Abstract
Purpose
To investigate demographic, imaging and laboratory characteristics, and treatment outcomes of acromegaly patients who have bihormonal (BA) growth hormone (GH) and prolactin (PRL) immunoreactive adenomas compared to patients who have densely granulated GH adenomas (DGA) and sparsely granulated GH adenomas (SGA).
Methods
Retrospective review of single-center surgically treated acromegaly patients; pathology was analyzed by a single neuropathologist using 2017 WHO criteria. Preoperative magnetic resonance imaging was assessed to evaluate tumor size, cystic component, invasion and T2 signal intensity.
Results
Seventy-seven patients; 19 BA (9 mammosomatotroph and 10 mixed GH and PRL adenomas) were compared with 30 DGA, and 28 SGA. Patients with BA were older than SGA (49.6 vs 38.5 years, p = 0.035), had a higher IGF-1 index (3.3 vs 2.3, p = 0.040) and tumors were less frequently invasive (15.8% vs 57.1%, p = 0.005). BA more frequently had a cystic component on MRI than both SGA and DGA (52.6% vs 14.3%, and 22%, p = 0.005 and 0.033, respectively). When all histological types were combined, biochemical remission postoperatively was more common in non-cystic than cystic tumors (50% vs 22.5%, p = 0.042). Somatostatin receptor ligand response rate was 66.7%, 90.9% and 37.5% in BA, DGA and SGA patients, respectively (p = 0.053).
Conclusion
Imaging characteristics are an increasingly important adenoma behavior determinant. An adenoma cystic component may suggest that a GH adenoma is a BA. Cystic tumors exhibited lower rates of surgical remission in this series; therefore, optimized individual patient treatment is needed, as patients could be candidates for primary medical treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acromegaly is a disease characterized by growth hormone (GH) and insulin-like growth factor-1 (IGF-1) excess, which is caused in more than 95% of patients by a pituitary adenoma [1, 2]. Growth hormone producing pituitary adenomas have several distinct histologic subtypes and delineation is important in predicting clinical course and treatment response [3]. Subtypes include densely granulated (DG), sparsely granulated (SG) or intermediate-type somatotroph adenomas, mixed GH- and prolactin (PRL) secreting adenomas, mammosomatotroph (MS) adenomas, and plurihormonal adenomas [4]. In particular, granulation pattern has been identified as an important predictor of tumor aggressiveness and response to medical treatment with somatostatin receptor ligands (SRLs) [5, 6]. Sparsely granulated GH adenomas (SGA) have been associated with more aggressive behavior and poorer response to SRLs compared to densely granulated GH adenomas (DGA) [7,8,9,10]. Interestingly, magnetic resonance imaging (MRI) characteristics are of increasing importance in distinguishing GH adenoma type. Sparsely granulated adenomas usually appear hyperintense on T2-weighted MRI, while DGA have been more commonly described as hypo- or isointense [11,12,13].
Information relating to the clinical course of mixed GH- and PRL expressing adenomas (mixed GH-PRL and MS adenomas) is sparse [5, 14,15,16]. In particular, the response to SRLs is uncertain and adenoma MRI appearance not been well characterized.
We conducted a retrospective analysis to identify characteristics of bihormonal (BA) GH and PRL adenomas (mixed GH-PRL and MS) in a large cohort of treatment-naïve acromegaly patients in the setting of a GH adenoma, using the 2017 World Health Organization (WHO) classification of pituitary adenomas [4]. We compared baseline clinical, pathological, imaging characteristics, and response to SRLs between BA, DGAs and SGAs.
Methods
Patients
The study was approved by the Oregon Health & Science University (OHSU) Institutional Review Board. A retrospective review of patients who underwent surgery for acromegaly at OHSU between January 2004 and December 2018 (15 years) was undertaken. Patients with prior history of pituitary surgery, pre-operative use of medical therapy (SRLs, dopamine agonists; DAs, GH receptor blockers), or radiation were excluded. Forty-six patients reviewed here were previously included in a published cohort (from 2006 to 2011) [5]. For this expanded retrospective analysis, all patient’s electronic medical records were re-reviewed and the cohort was extended to include 2011–2018, MRI data analyzed, and pathology slides were re-reviewed and categorized by a single neuropathologist according to the WHO 2017 criteria [4].
