Abstract
Purpose
Isolated adrenocorticotropic hormone deficiency is a rare disease; however, since immune check point inhibitors (ICIs) have become widely used, many more cases have been reported. In this study, we compared the human leukocyte antigen (HLA) signatures between ICI-induced isolated adrenocorticotropic hormone deficiency (IAD) and idiopathic IAD (IIAD).
Design and methods:
Clinical features and HLA frequencies were compared among 13 patients with ICI-induced IAD, 8 patients with IIAD, and healthy controls. HLA frequencies of healthy controls were adopted from a HLA database of Japanese population.
Results
Age and body mass index were higher, while the rate of weight loss was lower, in patients with ICI-induced IAD than in those with IIAD. No HLA alleles had a significantly higher frequency in patients with ICI-induced IAD than in healthy controls, whereas the frequencies of HLA-DRB1*09:01, HLA-DQA1*03:02, and DQB1*03:03 were significantly higher in patients with IIAD than in healthy controls.
Conclusions
ICI-induced IAD and IIAD were different in terms of HLA frequencies. There were no specific HLAs related to ICI-induced IAD, whereas several HLAs in strong linkage disequilibrium were associated with IIAD. This might suggest that the two diseases have different pathological mechanisms. HLAs unique to IIAD may be helpful in predicting its pathophysiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune check point inhibitors (ICIs) block cytotoxic T-lymphocyte antigen 4 (CTLA-4), programmed cell death protein 1 (PD-1), or programmed cell death protein ligand 1 (PDL-1) to induce an immune system attack on cancer cells. Now that ICIs are widely used in a variety of cancer therapies, immune-related adverse events (irAEs) have become problematic and cannot be ignored. IrAEs may occur in any organ or tissue in the body, but the skin, intestines, and endocrine system, including the pituitary, adrenal glands, thyroid, pancreas, and parathyroid gland, are targeted most frequently [1, 2].
Hypophysitis caused by ICIs is most common after anti-CTLA-4 antibody treatment, with a prevalence of 3.2–13% [3, 4], and is less common after anti-PD-1 or PDL-1 antibody treatment, with a prevalence of 0.1–0.5% [4, 5]. Among the pituitary hormone disorders, adrenocorticotropic hormone (ACTH) deficiency is clinically important as it must be treated immediately. ACTH deficiency in the absence of ICI treatment usually occurs in pituitary disease accompanied by other pituitary deficiencies [6]. Isolated ACTH deficiency (IAD) is very rare and caused by lymphocytic hypophysitis [7], Sheehan’s syndrome, radiotherapy [8], traumatic brain injury [9], subarachnoid hemorrhage [10], or mutations in the T-box transcription factor [11] or proopiomelanocortin [12] genes. Idiopathic IAD (IIAD) is diagnosed after excluding these secondary ACTH deficiencies, and the prevalence of acquired IIAD is 3.8–7.3 per 100,000 [13]. Due to the rare cases, the pathophysiology of IIAD has not been fully elucidated, but it has been shown to be associated with autoimmune disease [14]. Some specific human leukocyte antigens (HLAs) increase susceptibility to developing certain autoimmune diseases [15]. However, there are few reports of a link between IIAD and HLA. We investigated the relevance of HLAs in ICI-induced IAD and IIAD.
Subjects and methods
Patients
The study was approved by the Nippon Medical School and Faculty of Medicine Ethics Committee (no. 30-03-1098) and was conducted in accordance with the principles of the Declaration of Helsinki. We obtained informed consent from all individual participants in the study.
Sixteen patients developed pituitary hormone deficiencies after treated with ICIs for cancer during the study registration period. Three out of 16 patients were excluded as they had not only ACTH deficiency but also complicated with other pituitary hormone deficiencies. The remaining thirteen patients who developed hypophysitis as isolated ACTH deficiency after being treated with ICIs was expressed as ICI-induced IAD in this study. Those 13 patients with ICI-induced IAD and eight patients with acquired IIAD at our institution from 2014 to 2021 were enrolled in the study. Cases of ICI-induced IAD during a clinical trial were excluded.
