Abstract
Different garlic products reduce the cerebral ischemic damage due to their antioxidant properties. In this work, we investigated the effect of aged garlic extract (AGE) on cyclooxygenase-2 (COX-2) protein levels and activity, and its role as a possible mechanism of neuroprotection in a cerebral ischemia model. Animals were subjected to 1 h of ischemia plus 24 h of reperfusion. AGE (1.2 ml/kg weight, i.p.) was administered at onset of reperfusion. To evaluate the damage induced by cerebral ischemia, the neurological deficit, the infarct area, and the histological alterations were measured. As an oxidative stress marker to deoxyribonucleic acid, 8-hydroxy-2-deoxyguanosine (8-OHdG) levels were determined. Finally, as inflammatory markers, TNFα levels and COX-2 protein levels and activity were measured. AGE treatment diminished the neurological alterations (61.6%), the infarct area (54.8%) and the histological damage (37.7%) induced by cerebral ischemia. AGE administration attenuated the increase in 8-OHdG levels (77.8%), in TNFα levels (76.6%), and in COX-2 protein levels (73.6%) and activity (30.7%) induced after 1 h of ischemia plus 24 h of reperfusion. These data suggest that the neuroprotective effect of AGE is associated not only to its antioxidant properties, but also with its capacity to diminish the increase in TNFα levels and COX-2 protein expression and activity. AGE may have the potential to attenuate the cerebral ischemia-induced inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular disease is the second cause of death and the most frequent cause of non-traumatic disability in adults worldwide, according to the World Health Organization [1]. Noteworthy, acute ischemic stroke accounts for about 85% of all cases [2]. Today there is no effective treatment to reverse the morphological and behavioral alterations induced by stroke.
The most common cause of stroke is the sudden occlusion of a blood vessel, resulting in the activation of a series of biochemical events that eventually lead to neuronal death [3]. Although reperfusion of ischemic brain tissue is critical for restoring normal function, paradoxically it can result in a secondary damage, where oxidative stress mediators play a critical role [4]. Moreover, cerebral injury is a potent triggering of inflammatory cytokines and protease secretion by microglia, leukocytes and resident cells of the neurovascular unit. Once the neurovascular barriers are breached, multiple neuroinflammatory cascades become activated, potentially leading to further secondary brain injury [5]. Cyclooxygenase (COX) is a key enzyme in this event [6]; it catalyzes the first committed step of arachidonic acid (AA) conversion into the unstable intermediate prostaglandin G2, which in turns is rapidly converted to prostaglandin H2 by COX, and finally, into a series of biologically active prostaglandins and thromboxane A2 [7]. Two isoforms of COX, termed COX-1 and COX-2, have been identified. Unlike COX-1, COX-2 expression is dramatically induced by ischemia and it has been proposed to exacerbate brain injury [8].
Aged garlic extract (AGE) is an odorless garlic preparation widely studied, and its antioxidant properties have been reported [9, 10]. The previous administration of AGE [11, 12], garlic oil [13] or aqueous garlic extract [14] reduces cerebral ischemia induced damage and oxidative stress. On the other hand, aqueous garlic extract [15] and some oil-soluble sulfides [16] have shown an inhibitory effect on COX-2 protein and activity, suggesting an anti-inflammatory activity of both the extract and the compounds. However, the anti-inflammatory activity of AGE has not been evaluated yet. Therefore, in this study we evaluated the effect of AGE on TNFα levels and COX-2 protein expression and activity in a focal cerebral ischemia model.
Materials and Methods
Aged Garlic Extract (AGE)
AGE Kyolic® was obtained from Wakunaga of America Co., Ltd. (Mission Viejo, CA), and complies with the specifications established in the US Pharmacopeia/National Formulary [17].