Pathology
Histological staining was performed as previously described [5]. Cases were reviewed by a board-certified neuropathologist (M.D.W.), who was blinded to clinical history, tumor radiologic appearance, treatment outcome, and original pathological diagnosis. Minimum criteria for analysis inclusion were: (1) definitive histological diagnosis of a pituitary adenoma with adequate tissue sampling to interpret histochemical stains, (2) availability of a hematoxylin and eosin (H&E) stained section, and (3) availability of immunohistochemical stains for human GH, PRL, low molecular weight keratin (CAM5.2), and collagen-IV or a reticulin special stain. Prolactin and human GH staining was scored on a 5-point scale with the following cutoffs; 0 = no definitive tumor staining, 1 + ≤ 10% tumor staining, 2 + = 10–50% tumor staining, 3 + = 50–90% tumor staining, and 4 + ≥ 90% tumor staining. Cytokeratin CAM5.2 was scored as either negative in tumor or positive in tumor, and broken down by proportion of cells showing cytoplasmic/perinuclear staining versus dense juxtanuclear staining of fibrous bodies. When available, somatostatin receptor 2A was evaluated for membranous staining using a 4-point scale with the following cutoffs; 0 = negative, 1 + = weak, partial membranous staining, 2 + = intermediate, incomplete membranous staining, 3 + strong, circumferential membranous staining. Other staining was evaluated when available, including adrenocorticotrophic hormone, thyroid stimulating hormone (TSH), estrogen receptor, and synaptophysin.
Evaluable tumors that met the minimum inclusion criteria were categorized using the 2017 WHO criteria [4]. Briefly, tumors with > 70% of cells showing fibrous bodies were categorized as SGA, with no further stratification by PRL expression. Tumors with cytoplasmic/perinuclear cytokeratin staining and only occasional fibrous bodies (up to 30% of cells) were categorized as DGA, and then sub-stratified by PRL staining. Tumors containing 30–70% of cells with fibrous bodies were categorized as intermediate-type somatotroph adenomas and then sub-stratified by PRL staining. For sub-stratification by PRL, tumors were categorized as negative (score 0) or with focal PRL positivity (1 +, up to 10% of tumor cells positive). Densely granulated or intermediate-type tumors with greater than 10% PRL positivity were categorized as BA and this group included MS and mixed GH- and PRL. Definitive distinction between a MS and a mixed GH- and PRL can only be made by electron microscopy (EM), and further sub-stratification of this group of tumors by histology is highly subjective. Recognizing this subjectivity, tumors were categorized as likely MS when the GH and PRL scores could only be explained by a significant proportion of adenoma cells expressing both hormones. For example, > 50% of cells staining for both GH and PRL (i.e. at least 3 + for both markers), or when a tumor was diffusely positive for GH (4 + staining) and also shows significant PRL staining (i.e. > 2 +). Other cases were categorized as likely mixed GH-PRL adenomas when two distinct cell populations were observed, showing a reciprocal staining pattern on GH and PRL immunohistochemistry suggestive of two distinct adenoma cell subpopulations. It was rare for cases not to fall into one of these categories; e.g. 1 plurihormonal adenoma (positive for GH, PRL, and TSH), 1 possible Pit-1 positive plurihormonal adenoma (a diagnosis that was not codified at the time of original pathologic diagnosis), 1 possible acidophil stem cell adenoma, and 1 prolactinoma where GH-expressing regions could be attributed to entrapped anterior pituitary tissue in the evaluated sampling.
For the purposes of final analysis only BA (MS and mixed GH-PRL), DGA, and SGA, were included. Three intermediate-type adenomas, 4 adenomas with negative CAM 5.2, 3 with no CAM 5.2 stain available, 1 acidophil stem adenoma, 2 plurihormonal adenomas, and 1 collision meningioma-GH adenoma were also excluded.
Since precise distinction between MS and mixed cell GH-PRL adenomas is only possible with EM and practically not possible in the majority of centers, we combined all dual-expressing adenomas into one group; BA. However, we also undertook a separate analysis comparing MS and mixed GH-PRL adenomas.
