.
Results
Large patient improvements from admission to discharge were seen across all instruments (effect sizes from 0.8 to 1.5), including the Q-LES-Q (effect size 1.3). The Q-LES-Q correlated with existing symptom measures, and regression analyses revealed that quality of life predicted length of hospital stay even after symptoms of depression and anxiety were taken into account.
Conclusions
Although the Q-LES-Q was correlated with symptom measures already in use, it added to the ability to predict patient length of stay, and showed some divergence from measures of clinical outcomes. This pattern was seen despite intentionally restricting the sample to patients with mood and affective disorder diagnoses. The value of considering quality of life in a comprehensive assessment of mental health outcomes is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the past, the objective in medical research was to assess the status of physical health and functioning in patients. More recently, a greater emphasis has been placed on assessing and maintaining “quality of life”. The shift in focus has arisen because a cure is not always possible and patients must often come to terms with lasting lifestyle changes. A similar shift in reasoning has become apparent in the domain of mental health, as psychiatric settings look to patients for a consumer’s perspective of their experience to complement routine clinical assessments [1].
The quality of life literature has suffered from poor and contradictory conceptualisation [2–4], but a definition which has been broadly accepted is that proposed by the World Health Organisation’s Quality of Life (WHOQOL) working group: “quality of life… is an individual’s perception of their position in life, in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns…. [it incorporates] in a complex way individual’s physical health, psychological state, level of independence, social relationships, personal beliefs, and their relationships to salient features of the environment” [5] (p. 1,405). The core features of this definition are that quality of life offers a subjective, patient-centred focus (rather than an external clinical judgement), and that the concept is multidimensional (drawing on a number of domains besides physical and emotional wellbeing). In these ways quality of life assessment has been suggested to add important information that might be missed in traditional assessments of health functioning [1].
The relevance of this construct to psychiatric settings is underlined by research describing a consistently lower quality of life in individuals with a mental health diagnosis than those without [6–8]. In comparison with healthy community means, poorer subjective quality of life has been reported in individuals with schizophrenia spectrum disorders [9], depressive disorders [10], anxiety disorders [7], personality disorders [11], and substance use disorders [12]. In light of this, Ritsner [3] proposed that “quality of life impairment” should be considered an important syndrome in research and treatment of psychiatric disorders.
Despite the trend to complement mental health assessments with measures of quality of life, questions still remain about the value of adding quality of life measures to outcomes assessment in acute psychiatric hospital settings. A close relationship between symptom measures and subjective quality of life in psychiatric samples has been cited as evidence that quality of life measures add little value to understanding variables of interest to major stakeholders in psychiatric care [13]. The relationship between quality of life and symptoms of depression, in particular, has consistently been reported as strong [14–17]. As a result, some have suggested that to measure both quality of life and depressive symptomatology in a psychiatric population would be redundant [18].
It follows that if measures of quality of life and measures of symptoms (e.g., depression) assess identical or overlapping constructs, there may be little value to consumer or clinician in adding quality of life assessments to psychiatric outcome assessment batteries. This is particularly important to consider in acute hospital settings, where treatment focuses on the swift alleviation of symptomatic distress and the burden of completing lengthy assessment batteries with acutely unwell patients must be considered.
Fitzpatrick and colleagues [19] suggested for a quality of life assessment to be useful in a clinical setting, the instrument chosen must be appropriate in length and practical to apply in routine care, yet retain good measurement properties (such as construct validity and sensitivity to change in the period of concern). As mood state and subjective wellbeing are considered just two components of quality of life [2], the need for agreement with measures of clinical symptomatology, but not redundancy, was also highlighted [20]. In addition, Basu suggested that quality of life measures might be utilized to predict other outcomes of interest to psychiatric care [1]. As well as changes in clinical symptoms, the Australian National Mental Health Strategy suggested that proxy indicators of effectiveness (reduced numbers of re-admissions to hospital within 28 days) and efficiency (average length of acute inpatient stay) were also of interest in this setting [21].
Therefore, this study investigated the value of adding the short form of the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q; [14]) to outcomes assessment at a private psychiatric hospital. The value of the Q-LES-Q in this setting was evaluated by examining:
-
1.
the measure’s sensitivity to change from admission to discharge;
-
2.
the nature of relationships with other measures in use at the hospital; and
-
3.
the incremental ability to predict variables of interest to stakeholders (namely patient clinical outcomes, length of stay, and readmission within one month).
