Abstract
Objective
The purpose of this study was to investigate the effects of water exercise at a day service facility and the effects of water exercise frequency on health-related quality of life (HRQL).
Methods
Participants (n = 30) were randomly separated into three groups: two indicating exercise frequency, at once-weekly or twice-weekly, and a control group. One-hour exercise intervention sessions were carried out once or twice a week, accordingly, for 24 weeks. The water exercise session comprised a warm-up on land, activities of daily living (ADL) exercises, stretching, strength training, and relaxation in water. HRQL was evaluated using the Medical Outcomes Survey Short-Form 36 (SF-36) questionnaire, and ADL disability was assessed using the Functional Independence Measure.
Results
Significant differences were found between pre- and 6 months in both the once- and twice-weekly groups in HRQL (p < 0.05). No significant difference was found among pre-, 3 months, and 6 months. The effect size between the once and twice groups was moderate in both the physical component summary (0.72) and mental component summary (0.75) at 3 months. ADL disability shows significant correlation with HRQL.
Conclusion
Water exercise intervention at a day service facility improved participants’ HRQL for 6 months by improving exercise habits and ADL disability. Furthermore, the HRQL change differed according to exercise frequency: twice-weekly exercise showed more rapid improvement than once-weekly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elderly people receiving nursing care are reportedly more likely to exhibit decreased or compromised body function and structure, activity, participation, and health-related quality of life (HRQL) than those without nursing care [1,2]. The amount of decline in activities of daily living (ADL) ability was different among the specific activities. Lower extremity activities, such as mobility (locomotion), transfer, and going up and down stairs, significantly decreased earlier than upper extremity activities, such as eating, grooming and dressing [3]. It has been reported that exercise intervention slows the decrease in HRQL, but positive effects are not apparent in subjects with high levels of nursing care; such as eating, grooming and dressing [4]. Therefore, it is important to prevent increasing levels of nursing care for elderly people who still only require a low level of care; such as mobility (locomotion), transfer, and going up and down stairs. In Japan, various approaches have been undertaken to prevent the increasing level of nursing care and to reduce the number of persons receiving nursing care within the public nursing-care insurance system (PNCIS), which is the first and only system in the world for helping elderly people lead an independent life [5]. Almost all elderly people receiving a low level of nursing care use day service facilities through PNCIS; for that reason, it is beneficial to suggest various approaches to improve and maintain HRQL in day service facilities.
Exercise improves and maintains HRQL. Resistance exercise and balance exercise supported by PNCIS reportedly lead to improvement in HRQL [6, 7]. Unfortunately, physical activity increases the possibilities for falling. The perceived risk of falling is a widely recognized barrier to exercise [8, 9]. Additionally, elderly people who require nursing care are limited to available exercise programs which consider safety and effectiveness; therefore, it is important to carefully select the type of exercise they do. Water is a supportive, low-risk exercise environment that might reduce the likelihood of acute injury and fear of falling, and which might therefore improve participation and adherence to an exercise program [10, 11]. Therefore, the water environment is beneficial to elderly people who require a low level of nursing care, such as individuals who are frail, who suffer from pain, who are severely kyphotic, or who have poor balance [12].
Previous studies have elucidated the influences of water exercise on HRQL in women over 65 years of age [13], patients with chronic obstructive pulmonary disease [14] and those with fibromyalgia [15], although no studies have examined elderly people receiving nursing care. HRQL is related to body function and structure, activity, and participation [16, 17]. Results from our previous study clarified that participating in water exercise at a day service facility helps frail elderly people who require a low level of nursing care to foster exercise habits and improve ADL disability and lower muscle strength [18]. Additionally, the greater benefit of exercise for elderly people was observed in mental components rather than physical components in the Medical Outcomes Survey Short-Form 36 (SF-36) [19]. Consequently, it is expected that water exercise would improve HRQL in elderly people receiving a low level of nursing care.