Imaging
Pre-operative MRI was utilized for evaluation of pituitary adenoma imaging characteristics. While all patients underwent surgery at OHSU, pre-operative MRIs were performed at different outside hospitals. Dedicated pituitary MRI and subsequent reports were utilized to evaluate tumor size, presence of invasion into surrounding structures, and T2 signal intensity. The maximum diameter of the tumor as noted in the MRI report was utilized. The presence of invasion was determined if tumor invaded the cavernous sinus or/and sphenoid sinus in the report. In unclear cases, tumor diameter and invasion were confirmed with re-review by a board-certified neuroradiologist. A cystic or necrotic component of pituitary adenomas was assessed by a neuroendocrinologist familiar with reading pituitary MRIs and confirmed with a neuroradiologist. A cystic/necrotic component was defined as an area of marked T2 hyperintensity (similar to T2 intensity of cerebrospinal fluid) within the pituitary adenoma [17], and the adenomas were grouped by the presence of absence of the cystic component. One patient had a 6 mm focus of persistent increased signal on T1 and slightly hypointense T2, which was felt to represent proteinaceous fluid within a cyst by the neuroradiologist and therefore was grouped with tumors containing a cystic component. The maximum cyst diameter, the number of cysts (single or multiple), location, and the percent of the tumor occupied by the cyst(s) were recorded (> 50% or ≤ 50%).
Two neuroradiologists blinded to clinical data utilized T2 sequences to measure signal intensity. In 2 patients, T2 weight imaging was not available, and coronal fluid-attenuated inversion recovery (FLAIR) imaging was utilized as it had similar brain signal characteristics. Three circular regions of interest were placed on the same slice, including over the solid portion of the adenoma, the adjacent mesial temporal grey matter, and the adjacent mesial temporal white matter. The T2 signal intensity value obtained from the solid portion of the adenoma was compared to values for grey and white matter of the temporal lobe [11, 12]. The tumor was then assigned a classification of hypo-, iso-, or hyperintense; hypointense if the intensity of the adenoma was less than both the white and gray matter, isointense if the value was between white and gray matter, and hyperintense if the value was greater than that of white and gray matter.
Biochemical assessment
Insulin-like growth factor-1 and random GH measurements were performed using chemiluminescent immunoassays on an Immulite 2000 analyzer as previously described [5]. The performing laboratory changed in 2016, and the IGF-1 chemiluminescent immunoassay was performed on Diasorin Liaison XL. To account for this change as well as for the age- and sex-related differences, IGF-1 values were expressed as IGF-1 index (IGF-1/upper limit of normal for each patient). Nine patients had IGF-1 performed by a different assay (radioimmunoassay or other) and were not included in the calculation of the baseline mean IGF-1 index.
Prolactin levels were tested using electrochemiluminescence immunoassay on a Roche Cobas analyzer before 2017 and chemiluminescent immunoassay on a Siemens Centaur XP after 2017.
Treatment outcomes
Surgical remission was defined as IGF-1 within normal range for age and sex by 3 months after surgery and a random or nadir GH on oral glucose tolerance test < 1.0 ng/dl [1, 2].
Treatment with first generation SRLs (octreotide or lanreotide) was initiated in patients with elevated IGF-1 (adjusted for sex and age) by 6 months postoperatively and non-suppressed GH to glucose load [1]. The dose of SRL was adjusted as needed to target IGF-1 normalization. Complete SRL response was defined as normalization of IGF-1 within 12 months of therapy. Average IGF-1 reduction was calculated as the difference between absolute IGF-1 before SRL therapy and average IGF-1 during first 12 months of therapy with SRL divided by the pre-SRL IGF-1 value.
Recurrence was defined as an elevated IGF-1 and non-suppressible GH with or without evidence of tumor enlargement after achieving biochemical remission with surgery in patients followed for at least 12 months.
