Abstract
Purpose
Silent corticotroph adenomas (SCAs) are clinically silent and non-secreting, but exhibit positive adrenocorticotropic hormone (ACTH) immunostaining. We characterized a single center cohort of SCA patients, compared the SCAs to silent gonadotroph adenomas (SGAs), identified predictors of recurrence, and reviewed and compared the cohort to previously published SCAs cases.
Methods
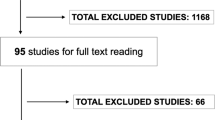
Retrospective review of SCA and SGA surgically resected patients over 10 years and 6 years, respectively. Definitions; SCA—no clinical or biochemical evidence of Cushing’s syndrome and ACTH positive immunostaining, and SGA—steroidogenic factor (SF-1) positive immunostaining. A systematic literature search was undertaken using Pubmed and Scopus.
Results
Review revealed 814 pituitary surgeries, 39 (4.8%) were SCAs. Mean follow-up was 6.4 years (range 0.5–23.8 years). Pre-operative magnetic resonance imaging demonstrated sphenoid and/or cavernous sinus invasion in 44%, 33% were > 50% cystic, and 28% had high ACTH levels pre-operatively. Compared to SGAs (n = 70), SCAs were of similar size and invasiveness (2.5 vs. 2.9 cm, p = 0.2; 44 vs. 41%, p = 0.8, respectively), but recurrence rate was higher (36 vs. 10%, p = 0.001) and more patients received radiation therapy (18 vs. 3%, p = 0.006). Less cystic tumors (0 vs. 50%, p < 0.001) and higher pre-operative ACTH levels (54 vs. 28 pg/ml, p = 0.04) were predictors of recurrence for SCAs.
Conclusion
This review is unique; a strict definition of SCA was used, and single center SCAs were compared with SGAs and with SCAs literature reviewed cases. We show that SCAs are aggressive and identify predictors of recurrence. Accurate initial diagnosis, close imaging and biochemical follow up are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First reported in late 1970s [1, 2], silent corticotroph adenomas (SCAs) are a distinct subtype of pituitary adenomas that represent approximately 20% of all corticotroph adenomas and approximately 5% [3] (3–19% depending on series) of non-functioning adenomas [4]. SCAs are defined as tumors with no biochemical hypercortisolism, no clinical evidence of Cushing’s disease (CD), and evidence of tumor immunoreactivity for adrenocorticotropic hormone (ACTH). Since there is no evidence of hypersecretion syndrome, SCAs tend to present as larger tumors with mass effects, such as headache and visual symptoms [4]. They constitute a diagnostic challenge as most are diagnosed post-resection and confirmation of preoperative clinical ACTH hypersecretion status cannot always be ascertained.
Published literature on clinical characteristics and outcome of SCAs is variable and cases include a range of different tumors, with variable clinical presentations and pathologic characteristics. Some studies, but not all, have demonstrated that SCAs have a more aggressive course with higher risk of recurrence than other non-functioning tumors [5,6,7,8,9].
Rigorous retrospective review of our center’s pre-operative evaluation and diagnosis, characteristics and outcome of SCAs, determination of predictors of recurrences, comparison to a series of silent gonadotroph adenomas (SGAs) resected at our center, and comparison to previously published SCAs, is presented.
Patients and methods
A retrospective, Institutional Review Board approved analysis of patients who underwent resection of a pituitary adenoma at Oregon Health & Science University (OHSU) over 10 years (June 2006 to June 2016) was undertaken. Patients had been clinically assessed using a unified protocol.
Clinical characteristics and definitions
Charts were retrospectively reviewed by one neuroendocrinologist and if there was ambiguous diagnostic information, a second opinion from another neuroendocrinologist was obtained. Hormonal evaluation and clinical assessment were obtained at baseline preoperatively, repeated at 1–3 months postoperatively, and regularly at scheduled interval based on a unified protocol by a single neuroendocrinologist. Central adrenal insufficiency (AI) diagnosis was based on clinical evaluation, baseline morning cortisol, ACTH levels and/or abnormal response to 1 µg ACTH stimulation test (30 min stimulated cortisol < 16–18 µg/dL). Central hypothyroidism was defined as low free thyroxine and low or normal thyroid stimulating hormone (TSH). Central hypogonadism was defined in men as low testosterone and low or normal follicle stimulating hormone (FSH) and luteinizing hormone (LH), in premenopausal women as oligo- or amenorrhea, low estradiol, and low or normal FSH and LH, and in post-menopausal women as lower LH and FSH than the reference range for post-menopausal status. Growth hormone (GH) deficiency was based on low insulin-like growth factor 1 (IGF-1) in patients with multiple pituitary deficiencies. GH stimulation tests were not routinely performed unless there was clinical indication. Hyperprolactinemia was defined as prolactin elevation above the normal range for sex. Hypopituitarism was defined as presence of two or more deficiencies in adenohypophyseal hormones. Biochemical work-up for CD for patients with elevated ACTH preoperatively and all patients (in the absence of AI) postoperatively included either one or combination of tests; urine free cortisol (UFC), salivary cortisol, overnight dexamethasone (DEX) suppression test and DEX/corticotropin-releasing hormone (CRH) as a confirmatory testing in selected cases. Radiological invasion was defined as either cavernous and/or sphenoid sinus invasion. Postoperative evaluation also included magnetic resonance imaging (MRI) at 3 months post-surgery, and gross surgical cure was defined as no residual tumor on MRI. Recurrence was defined as progression of a residual tumor or new tumor growth after total resection.