Method
Participants
The potential sample comprised 3,434 consecutive inpatient admissions treated at Perth Clinic (a 100 bed Australian private psychiatric clinic) over a two-year period. Because many admissions were brief (e.g., a one-day admission for ECT) the admission and discharge data relevant to this study were only available on a portion of the sample. Only those patients who had completed the Q-LES-Q as part of their routine hospital assessment at both admission and discharge were retained (N = 1,884). There were no significant differences between responders and non-responders in age (t (3,432) = 1.32, P = .17) or symptom severity (t (2,803) = 1.91, P = .06) at admission. However, the proportion of males in the non-response group (31%) was marginally higher than that of the response group (27%; χ 2(1, N = 3,434) = 5.21, P < .05). This trend suggests that males were less likely to participate in the study than females. Patients less inclined to respond were also those with a shorter length of stay (responders: M = 15.0 days, CI95% = 14.6–15.5; non-responders: M = 13.2 days, CI95% = 12.6–13.7) and had on average twice as many admissions as those who did respond (responders: M = 9.5, CI95% = 8.8–10.3; non-responders: M = 15.8, CI95% = 13.9–17.6). As the two groups did not differ in severity of illness, these differences might reflect a disinclination to complete the questionnaires following a brief hospital stay or in a series of admissions.
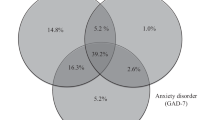
The retained sample consisted predominantly of patients who met diagnostic criteria for mood or affective disorders (68%), but also included patients admitted for treatment of an anxiety disorder (18%), substance use (6%), or schizophrenia (5%). To provide the most stringent picture of the incremental validity of the quality of life measure (given the strong relationship between affective symptoms and self-reported quality of life), the sample was restricted to only those patients with a mood or affective disorder diagnosis (N = 1,276). The socio-demographic characteristics of the final sample are shown in Table 1.
Each patient was admitted and discharged on the clinical judgement of their treating psychiatrist, who was also responsible for determining diagnosis at admission based on ICD-10-AM criteria [22]. The breakdown of primary diagnoses is outlined in Table 2. Most of the sample were assessed to be severely (50.9%) or mild-moderately (24.3%) depressed at the time of admission.
Admission and discharge questionnaires were administered within 24 h of each by ward nursing staff, whilst psychotherapeutic interventions were provided by a separate team of therapy staff (explained further below). Questionnaires administered were part of the routine admission and discharge procedures for the hospital, but written informed consent for use of the data was obtained from all patients upon admission. The research was also approved under National Health and Medical Research Council ethics guidelines. Hospital fees were covered to different extents by patients’ private health funds (22 funds were represented).
Treatment approaches
Virtually all inpatients admitted to the hospital undertake pharmacological treatment, which is prescribed or reviewed by their treating psychiatrist on admission, and monitored throughout their stay. A smaller proportion (roughly 13%) also undergo electroconvulsive therapy whilst an inpatient.
In accordance with hospital policy, all patients in the study were encouraged to participate in group psychotherapy programmes to complement their ongoing psychiatric care. Therapy streams at Perth Clinic accommodate a range of patient functioning and needs by offering a variety of treatment approaches, including cognitive behavioural therapy, interpersonal therapy, structured activity-based therapy, and relaxation and stress-management instruction. The therapy team includes clinical and counselling psychologists, occupational therapists, social workers, family therapists, and counsellors. Patients are allocated to therapy streams based on the recommendations of their treating psychiatrist, but these differences were not a focus of our analyses.
Measures
The Medical Outcomes Short Form Questionnaire (SF-36) is a patient self-report measure of health status that has been used widely across different patient groups and diagnostic categories [23]. Perth Clinic uses the four subscales which address mental health outcomes, consisting of 14 items assessing vitality, role functioning, social functioning, and mental psychological distress (over the past few days). Previous research has validated the use of the mental health subscales in psychiatric care [24]. As the Social and Role Functioning domain scores are determined by single items, our analyses involved only the Mental Health and Vitality subscales. Internal consistency has been reported as good (Cronbach’s α greater than 0.8) for both subscales [25], and the SF-36 has been shown to demonstrate good construct validity [23].
The 21-item shortened form of the Depression Anxiety Stress Scales (DASS; [26]) assesses levels of depression, anxiety and stress experienced over the past week. Responses are rated on a five-point scale, and high scores indicate more severe psychopathology. The internal consistency has been reported as high (Cronbach’s α = .97), and the construct validity as sound [26, 27]. While the subscale scores are considered individually for most analyses reported here, a combined DASS score was also used as a gauge of patient clinical outcome at discharge (derived by summing the scores of all three subscales, as suggested by the authors of the scale [26]).