Statistical analysis
Statistical analysis was performed using SPSS25. Analysis of variance (ANOVA) with Bonferroni post hoc analysis was performed for comparison of independent continuous parametric variables (age, maximum tumor diameter, and IGF-1 index). Kruskal–Wallis test with pairwise comparison was used for nonparametric continuous variables (baseline GH, and PRL), ordinal variables (GH staining intensity and SSTR2 staining intensity) and when the sample size was ≤ 10 (maximum % IGF-1 reduction). Student t-test was used for parametric variables and Mann–Whitney test was used for nonparametric and variables with sample size ≤ 10 for comparison between two groups where applicable. Cross tabulation (Pearson chi-square and Fisher’s exact test) was used to evaluate categorical variables. Descriptive statistics were used were applicable. For comparing categorical data in 2 × 3 contingency tables with observed values < 5, a Fisher–Freeman–Halton test was performed using Statxact (Cytel Inc.). Post hoc analysis for categorical data was achieved by assessing 2 × 2 contingency tables. Statistical values of < 0.05 were considered significant. An adjusted p value of 0.0042 was considered significant in the post hoc multi-group comparison of T2 intensity versus granulation pattern.
Results
Demographic characteristics
Seventy-seven patients were included; 19 BA (9 MS and 10 mixed GH-PRL), 30 DGA, and 28 SGA (Table 1). Patients were followed via multimodal treatment for a median of 37.4 months (range 0–192 months). Patients in the BA group were significantly older on average than SGA (mean age 49.6 vs 38.5 years, p = 0.035) and tended to have more females than DGA (73.6% vs 43.6%, p = 0.063).
Tumor characteristics
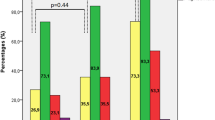
Bihormonal adenomas did not differ in tumor diameter from DGA or SGA and were less frequently invasive than SGA (15.8% vs 57.1%, p = 0.005). Bihormonal adenomas more frequently showed cystic change on MRI compared with SGA and DGA (52.6% vs 14.3% and 22.0%, p = 0.005 and 0.033, respectively). The size of the cystic component varied from < 3 mm (microcysts) to 15.5 mm in the largest diameter; the majority of the cysts were 3–7 mm in diameter. Cysts > 10 mm were observed in 4/10 BA, 2/6 DGA and 0/4 SGA. The number of cysts per tumor varied from single to multiple, and co-occurrence of large (> 10 mm) and multiple smaller cysts were seen in the same tumor in 3/10 BA, 2/10 DGA and 0/4 SGA. Single cystic change was observed in 2/10 BA, 2/6 DGA, and 1/4 SGA. Only 5 tumors had cysts that occupied > 50% of the tumor, including 1 DGA, 1 SGA and 3 BA. Location of the cysts in the tumor was variable without a tendency to occupy a specific part of the tumor. Magnetic resonance images of all cystic pituitary adenomas are shown in Fig. 1.
Analysis of MRI T2 intensity showed that approximately half of BA were isointense, majority of SGA were hyperintense, and DGA had a more variable T2 signal (Table 2). Post hoc analysis revealed that only SGA were associated with T2 hyperintensity (p < 0.001).
Clinical characteristics and treatment outcomes
Bihormonal adenomas had higher baseline IGF-1 index compared to SGA (3.3 vs 2.3, p = 0.040). However, there was no significant difference in random GH levels.
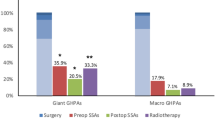
There was no difference in the surgical remission rates across the groups (38.9%, 40.0%, and 50.0%, p = 0.695 in BA, DGA and SGA, respectively).
Twenty-five patients started first generation SRL treatment postoperatively (6 BA, 11 DGA, and 8 SGA). Response rate was 66.7%, 90.9% and 37.5% in BA, DGA and SGA patients, respectively (p = 0.053), with DGA having significantly better responses than SGA (p = 0.041, Table 1). The median IGF-1 reduction in the BA group was 45.1%, which was not statistically different from DGA or SGA.
There was no difference in the recurrence rate across the groups (Table 1). Median time to recurrence was 48.4 (range 28.2–64.9) months. Other characteristics of the groups are also displayed in Table 1.
An analysis comparing MS and mixed GH-PRL adenoma revealed no significant difference in any parameters reviewed (Supplemental Table 1).
Cystic versus non-cystic tumors
Data from this cohort indicated a higher frequency of cystic radiologic features in BA. Histology of the BA cases was reviewed to evaluate for a histological correlate to cysts on radiology. Of the BA with a cystic change on MRI, 4 showed microscopic adenoma-associated cystic spaces containing acellular eosinophilic to slightly basophilic material, and 5 did not have this feature (Fig. 2). One BA with multiple microcysts and a larger cystic change on MRI had prominent papillary architecture, a histologic feature that has been described in association with radiographic cysts in corticotroph adenoma [18] and papillary architecture was not observed in 3 other patients with multimicrocystic radiologic features. Of the BA without cystic change on the MRI, 3 showed microscopic cystic spaces, and 4 did not have this feature. Two BA cases were not available for review, or did not have adequate tissue for detailed histological analysis.