Pathology was confirmed by one of three dedicated pituitary neuropathologists. We based tumor classification on immunochemistry. Adenoma immunohistochemical staining was performed using an automated immunohistochemical system (Benchmark XT, Ventana Medical Systems Inc., Tuscon, AZ, USA) with the following antibodies: ACTH, GH, PRL, Ki-67 (Ventana), SF-1 (ThermoFisher Scientific), cytokeratin CAM 5.2 (Beckton, Dickinson and Company, Franklin Lakes, NJ, USA) and SSTR2A (Gramsch Laboratories, Germany). ACTH, GH, PRL, SF-1 (from years 2011–2016), cytokeratin (CAM5.2), Ki-67 and p53 staining were routinely assessed; TSH and somatostatin receptor 2A (SSTR2A) were selectively stained as needed. Electron microscopy (EM) was available for selected cases.
Silent corticotroph adenomas
Patients were classified as having a SCA as follows; patient exhibited less than two signs or symptoms compatible with hypercortisolism, and most importantly, no biochemical hypercortisolism preoperatively. In patients found to have normal or elevated baseline ACTH levels, biochemical evaluation was pursued to exclude CD. Plurihormonal tumors were excluded. Cystic tumors were defined based on imaging as tumors with > 50% fluid content based on MRI T2 signal.
Silent gonadotroph adenomas
A group of patients with SGAs, resected at our center over 6 years (2011 to 2016; steroidogenic factor (SF-1) immunostaining was available only from 2011) by two dedicated pituitary neurosurgeons, was reviewed for comparisons with SCAs.
Literature review
A systematic literature search was undertaken using Pubmed and Scopus; using the following terms [silent/non-functioning, ACTH/corticotroph/Cushing’s, adenomas/tumors] for articles published from 1970 to 2016. Cited references within articles were also searched for relevancy to the topic. Clinical characteristics and outcome data of published cases were compared to our SCAs cohort.
Statistical analysis
A 2-tailed Student t test was used to perform parametric comparison between two variables with equal variances. Mann–Whitney rank sum test analyzed nonparametric comparisons for ACTH levels and Chi square test was used to compare categorical variables such as sex, cystic and invasiveness. A regression analysis was performed to define the relationship between variables for SCAs and SGAs. To analyze literature data, we used weighted average for continuous variables and percentage of occurrence of ordinal variables. Statistics were calculated using PASW 18 (IBM, Corp. Armonk, NY). P values were considered significant at < 0.05.
Results
Retrospective review revealed 814 pituitary surgeries in the 10-year time period specified, 39 of which were SCAs; prevalence was 4.8%. Mean age at diagnosis was 50 ± 14 years with no gender predominance (54% female). Additional patient characteristics are presented in Table 1 alongside previously published data [1, 2, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65].
In our patient cohort, the majority presented with headaches (59%) and/or visual symptoms (49%). Pre-operative MRI demonstrated that 90% (35/39) were macroadenomas with a mean tumor size of 2.5 cm. Sphenoid and/or cavernous sinus invasion was described in 44% and a third were mostly cystic (> 50% fluid content). Biochemical evaluation revealed that even though patients did not have biochemical evidence of hypercortisolism, 28% had elevated baseline ACTH. A quarter of the cohort also had mild hyperprolactinemia and 22% had hypopituitarism. The most frequent deficits were IGF-1 and gonadotrophins, as expected with macroadenomas. Baseline AI was present in only two patients and post-operatively, 23% developed new AI.
All tumors had low Ki-67 (< 3%) and one tumor expressed p53 (with no recurrence). Only one patient had a transformation in tumor with high proliferation index of 6% and p53 positivity at its last recurrence (5th surgery). ACTH staining was strong in 6 tumors and weak in 17 tumors; for the others (16/39), ACTH immunostaining was reported as present.
SCA patients were followed for a mean of 6.4 ± 5.9 years. Only 42% of patients achieved gross surgical cure. 14 of 39 patients (36%) recurred at a mean of 44 ± 37 months (range 3–132 months) and 18% had multiples recurrences. Most recurrences (11/14) were treated surgically; six patients underwent a second intervention, three patients had three resections, one patient four surgeries and one patient underwent five surgical resections (over 16 years, the three last interventions were conducted at our center). Seven patients (18%) received adjuvant radiotherapy, and 2 (5%) patients received temozolomide-based chemotherapy; of those, one patient had an impressive reduction in tumoral mass with a 60% reduction in the first 3 months leading to visual improvement; the other patient died from another primary cancer in the following year. No patient died because of tumor progression, nor experienced transformation to a corticotroph carcinoma. During the follow-up period, one patient switched phenotype from a silent adenoma to CD 5 months after a first surgery and one patient had a previously secreting tumor that became silent on a fourth recurrence (9 years post-diagnosis) before receiving radiation therapy. Both patients also had recurrent tumors.
