Abstract
Purpose
Arthropathy is a common and disabling complication of acromegaly. Since in this condition radiological findings rarely correspond to functional impairment, we elected to quantify in a large cohort of acromegalic patients: the degree of motor disability compared with data from general population, the impact of joint involvement on quality of life and work productivity, and to look for associated factors.
Methods
In 211 acromegalic patients, 131 with controlled disease and 80 with active disease, eight validated scales were used to evaluate the (i) prevalence and distribution of arthropathy, (ii) degree of motor disability and joint symptoms (VAS, AIMS symptoms and WOMAC), (iii) quality of life (AcroQoL and PASQ) and work capability (WPAI:GH) as consequences of joint complications.
Results
Using the WOMAC questionnaire, for which population based normative values are available, a significantly higher prevalence and severity of motor disability was detected in acromegalics compared to the general population from literature. The results provided by the different questionnaires turned out to be highly concordant. All measures of motor disability correlated both with impaired quality of life and motor disability and were worse in females and in patients with higher BMI.
Conclusions
The questionnaires VAS, AIMS symptoms, and WOMAC (this latter both as a whole and with its functionality subscale), with their scores, proved to be the most adequate tools to evaluate motor disability and its consequences on both quality of life and work productivity in acromegaly. Female gender and higher BMI are associated with worse articular symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Motor disability in acromegaly is chiefly accounted for by arthropathy, together with the less common myopathy and polyneuropathy. Arthropathy is present at diagnosis in most cases of acromegaly. Although it does not reduce life expectancy, it contributes to a significant impairing of patient’s quality of life, which is currently considered an important outcome in the management of chronic diseases. Moreover, articular impairment caused by growth hormone (GH) excess does not seem to entirely regress after hormonal normalization, so that therapies are often unable to restore joint function to its previous state [1, 2].
Pathogenesis of the disease-specific arthropathy seems articulated in two phases: initially GH and Insulin like Growth Factor 1 (IGF1) excess produce hypertrophy of the cartilages with consequent articular laxity and mechanical stress; over the time, the chronic trauma can result in irreversible degenerative arthrosis.
Arthrosis affects both spine and anti-gravity and not weight bearing peripheral joints [3,4,5]. The main symptom is articular pain, but stiffness and functional limitations are also frequent. Radiological manifestations are osteophytosis and joint space modifications consisting in the initial widening, caused by cartilage thickening, followed by its narrowing, due to the degeneration processes observed in more severe cases [6, 7].
As for other articular disorders, no consistent relation can be found between X-ray images and subjective discomfort or functional articular limitations, with the exception of rare severe cases presenting with joint space narrowing (JSN). Moreover, joint X-ray examination would miss the early stages of arthropathy, present in the vast majority of patients. Thus, the degree of articular dysfunction in acromegaly is difficult to establish [8, 9] even if it could be very important for rehabilitation purposes.
JSN is far less common in acromegaly than in primary osteoarthritis [3], affecting 10–15% of the patients with controlled acromegaly and with a higher prevalence in females and older patients [10]. Moreover, JSN in the hip has been demonstrated in cases of very active disease, characterized by higher pretreatment IGF1 and longer exposure to hormonal excess, suggesting a role of GH/IGF1 axis even in the late stages of this complication [10].
A prospective study aimed at investigating progression of acromegalic arthropathy identified a worsening of osteophytes and JSN in 72–74% of patients despite long-term biochemical control, being this progression more frequent in older patients, in those with higher GH/IGF1, and in those achieving disease control during somatostatin analogues (SSA) [11].
In this multicentric study, we used specific and validated questionnaires to determine in a large series of acromegalic the degree of joint involvement, functional impairment and motor disability, and their impact on patient quality of life (QoL) and working productivity. These data were then correlated with specific clinical and biochemical parameters.