Left BA with a large cyst on MRI (inset) with microscopic cystic spaces containing acellular material (hematoxylin and eosin, scale bar = 100 microns). Right BA with multiple < 3 mm cysts [multimicrocystic pattern] and a large central region of cystic change (inset) with papillary architecture on hematoxylin and eosin staining (scale bar = 200 microns)
When all tumors (BA, DGA, and SGA) were grouped by the presence of cystic component irrespective of their histologic category, cystic tumors were found to have higher GH levels than non-cystic tumors (24.7 vs 5.8 ng/mL, p = 0.014), whereas IGF-1 levels were similar. Surgical remission was more common in the non-cystic tumors (50%) than in cystic tumors (22.5%, p = 0.042, Table 3).
Discussion
We retrospectively examined a large, single center cohort of acromegaly patients, naïve to treatment at presentation to our Center. We focused on clinical features, imaging characteristics and treatment outcome of BA compared to DGA and SGA. In this analysis, the BA group included combined results for both MS and mixed GH-PRL adenomas because precise distinction between the 2 subtypes of BA requires EM or supplementation by double-label pathology staining and currently is not recommended by WHO [4, 7, 19]. We observed that BA resembled DGA in many parameters. Similar to DGA, BA presented at older age, were less invasive, tended to be smaller and had higher IGF-1 index than SGAs.
A novel finding in this series is that a cystic component on radiology was more common in BA compared with SGAs and DGA. To our knowledge, a cystic component has not been examined previously in relation to different histologic types of GH adenomas. This finding has potential implications for patient treatment and monitoring. In general, GH adenomas less commonly contain a cystic change compared to prolactinomas and non-functioning pituitary adenomas (NFPA) [20]. However, the mechanism of cyst formation is not entirely clear and our study did not identify a clear histological correlate to macroscopic cyst formation in this adenoma subtype.
Cystic change is thought to occur in response to ischemia, necrosis, or hemorrhage within the pituitary adenoma [21]. Larger and fast-growing tumors, have more tendency to develop ischemia and necrosis [22]. Uneven blood supply in different parts of pituitary adenoma, particularly in the upper region of the adenoma could predispose to infarction and cyst formation more commonly in that region [21]. In our cohort, BAs tended to be smaller and were less invasive than DGA or SGA, yet more were cystic compared to larger and more aggressive SGAs. The cysts were located in various parts of the tumor and did not have a tendency to be in the specific region of the tumor. Significant necrosis, hemorrhage, or ischemic changes were not observed on histologic examination, suggesting that a mechanism other than ischemia/hemorrhage might be responsible for cystic change in the BAs.
Another mechanism of cyst formation proposed by Horvath and Kovach, is a “misplaced exocytosis” [23]. The postulate is that tumor cells extrude their hormone containing granules in the interstellar space away from capillaries of the pituitary plexus. This may occur due to inadequate amount of blood vessels per number of tumor cells or due to abnormal tumor cell function. Accumulation of these granules is thought to result in formation of the cysts. Ram et al. aspirated fluid from pituitary cysts intraoperatively and examined the fluid for hormone content [24]. They found high concentrations of hormones in the cyst fluid, often with concomitant elevation of other pituitary hormones suggesting mixed secretory pattern in these tumors. Based on this finding, we hypothesized that BA have higher propensity to form cysts by misplaced exocytosis due to their greater secretory potential in the setting of dual hormone expression. When we examined BA histologically, we did not identify a clear histological correlate separating BA with and without radiographic cysts. Future, more detailed histological studies on a larger cohort of BA cases could resolve this issue.