In the group of ICI-induced IAD, there were five patients who received a combination therapy of Nivolumab and Ipilimumab. In general, Ipilimumab causes a hypophysitis with not only ACTH but multiple pituitary hormone deficiencies. We evaluated pituitary functions of these patients as follows and confirmed that only ACTH was affected. Therefore, those five patients which received a combination therapy were included in this study.
Pituitary hormone evaluation
The patients underwent baseline hormone evaluations. Overt ACTH deficiency was defined as a morning cortisol level below 4 µg/dL without elevated ACTH or as a peak cortisol level below 18 µg/dL in an ACTH or corticotropin-releasing hormone test (100 µg administration). Central hypothyroidism was diagnosed based on a low free thyroxine level with a normal or low thyroid stimulating hormone level. Hypogonadotropic hypogonadism was diagnosed in premenopausal women with irregular menstruation or amenorrhea, after confirming normal serum gonadotropin, estradiol, and prolactin levels to exclude hyperprolactinemia or ovarian disease, and in postmenopausal women with a low estradiol level but without a sufficiently elevated gonadotropin level. In men, hypogonadotropic hypogonadism was defined as a low serum testosterone level without an elevated gonadotropin level. Thyroid stimulating hormone and PRL responses on a thyrotropin releasing hormone test, and luteinizing hormone and follicle-stimulating hormone responses on a luteinizing hormone-releasing hormone test, were also referenced if available. Severe GH deficiency was defined as a peak GH level below 9 ng/mL, determined by a growth hormone releasing peptide-2 test [16]. PRL deficiency was diagnosed when the PRL level was below 1.5 ng/mL on several days.
Clinical characteristics
Sex, age, BMI, symptoms, hyponatremia (serum sodium level < 135 mEq/L), hypoglycemia (blood glucose level < 70 mg/dL), eosinophilia (eosinophil/white blood cell count > 7%), pituitary MRI, and levels of anti-pituitary antibody, anti-thyroperoxidase antibody (positive at ≥ 16.0 IU/mL), anti-thyroglobulin antibody (positive at ≥ 28.0 IU/mL), antinuclear antibody (positive at ≥ 1:40), and immunoglobulin G4 (positive at ≥ 135 mg/dL) levels were evaluated in the ICI-induced IAD and IIAD groups. An anti-pituitary antibody assay (SRL, Inc, Tokyo, Japan) was established using the biotin/avidin system with rat pituitary glands [17].
HLA genotyping
The HLA-A, B, C, DRB1, DRB3/4/5, DQA1, DQB1, DPA1, and DPB1 alleles were genotyped using next-generation sequencing using a MiSeq system (Illumina, Inc. San Diego CA, USA) with HLA typing Kit (Scisco Genetics, Inc. Seattle WA, USA) at HLA Laboratory, Kyoto, Japan. The HLA alleles in this study were compared with those from a database of a healthy Japanese population [18, 19].
Statistical analysis
Continuous variables are expressed as means ± standard deviation. Differences between groups were assessed using the nonparametric Wilcoxon rank sum test for continuous data and Fisher’s exact test for categorical data, and differences were considered significant at p < 0.05. Statistical analyses were performed using JMP, version 14.1.0 (SAS Institute, Cary, NC, USA).
Results
Characteristics of patients with ICI-induced IAD
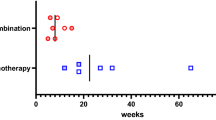
The characteristics of the 13 patients who developed ICI-induced IAD are summarized in Table 1. Five patients (four males and one female) with non-small cell lung cancer received pembrolizumab or atezolizumab. Four male patients with kidney cancer received nivolumab monotherapy or nivolumab plus ipilimumab. Two patients (one male and one female) with melanoma received nivolumab plus ipilimumab. One male patient with bladder cancer received pembrolizumab. One male patient with nasal cancer received pembrolizumab. The median number of ICI courses before the development of ACTH deficiency was 9 [3.5–13.5, (25–75%)]. Endocrine disorders other than ACTH deficiency included two cases of primary hypothyroidism and one case of type 1 diabetes.