Patients and methods
Two hundred and eleven acromegalic patients (94 men and 117 women, age 20–90 years) were enrolled in this cross-sectional Italian multicentric study (9 centers). Patients who had received clinical diagnosis together with high IGF1 levels, or GH not suppressed after oral glucose tolerance test, were included. At the time of study inclusion, 131 patients had controlled disease, intended as the normalization of IGF1 and/or GH levels. Of these, 109 were on pharmacological therapy, while 22 were off treatment after pituitary surgery. On the other hand, 80 patients displayed active disease either with or without medical treatment. There was no inclusion restriction based on age, gender, treatment or acromegalic disease status, while patients with known inflammatory rheumatic diseases were excluded. Of the 109 patients controlled by medical therapy, 58% had undergone surgical intervention (multiple in 3.5%) and 15% had undergone radiation therapy (radiosurgery in 81% of them). Sixty-nine were on SSA therapy, while 14 were on pegvisomant, 7 on combined SSA and pegvisomant, 15 were on SSA and dopamine agonists (DA), 3 with pegvisomant and DA, and one was on treatment with all three drugs.
Of the 80 subjects with uncontrolled disease, 41.5% had been surgically treated, multiple times in 8%. Eleven percent had undergone radiation therapy (radiosurgery in 7.5%). Twenty-nine were on SSA treatment, 6 on combined therapy with pegvisomant and SSA (2 on SSA, pegvisomant and DA), 7 on SSA and DA, 4 on pegvisomant, one on pegvisomant and DA, and one on DA. In nine cases the disease was still active after recent surgery and 23 patients had just received diagnosis.
Clinical and anamnestic parameters
Arthropathy was defined as the presence of self-reported pain (resting or movement), or stiffness or functional impairment at the level of the examined joints (i.e. shoulders, elbows, forearms, wrists, hips, knees, ankles, feet, cervical, dorsal or lumbar spine), both bilateral or unilateral. Body mass index (BMI) was calculated in each patient. The size of adenoma at diagnosis was approximated using the maximum diameter measured at MRI or CT scan.
The time elapsed from diagnosis was calculated as the time interval from diagnosis to study enrollment. The duration of active disease was calculated as the time interval from diagnosis to enrollment for those patients who had never achieved disease control or cure, and as the time elapsed from diagnosis to normalization of IGF1 and/or GH levels (< 1 ng/mL during medical treatment with SSA, < 0.4 ng/mL after OGTT in cured patients; GH levels were not considered in patients using pegvisomant) in those achieving control. GH/IGF-I levels at diagnosis and therapies were also registered. Information about the presence of concomitant hormonal defects and diabetes mellitus was collected from each patient’s history. All the patients who received a diagnosis of hormonal insufficiency were receiving replacement therapy (l-thyroxine, glucocorticoids, sex steroids), with the exception of three hypogonadal patients recently diagnosed with acromegaly. If patients assumed analgesic drugs all scores were referred to symptoms without those therapies.
Scales
Each patient was administered eight validated scales: (1) two of them, AcroQoL [12, 13] and Patient-assessed Acromegaly Symptom Questionnaire (PASQ) [14, 15], were quality of life scales; (2) three were motor disability scales and included: Visual Analogue Scale (VAS) [16, 17] for average pain felt during last week (both resting and during movements), the Arthritis Impact Measurement Scale (AIMS) [18, 19] evaluating both symptoms and functional impairment, and Western Ontario and McMaster universities osteoArthritis Index (WOMAC) [20, 21], composed of three scales evaluating articular pain, stiffness and functionality; (3) two questionnaires investigated daily living activities (ADL/IADL) [22, 23]; and (4) the work productivity scale: Work Productivity and Activity Impairment-General Health (WPAI-GH) [24, 25], evaluating patient productivity.
Since WOMAC questionnaire was the only one for which population-based normative values have been published [26] comparisons between the WOMAC median values of patients and the scores reported for the normal population were carried out; for this comparison we evaluated each separate subscale in order to use the data thus reported in literature.