Animals
Male Wistar rats (280–350 g) were provided with a standard commercial rat chow diet (Laboratory rodent diet 5001, PMI Feeds Inc., Richmond, IN) and water ad libitum. Rats were maintained under constant conditions of temperature (25 ± 3 °C), humidity (50 ± 10%), and light (12 h light:dark cycle). All experiments with animals were carried out according to the National Institutes of Health Guide for the Care and Use of Animals, and the Local Guidelines on the Ethical Use of Animals from the Health Ministry of Mexico. During the experiment, all efforts were made to minimize animal suffering.
Experimental Design
Animals were divided randomly into five groups (n = 4-10): 1) CT, control; 2) Sham, animals subjected to the same surgical procedures that IR animals, but without blood flow occlusion and treated with saline solution; 3) AGE, animals treated with aged garlic extract; 4) IR, animals subjected to 1 h of ischemia and 24 h of reperfusion; and 5) IR+AGE.
Rats received saline solution or AGE (1.2 ml/kg weight, i.p.) at the onset of reperfusion. Twenty four h after reperfusion, animals were anesthetized with sodium pentobarbital (200 mg/kg weight, i.p.) and transcardially perfused with ice-cold isotonic sterile saline, followed by 10% buffered formaldehyde/saline (pH 7.4). The brains were removed, postfixed in 10% formalin and embedded in paraffin. Coronal sections were obtained and used for histological and immunohistochemical analyses. For the histological examination the quantification was carried out in the left striatum, while the immunohistochemical quantification was carried out in the left cortex. In other groups of animals, brain and cortex were obtained 24 h after reperfusion to measure the infarct area and the COX-2 activity, respectively.
Focal Cerebral Ischemia
Animals were anesthetized with a mixture of isoflurane (2.5–3.0%), oxygen and nitrogen. The focal cerebral ischemia was induced in rats by the introduction of a 3–0 nylon filament into the middle cerebral artery [18]. Sham animals were subjected to the same surgical procedures except that the filament was not advanced into the cerebral artery. Rectal temperature was maintained at 37.0 ± 0.5 °C with a feedback-regulated heating pad during the surgical procedure.
Neurological Deficit and Quantification of the Infarct Area
Evaluation of the neurological deficit was performed 30 min before sacrifice by five tests as previously reported [12]. Infarct area was visualized using 2,3,5-triphenyltetrazolium chloride staining [12].
Histological Examination
Sections (5 μm) were stained with hematoxylin and eosin. The morphometric parameters were calculated following the “random systematic sampler”. The general criteria to score damaged neurons included pyknotic nuclei, cytoplasmic vacuolation, shrunken perykaria and neuronal atrophy. The number of neuronal cells, preserved, damaged or total, was obtained as an average of five randomly selected fields of three sections per rat. Data are expressed as the percentage of neuronal damage per field.
Immunohistochemistry
Sections (5 μm) were deparaffined and then boiled in 3% sodium citrate with 0.2% triton X-100 to unmask antigen sites. Endogenous peroxidase activity was quenched with 1% H2O2. Nonspecific binding was avoided using a blocking solution. The sections were incubated with anti-COX-2 (1:200), anti-8-OHdG (1:200), or anti-TNFα (1:2000) antibodies and then incubated with a universal kit (secondary antibodies, peroxidase). Finally, all sections were incubated with diaminobenzidine and counterstained with hematoxylin. The average percent of positive cells per field was determined with a computerized image analyzer KS-300 3.0 (Hallbergmoos, Germany).
COX-2 Activity
Cortex samples were homogenized in lysis buffer pH 7.9 (containing 10 mM Tris–HCl, 15 mM NaCl, 0.25 mM sucrose and proteases inhibitors), and centrifuged at 13,000 × g for 30 min. The supernatants were used to determine COX-2 activity using a COX Fluorescent Activity Assay Kit (Cayman Chemical Co., Ann Arbor, MI, Cat No. 700200).
Statistical Analysis
Data are expressed as mean ± S.E.M. and were analyzed by one-way analysis of variance (ANOVA) followed by a post-hoc Tukey’s test. Data of infarct area were analyzed by unpaired t test. All data were analyzed using the software Graph Pad 5.01 (San Diego, CA). p < 0.05 was considered as statistically significant.