Clinical characteristics of patients with ICI-induced IAD versus IIAD
The clinical characteristics of the 13 patients with ICI-induced IAD and 8 patients with IIAD were compared (Table 2). Age (71.3 ± 9.1 vs. 57.8 ± 11.4 years, p = 0.007) and BMI (20.9 ± 3.8 vs. 17.9 ± 2.6, p = 0.032) were higher in the ICI-induced IAD group than the IIAD group. In terms of ACTH deficiency symptoms, weight loss occurred less frequently in the ICI-induced IAD group than the IIAD group (3/13 vs. 6/8, p = 0.032). Other symptoms such as anorexia, fatigue, nausea, diarrhea, and disturbance of consciousness were not significantly different between the two groups. In the blood analysis, the ICI-induced IAD and IIAD groups did not differ in the frequency of hyponatremia (6/13 vs. 4/7, p = 1.00), hypoglycemia (4/13 vs. 2/7, p = 1.000), or eosinophilia (5/13 vs. 0/7, p = 0.114). In the immunological examination, cases of anti-pituitary antibody (1/7), anti-thyroperoxidase antibody (TPOAb) (2/13), antithyroglobulin antibody (TgAb) (4/13), antinuclear antibody (ANA) (1/13), and immunoglobulin G4 (IgG4) (2/13) positivity were detected in the ICI-induced IAD group. On the other hand, none of the patients in the IIAD group were positive for any of these markers. Pituitary MRI examination revealed that in the ICI-induced IAD group, one patient (patient No. 3 in Table 1) had a shrunken pituitary, one other patient (patient No. 8 in Table 1) had an enlarged pituitary, while the other 11 patients had normal pituitaries. In the IIAD group, one patient had a shrunken pituitary, another patient had an enlarged pituitary, and the other six patients had normal pituitaries.
HLA allele frequencies in ICI-induced IAD patients, IIAD patients, and healthy controls
The HLA alleles with higher frequencies in the ICI-induced IAD group than in the IIAD group are shown in Table 3. In the ICI-induced IAD group, no alleles had significantly higher frequencies compared with the healthy controls. On the other hand, the frequencies of HLA-DRB1*09:01 (87.5% (7/8) vs. 26.6%, p < 0.001), HLA-DQA1*03:02 (87.5% (7/8) vs. 26.8%, p < 0.001), and DQB1*03:03 (87.5% (7/8) vs. 28.7% p = 0.001) were significantly higher in the IIAD patients than in healthy controls. Compared with the ICI-induced IAD group, the IIAD group had significantly higher frequencies of HLA-DRB1*09:01 (3/13 vs. 7/8, p = 0.008), HLA-DQA1*03:02 (3/13 vs. 7/8, p = 0.008), DQB1*03:03 (3/13 vs. 7/8 p = 0.001) and HLA-DPA1*02:02 (7/13 vs. 8/8 p = 0.046).
Discussion
In this study, we investigated the characteristics of patients with ICI-induced IAD or IIAD and their relationships with HLA allele frequencies. Patients in the ICI-induced IAD group were older, had a higher BMI, and less frequently suffered from weight loss. This might be because all patients in the ICI-induced IAD group had cancer and attended a hospital to receive ICI therapy regularly; therefore, they were diagnosed earlier compared with the IIAD patients.
There were no differences in the frequency of hyponatremia, hypoglycemia, or eosinophilia, or in the positive rate of immunological examinations we measured (i.e. TPOAb, TgAb, ANA, IgG4), between the two groups. IIAD has a close association with autoimmune disease, but no patients in the IIAD group were positive for autoimmune antibodies. Regarding previous autoimmune diseases, one patient had a medical history of Schoenlein–Henoch purpura. A study from Poland revealed that 73% of 151 IIAD patients had autoimmune disease and/or thyroid antibodies [20]. On the other hand, only 12.6% of 103 Japanese patients with IIAD were positive for antithyroid antibodies [21], which was no higher than the prevalence in the healthy Japanese population. Whether this difference was due to the different ethnicities of the study groups was not elucidated.