The Health of the Nation Outcome Scale (HoNOS; [28]) is a clinician-rated scale which assesses patient functioning over the past two weeks in 12 domains. It is sensitive to change [29], and demonstrates good construct validity [28] and moderate internal consistency (a product of the diverse range of the scale items [30]). Staff received regular training in administering the HoNOS during the study period to ensure inter-rater reliability.
The Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q; [14]) is a self-report measure designed to assess the degree of enjoyment and satisfaction experienced in daily functioning by individuals over the past week. The General Activities section of the Q-LES-Q is suggested by the developers of the scale to be an appropriate short form of the instrument, and was adopted here as more practical for routine application. The short form consists of 14 items, assessing satisfaction in the domains of: physical health; mood; work; household activities; social and family relationships; leisure activities; daily functioning; sexual drive and interest; economic status; living situation; physical stability; vision; and overall sense of wellbeing. There are two additional items (satisfaction with medication and overall satisfaction) which are not included in the scoring. Each item is rated on a scale of 1–5, and an individual’s score is determined as a percentage of the maximum possible score of 70 (where a higher score represents a better perceived quality of life). The internal consistency of the short form has been reported as high (Cronbach’s α = 0.89–0.95) with good construct validity [7, 31].
Design and statistical analyses
A repeated measures design allowed patient outcomes and instrument sensitivity to be examined. All measures listed above were routinely administered at admission and discharge from the hospital. Mean length of stay for the sample (and hence mean time between test and retest) was 15.62 days (SD = 9.77). Mean improvements between admission and discharge were evaluated by calculating effect size (where ES = discharge mean−admission mean)/admission standard deviation). It is recommended to interpret effect sizes of 0.4–0.8 as moderate, and those over 0.8 as large [32].
The relationships between measures at admission and discharge were examined through correlation and multiple regression analyses.
Multiple regression analyses were used to predict patient outcomes (as measured by the DASS composite score at discharge), length of stay, and number of days to readmission. The criterion variables were inspected for normality of distributions. The distribution of the composite DASS score was improved by a square-root transformation and length of hospital stay by a logarithmic transformation.
Given the large number of comparisons, a criterion value of P < .01 was taken as significant.
Results
Sensitivity to change
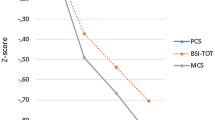
Table 3 shows mean scores for all assessment measures at admission to and discharge from the hospital. Moderate to large patient improvements from admission to discharge were seen across all instruments [32]. This confirms that even in the relatively short period of an acute inpatient admission, improvements are evident in both symptomatology and subjective quality of life. Scores on the Q-LES-Q showed a 1.31 standard deviation improvement, which was considered a large effect size [32], and comparable in magnitude with improvements in symptom measures.
Relationship with other measures
The relationships between the Q-LES-Q and other measures in the hospital’s assessment battery were examined via correlation analyses (Table 4). Unsurprisingly, scores on the Q-LES-Q appear to be closely related to clinical measures over the same period. At admission, correlations with the Q-LES-Q ranged from −.22 (with the HoNOS) to −.58 (with the depression subscale of the DASS). At discharge the Mental Health (r = .74) and Vitality (r = .73) subscales of the SF-36 demonstrated the strongest relationship with the Q-LES-Q (note that the direction of this correlation is reflective of the positive scoring of both the Q-LES-Q and the SF-36). All relationships between the Q-LES-Q and symptom measures increased in magnitude from admission to discharge.
The comparatively weaker relationship between the HoNOS scale and other measures has been reported elsewhere, and can be attributed to the restricted range of the HoNOS scale [29].
Predictive ability
Multiple regression analyses were conducted to determine the ability of the various measures to predict outcomes of interest: patient outcomes at discharge; length of stay in hospital; and number of days to next readmission. Incremental predictive ability was compared across three sets of predictors:
-
1.
demographic information (patient gender, age at admission, marital status, and socio-economic status);
-
2.
symptom-based assessment measures (DASS Depression, Anxiety and Stress subscales; the SF-36 Mental Health and Vitality subscales; and total HoNOS score); and
-
3.
the Q-LES-Q scores (admission and discharge).
A summary of the analyses is presented in Table 5.
Patient outcomes at discharge
Preliminary regression analysis suggested that all three sets of predictors combined could account 20% of the variance in patient outcome at discharge.