Results
Neurological Deficit
AGE decreased significantly the neurological impairment induced by 1 h of ischemia and 24 h of reperfusion from 3.6 ± 0.2 in the IR group to 1.4 ± 0.5 in the IR+AGE group. CT, sham, and AGE groups did not show any motor behavioral alterations (Fig. 1).
Infarct Area
The lesion produced by 1 h of ischemia plus 24 h of reperfusion (IR) showed an infarct area of 46.7 ± 2.4. The administration of AGE at the beginning of reperfusion significantly reduced the infarct area to 21.1 ± 2.7 in the IR+AGE group. There was no evidence of infarct in the CT, sham, and AGE groups (Table 1).
Histological Examination
In contrast to a well-preserved appearance of the striatal tissue from CT and sham animals, cerebral ischemia resulted in a considerable cellular damage revealed by extensive neuronal cell loss along the dorsal striatum; abundant pycnotic nuclei, shrunken cells, and destruction of neuropil were observed. AGE administration attenuated some alterations evoked by cerebral ischemia, whereas the treatment with AGE alone produced a normal appearance of striatal tissue similar to CT and sham groups (Fig. 2, upper panels). These findings were strengthened by the quantitative assessment of nerve tissue damage: animals from the IR+AGE group showed a decrease of 37.7% in the number of damaged neurons per field produced by cerebral ischemia in the striatum (Fig. 2, lower panel).
Effect of aged garlic extract (AGE) on neuronal damage. Histological alterations were evaluated 24 h after the onset of reperfusion. A representative photomicrograph of each group is shown (upper panels). Affected neurons (arrows), edema in the interstitial neuropil (asterisks), and karyorexis (arrowhead) are shown. Magnification: 40x. Graph represents the quantitative cell damage. Values are expressed as mean ± S.E.M. n = 5. a p < 0.001 vs. CT, Sham, and AGE; b p < 0.001 vs. CT, Sham, AGE, and IR
8-OHdG Levels
AGE treatment prevented by 77.8% the increase in the number of 8-OHdG immune-positive cells observed in the IR group. CT, Sham and AGE groups showed similar levels of 8-OHdG (Fig. 3).
Effect of aged garlic extract (AGE) on 8-hydroxy-2-deoxyguanosine (8-OHdG) levels. 8-OHdG levels were evaluated 24 h after the onset of reperfusion. A representative photomicrograph of 8-OHdG immunodetection on each group is shown (upper panels). Arrows: Immunoreactive cell. Magnification: 40x. Graph represents the quantitative analysis scored in the different groups. Values are expressed as mean ± S.E.M. n = 5. a p < 0.001 vs. CT, Sham, AGE, and IR+AGE
TNFα Levels
TNFα levels augmented 12.3 fold after ischemia and reperfusion when compared to CT group, and AGE treatment prevented this increase in the IR+AGE group. CT, Sham and AGE groups showed similar levels of TNFα (Fig. 4).
Effect of AGE on TNFα levels. TNFα levels were evaluated 24 h after the onset of reperfusion. A representative photomicrograph of TNFα inmunodetection on each group is shown (upper panel). Arrowheads: Immunoreactive cell. Magnification: 40x. Graph represents the quantitative analysis scored in the different group. Values are expressed as mean ± S.E.M. n=4. a p < 0.001 vs CT, Sham, AGE, and IR+AGE
Cyclooxygenase-2 (COX-2) Protein Levels and Activity in Cortex
Animals submitted to 1 h of ischemia and 24 h of reperfusion (IR group) showed an increase in both the number of COX-2 immunoreactive cells (Fig. 5, upper panels) and COX-2 activity (Fig. 4b) when are compared with CT and sham animals. The AGE treatment significantly diminished the increase in COX-2 protein levels (73.6%) and activity (30.7%) induced by cerebral ischemia. The protein content (Fig. 5a) and the activity (Fig. 5b) of COX-2 diminished with AGE alone.