Compared to SGAs, SCAs had similar tumor size (2.5 vs. 2.9 cm; not significant) and invasiveness (44 vs. 41%; not significant) but a threefold higher recurrence rate (36 vs. 10%, p = 0.001). Radiation therapy was performed in 18% of SCAs versus 3% of SGAs (p = 0.006, Table 2).
When comparing recurrent SCAs versus non-recurrent SCAs, an association between recurrence and tumor size (3.2 vs. 2.1 cm, p = 0.019), and cavernous and/or sphenoid sinus invasion (79 vs. 25%, p = 0.001) was found (Table 3). Of note, on regression analysis, patients with cavernous sinus invasion were three times more likely to have recurrence (p = 0.006).
None of the patients with recurrent SCAs had cystic tumors (0 vs. 50%, p < 0.001), however, higher baseline ACTH levels were significantly associated with recurrence (54 vs. 28 pg/ml, p = 0.04). Although in our sample more recurrence occurred in males, this was not statistically significant, within our small recurrence sample (62 vs. 33%, p = 0.09). Likewise, there was no relationship with recurrence and age at diagnosis. Post-surgical AI onset was not found in patients with tumor recurrence compared to 35% of those with non-recurrent tumors (p < 0.001, Table 3).
Discussion
In this retrospective single institution cohort review with a uniform definition of silent tumors and long follow-up period, we confirmed that SCAs are aggressive tumors with a recurrence rate of 36% over 6 years. In studies with smaller number of patients and/or shorter follow up periods, recurrence rates are reportedly 25 to 42% [6,7,8,9, 34]. The review is unique in that new insights regarding predictors of recurrence are noted and discussed. Higher baseline ACTH levels and less cystic tumors are novel characteristics to make note of and may play an important role in patient management as they may indicate a worse prognosis in terms of recurrence. As noted, no cystic tumors were found to have recurred during follow-up. Interestingly, proliferation indices were not predictors of recurrence, as almost all tumors expressed low Ki67, concordant with previously published series data [5, 9]. Age was not identified as a predictor of recurrence, however mean age in the cohort (50.0 ± 14.2 years) was similar to the published literature, but older than the series by Cho et al., that showed that young patients (< 30 years of age) with SCA were most likely to recur [7]. Compared to SGAs treated in the same institution, SCAs were three times more likely to recur and had a sixfold increase in need for radiation therapy. Different follow-up periods could have influenced the observed outcome comparing SCAs to SGAs, however, clinically relevant differences and a shorter time interval to recurrence for SCAs versus SGAs were observed.
SCAs in this single institution cohort were slightly less prevalent than that reported in the literature (4.8 vs. 6.8%, respectively) but with a similar epidemiological profile (Table 1). The clinical presentations observed were mostly symptoms of mass effect (headaches and visual symptoms) and rarely oligomenorrhea/galactorrhea. Tumor size was large as previously published [4], however with the inherent bias of a surgical-based cohort where microadenomas are usually poorly represented. Only one patient presented with apoplexy, which is much less than that reported in previously published series (2.6 vs. 12.5% p = 0.006) [11]. We hypothesize that this difference could be due either to selection or reporting bias since most published cases were diagnosed during a symptomatic event such as acute apoplexy. The review we present included post-operative tumors in the contemporary setting of high definition imaging and increased detection, so a higher number were diagnosed during investigation of headaches or in completely asymptomatic patients. Moreover, fewer had elevated baseline ACTH levels compared to published cases and case-series, but clinical presentation of SCA in the literature review may be tainted by cases of subclinical CD.
In the cohort described, all patients defined as having a SCA had undergone a complete biochemical evaluation and CD had been ruled out prior to surgery. Since a SCA diagnosis is established post-operatively, it is possible that for some published cases mild early CD may have been present pre-operatively if a full biochemical work up was not completed. There also may be an overlap between silent ACTH and cyclical CD and some SCAs may be a form of CD with very low cyclicity or represent the controversial subcategory of cyclic and subclinical CD [66]. The longest intercyclic interval reported was 4.5 years [67]. Notably, we place emphasis on the clinical importance of measuring pre-operatively ACTH levels and on pursuing investigation of subclinical CD as needed. Diagnostic clarification is important as additional baseline investigations can help determine if the tumor secretes bioactive ACTH, thus modifying perioperative management and anticipating AI postoperatively. A more stringent sequential imaging and hormonal testing plan can also be made.
Notably, in our cohort of SCA patients, a wide spectrum of presentations was seen, from totally silent tumors with low secreting ability, to ACTH elevation without hypercortisolism, to very aggressive tumors requiring multimodal therapies. We hypothesize that SCAs, usually classified based on pathology as subtype 1 (strong ACTH immunostaining) and subtype 2 (weak ACTH immunostaining) are derived from two different populations.