To plan an optimally beneficial water exercise prescription, it is necessary to examine the effects of the program, term, frequency, and intensity of water exercise. Previous studies have reported improvement in HRQL by water exercise, irrespective of the exercise frequency: once a week for 6 months [15], or twice [13] or three times [14] a week for 3 months. However, no previous research investigated the effects of different frequencies of water exercise on HRQL among frail elderly people who require nursing care. Results from our previous study clarified that among frail elderly requiring a low level of nursing care who participated in water exercise once a week, ADL disability took 6 months to show improvement, although water exercise twice a week at a day service facility improved ADL disability for 3 months and subsequently plateaued after that [18]. HRQL is related to ADL disability [16]. Therefore, HRQL changes might differ according to exercise frequency. Within PNCIS, the level of nursing care determines the amount of the received service. Accordingly, it is important to examine the effects of water exercise frequency on HRQL.
The present study was intended to investigate the effect of water exercise within PNCIS and how water exercise frequency affected the change in HRQL among frail elderly people receiving a low level of nursing care. We hypothesized that among frail elderly people receiving a low level of nursing care, water exercise twice a week would elicit rapid improvement in HRQL at 3 months and subsequently plateau after that, as in our previous study of ADL disability [18], with less dramatic gains from exercise once a week.
Methods
Design
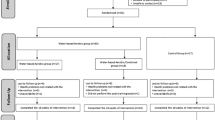
This was a single-blind, randomized pilot study with study enrollment carried out between September 2004 and July 2005. The Ethical Committee of the University of Tsukuba in Japan approved this study. Informed consent was obtained from all participants.
Participants
Participants who were frail elderly persons receiving nursing care and who used day services within PNCIS were recruited through informational talks. They lived in the central and southern area of Ibaraki prefecture. Participants were enrolled after an assessment screening for eligibility criteria as follows: (a) help with daily living is necessary according to certification requirements for receiving long-term care; (b) aged 65 years or more; (c) no cognitive impairment precluding understanding of the written informed consent; (d) no regular exercise outside of this study; (e) no cardiopulmonary or mental disease or orthopedic disorder; (f) no wheelchair use; (g) no recent hospitalization (within 6 months); (h) permission of water exercise participation by their doctor; (i) postmenopausal; (j) in retirement and living on a pension; (k) first use of this day-service facility; (l) performing, with nursing assistance, at least one of five mobility-related ADL tasks before starting water exercise intervention: transfer (to chair and bed), toilet transfer, bathing transfer, mobility (locomotion), and stair climbing; and (m) does not require nursing care to perform any functions other than mobility-related ADL tasks. ADL disability was evaluated using the Functional Independence Measure (FIM) [20]. Each item is scored using 1–7 points: 1 for total assistance; 2 for maximal assistance; 3 for moderate assistance; 4 for minimal assistance; 5 for supervision or prior preparation; 6 for modified independence; or 7 for complete independence.
All eligible participants were randomly assigned to either the once-weekly or twice-weekly intervention group or the control group, thus indicating their exercise frequency during the study. The group distribution was carried out by the nursing care manager, who was unrelated to this intervention study.
Intervention
The water exercise program was conducted at the indoor pool in a day service facility, which had a water depth of 1.05–1.15 m, water temperature of 33°C, and ambient temperature of 30°C. Each exercise session was supervised by at least two experienced instructors who belonged to a private swimming school, one clinical nurse, and three caregivers from the day service facility. Before each exercise session, the clinical nurse measured the heart rate, blood pressure, and body temperature of each participant.
Exercise sessions were divided into a 10-min warm-up consisting of flexibility exercise on land and 50 min of exercise in water. The 50-min water exercise program consisted of 20 min of walking, 10 min of ADL exercise, 10 min of stretching and strength, and 10 min of relaxation in water. The ADL exercise was aimed at improving and maintaining ADL disability, especially functional mobility including transfer, bathing transfer, toilet transfer, mobility, and stair climbing [18]. Participants performed functional mobility in the water. Exercise intensities of both programs were set at 11 on a rating of perceived exertion (RPE) scale [21].
All participants used the day services. The once and twice groups participated in the water exercise for 1 h once-weekly and twice-weekly, respectively. Participants in the control group instead spent time at lunch, bathing, watching TV, communicating with each other and in recreation. These programs were designed to provide attention and social interaction, and were designed as a ‘placebo’ intervention.