Effect of aged garlic extract (AGE) on cyclooxygenase-2 (COX-2) levels and activity in cortex. A representative photomicrograph of COX-2 immunodetection on each group is shown (upper panels). Arrows: Immunoreactive cell. Magnification: 40x. a Graph represents the quantitative analysis of COX-2 protein levels. b Graph represents the COX-2 activity. Values are expressed as mean ± S.E.M. n = 5. a p < 0.05 vs. CT; b p < 0.01 vs CT, Sham, AGE, and IR+AGE
Discussion
AGE Decreased the Neurological Deficit, the Infarct Area, and the Histological Alterations Induced by Cerebral Ischemia
AGE treatment decreased the neurological impairment induced by 1 h of ischemia and 24 h of reperfusion. Our findings also show an important protective effect of AGE on the infarct area and morphological alterations. Altogether, these results suggest that the protective effect of AGE on neurological impairment could be associated with the amelioration of morphological damage induced by cerebral ischemia.
AGE Decreased the Oxidative Stress Induced by Cerebral Ischemia
The physiopathological mechanisms underlying the neuronal injury in the stroke are complex and multifactorial. Oxidative stress actively participates during post-ischemic brain injury [19, 20], and the treatment with antioxidants has a beneficial effect in experimental cerebral ischemia models [21]. In this work, the oxidative damage to deoxyribonucleic acid was evidenced by the increase in the number of positive cells to 8-OHdG in the ipsilateral hemisphere of animal exposed to cerebral ischemia, and this marker was decreased by the administration of AGE. It has been suggested that the antioxidant properties of AGE are involved in ischemic neuroprotection [11, 12]. Similar to those reports, data obtained in this work support the antioxidant effect of AGE in this model.
AGE Showed Anti-Inflammatory Properties in Cerebral Ischemia Model
After loss of blood flow in a region of the brain, the ischemic cascade is rapidly initiated and two important physiopathological mechanisms are triggered: oxidative stress and inflammation. Ischemic stroke begins with severe focal hypoperfusion that leads to excitotoxicity and oxidative damage, which in turn cause microvascular injury, blood brain barrier dysfunction and post-ischemic inflammation [22]. Post-ischemic inflammation can contribute to ischemic damage by different mechanisms. In rodent models of cerebral ischemia, as well as in patients with stroke, infiltrating neutrophils produce enhanced levels of inducible nitric oxide synthase, an enzyme responsible of producing toxic amounts of nitric oxide. In addition, ischemic neurons express COX-2, an enzyme that mediates ischemic injury by producing superoxide anion and toxic prostanoids. Ischemic neurons also produce TNFα, a cytokine involved in the exacerbation of ischemic injury [Reviewed in 3].
In this work, AGE treatment attenuated significantly the increase induced by cerebral ischemia in TNFα and COX-2 protein levels and activity of COX-2, suggesting that this extract has anti-inflammatory properties. The effect of AGE on COX-2 could be associated, at least in part, with its ability to decrease TNFα levels. It has been reported that COX-2 upregulation is attributed to activation of different protein kinases and transcriptional factors that are greatly regulated by TNFα [23].
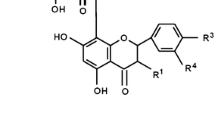
In addition, to our knowledge there are no other reports describing the effect of AGE alone on COX-2 protein levels and activity. Aqueous garlic extract [15] and some oil-soluble sulfides such as diallyl sulfide, diallyl disulfide, and diallyl trisulfide [16] have shown an inhibitory effect on COX-2 protein and activity, suggesting an anti-inflammatory effect of both extract and isolated compounds. In AGE, oil-soluble sulfides are completely lost after three months due to their evaporation [24]; therefore, these compounds can not be responsible of the effect of AGE found in this work. On the other hand, Sendl et al. [25] suggested that COX-2 inhibition by aqueous garlic extract is due to the presence of gamma-glutamylcysteine sulfoxide and other gamma-glutamylcysteines. Similar to the oil-soluble sulfides, gamma-glutamylcysteines in AGE are completely hydrolyzed [24] and these compounds neither can be the responsible of the AGE effect found in this work. An interesting alternative explanation has emerged in two recently compounds isolated from raw garlic (both with flavonoid structure): N-feruloyltyramine [26] and thiacremonone [27] that showed a potent inhibitory effect on COX-1 and COX-2.