Pseudopapillary dehiscences have been observed on histological examination of corticotroph adenomas (mostly silent type) that had a multimicrocystic pattern on T2 MRI [18, 25]. It was proposed that fluid causes easy dissociation of the smooth and fragile parts of the tumor. In our cohort, a multimicrocyctic radiologic pattern was observed in only 4 tumors in total, and only one such tumor (BA) had a characteristic papillary architecture. This suggests that the association between papillary architecture and multimicrocystic radiology identified in corticotroph adenomas may not necessarily hold for GH adenomas.
Other causes of cyst formation are radiation therapy, long-term bromocriptine therapy, trauma, and steroid administration [26], pregnancy, and anticoagulant therapy, however no patients in our series had such history documented.
The clinical or prognostic significance of a cystic component in pituitary adenomas is uncertain, and it is unclear if such associations will be applicable to all adenomas or only to specific subtypes. Cystic prolactinomas were previously assumed resistant to DA therapy and were primarily treated surgically; however, it has been shown in some studies that treatment is effective with DAs [27]. Less cystic silent corticotroph adenomas are more likely to recur after surgery suggesting that solid corticotroph tumors are more aggressive than cystic tumors [28, 29]. Here, we found that BA were more cystic and exhibited less aggressive radiographic characteristics (i.e. tended to be smaller and were less invasive) compared with SGA, which were less frequently cystic. However, interestingly, when we compared all cystic tumors, irrespective of their histologic type, to non-cystic tumors, cystic tumors had higher preoperative GH levels and lower surgical remission rate, possibly suggesting a higher hormone secreting potential.
Examination of tumor MRI T2 intensity revealed that although the majority of BAs were isointense, this was not statistically significant and there was no association between the type of BA and MRI T2 intensity. It appears that sparse granulation is the major factor determining MRI T2 intensity, however, other factors such as collagen content, fibrosis and amyloid deposition may also play a role (not examined here) [11].
Biochemical response of BA to the first generation SRLs in comparison to DGA and SGA has not been assessed by others, to our knowledge. In our previous study, both BA and SGA seemed to have a poorer response to SRLs however; the sample size was too small to detect the difference [5]. In the current study with a larger sample size, we found that response of the BA group was similar to SGA and DGA despite numerical difference. We believe that this could be due to insufficient sample size and needs further study.
Acknowledging the limitations of a small sample size and lack of EM, we noted no significant difference between MS and mixed GH-PRL tumor characteristics. In previous reports, MS were described as similar to DGA in behavior while mixed GH-PRL adenomas were described as more invasive and resembling more aggressive prolactinomas [19, 30]. This description was based, however on authors’ personal experience and reports with a limited number of patients with MS and mixed GH-PRL tumors [14, 19, 30].
A strength of our retrospective review is that all patients were treatment naïve prior to surgery, thus eliminating a possible confounding effect of SRLs or DAs on granulation [31] or PRL cell staining pattern. All patients were followed in a tertiary Pituitary Center using a uniform protocol. Furthermore, all cases were re-reviewed by a neuropathologist and classified according to current WHO criteria [4] using uniform scoring criteria.
This study has limitations inherent to retrospective analysis; incomplete data sets and shorter follow-up for some patients returning to a local endocrinologist postoperatively. However, median follow up was 37.4 months (range 0–192 months) for this single center study. Changes in the laboratory utilized over time is also a limitation, but the IGF-1 and GH assay type remained the same. The lack of reproducible, uniform histological criteria for BA categorization presents a challenge that could be addressed by future studies.
Conclusion
In this retrospective single center data review, we describe for the first time that BA more often contain a cystic component despite tending to be smaller in size and less invasive. We confirmed that BA have many characteristics similar to DGA such as older age, less tumor invasiveness and higher baseline IGF-1 index, compared to SGA. Cystic tumors in patients with acromegaly, had lower rates of biochemical remission after surgery, regardless of histological subtype. Awareness of this association could help optimize individualized treatment; some patients could be candidates for primary medical treatment if lack of surgical remission is anticipated. Lastly, BA, while not a definite prognosticator for SRL therapy response, may be considered as potentially requiring therapy optimization earlier in disease course (either by escalation of SRL doses or additional combination therapy).