Biochemical parameters
In order to circumvent bias associated with different assays used in the various Centers, IGF1 was considered both in terms of absolute values and estimated standard deviations (eSD). The standardization was obtained using reference interval for age of each specific measurement from the general population assuming that IGF1 values are distributed in a normal pattern. To estimate the effective hormonal condition of our patients compared to the general population, standardized values were obtained with one of the methods reported by Christy Chuang-Stein in 1992 [27], that considers both the upper (97.5th) percentile and the lower (2.5th) percentile of the general population, as reported by each manufacturer.
The standardized values were obtained as follows:
where eSD = (mean-lower reference value)/2 and mean = (higher reference value + lower reference value)/2. GH values were not standardized.
Possible correlations between questionnaire-derived scores for disability and QoL and the abovementioned clinical and biochemical parameters were investigated.
Statistical analysis
Sociodemographic and clinical continuous variables were expressed as mean ± standard deviation (SD), or median with interquartile range (IQ); categorical data were expressed as frequencies and proportions. Based on the skewness of the different outcome variables, as shown by histogram and QQ plots, we used: (i) median test, which allows to test whether, in each area of WOMAC score (pain, stiffness and physical function), the sample median of acromegalic subjects differed from the median of general population using WOMAC scores from reference data from Bellamy et al. [26]; (ii) Spearman correlation, to test the correlation between questionnaire-derived scores of disability and both the QoL questionnaires and work productivity score; (iii) log-gamma model, to examine the relation between sociodemographic and clinical parameters with the degree of arthropathy, as measured by different indices as the total WOMAC, VAS, functionality AIMS and AIMS symptoms in whole population and in both active and controlled diseases.
Results
In our series, 75% of the patients presented arthropathy to least one joint: in particular the prevalence was 77% in patients with active disease versus 73% in those with disease remission. The spine was the most affected site, causing pain, stiffness or articular impairment in 62% of patients. Lumbar, cervical, and dorsal tracts were involved in 54, 43 and 24% of cases, respectively, with 20% of patients complaining of symptoms in all spinal tracts. Among peripheral joints, knee, shoulder and hip were affected in 46, 34 and 31% of patients, respectively. Twenty-four percent of the patients reported wrist problems, while feet, elbows, ankles and forearms were less affected (13, 9, 6 and 4%, respectively). The majority of patients had a symmetric involvement of peripheral joints (57% with only bilateral signs or symptoms) whereas a small percentage of subjects with peripheral involvement had only unilateral signs or symptoms (23%); the remaining 20% had mixed symmetric and asymmetric involvement of different articulations. The median (interquartile range) number of affected joint sites was 4 (1–6).
The time elapsed from diagnosis to the study enrollment varied from few months (new diagnosis) to 49 years (median: 7.72 years, interquartile range 1.87–15.78 years). Table 1 shows main patient clinical and sociodemographic characteristics. Mean and median values, and interquartile ranges for all questionnaires are reported in Table 2; (regarding WOMAC subscales: median WOMAC pain score was 4/20, median WOMAC stiffness was 2/8 and median WOMAC functionality score was 10/68).
Three questionnaires, i.e. AIMS functionality, ADL and IADL, showed low discriminating performance in this sample. In particular, the application of AIMS functionality subscale in our acromegalics showed a floor effect, with 64% of patients obtaining a total score lesser than 1/10, while ADL and IADL displayed an evident ceiling effect, with more than 70% of patients obtaining the maximum score.
Other scales, i.e. VAS, WOMAC pain, WOMAC stiffness, WOMAC functionality, WOMAC total and AIMS symptoms, displayed higher variable results and thus a better performance (IQ VAS: 48.5; IQ WOMAC pain: 7; IQ WOMAC stiffness: 4; IQ WOMAC functionality: 25; IQ WOMAC total: 35; IQ AIMS symptoms: 5; IQ AIMS functionality: 1.06; IQ ADL and IQ IADL: 0).