Stepwise regression analysis was used to examine the incremental predictive ability of each set of variables. Demographic information accounted for 3.4% of the variance in discharge outcome, and the inclusion of symptom measures accounted for an additional 16.2% of variance in discharge outcome. The inclusion of the Q-LES-Q scores added no statistical value to this model.
Length of stay
The same three sets of predictors were applied to predicting length of stay. A small but significant amount of variance in length of stay (7%) was accounted for by the combined regression model.
A stepwise analysis was conducted to evaluate incremental predictive ability. All three sets of predictors yielded significant regression equations. Demographic information alone accounted for 1.2% of the variance in length of stay, while the inclusion of symptom measures accounted for an additional 4.2% of the variance.
The addition of Q-LES-Q data accounted for a further 1.6% of variance in length of stay. This was significant even after taking into account the contribution made by demographic information and all symptom measures at admission and at discharge.
Readmission
The ability to predict the number of days passing before readmission to the hospital was explored in the same manner. The inclusion of all three sets of predictors yielded poor and non-significant predictive ability (R 2 = −.01, P = 0.58), and so the incremental validity of each set was not explored.
Discussion
Analyses revealed that all of the outcome measures used were sensitive to change and showed large improvements in the sample during the relatively short period from admission to discharge. Therefore in comparison with the other measures reported here, the short form of the Q-LES-Q demonstrated appropriate sensitivity to change. In a quality-assurance sense, the improvements reported here are important information for a psychiatric service provider, in that large change can be effected over a brief admission in both symptomatology and quality of life (despite, perhaps, the latter not being the overt focus of treatment).
The results imply that improvements in Q-LES-Q scores are associated with a reduction in depressive symptoms (as measured by the DASS) and improvements in overall mental health and vitality (as measured by the SF-36), but are not equivalent to them. That is, despite the stringent test provided by the restricted sample, the Q-LES-Q scores appear to provide additional information to that currently being captured by the hospital’s measures.
The increase in the strength of the relationships between symptom measures and the Q-LES-Q from admission to discharge might be related to the patients’ change in context. Quality of life judgments might be mediated by a greater number of variables at admission (when the patient considers their functioning over the past two weeks within their normal home, work, and relationship environments) than at discharge (when their frame of reference is a structured hospital environment with a daily focus on symptomatology). It might therefore be expected that quality of life reports will mirror symptom measures more closely at discharge from an acute hospital stay.
One possibility considered was that satisfaction with the hospital stay might be a mediator of these converging scores. We had available a dataset of patients (N = 280) for exploration of this possibility who had filled out satisfaction with the treatment they had received at the hospital (Page, manuscript in preparation). There was no relationship with satisfaction ratings and admission measures of quality of life or symptomatology, and only a weak relationship between satisfaction ratings and these measures at discharge. When satisfaction was partialled out of correlation analyses, the relationships seen at admission and at discharge between quality of life and symptoms remained unchanged. These data suggest that there is a weak relationship between satisfaction with the hospital stay and quality of life, and a weak relationship between satisfaction with the hospital stay and symptoms, but this is independent of the relationship between quality of life and symptoms. We acknowledge that this cannot completely eliminate the possibility satisfaction is a mediator, but we would suggest future research might explore this more broadly.
Scores on the Q-LES-Q did not add to the ability to predict clinical outcomes. Not surprisingly, the greatest predictor of psychological symptoms at discharge was the same construct being measured at admission to the hospital.
A small but significant contribution of quality of life to predicting length of stay was seen. Although this was a small effect, it must be considered that this is separate and additional variance to what could be explained by a range of other outcome measures and demographic characteristics combined. The relationship might reflect that a poor evaluation of quality of life is associated with an increase in anxiety as the possibility of discharge approaches (related to a patient’s negative appraisal of their own ability to function in day-to-day life). This could reduce a patient’s perceived readiness for discharge, potentially extending their length of stay. If this is true there may in future be a role for applying the information captured by the Q-LES-Q at a more individualised, clinical level. The content of the scale has potential for informing treatment and discharge planning, and may facilitate suitable referrals for support within the community or identify areas of concern for the patient which could be increasing anxiety levels and delaying their discharge. As this was not the focus of the study reported here, this would warrant exploration in future research.
None of the outcome measures accurately predicted readmission. Despite being an outcome of interest noted by the Australian National Mental Health Working Group [21], readmission is notoriously difficult to predict. This has been suggested to be a product of the wide range of variables that might influence readmission (including community support issues, severity or chronicity of disorder, and clinician or hospital admission policies [33]).