Each garlic preparation has a characteristic chemical composition. In AGE, S-allylcysteine and S-allylmercaptocysteine have been reported as the major components; however, tetrahydro-beta-carbolines (1-methyl-1,2,3,4-tetrahydro-beta-carboline-3-carboxylic acid and 1-methyl-1,2,3,4-tetrahydro-beta-carboline-1,3-dicarboxylic acid) have also been isolated from AGE [28]. Tetrahydro-beta-carbolines are biologically active alkaloids and are structurally similar to flavonoids, suggesting that the tetrahydro-beta-carbolines in AGE could be responsible for the AGE alone effect observed on COX-2 protein and activity. However, this hypothesis remains to be proved.
Altogether, these results suggest that AGE treatment decreases the morphological alterations and the infarct area, which was associated to the diminution of oxidative stress (8-OHdG levels) and inflammation (TNFα and COX-2) induced by cerebral ischemia.
In conclusion, the protective effect of AGE on neuronal deficit, infarct area, and neuronal damage induced by cerebral ischemia was associated with the diminution of oxidative stress and with the attenuation of the increase in TNFα levels, and protein expression and activity of COX-2. To our knowledge, this is the first report of the potentially anti-inflammatory activity of AGE.
Abbreviations
- AGE:
-
aged garlic extract
- COX-2:
-
cyclooxygenase-2
- IR:
-
ischemia and reperfusion
- 8-OHdG:
-
8-hydroxy-2-deoxyguanosine
References
WHO (2005) Preventing chronic diseases: a vital investment. World Health Organization, Geneva
Díez-Tejedor E, Del Brutto O, Álvarez-Sabín J, Muñoz M, Abiusi G (2001) Classification of the cerebrovascular diseases. Rev Neurol 33:455–464
Dirnagl U, Ladecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: An integrated view. Trends Neurosci 22:391–397
Wong CH, Crack PJ (2008) Modulation of neuro-inflammation and vascular response by oxidative stress following cerebral ischemia-reperfusion injury. Curr Med Chem 15:1–14
Danton GH, Dietrich WD (2003) Inflammatory mechanism after ischemia and stroke. J Neuropathol Exp Neurol 62:127–136
Choi SH, Aid S, Bosetti F (2009) The distinct roles of cyclooxygenase-1 and −2 in neuroinflammation: Implications for translational research. Trends Pharmacol Sci 30:174–181
Yang H, Chen C (2008) Cyclooxygenase-2 in synaptic signaling. Curr Pharm Des 14:1443–1451
Candelario-Jalil E, Fiebich BL (2008) Cyclooxygenase inhibition in ischemic brain injury. Curr Pharm Des 14:1401–1418
Morihara N, Hayama M, Fujii H (2011) Aged garlic extract scavenges superoxide radicals. Plant Foods Hum Nutr 66:17–21
Nencini C, Menchiari A, Franchi GG, Micheli L (2011) In vitro antioxidant activity of aged extracts of some Italian Allium species. Plant Foods Hum Nutr 66:11–16
Numagami Y, Sato S, Ohnishi ST (1996) Attenuation of rat ischemic brain damage by aged garlic extracts: A possible protecting mechanism as antioxidants. Neurochem Int 29:135–143
Aguilera P, Chánez-Cárdenas ME, Ortiz-Plata A, León-Aparicio D, Barrera D, Espinoza-Rojo M, Villeda-Hernández J, Sánchez-García A, Maldonado PD (2010) Aged garlic extract delays the appearance of infarct area in a cerebral ischemia model, an effect likely conditioned by the cellular antioxidant systems. Phytomedicine 17:241–247
Gupta R, Singh M, Sharma A (2003) Neuroprotective effect of antioxidants on ischaemia and reperfusion-induced cerebral injury. Pharmacol Res 48:209–215