Comparison with the general population for WOMAC subscales
Comparing scores obtained in our acromegalic patients with reference data from general population we found no difference in terms of age and BMI, but acromegalics displayed significantly higher (i.e. worse) median scores for all WOMAC subscales (p value < 0.001 for pain, stiffness and function) (Table 3).
Quantification of motor disability and correlation with quality of life (QoL) and work productivity
Significant positive correlations were found between WOMAC functionality and AIMS functionality scores (Rho: 0.62, p-value < 0.0001), between WOMAC pain and VAS scores (Rho: 0.68, p-value < 0.0001), and between the sum of WOMAC pain and stiffness scores and AIMS symptoms (Rho: 0.85, p-value < 0.0001).
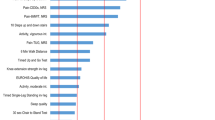
Furthermore, WOMAC total, AIMS symptoms and VAS scores were significantly correlated with the scores of the two questionnaires investigating the quality of patients’ life and with work productivity indices (i.e. percentage of worktime loss, perceived impact of the disease on working efficacy and in regular daily activities) (Table 4).
Relations with other sociodemographic and clinical parameters
In each multivariate adjusted model, BMI and female gender were significantly and positively related to the scores of WOMAC total, VAS, AIMS functionality and AIMS symptoms, while time lapsed from diagnosis and GH were not (Table 5). Moreover, significant inverse correlations between standardized IGF1 at the moment of the study and VAS, AIMS functionality and AIMS symptoms were observed. A significant positive correlation was found between age and AIMS functionality scores, whereas WOMAC score was significantly worse in diabetic versus non-diabetic acromegalic patients (median WOMAC total 33 vs. 12). Mean age was also significantly higher in diabetic patients (64.2 ± 12 vs. 54.5 ± 13.4, p < 0.0001).
On the contrary, no associations were found with duration of active disease, with IGF1 at diagnosis, with adenoma volume, concomitant hormonal deficiencies and with kinds of medical treatment. Finally, the above described positive and negative correlations were present in both subsets of patients, i.e. those with active disease and those with biochemically controlled disease at the moment of observation whereas these two population showed no significant difference in all the above-mentioned parameters (data not shown).
Discussion
The questionnaire-based approach to the evaluation of acromegalic arthropathy, besides confirming the high prevalence of this complication, allowed to establish the suitability of some questionnaires for quantifying the severity of the disorder and to define its impact on the quality of life. To the best of our knowledge, this is the most extensive patient-reported evaluation of motor disability carried out such a large series of patients with acromegaly, which is a rare disease by definition.
In our experience, an impressive prevalence of joint impairment was reported, with almost three out of four patients complaining of articular pain, stiffness or limitations during both active and biochemically controlled disease. In agreement with previous reports [28], we found a higher occurrence of spinal involvement, present in more than 60% of patients, followed by symptoms at knees, shoulders and hips. The involvement of peripheral joints was mostly symmetric. Worth noting, in our series the frequency of hip involvement was greater than that commonly reported in literature [28].
Acromegalic patients displayed significantly worse scores in all WOMAC items compared to general population, and these scores were strongly correlated with the other disability questionnaires, with quality of life, percentage of worktime loss and perceived impact on work productivity and on regular daily activities.
Overall, most of the questionnaires used in this study appeared useful and accurate to quantify articular impairment and its daily consequences in acromegaly, except for ADL and IADL due to their poor discriminating ability. Therefore, we suggest against their application in common practice and in future studies assessing the degree of disability in acromegaly.
In our series, female gender and higher BMI were associated with worse articular impairment. Gender differences in joint damage had already been described in acromegaly as well as in the general population [28, 29], even if in those settings worse values in postmenopausal women have been attributed to estrogen deficiency. This hypothesis is strengthened by the observation that prevalence, progression and extension of articular impairment in primary osteoarthritis are higher only in postmenopausal women than in men [30], differently from our cohort.