In this study, no alleles were statistically more frequent in the ICI-induced IAD group than in healthy controls. Inaba et al. reported that HLA-DQB1*06:01, DPB1*09:01, and DRB5*01:02 increase the susceptibility to ACTH deficiency induced by anti-PD-1 therapy [22]. Furthermore, patients with pituitary irAEs had significantly increased frequencies of HLA-DR15, B52, and Cw12, as reported by Yano et al. [23], and of HLA-Cw12, DR15, DQ7, and DPw9, as reported by Kobayashi et al. [24]. Some of these HLA alleles tended to be more prevalent in our ICI-induced IAD group than in healthy controls, but not significantly so (HLA-B*52:01 (serotype B52): 38.5% (5/13) vs. 21.6%, p = 0.171; HLA-C*12:02 (serotype Cw12): 38.5% (5/13) vs. 21.0%, p = 0.164; HLA-DRB1*15:02 (serotype DR15): 38.5% (5/13) vs. 20.1%, p = 0.155; and HLA-DPB1*09:01 (serotype DPw9): 38.5% (5/13) vs. 18.9%, p = 0.083). These HLA alleles are more prevalent in the Japanese population. Furthermore, the study populations of the abovementioned studies were small (8 patients in [22], 11 patients in [23], and 17 patients in [24]), and the type of ICI used differed among the studies. In addition, Kobayashi et al. recruited a unique control population comprising only 40 patients without pituitary irAEs who received ICI treatment; this also might have affected the results. Inaba et al. analyzed HLA allele frequencies using a direct counting method, in contrast to HLA prevalences as in this study; however, the use of their method would not have changed our results.
Although the pathogenesis of pituitary irAEs remains unknown, CTLA-4 is expressed in the human pituitary gland at different levels, and an autopsy study showed that anti-CTLA-4 therapy can lead to type II and IV immune mechanisms in pituitaries expressing high levels of CTLA-4 [25]. PDL-1 expression has been detected in human pituitary tumors [26], but whether such tumors express PDL-2 or PD-1 is unknown. Another study reported that ICI therapy using antibodies targeting CTLA-4, PD-1, and PDL-1 resulted in uncontrollable type 2 macrophages and depletion of regulatory T cells, thereby inducing pituitary irAEs [27]. Further studies are necessary to clarify whether these pathological mechanisms are related to HLA allele frequencies.
The frequencies of HLA-DRB1*09:01, DQA1*03:02, and DQB1*03:03 were significantly higher in the IIAD group than in healthy controls in this study. Inaba et al. also showed significantly increased frequencies of HLA-DRB1*09:01 and DQB1*03:03 in IIAD patients [22]. DRB1*09:01 and DQB1*03:03 are associated with acute-onset type 1 diabetes [28, 29] and autoimmune polyglandular syndrome type III (thyroid autoimmunity plus other autoimmune diseases or type 1 diabetes excluding Addison’s disease) [30] in the Japanese population. Regarding as Type 1 diabetes, Miyadera et al. reported that the instability of HLA-DQ protein mediates the development of autoimmune disorders, analyzing the level of cell-surface MHC (major histocompatibility complex) density of HLA-DQ proteins [31]. This may have some common features with IIAD mechanisms. It must be taken into consideration that DRB1*09:01 is the most common DRB1 allele in Japanese population and in strong linkage disequilibrium with DQA1*03:02, and DQB1*03:03. Although this haplotype was expected to increase in the IIAD group, those findings were still observed significantly higher frequency in the IIAD group than ICI-induced IAD group, suggesting that the two groups might have different characteristics.