On the one hand, preoperative ACTH levels indicate that one-quarter of SCAs secrete biologically inactive ACTH, and higher circulating ACTH levels could be a marker of a more aggressive subset of SCA. These tumors could represent poorly differentiated tumors arising from the Prop-1 lineage with less secretory ability, but with the potential for phenotypic change and recurrence over time. They may relate to SCA subtype 1 with strong ACTH immunopositivity, and previously reported to be more aggressive by Jahangiri et al. [34]. In our cohort, strong ACTH immunostaining was observed as twofold more prevalent in the recurrent compared to the non-recurrent group. Temozolomide might be an additional therapeutic option in very aggressive SCAs [68].
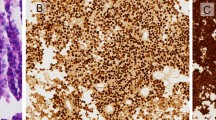
On the other hand, publications by Horvath and colleagues, suggest that SCA arise from the pars intermedia, as corticotrophs of the pars intermedia have low ACTH secretion activity [69], and Kasuki et al. showed that a high proportion of SCAs have a microcystic aspect [18, 70]. In our cohort, weak ACTH immunostaining was present in 12/15 (80%) of the non-recurrent group. In line with the results we present, some SCAs may originate from the pars intermedia cells, as one-third were predominantly cystic and none of these tumors recurred. This subgroup could account for more indolent tumors that may have the pathologic appearance of subtype 2 and weakly express ACTH immunopositivity (Fig. 1). In our cohort, as well as in a large German registry [3], SCA subtype 2 were 2–4 times more prevalent than their densely-granulated (subtype 1, more aggressive) counterpart.
Representative magnetic resonance imaging (MRI) SCAs cases. a MRI T1 gadolinium positive, recurrent SCA case in a 58 year-old male with a solid tumor, pre-operative ACTH 168 pg/ml, strong tumoral ACTH immunoreactivity and poorly differentiated corticotroph cells. b MRI T2, non-recurrent SCA case in a 46 year-old female with a cystic tumor, pre-operative ACTH 6 pg/ml, weak tumoral ACTH immunoreactivity, and pars intermedia-derived corticotroph cells
Here we also show that SCAs have the potential to change phenotype over time, which is in agreement with previous publications [9, 13, 17, 27, 59, 60, 68], and as such requires further study. Many pathogenic processes have been identified and help explain SCA phenotype. First, low or absent biologic activity of ACTH can result from alteration in hormone processing, and more specifically from a deficit in prohormone convertase 1/3 (PC1/3) [34, 42, 45, 53]. Even in CD, larger tumors have been shown to less efficiently process proopiomelanocortin (POMC) to ACTH compared to microadenomas [28]. Righi et al. recently demonstrated that PC1/3 activity was acquired in tumors of patients changing from silent to active CD over time [47]. Another hypothesis is the secretion of fragments of ACTH-POMC, or high molecular weight ACTH, by the tumor, resulting in cross reactivity with the ACTH immunoassay [46, 58]. Fluctuation from silent to clinical disease has also been demonstrated in somatotroph adenomas resulting in silent to clinical acromegaly [71]. Changing phenotype has also been related to radiotherapy in some cases [40], this could be via direct radiation-induced changes in the tumor, or could also be an indirect relationship associated with more aggressive tumors. In our cohort, the change in phenotype cannot be attributed to radiotherapy, since the two patients who experienced a change in phenotype did not receive previous radiation therapy.
Role of tissue specific transcription factors, more specifically T-pit, has also been implicated in phenotypic silence. T-pit plays an important role in pathways of cellular differentiation, directing cells towards corticotroph differentiation, and T-pit dysfunction could be an early abnormality leading to development of a SCA. However, T-pit testing yielded variable and inconclusive results in SCAs [72].
Some authors have hypothesized that silent ACTH tumors overlap with gonadotrophs, since they harbor SF-1 positivity, honeycomb golgi and increased mitochondrial density [22]. Others conclude that honeycomb golgi might be a non-specific marker of non-functionality [59, 73]. In our cohort, we have not been able to study SF-1 extensively (only routinely available from 2011), but SF-1 was absent in a third (0/13) of the SCA cohort tested, arguing against a common tumor origin.
Expression of genes implicated in tumorigenesis seems increased in silent ACTH tumors compared to their non-functional counterparts. Galectin-3 gene is mutated in a series of SCAs and its protein, functioning as an oncogene, promotes tumorigenesis and is associated with tumor aggressiveness (e.g. increased expression in carcinomas) [74, 75]. Other proteins implicated in extra-cellular matrix interaction have been associated with SCAs versus non-functioning pituitary adenomas; higher expression of beta 1 integrin and osteopontin (as determined by immunostaining), which promote cell motility and migration and high fibroblast growth factor receptor-4/matrix metallopeptidase 1 (FGFR4/MMP-1) profile has been related to more tumoral invasiveness [76]. With the advent of directed enzyme prodrug therapy, specific protein targeting could be a potential future therapeutic option.