The influence of BMI found in our large group of patients confirms the previous observation of Claessen et al. [9], who described high baseline BMI as a risk factor for functional deterioration of lower limbs in a smaller series of acromegalic subjects. Obesity is known to be an important modifiable risk factor for poor joint condition, since it generates an important mechanical stress upon the already altered acromegalic joints, determining faster progression to irreversible disease and should therefore be readily addressed.
Patients with diabetes mellitus showed worse WOMAC scores than their non-diabetic counterpart, thus confirming a negative impact of diabetic disease on motor disability, possibly due to associated neuropathy and myopathy; however, a concomitant role played by older age cannot be ruled out. On the contrary, we failed to disclose differences between patients receiving hormone replacement therapy and those without hormonal deficiencies; however, this finding could be due to a lack of statistical power deriving from the evaluation of small subsets of patients.
Interestingly, there was no correlation between the degree of motor disability and the status of disease (active or controlled) at the enrollment. On the contrary, standardized IGF1 at the time of observation showed an inverse correlation with joint complaints and limitations in the adjusted model, thus apparently acting as a protective factor. This paradoxical effect, already reported by others [28], could be explained with a trophic, though transient, activity exerted by the anabolic hormone excess. Indeed, during active disease, high IGF1 levels produce cartilage hypertrophy, thus widening articular spaces and delaying the painful and disabling JSN [3]. Over time, however, this effect is overcome by supervening articular irregularities leading to chronic mechanical friction and arthritis. In another study, performed with MRI techniques [31], this joint space widening was associated to an altered composition of articular cartilages, consisting in an unhealthy increase in watery content: this reversible abnormality is thought to pave the way for subsequent degenerative processes.
The lack of correlation between articular impairment and time elapsed from diagnosis was in contrast with Layton et al. [32] and Claessen et al. [10, 11] who investigated the radiological progression of acromegalic arthropathy, but in line with other groups [28].
The cross-sectional design of the present study did not allow to establish causal connections or determinants of the progression of arthropathy. Indeed, the effects of medical treatment on disease activity and articular impairment could not be adequately addressed in our study. Moreover, the great variability in the time lapsed from diagnosis to enrollment and in the duration of active disease, makes hardly possible to establish any correlation between the basic disease and the articular complications. In order to compare the progression of arthropathy between patients with controlled and uncontrolled disease and evaluate differences between surgically cured and therapy-controlled patients, a long-term prospective evaluation is mandatory.
However, the use of many highly concordant questionnaires, strictly relating to quality of life and work productivity, allowed us to evaluate the functional consequences of articular impairment in the largest number of acromegalics ever studied with respect to this complication. Our experience contributed to establish functional correlates of acromegalic arthropathy, which turned out to be linked to both modifiable (BMI) and not modifiable (gender) factors. Our finding of a significant inverse correlation with standardized IGF1, combined with recent findings obtained by others using MRI [31], provides new information about early pathophysiological stages of this complication.
Among the questionnaires tested in acromegaly, we suggest the use of VAS, AIMS symptoms, and WOMAC (both as a whole and with as functionality subscales), since they proved to be a simple tool quantifying motor disability strongly associated to loss of QoL and work productivity, which are the main outcomes of this complication. Furthermore, if validated also in acromegaly, the reliability of these questionnaires could be relevant not only for insurance purposes but also in daily clinical practice to screen patients for pain therapy (VAS, WOMAC pain, AIMS symptoms) or physiatric-orthopedic counseling (WOMAC functionality).