Measurement
Health-related quality of life and ADL disability were measured before the exercise intervention began (pre) and after 3 and 6 months.
Health-related quality of life
The Medical Outcomes Survey SF-36 questionnaire was administered to assess HRQL over the preceding 4 weeks [22]. The SF-36 questionnaire in Japanese was used in this study [22]. The SF-36 is a widely used, reliable, and valid criterion measure of HRQL in numerous populations [23, 24]. The SF-36 questionnaire has 36 questions that are scored to measure eight domains of HRQL pertaining to both physical and mental health (MH). The domains of physical functioning (PF), role limitations due to physical health (RP), bodily pain (BP), and general health (GH) comprise the physical component summary (PCS) of HRQL, while the domains of vitality (VT), social functioning (SF), role limitations due to emotional health (RE), and MH comprise the mental component summary (MCS) of HRQL. Each domain was scored using a scale of 0–100. The higher scores indicate higher HRQL than lower scores. The internal consistency of SF-36 is good, with Cronbach’s alpha of 0.76–0.90 for all domains of the questionnaire [25].
Activities of daily living disability
Activities of daily living disability was evaluated using the FIM [20]. A clinical nurse working full-time at the day-service facility evaluated the FIM. The FIM consists of 18 basic ADL items. Each item is scored using 1–7 points. ADL disability in this study was represented using a sum score of transfer, toilet transfer, bathing transfer, mobility, and stair climbing items. Table 1 shows the relationship between the FIM score and ADL disability. The reliability and validity of the FIM are reported in previous studies [26, 27].
Exercise intensity
Exercise intensity was evaluated using Borg’s RPE scale after each exercise session [20]. Borg’s scale in Japanese was used in this study [28]. It ranges from 6 to 20: from “very, very light” to “very, very hard” exercise intensity. The higher scores indicate higher exercise intensity than lower scores. The score was correlated with heart rate and other physiological variables [29].
Statistical analysis
The data were presented as mean ± standard deviation (SD) and analyzed using computer software (SPSS v.14; SPSS Inc.).
The FIM score was treated as non-parametric data because of the ordinal scale. Other data were treated as parametric data when the data were similar to normal distribution, and as non-parametric data when the data were significantly different from normal distribution. Baseline values were compared among groups with one-way ANOVA for parametric data or the Kruskal–Wallis test for non-parametric data.
Differences within groups were analyzed statistically using the Freedman test and post hoc test, with Wilcoxon’s sign rank test and Bonferroni’s inequality for non-parametric data. Statistical significance was inferred for p < 0.0167 because of the comparison of three combinations in the post hoc test. Differences among the three groups were analyzed statistically using the Kruskal–Wallis test and post hoc test, with the Steel–Dwass test for non-parametric data.
For parametric data, a group × time (3 × 3) repeated measures ANOVA was used to analyze the significance of changes with time among all groups, and Tukey’s post hoc test was used.
Spearman’s correlations were used to examine the relationship between HRQL (SF-36 score) and ADL disability (FIM score). Statistical significance was inferred for p < 0.05.
Effect size (ES) was calculated in order to examine the size of the observed effects according to water exercise frequency. The ES between the once group and twice group was determined as follows:
ES = (Δtwice group - Δonce group)/pooled SD
ES of 0.2, 0.5, and 0.8 were considered respectively as small, moderate, and large [30].
Power analyses performed a priori indicated that 12 total participants would be needed to detect an ES of 0.7, with alpha set at 0.05 and beta at 0.20.
Results
Recruitment and participant characteristics
Eighty-one participants volunteered to participate in this study, and of those, 51 did not meet the eligibility criteria. Therefore, 30 eligible participants were randomly assigned to either one of the intervention groups, the once group (n = 10) or the twice group (n = 12), or the control group (n = 8). One participant from the twice group did not complete the intervention because of reclassification as independent. Elderly who are classified as independent cannot receive any services through PNCIS [4]. The final participants for this study included 10 in the once group, 11 in the twice group, and 8 in the control group. No significant differences were found among the three groups in measured characteristics at baseline. The baseline characteristics of the participants are presented in Table 1.