Limitations of this study include the retrospective design in a tertiary center study with inherent referral bias. Specific tumor subtyping was not reported by neuropathologists until 2011. Transcription factors or mRNA measurements were not available as routine clinical studies, but ACTH staining was determined by dedicated neuropathologists. Study strengths are a unified clinical and biochemical evaluation for both hypopituitarism and CD by one dedicated neuroendocrinologist, routine follow-up protocol for all patients and MRI readings by dedicated neuroradiologists.
Conclusion
We show for the first time that patients with recurrent SCAs had less cystic tumors and higher pre-operative ACTH levels than those with non-recurrent SCA tumors. Furthermore, though SCAs are overall rare pituitary adenomas, they have potentially aggressive behavior and can switch phenotype over time, mandating accurate initial diagnosis, close imaging and biochemical follow up. Further large multicenter research studies are needed to elucidate the epidemiology and biology of SCAs.
References
Horvath E, Kovacs K, Killinger DW, Smyth HS, Platts ME, Singer W (1980) Silent corticotropic adenomas of the human pituitary gland: a histologic, immunocytologic, and ultrastructural study. Am J Pathol 98(3):617–638
Kovacs K, Horvath E, Bayley TA, Hassaram ST, Ezrin C (1978) Silent corticotroph cell adenoma with lysosomal accumulation and crinophagy. A distinct clinicopathologic entity. Am J Med 64(3):492–499
Saeger W, Ludecke DK, Buchfelder M, Fahlbusch R, Quabbe HJ, Petersenn S (2007) Pathohistological classification of pituitary tumors: 10 years of experience with the German Pituitary Tumor Registry. Eur J Endocrinol 156(2):203–216
Cooper O (2015) Silent corticotroph adenomas. Pituitary 18(2):225–231
Scheithauer BW, Jaap AJ, Horvath E, Kovacs K, Lloyd RV, Meyer FB, Laws ER Jr, Young WF Jr (2000) Clinically silent corticotroph tumors of the pituitary gland. Neurosurgery 47(3):723–729
Webb KM, Laurent JJ, Okonkwo DO, Lopes MB, Vance ML, Laws ER (2003) Clinical characteristics of silent corticotrophic adenomas and creation of an internet-accessible database to facilitate their multi-institutional study. Neurosurgery 53(5):1076–1085
Cho HY, Cho SW, Kim SW, Shin CS, Park KS, Kim SY (2010) Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin Endocrinol 72(5):648–653
Bradley KJ, Wass JA, Turner HE (2003) Non-functioning pituitary adenomas with positive immunoreactivity for ACTH behave more aggressively than ACTH immunonegative tumours but do not recur more frequently. Clin Endocrinol 58(1):59–64
Baldeweg SE, Pollock JR, Powell M, Ahlquist J (2005) A spectrum of behaviour in silent corticotroph pituitary adenomas. Br J Neurosurg 19(1):38–42
Abe M, Sawabe Y, Mochizuki Y, Sunaga S, Izumiyama H, Matsumoto K, Kushima M, Taniyama M, Ban Y, Sano T (2001) Corticotroph cell adenoma without typical manifestations of Cushing’s disease presenting with cavernous sinus syndrome following pituitary apoplexy. Endocr J 48(4):503–507
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F, Asa SL, Zadeh G (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir 154(8):1493–1498
Al-Sarraj S, King A, Harris P, Lantos P (2002) Atypical pituitary adenoma (silent corticotroph pituitary adenoma). Neuropathol Appl Neurobiol 28(2):157–158
Ambrosi B, Colombo P, Bochicchio D, Bassetti M, Masini B, Faglia G (1992) The silent corticotropinoma: is clinical diagnosis possible? J Endocrinol Invest 15(6):443–452
Benaiges D, Puig J, Lafuente J, Gimeno J, Prados M, Sagarra E, Flores-Le-Roux J (2012) Biochemical behaviour of an incidentally diagnosed silent corticotroph adenoma. Neuro Endocrinol Lett 33(3):290–293
Bordo G, Duong H, McLaughlin N, Cornell R, Findling J, Kelly D (2012) Case report: silent corticotroph adenoma progressing to cushing’s disease then to pituitary carcinoma with dramatic treatment response. J Neurol Surg Part B 73:02
Braithwaite SS, Clasen RA, D’Angelo CM (1997) Silent corticotroph adenoma: case report and literature review. Endocr Pract 3(5):297–301
Brown RL, Wollman R, Weiss RE (2007) Transformation of a pituitary macroadenoma into to a corticotropin-secreting carcinoma over 16 years. Endocr Pract 13(5):463–471