References
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A et al (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):3933–3951. https://doi.org/10.1210/jc.2014-2700
Melmed S (2020) Pituitary-tumor endocrinopathies. N Engl J Med 382(10):937–950. https://doi.org/10.1056/NEJMra1810772
Zahr R, Fleseriu M (2018) Updates in diagnosis and treatment of acromegaly. Eur Endocrinol 14(2):57–61. https://doi.org/10.17925/EE.2018.14.2.57
Lloyd R, Osamura R, Klöppel G, Rosai J (2017) WHO classification of tumours of endocrine organs, 4th edn. International Agency for Research on Cancer, Lyon
Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M (2013) Growth hormone granulation pattern and somatostatin receptor subtype 2A correlate with postoperative somatostatin receptor ligand response in acromegaly: a large single center experience. Pituitary 16(4):490–498. https://doi.org/10.1007/s11102-012-0445-1
Fougner SL, Casar-Borota O, Heck A, Berg JP, Bollerslev J (2012) Adenoma granulation pattern correlates with clinical variables and effect of somatostatin analogue treatment in a large series of patients with acromegaly. Clin Endocrinol (Oxf) 76(1):96–102. https://doi.org/10.1111/j.1365-2265.2011.04163.x
Syro LV, Rotondo F, Serna CA, Ortiz LD, Kovacs K (2017) Pathology of GH-producing pituitary adenomas and GH cell hyperplasia of the pituitary. Pituitary 20(1):84–92. https://doi.org/10.1007/s11102-016-0748-8
Mete O, Asa SL (2012) Clinicopathological correlations in pituitary adenomas. Brain Pathol 22(4):443–453. https://doi.org/10.1111/j.1750-3639.2012.00599.x
Obari A, Sano T, Ohyama K, Kudo E, Qian ZR, Yoneda A et al (2008) Clinicopathological features of growth hormone-producing pituitary adenomas: difference among various types defined by cytokeratin distribution pattern including a transitional form. Endocr Pathol 19(2):82–91. https://doi.org/10.1007/s12022-008-9029-z
Kiseljak-Vassiliades K, Carlson NE, Borges MT, Kleinschmidt-DeMasters BK, Lillehei KO, Kerr JM et al (2015) Growth hormone tumor histological subtypes predict response to surgical and medical therapy. Endocrine 49(1):231–241. https://doi.org/10.1007/s12020-014-0383-y
Hagiwara A, Inoue Y, Wakasa K, Haba T, Tashiro T, Miyamoto T (2003) Comparison of growth hormone-producing and non-growth hormone-producing pituitary adenomas: imaging characteristics and pathologic correlation. Radiology 228(2):533–538. https://doi.org/10.1148/radiol.2282020695
Heck A, Ringstad G, Fougner SL, Casar-Borota O, Nome T, Ramm-Pettersen J et al (2012) Intensity of pituitary adenoma on T2-weighted magnetic resonance imaging predicts the response to octreotide treatment in newly diagnosed acromegaly. Clin Endocrinol (Oxf) 77(1):72–78. https://doi.org/10.1111/j.1365-2265.2011.04286.x
Dogansen SC, Yalin GY, Tanrikulu S, Tekin S, Nizam N, Bilgic B et al (2018) Clinicopathological significance of baseline T2-weighted signal intensity in functional pituitary adenomas. Pituitary 21(4):347–354. https://doi.org/10.1007/s11102-018-0877-3
Kreutzer J, Vance ML, Lopes MB, Laws ER Jr (2001) Surgical management of GH-secreting pituitary adenomas: an outcome study using modern remission criteria. J Clin Endocrinol Metab 86(9):4072–4077. https://doi.org/10.1210/jcem.86.9.7819
Rick J, Jahangiri A, Flanigan PM, Chandra A, Kunwar S, Blevins L et al (2018) Growth hormone and prolactin-staining tumors causing acromegaly: a retrospective review of clinical presentations and surgical outcomes. J Neurosurg 131(1):147–153. https://doi.org/10.3171/2018.4.JNS18230
Lv L, Jiang Y, Yin S, Hu Y, Chen C, Ma W et al (2019) Mammosomatotroph and mixed somatotroph-lactotroph adenoma in acromegaly: a retrospective study with long-term follow-up. Endocrine 66(2):310–318. https://doi.org/10.1007/s12020-019-02029-1