Exercise attendance rate and exercise intensity
Attendance rates were 95.0 ± 4.7% and 95.3 ± 5.8% in the once and twice groups, respectively, which were not significantly different. The RPE were 11.1 ± 0.3 and 10.9 ± 0.5 in the once and twice groups, respectively, which were not significantly different.
Health-related quality of life
Differences within and among groups in PCS and MCS are presented in Table 2 and Fig. 1. PCS and MCS significantly increased at 3 and 6 months compared to pre, in the once and twice groups (p < 0.05). Significant increments of PCS and MCS were found between 3 and 6 months only in the once group (p < 0.05). PCS in the twice group was significantly higher than in the once and control groups at 3 months (p < 0.05), but was similar in the once group at 6 months. MCS in the twice group was significantly higher than the control group at 3 months (p < 0.05), and there was no significant difference compared to the once group. The ES between once and twice groups were moderate for PCS (0.72) and MCS (0.75) at 3 months, and small (−0.27 and −0.27) at 6 months.
Table 3 presents the eight domains of the SF-36 at baseline, 3 and 6 months. Significant differences in RP, BP, GH, VT, RE between pre and 6 months were found in both the once and twice groups (p < 0.05). On the other hand, no significant difference was found among pre, 3 and 6 months for PF in the once and twice groups. In the control group, significant decrements were found between pre and 3 months for PF, and pre and 6 months for RP and VT. No significant difference was found among pre, 3 and 6 months in other domains in the control group. Significant differences between the once and twice groups were seen for RP, GH and RE at 3 months (p < 0.05), but not at 6 months. The negative ES of RP, BP, GH, VT, SF, and RE between the once and twice groups were small at 6 months.
ADL disability
Differences within and among groups in FIM score are presented in Table 4. Significant differences in FIM score were found between pre and 6 months for both the once and twice groups (p = 0.004, 0.002), and between pre and 3 months only in the twice group (p = 0.002). No significant difference was found between pre, 3 and 6 months in the control group.
Correlation between HRQL and ADL disability
Table 5 shows the relationship between HRQL and ADL disability for all data. ADL disability has a significant correlation with PCS (r = 0.452, p < 0.05) and MCS (r = 0.383, p < 0.05).
Discussion
This study clarified the effects of water exercise at a day service facility on HRQL in elderly people receiving a low level of nursing care, and how water exercise frequency affected the change in HRQL. This is the first study to investigate the effects of water exercise on HRQL in frail elderly people. The findings reached in this study are applicable to water exercise prescription at a day service facility within PNCIS.
Water exercise at a day service facility in this study improved PCS and MCS (RP, BP, GH, VT, SF, and RE) for 6 months, irrespective of the exercise frequency. The HRQL of the person who exercises regularly is higher than that of the person who does not [17], and it is reported that the adherence to exercise improves HRQL [13]. A previous study reported improvement in PCS through water exercise; the exercise attendance rate affected the improvement, and a higher attendance rate improved it more [14]. Overall, exercise attendance rates in the once and twice groups in the present study were 95.0 ± 4.7% and 95.3 ± 5.8%, respectively. The present result is slightly better than those of previous water exercise intervention studies (84–90%) [13, 29, 30] and for land exercise in a care facility (70–81%) [31, 32]. Frail individuals have more difficulty continuing an exercise program according to their low exercise capacity [33–35]. Water exercise improves participation and adherence to an exercise program according to the group interaction and socialization resulting from the water exercise intervention [13]. The present water exercise program, which included ADL exercise, [18] was safely executed in a group, which might had have a positive effect on the attendance rate. The factors contributing to this result were the water exercise program and the execution under PNCIS, which indicate that water exercise programs within PNCIS ensure high exercise continuity and adherence. Therefore, it is suggested that water exercise at a day service facility improves continuity and adherence to exercise and improves HRQL in frail elderly people receiving a low level of nursing care, irrespective of the exercise frequency, for 6 months.