The generalisations that can be made from the current dataset need to be considered in terms of the strengths and limitations of the study. One limitation was the naturalistic, hospital-based context used for data collection. This context meant that variables such as medications received, range of psychotherapy groups attended, and previous psychiatric history were not controlled for. Hence, some internal validity was sacrificed to ensure greater ecological validity in appraisal of the value of the Q-LES-Q for use in this specific setting. Another limitation is the difference between some characteristics of the retained sample and those of the non-responders. Patients who did not complete the assessment measures were more likely to be male, have had only a brief stay at the hospital, or be in a series of admissions. Thus care needs to be taken when generalising to these groups. However, the large sample of clinical data presented here and the comparisons allowed by the longitudinal design of the study offer valuable information for stakeholders in psychiatric care.
This study has reinforced previous findings that considerable impairments in quality of life are associated with acute presentations of mental illness [34, 35]. Encouraging, however, is the demonstration that large improvements in quality of life can be effected over the relatively short period of a psychiatric admission. The Q-LES-Q was appropriately sensitive to change within this timeframe, but its ability to contribute to predicting outcomes of interest had minimal implications for service delivery. A convergence in the relationship between symptom measures and the Q-LES-Q might reflect the narrowing of appraisal context seen within an inpatient stay. What remains now is to explore how best to integrate this information into an acute inpatient model of care.
References
Basu, D. (2004). Quality of life issues in mental health care: Past, present and future. German Journal of Psychiatry, 7, 35–43.
Camfield, L., & Skevington, S. M. (2008). On subjective well-being and quality of life. Journal of Health Psychology, 13, 764–775. doi:10.1177/1359105308093860.
Ritsner, M. (2007). The distress/protection vulnerability model of quality of life impairment syndrome. In M. Ritsner & A. G. Awad (Eds.), Quality of life impairment in schizophrenia, mood and anxiety disorders: New perspectives on research and treatment. Dordrecht, The Netherlands: Springer.
Rapley, M. (2003). Quality of life research: A critical introduction. London: SAGE Publications.
The WHOQOL Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science and Medicine, 41(10), 1403–1409. doi:10.1016/0277-9536(95)00112-K.
Masthoff, E. D., et al. (2006). Quality of life and psychopathology: Investigations into their relationship. The Australian and New Zealand Journal of Psychiatry, 40, 333–340. doi:10.1111/j.1440-1614.2006.01799.x.
Rapaport, M. H., et al. (2005). Quality of life impairment in depressive and anxiety disorders. The American Journal of Psychiatry, 162, 1171–1178. doi:10.1176/appi.ajp.162.6.1171.
Evans, S., et al. (2006). The impact of mental illness on quality of life: A comparison of severe mental illness, common mental disorder and healthy population samples. Quality of Life Research, 16, 17–29. doi:10.1007/s11136-006-9002-6.
Ritsner, M., & Gibel, A. (2007). Quality of life impairment syndrome in schizophrenia. In M. S. Ritsner & A. G. Awad (Eds.), Quality of life impairment in schizophrenia, mood and anxiety disorders: New perspectives on research and treatment. Springer: Dordrecht: The Netherlands.
Trompenaars, F. J., et al. (2006). Relationship between mood related disorders and quality of life in a population of Dutch adult psychiatric outpatients. Depression and Anxiety, 23, 353–363. doi:10.1002/da.20180.
Cramer, V., Torgersen, S., & Kringlen, E. (2007). Socio-demographic conditions, subjective somatic health, axis I disorders and personality disorders in the common population: The relationship to quality of life. Journal of Personality Disorders, 21, 552–567. doi:10.1521/pedi.2007.21.5.552.
Connor, J. P., Saunders, J. B., & Feeney, G. F. X. (2006). Quality of life in substance use disorders. In H. Katschnig, H. Freeman, & N. Sartorius (Eds.), Quality of life in mental disorders (pp. 199–208). Chichester: Wiley.
Katschnig, H. (1997). How useful is the concept of quality of life in psychiatry? In H. Katschnig, H. Freeman, & N. Sartorius (Eds.), Quality of life in mental disorders. Chichester: Wiley.
Endicott, J., et al. (1993). Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacology Bulletin, 29, 321–326.
Goldberg, J. F., & Harrow, M. (2005). Subjective life satisfaction and objective functional outcome in bipolar and unipolar mood disorders: A longitudinal analysis. Journal of Affective Disorders, 89, 79–89. doi:10.1016/j.jad.2005.08.008.