Bonneville J-F, Bonneville F, Cattin F, Nagi S (2016) MRI of the pituitary gland. Springer International Publishing, Cham
Cazabat L, Dupuy M, Boulin A, Bernier M, Baussart B, Foubert L et al (2014) Silent, but not unseen: multimicrocystic aspect on T2-weighted MRI in silent corticotroph adenomas. Clin Endocrinol (Oxf) 81(4):566–572. https://doi.org/10.1111/cen.12443
Lopes MB (2010) Growth hormone-secreting adenomas: pathology and cell biology. Neurosurg Focus 29(4):E2. https://doi.org/10.3171/2010.7.FOCUS10169
Lundin P, Nyman R, Burman P, Lundberg PO, Muhr C (1992) MRI of pituitary macroadenomas with reference to hormonal activity. Neuroradiology 34(1):43–51. https://doi.org/10.1007/BF00588432
Zhang J, Gu J, Ma Y, Huang Y, Wang J, Wu Z et al (2017) Uneven distribution of regional blood supply prompts the cystic change of pituitary adenoma. World Neurosurg 103:37–44. https://doi.org/10.1016/j.wneu.2017.03.109
Liu ZH, Tu PH, Pai PC, Chen NY, Lee ST, Chuang CC (2012) Predisposing factors of pituitary hemorrhage. Eur J Neurol 19(5):733–738. https://doi.org/10.1111/j.1468-1331.2011.03619.x
Horvath E, Kovacs K (1974) Misplaced exocytosis. Distinct ultrastructural feature in some pituitary adenomas. Arch Pathol 97(4):221–224
Ram Z, Hadani M, Berezin M, Findler G, Sahar A, Shacked I (1989) Intratumoural cyst formation in pituitary macroadenomas. Acta Neurochir (Wien) 100(1–2):56–61. https://doi.org/10.1007/BF01405275
Kasuki L, Antunes X, Coelho MCA, Lamback EB, Galvao S, Silva Camacho AH et al (2020) Accuracy of microcystic aspect on T2-weighted MRI for the diagnosis of silent corticotroph adenomas. Clin Endocrinol (Oxf) 92(2):145–149. https://doi.org/10.1111/cen.14133
Bahuleyan B, Menon G, Nair S, Rao BRM, Easwer HV, Krishna K (2009) Non-surgical management of cystic prolactinomas. J Clin Neurosci 16(11):1421–1424. https://doi.org/10.1016/j.jocn.2009.03.024
Faje A, Chunharojrith P, Nency J, Biller BM, Swearingen B, Klibanski A (2016) Dopamine agonists can reduce cystic prolactinomas. J Clin Endocrinol Metab 101(10):3709–3715. https://doi.org/10.1210/jc.2016-2008
Cho HY, Cho SW, Kim SW, Shin CS, Park KS, Kim SY (2010) Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin Endocrinol (Oxf) 72(5):648–653. https://doi.org/10.1111/j.1365-2265.2009.03673.x
Langlois F, Lim DST, Yedinak CG, Cetas I, McCartney S, Cetas J et al (2018) Predictors of silent corticotroph adenoma recurrence; a large retrospective single center study and systematic literature review. Pituitary 21(1):32–40. https://doi.org/10.1007/s11102-017-0844-4
Horvath E, Kovacs K (2006) Pathology of acromegaly. Neuroendocrinology 83(3–4):161–165. https://doi.org/10.1159/000095524
Ezzat S, Horvath E, Harris AG, Kovacs K (1994) Morphological effects of octreotide on growth hormone-producing pituitary adenomas. J Clin Endocrinol Metab 79(1):113–118. https://doi.org/10.1210/jcem.79.1.8027215
Acknowledgements
The authors thank Shirley McCartney, Ph.D. for editorial assistance.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MF reports serving as an investigator with research grants to Oregon Health & Science University (OHSU) for Chiasma, Crinetics, Ionis; and serving as an occasional consultant to Chiasma, Crinetics, Ionis, Pfizer. All other authors have no conflict to report.
Ethics approval
Institutional Review Board approval was received.
Informed consent
A waiver of subject consent was approved. All authors approve the submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Varlamov, E.V., Wood, M.D., Netto, J.P. et al. Cystic appearance on magnetic resonance imaging in bihormonal growth hormone and prolactin tumors in acromegaly. Pituitary 23, 672–680 (2020). https://doi.org/10.1007/s11102-020-01075-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-020-01075-7