Health-related quality of life declines with age [36] and deterioration in ADL ability [36]. Scores in PCS and MCS prior to the water exercise intervention were slightly lower than normal values for healthy Japanese people aged 70–80 and were found to be related to ADL disability in this study. Additionally, improvements in ADL disability were apparent, as in our previous study [18]. These results suggest that the present improvements in HRQL were affected by the improvements in ADL disability. Furthermore, the HRQL value after water exercise intervention showed values similar to normal values for healthy Japanese people aged 70–80. Therefore, it is indicated that elderly people receiving a low level of nursing care can achieve similar HRQL to healthy people through participation in water exercise at a day service facility.
Many studies have reported that exercise interventions including water, resistance, and balance exercise improved ADL disability, symptoms and body functions; as a result, PF in the SF-36 was improved [7, 13, 30]. In contrast to those precedent studies, PF did not change in this study. Elderly people with nursing care had little confidence in their physical functions compared to healthy elderly people [36]. Although an improvement in ADL disability was observed in this research, the participants still required nursing care after the present water exercise intervention. Apparently, the improvement in ADL disability was insufficient to improve PF in this study. Nevertheless, although PF is reported to decrease with aging [19], higher PF was noted compared to that of the control group after 6 months in this study. Consequently, these results suggest that the present water exercise at a day service facility maintains PF in the SF-36, against its usual decline with aging, irrespective of exercise frequency. Further study is necessary to investigate the effects of water exercise within PNCIS on HRQL, including PF in elderly people receiving nursing care.
Despite the increasing number of studies that have examined the effects of water exercise on HRQL [13, 14, 30], no findings describe exercise frequency to improve and maintain HRQL. The results of between-group variation in HRQL show that the influence of the exercise frequency became greater at 3 months and smaller at 6 months. This supported the hypothesis that water exercise twice a week would elicit rapid improvement in HRQL and ADL disability at 3 months and subsequently plateau after that, with less dramatic gains from exercise once a week. It has been reported that ADL disability is one factor contributing to the decline in HRQL [36]. Therefore, it is indicated that water exercise frequency affects the change in HRQL among frail elderly people receiving nursing care, and that HRQL was related with ADL disability. A small negative ES was seen, though HRQL scores were similar between the once and twice groups at 6 months. It is reported that low-frequency exercise intervention is more acceptable because of the frail elderly’s poor participation, high drop-out rates, and low exercise capacity [34]. As such, those results might mean low exercise frequency is also acceptable. The findings in this study are applicable for water exercise prescription at a day service facility. Although this intervention only had a short term of 6 months, aging continues until the end of life; consequently, it is necessary to verify the long-term effects on HRQL of the frequency of water exercise within PNCIS.
There are several limitations in this study. First, the investigators who conducted the assessments were not blinded to the participants, which increased the possibility of bias during the assessment at 3 and 6 months. Second, we did not include other factors that may have contributed to the changes in HRQL, such as body functions, body structure or relationships with family. Third, SF-36 scores do not present HRQL at a point in time but during the preceding 4 weeks. Finally, the sample size in this study is small. Frail elderly people have various difficulties related to participating in water exercise. There are few existing facilities with a pool of the type in the day service center in this study. Additionally, it costs a lot of money to maintain and manage the equipment. For that reason, no research has examined the effects of water exercise among frail elderly people. Consequently, further research is needed to clarify the effects of water exercise on HRQL and ADL disability among frail elderly people.
In conclusion, this type of water exercise intervention at a day service facility within PNCIS can improve HRQL for 6 months by fostering exercise habits and improvements in ADL disability. In addition, the change in HRQL is different according to the exercise frequency: exercise twice a week elicited rapid improvement compared to exercise once a week, with a subsequent plateau of benefits.