Cazabat L, Dupuy M, Boulin A, Bernier M, Baussart B, Foubert L, Raffin-Sanson ML, Caron P, Bertherat J, Gaillard S (2014) Silent, but not unseen: multimicrocystic aspect on T2-weighted MRI in silent corticotroph adenomas. Clin Endocrinol 81(4):566–572
Chen SC, Chung WY (2015) Progression rate of silent corticotroph adenomas after stereotactic radiosurgery. In regard to Xu et al. Int J Radiat Oncol Biol Phys 91(5):1113–1114
Coire CI, Horvath E, Kovacs K, Smyth HS, Sasano H, Iino K, Feig DS (1998) A composite silent corticotroph pituitary adenoma with interspersed adrenocortical cells: case report. Neurosurgery 42(3):650–654
Cooper ME, Murray RM, Kalnins R, Woodward J, Jerums G (1987) The development of Cushing’s syndrome from a previously silent pituitary tumour. Aust N Z J Med 17(2):249–251
Cooper O, Ben-Shlomo A, Bonert V, Bannykh S, Mirocha J, Melmed S (2010) Silent corticogonadotroph adenomas: clinical and cellular characteristics and long-term outcomes. Horm Cancer 1(2):80–92
Fang H, Tian R, Wu H, Xu J, Fan H, Zhou J, Zhong L (2015) Cushing disease after treatment of nonfunctional pituitary adenoma: a case report and literature review. Medicine 94(51):e2134
Farrell WE, Coll AP, Clayton RN, Harris PE (2003) Corticotroph carcinoma presenting as a silent corticotroph adenoma. Pituitary 6(1):41–47
Felix I, Asa SL, Kovacs K, Horvath E (1991) Changes in hormone production of a recurrent silent corticotroph adenoma of the pituitary: a histologic, immunohistochemical, ultrastructural, and tissue culture study. Hum Pathol 22(7):719–721
Gheri RG, Boddi W, Ammannati F, Olivotto J, Nozzoli C, Franchi A, Bordi L, Luisi ML, Mennonna P (1997) Two-step development of a pituitary adenoma: from hyperprolactinemic syndrome to Cushing’s disease. J Endocrinol Invest 20(4):240–244
Ghervan C (2014) Silent corticotroph adenoma transformed in secreting adenoma with severe Cushing’s disease after two pituitary surgeries. Acta Endocrinol 10(2):283–292
Gibson S, Ray DW, Crosby SR, Dornan TL, Jennings AM, Bevan JS, Davis JR, White A (1996) Impaired processing of proopiomelanocortin in corticotroph macroadenomas. J Clin Endocrinol Metab 81(2):497–502
Gogel EL, Salber PR, Tyrrell JB, Rosenblum ML, Findling JW (1983) Cushing’s disease in a patient with a ‘nonfunctioning’ pituitary tumor: spontaneous development and remission. Arch Intern Med 143(5):1040–1042
Guttenberg KB, Mayson SE, Sawan C, Kharlip J, Lee JY, Martinez-Lage M, Loevner LA, Ewanichak J, Grady MS, Snyder PJ (2016) Prevalence of clinically silent corticotroph macroadenomas. Clin Endocrinol 85(6):874–880
He L, Forbes JA, Carr K, Highfield Nickols H, Utz A, Moots P, Weaver K (2016) Response of silent corticotroph pituitary carcinoma to chemotherapy: case report. J Neurosurg Sci 60(2):272–280
Ikeda H, Yoshimoto T, Kovacs K, Horvath E (1995) Cushing’s disease due to female gonadotroph adenoma of the pituitary. Clin Endocrinol 43(3):383–386
Ioachimescu AG, Eiland L, Chhabra VS, Mastrogianakis GM, Schniederjan MJ, Brat D, Pileggi AV, Oyesiku NM (2012) Silent corticotroph adenomas: Emory University cohort and comparison with ACTH-negative nonfunctioning pituitary adenomas. Neurosurgery 71(2):296–303
Jahangiri A, Wagner JR, Pekmezci M, Hiniker A, Chang EF, Kunwar S, Blevins L, Aghi MK (2013) A comprehensive long-term retrospective analysis of silent corticotrophic adenomas vs hormone-negative adenomas. Neurosurgery 73(1):8–17
Kojima Y, Suzuki S, Yamamura K, Ohhashi G, Yamamoto I (2002) Comparison of ACTH secretion in Cushing’s adenoma and clinically silent corticotroph adenoma by cell immunoblot assay. Endocr J 49(3):285–292
Iino K, Oki Y, Matsushita F, Yamashita M, Hayashi C, Miura K, Nishizawa S, Nakamura H (2007) Immunohistochemical properties of silent corticotroph adenoma and Cushing’s disease. Pituitary 10(1):35–45
Lipatenkova A, Dzeranova L, Pigarova E, Ektova A (2014) Clinical case: silent corticotroph pituitary macroadenoma transforming into Cushing disease. Endocr Abstr. doi:10.1530/endoabs.35.P915
Lopez JA, Kleinschmidt-Demasters BK, Sze C-I, Woodmansee WW, Lillehei KO (2004) Silent corticotroph adenomas: Further clinical and pathological observations. Hum Pathol 35(9):1137–1147