A study by Heaney et al. reported that lymphocytic hypophysitis was associated with HLA-DQ8 and HLA-DR53 in European and Asian ethnicities [32]. The frequencies of these HLA alleles were not increased in either the ICI-induced IAD or IIAD group, compared with the healthy controls, in this study. However, our results could not be compared with those of Heaney et al. because of ethnic differences between the study populations. Since HLA prevalence depends on ethnicity, a strength of this study was evaluation of patients with the same ethnicity.
This study has some limitations. First, the sample sizes of the ICI-induced IAD and IIAD groups were small due to the rarity of each disease. Further investigations of the relevance of HLA alleles in ACTH deficiency in larger study populations are necessary. Second, patients were treated with monotherapy or combination therapy consisting of anti-PD-1, anti-PDL-1, or anti-CTLA-4, and the mechanisms of each agent in pituitary irAE development might differ; therefore, it is ideal to evaluate each therapy individually to clarify the differences in HLA allele frequencies among these therapies. Third, the control group was healthy Japanese individuals, differing from the ICI-induced IAD patients, all of whom had cancer. Although examination of HLA allele frequencies in cancer patients who did not develop ICI-induced IAD as the control population is ideal, this is ethically difficult and almost impossible to recruit such individuals.
In conclusion, ICI-induced IAD and IIAD were different in terms of HLA frequencies. No specific HLAs were correlated with ICI-induced IAD, whereas several HLAs in strong linkage disequilibrium (HLA-DRB1*09:01, HLA-DQA1*03:02, and DQB1*03:03) were associated with IIAD. This may suggest differences in the pathological mechanisms between the two diseases. HLAs unique to IIAD may be helpful in predicting its pathophysiology.
References
Postow MA, Robert Sidlow MD, Hellmann MD (2018) Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 378:158–168
Bajwa R, Cheema A, Khan T, Amirpour A, Paul A, Chaughtai S, Patel S, Patel T, Bramson J, Gupta V, Levitt M, Asif A, Hossain MA (2019) Adverse effects of immune checkpoint inhibitors (programmed death-1 inhibitors and cytotoxic T-lymphocyte-associated protein-4 inhibitors): Results of a retrospective study. J Clin Med Res 11:225–236
Min L, Hodi FS, Giobbie-Hurder A, Ott PA, Luke JJ, Donahue H, Davis M, Carroll RS, Kaiser UB (2015) Systemic high-dose corticosteroid treatment does not improve the outcome of ipilimumab-related hypophysitis: a retrospective cohort study. Clin Canser Res 21:749–755
Barroso-Sousa R, Barry WT, Garrido-Castro AC, Hodi FS, Min L, Krop IE, Tolaney SM (2018) Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: A systematic review and meta-analysis. JAMA Oncol 4:173–182
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L, Carcereny E, Ahn MJ, Felip E, Lee JS, Hellmann MD, Hamid O, Goldman JW, Soria JC, Dolled-Filhart M, Rutledge RZ, Zhang J, Lunceford JK, Rangwala R, Lubiniecki GM, Roach C, Emancipator K, Gandhi L (2015) Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 372:2018–2028
Sherlock M, Ayuk J, Tomlinson JW, Toogood AA, Aragon-Alonso A, Sheppard MC, Bates AS, Stewart PM (2010) Mortality in patients with pituitary disease. Endocr Rev 31:301–342