Abbreviations
- HRQL:
-
Health-related quality of life
- ADL:
-
Activities of daily living
- PNCIS:
-
The public nursing-care insurance system
- SF-36:
-
The Medical Outcomes Survey Short form-36
- FIM:
-
Functional Independence Measure
- COPD:
-
Chronic obstructive pulmonary disease
- FM:
-
Fibromyalgia
- PF:
-
Physical functioning
- RP:
-
Role limitations due to physical health
- BP:
-
Bodily pain
- GH:
-
General health
- PCS:
-
Physical component summary
- VT:
-
Vitality
- SF:
-
Social functioning
- RE:
-
Role limitations due to emotional health
- MH:
-
Mental health
- MCS:
-
Mental component summary
- BMI:
-
Body mass index
- RPE:
-
Rating of perceived exertion scale
- SD:
-
Standard deviation
- ES:
-
Effect size
References
Spector, W. D., Katz, S., & Murphy, J. B. (1987). The hierarchical relationship between activities of daily living and instrumental activities of daily living. Journal of Chronic Diseases, 40, 481–489.
Katz, S., Branch, L. G., & Branson, M. H. (1983). Active life expectancy. The New England Journal of Medicine, 309, 1218.
Sato, S., Demura, S., Kobayashi, H., & Nagasawa, Y. (2002). The relationship and its change with aging between ADL and daily life satisfaction characteristics in independent Japanese elderly living at home. Journal of Physiological Anthropology and Applied Human Science, 21(4), 195–204.
Luulinen, H., Lehtola, S., Jokelainen, J., Vaananen-Sainio R., Lotvonen S., & Koistinen P. (2006). Prevention of disability by exercise among the elderly: A population-based, randomized, controlled trial. Scandinavian Journal of Primary Health Care, 24, 199–205.
Health, Labour and Welfare Ministry, http://www.mhlw.go.jp/.
Satake, K., Knazawa, N., Takemura, S., Fujita, K., Yamase, T., & Nishijima, T. (2004). The effect of resistance training in the elderly with nursing care. Hokkaido Journal of Public Health, 18, 34–42.
Ishihara, K., Nishimoto, K., Mimura, T., Tanaka, S., Kurihara, N., & Fujimoto, S. (2001). Effects of a balance training program on balance function in geriatric health services facility residents (vol 16, pp. 18–25). Tokyo: Research Aid Report, Physical Fitness Research Institute: Meiji Yasuda Life Foundation of Health and Welfare.
Gregg, E. W., Pereira, M. A., & Caspersen, C. J. (2000). Physical activity, falls, and fractures among older adults: A review of the epidemiologic evidence. Journal of the American Geriatrics Society, 48, 883–893.
Tinetti, M. E., Speechley, M., & Ginter, S. F. (1988). Risk factors for falls among the elderly. The New England Journal of Medicine, 319, 1800–1806.
Hauer, K., Specht, N., Schuler, M., Bartsch P., & Oster P. (2002). Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing, 31, 49–57.
Skelton, D., & Dinan, S. M. (1999). Exercise for falls management: Rationale for an exercise programme aimed at reducing postural instability. Physiotherapy Theory and Practice, 15, 105–120.
Forwood, M. R., & Larsen, J. A. (2000). Exercise recommendations for osteoporosis. A position statement of the Australian and New Zealand Bone Mineral Society. Australian Family Physician, 29, 761–764.
Devereux, K., Robertson, D., & Briffa, N. K. (2005). Effects of a water-based program on women 65 years and over: A randomised controlled trial. Australian Journal of Physiotherapy, 51, 102–108.
Wadell, K., Sundelin, G., Larsen, H. K., & Lundgren, R. (2004). High-intensity physical group training in water-an effective training modality for patients with COPD. Respiratory Medicine, 98, 428–438.
Mannerkorpi, K., Ahimen, M., & Ekdahl, C. (2002). Six- and 24-month follow-up pool exercise therapy and education for patients with fibromyalgia. Scandinavian Journal of Rheumatology, 31, 306–310.
Demura, S., Kobayashi, H., & Kitabayashi, T. (2005). QOL models constructed for the community-dwelling elderly with ikigai (purpose in life) as a composition factor, and the effect of habitual exercise. Journal of Physiological Anthropology and Applied Human Science, 24(5), 525–533.