Matsuno A, Okazaki R, Oki Y, Nagashima T (2004) Secretion of high-molecular-weight adrenocorticotropic hormone from a pituitary adenoma in a patient without Cushing stigmata: case report. J Neurosurg 101(5):874–877
Mindermann T, Kovacs K, Wilson CB (1994) Changes in the immunophenotype of recurrent pituitary adenomas. Neurosurgery 35(1):39–44
Moshkin O, Syro LV, Scheithauer BW, Ortiz LD, Fadul CE, Uribe H, Gonzalez R, Cusimano M, Horvath E, Rotondo F, Kovacs K (2011) Aggressive silent corticotroph adenoma progressing to pituitary carcinoma: the role of temozolomide therapy. Hormones 10(2):162–167
Ohta S, Nishizawa S, Oki Y, Yokoyama T, Namba H (2002) Significance of absent prohormone convertase 1/3 in inducing clinically silent corticotroph pituitary adenoma of subtype I–immunohistochemical study. Pituitary 5(4):221–223
Pawlikowski M, Kunert-Radek J, Radek M (2008) “Silent" corticotropinoma. Neuro Endocrinol Lett 29(3):347–350
Psaras T, Honegger J, Buslei R, Saeger W, Klein D, Capper D, Meyermann R, Mittelbronn M (2007) Atypical type II silent corticotrophic adenoma developing into Cushing’s disease upon second recurrence. Exp Clin Endocrinol Diabetes 115(9):610–615
Raverot G, Wierinckx A, Jouanneau E, Auger C, Borson-Chazot F, Lachuer J, Pugeat M, Trouillas J (2010) Clinical, hormonal and molecular characterization of pituitary ACTH adenomas without (silent corticotroph adenomas) and with Cushing’s disease. Eur J Endocrinol 163(1):35–43
Reincke M, Allolio B, Saeger W, Kaulen D, Winkelmann W (1987) A pituitary adenoma secreting high molecular weight adrenocorticotropin without evidence of Cushing’s disease. J Clin Endocrinol Metab 65(6):1296–1300
Righi A, Faustini-Fustini M, Morandi L, Monti V, Asioli S, Mazzatenta D, Bacci A, Foschini MP (2017) The changing faces of corticotroph cell adenomas: the role of prohormone convertase 1/3. Endocr 56(2):286–297
Sakaguchi H, Koshiyama H, Sano T, Inoue D, Hashimoto N, Aoki N, Nakao K (1997) A case of nonfunctioning pituitary adenoma resembling so-called silent corticotroph adenoma. Endocr J 44(2):329–333
Sano T, Kovacs K, Asa SL, Yamada S, Sanno N, Yokoyama S, Takami H (2002) Pituitary adenoma with “honeycomb Golgi” appearance showing a phenotypic change at recurrence from clinically nonfunctioning to typical Cushing disease. Endocr Pathol 13(2):125–130
Scheithauer BW, Gaffey TA, Lloyd RV, Sebo TJ, Kovacs KT, Horvath E, Yapıcıer Ö, Young WF, Meyer FB, Kuroki T, Riehle DL, Laws ER (2006) Pathobiology of pituitary adenomas and carcinomas. Neurosurgery 59(2):341–353
Serri O, Robert F, Pelletier G, Beauregard H, Hardy J (1987) Hyperprolactinemia associated with clinically silent adenomas: endocrinologic and pathologic studies; a report of two cases. Fertil Steril 47(5):792–796
Tan EU, Ho MS, Rajasoorya CR (2000) Metamorphosis of a non-functioning pituitary adenoma to Cushing’s disease. Pituitary 3(2):117–122
Tateno T, Izumiyama H, Doi M, Akashi T, Ohno K, Hirata Y (2007) Defective expression of prohormone convertase 1/3 in silent corticotroph adenoma. Endocr J 54(5):777–782
Tateno T, Kato M, Tani Y, Oyama K, Yamada S, Hirata Y (2009) Differential expression of somatostatin and dopamine receptor subtype genes in adrenocorticotropin (ACTH)-secreting pituitary tumors and silent corticotroph adenomas. Endocr J 56(4):579–584
Ueyama T, Tamaki N, Kondoh T, Kurata H (1998) Large and invasive silent corticotroph-cell adenoma with elevated serum ACTH: a case report. Surg Neurol 50(1):30–31
Walsh MT, Couldwell WT (2010) Symptomatic cystic degeneration of a clinically silent corticotroph tumor of the pituitary gland. Skull Base 20(5):367–370
Yamada S, Ohyama K, Taguchi M, Takeshita A, Morita K, Takano K, Sano T (2007) A study of the correlation between morphological findings and biological activities in clinically nonfunctioning pituitary adenomas. Neurosurgery 61(3):580–584
Yamakita N, Murai T, Kawamura S, Teramachi H, Matsuhisa T, Hirata T, Ikeda T, Morita H, Mune T, Yasuda K (1999) High molecular weight corticotropin measured with immunoradiometric assay in a patient with asymptomatic pituitary corticotropinoma. Endocr J 46(4):563–571