Escobar-Morreale H, Serrano-Gotarredona J, Varela C (1994) Isolated adrenocorticotropic hormone deficiency due to probable lymphocytic hypophysitis in a man. J Endocrinol Invest 17:127–131
Agha A, Sherlock M, Brennan S, O’Connor SA, O’Sullivan E, Rogers B, Faul C, Rawluk D, Tormey W, Thompson CJ (2005) Hypothalamic-pituitary dysfunction after irradiation of nonpituitary brain tumors in adults. J Clin Endocrinol Metab 90:6355–6360
Hannon MJ, Crowley RK, Behan LA, O’Sullivan EP, O’Brien MM, Sherlock M, Rawluk D, O’Dwyer R, Tormey W, Thompson CJ (2013) Acute glucocorticoid deficiency and diabetes insipidus are common after acute traumatic brain injury and predict mortality. J Clin Endocrinol Metab 98:3229–3237
Hannon MJ, Behan LA, O’Brien MM, Tormey W, Ball SG, Javadpour M, Sherlock M, Thompson CJ (2014) Hyponatremia following mild/moderate subarachnoid hemorrhage is due to SIAD and glucocorticoid deficiency and not cerebral salt wasting. J Clin Endocrinol Metab 99:291–298
Couture C, Saveanu A, Barlier A, Carel JC, Fassnacht M, Flück CE, Houang M, Maes M, Phan-Hug F, Enjalbert A, Drouin J, Brue T, Vallette S (2012) Phenotypic homogeneity and genotypic variability in a large series of congenital isolated ACTH-deficiency patients with TPIT gene mutations. 97:E486–E495
Krude H, Biebermann H, Gruters A (2003) Mutations in the human proopiomelanocortin gene. Ann N Y Acad Sci 994:233–239
Yamamoto T, Kamoi K (2008) Prevalence of maturity-onset isolated ACTH deficiency (IAD) in 2005: Japanese cohort studies. Endocr J 55:939–941
Hannon AM, Hunter S, Smith D, Sherlock M, O’Halloran D, Thompson CJ, Irish Pituitary Database Group (2018) Clinical features and autoimmune associations in patients presenting with idiopathic isolated ACTH deficiency. Clin Endocrinol (Oxf) 88:491–497
Matzaraki V, Kumar V, Wijmenga C, Zhernakova A (2017) The MHC locus and genetic susceptibility to autoimmune and infectious diseases. Genome Biol 18:76
Chihara K, Shimatsu A, Hizuka N, Tanaka T, Seino Y, Katofor Y, KP-102 Study Group (2007) A simple diagnostic test using GH-releasing peptide-2 in adult GH deficiency. Eur J Endocrinol 157:19–27
Sugiura M, Hashimoto A, Shizawa M, Tsukada M, Maruyama S, Ishido T, Kasahara T, Hirata Y (1986) Heterogeneity of anterior pituitary cell antibodies detected in insulin-dependent diabetes mellitus and adrenocorticotropic hormone deficiency. Diabetes 3:111–114
HLA LABORATORY, Japan INC (2021) https://hla.or.jp/med/frequency_search/en/allele/. Accessed 1
Japanese Society for Histocompatibility and Immunogenetics (2021) http://jshi.umin.ac.jp/standarization/file/JSHI-hyokiallele-2021list.pdf Accessed 1
Kasperlik-Załuska AA, Czarnocka B, Czech W (2003) Autoimmunity as the most frequent cause of idiopathic secondary adrenal insufficiency: report of 111 cases. Autoimmunity 36:155–159
Murakami T, Wada S, Katayama Y, Nemoto Y, Kugai N, Nagata N (1993) Thyroid dysfunction in isolated adrenocorticotropic hormone (ACTH) deficiency: case report and literature review. Endocr J 40:473–478
Inaba H, Ariyasu H, Iwakura H, Ueda Y, Kurimoto C, Uraki S, Takeshima K, Yamaoka H, Furukawa Y, Morita S, Nishi M, Akamizu T (2019) Comparative analysis of human leucocyte antigen between idiopathic and anti-PD-1 antibody induced isolated adrenocorticotropic hormone deficiency: A pilot study. Clin Endocrinol (Oxf) 91:786–792