Acree, L. S., Longfors, J., Fjeldstad, A. S., Fjeldstad, C., Schank, B., Nickel, J. K., et al. (2006). Physical activity is related to quality of life in older adults. Health and Quality of Life Outcomes, 4, 37.
Sato, D., Kaneda, K., Wakabayashi, H., & Nomura, T. (2007). Some effects of water exercise frequency on functional mobility in nursing care elderly. Japanese Journal of Physical Fitness and Sports Medicine, 56, 141–148.
Matsushita, T., & Matsushima, E. (2004). The relationship between QOL and lifestyle in the elderly. Quality of Life Journal, 5(1), 19–28.
Granger, C. V., Hamilton, B. B., & Keith, R. A. (1986). Advance in functional assessment for medical rehabilitation. Topics in Geriatric Rehabilitation, 1, 59–74.
Borg, G. (1970). Perceived exertion as an indicator of somatic stress. Scandinavian Journal of Rehabilitation Medicine, 2, 92–98.
Fukuhara, S., Ikegami, N., Torrance, G. W., Nishimura, S., Drummond, M., & Schubert, F. (2002). The development and use of quality of life measures to evaluate health outcomes in Japan. PharmacoEconomics, 20(2), 17–23.
Fukuhara, S., Bito, S., Hsiao, A., Green, J., & Kurokawa, K. (1998). Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. Journal of Clinical Epidemiology, 51(11), 1037–1044.
Fukuhara, S., Ware, J. E., Kosinski, M., Wada, S., & Gandek, B. (1998). Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. Journal of Clinical Epidemiology, 51(11), 1045–1053.
Jenkinson, C., Wright, L., & Coulter, A. (1994). Criterion validity and reliability of the SF-36 in a population sample. Quality of Life Research, 3, 7–12.
Pollak, N., Rheault, W., & Stoecker, L. (1996). Reliability and validity of the FIM for person aged 80 years and above from a multilevel continuing care retirement community. Archives of Physical Medicine and Rehabilitation, 77, 1056–1061.
Stineman, M. G., Jette, A., & Tassoni, C. J. (1996). The Functional Independence Measure: Test of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Archives of Physical Medicine and Rehabilitation, 77, 1101–1108.
Onodera, K., & Miyashita, M. (1976). A study on Japanese scale for rating of perceived exertion in endurance exercise. Japanese Journal of Physical Education, 21(4), 191–203.
Mihevic, P. M. (1981). Sensory cues for perceived exertion: A review. Medicine and Science in Sports and Exercise, 13, 150–163.
Cohen, J. (1988). Statistical power analysis for the behavioral science (2nd ed.). Mahwah: Lawrence Erlbaum.
Suomi, R., & Collier, D. (2003). Effects of arthritis exercise programs on functional fitness and perceived activities of daily living measures in older adults with arthritis. Archives of Physical Medicine and Rehabilitation, 84, 1589–1594.
Foley, A., Halbert, J., Hewitt, T., & Crotty, M. (2003). Does hydrotherapy improve strength and physical function in patients with osteoarthritis—A randomized controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Annals of the Rheumatic Diseases, 62, 1162–1167.
Littbrand, H., Rosendahl, E., & Lindelof, N. (2006). A high-intensity weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: Evaluation of the applicability with focus on cognitive function. Physical Therapy, 86(4), 489–498.
Chin, A., Poppel, M., Twisk, J., & Mechelan, W. (2006). Once a week not sufficient, twice a week not feasible? A randomized controlled exercise trial in long-term care facilities [ISRCTN87177281]. Patient Education and Counseling, 63, 205–214.
Alexander, B., Gross, M., Medell, L., & Hofmeyer, R. M. (2001). Effects of functional ability and training on chair-rise biomechanics in older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56(9), 538–547.
Ide, H., Hirao, T., & Hashimoto, M. (2001). Health-related quality of life in human community. Journal of Health and Welfare Statistics, 48, 6–11.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, D., Kaneda, K., Wakabayashi, H. et al. The water exercise improves health-related quality of life of frail elderly people at day service facility. Qual Life Res 16, 1577–1585 (2007). https://doi.org/10.1007/s11136-007-9269-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-007-9269-2