Yokoyama S, Kawahara Y, Sano T, Nakayama M, Kitajima S, Kuratsu J (2001) A case of non-functioning pituitary adenoma with Cushing’s syndrome upon recurrence. Neuropathology 21(4):288–293
Zoli M, Faustini-Fustini M, Mazzatenta D, Marucci G, De Carlo E, Bacci A, Pasquini E, Lanzino G, Frank G (2015) ACTH adenomas transforming their clinical expression: report of 5 cases. Neurosurg Focus 38(2):E15
Barr K, Pillinger DA, Miller CR, Wan Y, Sharpless JL (2016) ACTH staining does not predict retx in silent acth adenomas. Poster presentation, Endocrine Society Meeting SUN-487
Bonner RA, Mukai K, Oppenheimer JH (1979) Two unusual variants of Nelson’s syndrome. J Clin Endocrinol Metab 49(1):23–29
Petrossians P, Ronci N, Valdes Socin H, Kalife A, Stevenaert A, Bloch B, Tabarin A, Beckers A (2001) ACTH silent adenoma shrinking under cabergoline. Eur J Endocrinol 144(1):51–57
Sahli R, Christ ER, Seiler R, Kappeler A, Vajtai I (2006) Clinicopathologic correlations of silent corticotroph adenomas of the pituitary: report of four cases and literature review. Pathol Res Pract 202(6):457–464
Salgado LR, Machado MC, Cukiert A, Liberman B, Kanamura CT, Alves VA (2006) Cushing’s disease arising from a clinically nonfunctioning pituitary adenoma. Endocr Pathol 17(2):191–199
Asano S, Ooka H, Okazaki R, Ishikawa T, Ochiai H, Nakashima M, Ide F, Hasegawa I, Miyawaki S, Nakaguchi H, Murakami M, Ogino Y, Takano K, Matsuno A (2007) Long-term remission of cyclic Cushing’s disease that was diagnosed and treated surgically in non-active phase. Endocr J 54(3):407–412
Popovic V, Micic D, Nesovic M, Howlett T, Doniach I, Kendereski A, Djordjevic P, Manojlovic D, Micic J, Besser M (1990) Cushing’s disease cycling over ten years. Exp Clin Endocrinol 96(2):143–148
Ceccato F, Lombardi G, Manara R, Emanuelli E, Denaro L, Milanese L, Gardiman MP, Bertorelle R, Scanarini M, D’Avella D, Occhi G, Boscaro M, Zagonel V, Scaroni C (2015) Temozolomide and pasireotide treatment for aggressive pituitary adenoma: expertise at a tertiary care center. J Neurooncol 122(1):189–196
Nishioka H, Hirano A, Asa SL (1992) Silent corticotroph adenoma with multiple cysts: Pars intermedia tumor? Endocr Pathol 3(1):47–51
Kasuki L, Ventura N, Wildemberg L, Cardão Chimelli L, Gadelha M (2017) Accuracy of microcystic aspect on T2-weighted magnetic resonance imaging for the diagnosis of silent corticotropinomas. Presented at the 99th Endocrine Society Meeting, Orlando, April 2017 SAT 469
Kovacs K, Lloyd R, Horvath E, Asa SL, Stefaneanu L, Killinger DW, Smyth HS (1989) Silent somatotroph adenomas of the human pituitary. A morphologic study of three cases including immunocytochemistry, electron microscopy, in vitro examination, and in situ hybridization. Am J Pathol 134(2):345–353
Cooper O, Melmed S (2012) Subclinical hyperfunctioning pituitary adenomas: the silent tumors. Best Pract Res Clin Endocrinol Metab 26(4):447–460
Sano T, Mader R, Asa SL, Qian ZR, Hino A, Yamada S (2003) “Honeycomb Golgi” in pituitary adenomas: not a marker of gonadotroph adenomas. Endocr Pathol 14(4):363–368
Jin L, Riss D, Ruebel K, Kajita S, Scheithauer BW, Horvath E, Kovacs K, Lloyd RV (2005) Galectin-3 expression in functioning and silent ACTH-producing adenomas. Endocr Pathol 16(2):107–114
Thodou E, Argyrakos T, Kontogeorgos G (2007) Galectin-3 as a marker distinguishing functioning from silent corticotroph adenomas. Hormones 6(3):227–232
Mete O, Hayhurst C, Alahmadi H, Monsalves E, Gucer H, Gentili F, Ezzat S, Asa SL, Zadeh G (2013) The role of mediators of cell invasiveness, motility, and migration in the pathogenesis of silent corticotroph adenomas. Endocr Pathol 24(4):191–198
Acknowledgements
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
The study was approved under an IRB approved data repository with waiver of consent.
Rights and permissions
About this article
Cite this article
Langlois, F., Lim, D.S.T., Yedinak, C.G. et al. Predictors of silent corticotroph adenoma recurrence; a large retrospective single center study and systematic literature review. Pituitary 21, 32–40 (2018). https://doi.org/10.1007/s11102-017-0844-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0844-4