Herrman, H., et al. (2002). Longitudinal investigation of depression outcomes in primary care in six countries: The LIDO study. Functional status, health service use and treatment of people with depressive symptoms. Psychological Medicine, 32, 889–902. doi:10.1017/S003329170200586X.
Holloway, F., & Carson, J. (2002). Quality of life in severe mental illness. International Review of Psychiatry (Abingdon, UK), 14, 175–184. doi:10.1080/09540260220145000.
Katschnig, H., & Angermeyer, M. C. (1997). Quality of life in depression. In H. Katschnig, H. Freeman, H. Katschnig, H. Freeman, & N. Sartorius (Eds.), Quality of life in mental disorders. Chichester: Wiley.
Fitzpatrick, R., et al. (1992). Quality of life measures in health care: I. Applications and issues in assessment. British Medical Journal, 305, 1074–1077.
Fletcher, A., et al. (1992). Quality of life measures in health care: II. Design, analysis and interpretation. British Medical Journal, 305, 1145–1148.
Australian Health Ministers. (1992). National mental health policy. Canberra: Commonwealth Department of Human Services and Health.
National Centre for Classification in Health Publications. (2002). The international statistical classification of diseases and related health problems, tenth revision, Australian modification (ICD-10-AM) (3rd ed.). Geneva: National Centre for Classification in Health Publications.
Ware, J. E., et al. (1993). SF-36 health survey: Manual and interpretation guide. Boston: The Health Institute, New England Medical Center.
Newnham, E. A., Harwood, K. E., & Page, A. C. (2007). Evaluating the clinical significance of responses by psychiatric inpatients to the mental health subscales of the SF-36. Journal of Affective Disorders, 98, 91–97. doi:10.1016/j.jad.2006.07.001.
Scott, K. M., et al. (1991). SF-36 health survey reliability, validity and norms for New Zealand. Australian and New Zealand Journal of Public Health, 23, 401–406. doi:10.1111/j.1467-842X.1999.tb01282.x.
Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd ed.). Sydney: Psychology Foundation.
Crawford, J. R., & Henry, J. D. (2003). The depression anxiety stress scales (DASS): Normative data and latent structure in a large non-clinical sample. The British Journal of Clinical Psychology, 42, 111–131. doi:10.1348/014466503321903544.
Wing, J. K., et al. (1998). Health of the nation outcomes scales (HoNOS): Research and development. The British Journal of Psychiatry, 172, 11–18. doi:10.1192/bjp.172.1.11.
Page, A. C., Hooke, G. R., & Rutherford, E. M. (2001). Measuring mental health outcomes in a private psychiatric clinic: Health of the nation outcome scales and medical outcomes short form SF-36. The Australian and New Zealand Journal of Psychiatry, 35, 377–381. doi:10.1046/j.1440-1614.2001.00908.x.
Trauer, T. (1999). The subscale structure of the health of the nation outcome scales. Journal of Mental Health, 8(5), 499–509. doi:10.1080/09638239917193.
Ritsner, M., et al. (2002). Subjective quality of life in severely mentally ill patients: A comparison of two instruments. Quality of Life Research, 11, 553–561. doi:10.1023/A:1016323009671.
Kazis, L. E., Anderson, J. J., & Meenan, R. F. (1989). Effect sizes for interpreting changes in health status. Medical Care, 27(3, suppl), S178–S189. doi:10.1097/00005650-198903001-00015.
Lyons, J., et al. (1997). Predicting readmission to the psychiatric hospital in a managed care environment: implications for quality indicators. The American Journal of Psychiatry, 154, 337–340.
Ritsner, M. (2003). Predicting changes in domain-specific quality of life in major psychoses: A naturalistic follow-up study. The Journal of Nervous and Mental Disease, 191, 287–294. doi:10.1097/00005053-200305000-00003.
Russo, J., et al. (1997). Longitudinal assessment of quality of life in acute psychiatric inpatients: Reliability and validity. The Journal of Nervous and Mental Disease, 185(3), 166–175. doi:10.1097/00005053-199703000-00006.
Acknowledgments
The authors would like to thank Moira Munro and the staff at Perth Clinic for their ongoing support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hope, M.L., Page, A.C. & Hooke, G.R. The value of adding the Quality of Life Enjoyment and Satisfaction Questionnaire to outcome assessments of psychiatric inpatients with mood and affective disorders. Qual Life Res 18, 647–655 (2009). https://doi.org/10.1007/s11136-009-9478-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-009-9478-y