Saleem S, Ahmad M, Ahmad AS, Yousuf S, Ansari MA, Khan MB, Ishrat T, Islam F (2006) Behavioral and histologic neuroprotection of aqueous garlic extract after reversible focal cerebral ischemia. J Med Food 9:537–544
Sengupta A, Ghosh S, Das S (2004) Modulatory influence of garlic and tomato on cyclooxygenase-2 activity, cell proliferation and apoptosis during azoxymethane induced colon carcinogenesis in rat. Cancer Lett 208:127–136
Elango EM, Asita H, Nidhi G, Seema P, Banerji A, Kuriakose MA (2004) Inhibition of cyclooxygenase-2 by diallyl sulfides (DAS) in HEK 293 T cells. J Appl Genet 45:469–471
Aged Garlic Extract (2006) Research excerpts from peer reviewed scientific journals & scientific meetings. Wakunaga of America Co. Ltd., Mission Viejo
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84–91
Peters O, Back T, Lindauer U, Busch C, Megow D, Dreier J, Dirnagl U (1998) Increased formation of reactive oxygen species after permanent and reversible middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab 18:196–205
Rodrigo J, Fernandez AP, Serrano J, Peinado MA, Martinez A (2005) The role of free radicals in cerebral hypoxia and ischemia. Free Radic Biol Med 39:26–50
Aguilera P, Chanez-Cardenas ME, Maldonado PD (2007) Recent advances in the use of antioxidant treatments in cerebral ischemia. In: Santamarıa A, Jimenez-Capdeville ME (eds), New Perspectives on Brain Cell Damage, Neurodegeneration and Neuroprotective Strategies. Kerala/India, Research Signpost, pp 145–159
Lakhan SE, Kirchgessner A, Hofer M (2009) Inflammatory mechanisms in ischemic stroke: Therapeutic approaches. J Transl Med 7:97
Medeiros R, Figueiredo CP, Pandolfo P, Duarte FS, Prediger RD, Passos GF, Calixto JB (2010) The role of TNF-alpha signaling pathway on COX-2 upregulation and cognitive decline induced by beta-amyloid peptide. Behav Brain Res 209:165–173
Lawson LD (1998) Garlic: A view of its medicinal effects and indicated active compounds. In: Lawson LD, Bauer R (eds), Phytomedicines of Europe: Chemistry and Biological Activity. American Chemical Society/Washington: ACS Symposium Series 691, pp 176–209
Sendl A, Elbl G, Steinnke B, Redl K, Breu W, Wagner H (1992) Comparative pharmacological investigations of Allium ursinum and Allium sativum. Planta Med 58:1–7
Park JB (2009) Isolation and characterization of N-feruloyltyramine as the P-selectin expression suppressor from garlic (Allium ursinum). J Agric Food Chem 14:8868–8872
Ban JO, Oh JH, Kim TM, Kim DJ, Jeong HS, Han SB, Hong JT (2009) Anti-inflammatory and arthritic effects of thiacremonone, a novel sulfur compound isolated from garlic via inhibition of NF-kappaB. Arthritis Res Ther 11:R145
Ichikawa M, Yoshida J, Ide N, Sasaoka T, Yamaguchi H, Ono K (2006) Tetrahydro-beta-carboline derivatives in aged garlic extract show antioxidant properties. J Nutr 136:726S–731S
Acknowledgement
This study was supported by CONACYT (Grant No. 103527 to PDM).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Colín-González, A.L., Ortiz-Plata, A., Villeda-Hernández, J. et al. Aged Garlic Extract Attenuates Cerebral Damage and Cyclooxygenase-2 Induction after Ischemia and Reperfusion in Rats. Plant Foods Hum Nutr 66, 348–354 (2011). https://doi.org/10.1007/s11130-011-0251-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11130-011-0251-3