Yano S, Ashida K, Sakamoto R, Sakaguchi C, Ogata M, Maruyama K, Sakamoto S, Ikeda M, Ohe K, Akasu S, Iwata S, Wada N, Matsuda Y, Nakanishi Y, Nomura M, Ogawa Y (2020) Human leucocyte antigen DR15, a possible predictive marker for immune checkpoint inhibitor-induced secondary adrenal insufficiency. Eur J cancer 130:198–203
Kobayashi T, Iwama S, Sugiyama D, Yasuda Y, Okuji T, Ito M, Ito S, Sugiyama M, Onoue T, Takagi H, Hagiwara D, Ito Y, Suga H, Banno R, Nishikawa H, Arima H(2021) : Anti-pituitary antibodies and susceptible human leukocyte antigen alleles as predictive biomarkers for pituitary dysfunction induced by immune checkpoint inhibitors. J Immunother Cancer. 9, e002493
Caturegli P, Di Dalmazi G, Lombardi M, Grosso F, Larman HB, Larman T, Taverna G, Cosottini M, Lupi I (2016) Hypophysitis secondary to cytotoxic T-lymphocyte-associated protein 4 blockade: Insights into pathogenesis from an autopsy series. Am J Pathol 186:3225–3235
Mei Y, Bi WL, Greenwald NF, Du Z, Agar NY, Kaiser UB, Woodmansee WW, Reardon DA, Freeman GJ, Fecci PE, Laws ER Jr, Santagata S, Dunn GP, Dunn IF (2016) Increased expression of programmed death ligand 1 (PD-L1) in human pituitary tumors. Oncotarget 7:76565–76576
Mihic-Probst D, Reinehr M, Dettwiler S, Kolm I, Britschgi C, Kudura K, Maggio EM, Lenggenhager D, Rushing EJ (2020) The role of macrophages type 2 and T-regs in immune checkpoint inhibitor related adverse events. Immunobiology 225:152009
Kawabata Y, Ikegami H, Awata T, Imagawa A, Maruyama T, Kawasaki E, Tanaka S, Shimada A, Osawa H, Kobayashi T, Hanafusa T, Tokunaga K, Makino H (2009) Committee on type 1 diabetes, Japan diabetes society. Differential association of HLA with three subtypes of type 1 diabetes: fulminant, slowly progressive and acute-onset. Diabetologia 52:2513–2521
Katahira M, Ishiguro T, Segawa S, Kuzuya-Nagao K, Hara I, Nishisaki T (2008) Reevaluation of human leukocyte antigen DR-DQ haplotype and genotype in type 1 diabetes in the Japanese population. Horm Res 69:284–289
Hashimoto K, Maruyama H, Nishiyama M, Asaba K, Ikeda Y, Takao T, Iwasaki Y, Kumon Y, Suehiro T, Tanimoto N, Mizobuchi M, Nakamura T (2005) Susceptibility alleles and haplotypes of human leukocyte antigen DRB1, DQA1, and DQB1 in autoimmune polyglandular syndrome type III in Japanese population. Horm Res 64:253–260
Miyadera H, Ohashi J, Lernmark Ã, Kitamura T, Tokunaga K (2015) Cell-surface MHC density profiling reveals instability of autoimmunity-associated HLA. J Clin Invest 125:275–291
Heaney AP, Sumerel B, Rajalingam R, Bergsneider M, Yong WH, Liau LM (2015) HLA markers DQ8 and DR53 are associated with lymphocytic hypophysitis and may aid in differential diagnosis. J Clin Endocrinol Metab 100:4092–4097
Author information
Authors and Affiliations
Contributions
Ono M and Fukuda I designed the study. Ono M extracted the data and performed the statistical analysis. Ono M and Fukuda I wrote the manuscript. Nagao M, Tomiyama K, Okazaki-Hada M, Shuto Y, Kobayashi S, Yuji Y, Nagamine T, Nakajima Y, and Inagaki-Tanimura K contributed to the care of the patients and acquisition of the data. Sugihara H critically reviewed the article.
Corresponding author
Ethics declarations
Statements and declarations
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ono, M., Fukuda, I., Nagao, M. et al. HLA analysis of immune checkpoint inhibitor-induced and idiopathic isolated ACTH deficiency. Pituitary 25, 615–621 (2022). https://doi.org/10.1007/s11102-022-01231-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01231-1