References
Colao A, Pivonello R, Scarpa R et al (2005) The acromegalic arthropathy. J Endocrinol Invest 28:24–31
Claessen KMJA, Mazziotti G, Biermasz NR, Giustina A (2015) Bone and joint disorders in acromegaly. Neuroendocrinology 103(1):86–95. https://doi.org/10.1159/000375450
Wassenaar MJE, Biermasz NR, Bijsterbosch J et al (2011) Arthropathy in long-term cured acromegaly is characterised by osteophytes without joint space narrowing: a comparison with generalised osteoarthritis. Ann Rheum Dis 70:320–325. https://doi.org/10.1136/ard.2010.131698
Biermasz NR, van’t Klooster R, Wassenaar MJE et al (2012) Automated image analysis of hand radiographs reveals widened joint spaces in patients with long-term control of acromegaly: relation to disease activity and symptoms. Eur J Endocrinol 166:407–413. https://doi.org/10.1530/EJE-11-0795
Scarpa R, De Brasi D, Pivonello R et al (2004) Acromegalic axial arthropathy: a clinical case-control study. J Clin Endocrinol Metab 89:598–603. https://doi.org/10.1210/jc.2003-031283
Bluestone R, Bywaters EG, Hartog M et al (1971) Acromegalic arthropathy. Ann Rheum Dis 30:243–258
Lieberman SA, Björkengren AG, Hoffman AR (1992) Rheumatologic and skeletal changes in acromegaly. Endocrinol Metab Clin North Am 21:615–631
Wassenaar MJE, Biermasz NR, Kloppenburg M et al (2010) Clinical osteoarthritis predicts physical and psychological QoL in acromegaly patients. Growth Horm IGF Res 20:226–233. https://doi.org/10.1016/j.ghir.2010.02.003
Claessen KMJA, Ramautar SR, Pereira AM et al (2014) Increased clinical symptoms of acromegalic arthropathy in patients with long-term disease control: a prospective follow-up study. Pituitary 17:44–52. https://doi.org/10.1007/s11102-013-0464-6
Claessen KMJA, Kloppenburg M, Kroon HM et al (2013) Two phenotypes of arthropathy in long-term controlled acromegaly? A comparison between patients with and without joint space narrowing (JSN). Growth Horm IGF Res 23:159–164. https://doi.org/10.1016/j.ghir.2013.05.003
Claessen KMJA, Ramautar SR, Pereira AM et al (2012) Progression of acromegalic arthropathy despite long-term biochemical control: a prospective, radiological study. Eur J Endocrinol 167:235–244. https://doi.org/10.1530/EJE-12-0147
Webb SM, Badia X, Spanish AcroQol Study Group (2006) Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur J Endocrinol 155:269–277. https://doi.org/10.1530/eje.1.02214
Badia X, Webb SM, Prieto L, Lara N (2004) Acromegaly Quality of Life Questionnaire (AcroQoL). Health Qual Life Outcomes 2:13. https://doi.org/10.1186/1477-7525-2-13
Trainer PJ, Drake WM, Katznelson L et al (2000) Treatment of acromegaly with the growth hormone-receptor antagonist pegvisomant. N Engl J Med 342:1171–1177. https://doi.org/10.1056/NEJM200004203421604
Neggers SJCMM, Van Aken MO, De Herder WW et al (2008) Quality of life in acromegalic patients during long-term somatostatin analog treatment with and without pegvisomant. J Clin Endocrinol Metab 93:3853–3859. https://doi.org/10.1210/jc.2008-0669
Ohnhaus EE, Adler R (1975) Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain 1:379–384
Sriwatanakul K, Kelvie W, Lasagna L et al (1983) Studies with different types of visual analog scales for measurement of pain. Clin Pharmacol Ther 34:234–239
Meenan RF, Gertman PM, Mason JH, Dunaif R (1982) The arthritis impact measurement scales. Further investigations of a health status measure. Arthritis Rheum 25:1048–1053
Cavalieri F, Salaffi F, Ferraccioli GF (1991) Relationship between physical impairment, psychological variables and pain in rheumatoid disability. An analysis of their relative impact. Clin Exp Rheumatol 9:47–50
Bellamy N, Buchanan WW, Goldsmith CH et al (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Salaffi F, Leardini G, Canesi B et al (2003) Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged. The index of adl: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Reilly MC, Zbrozek AS, Dukes EM (1993) The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 4:353–365. https://doi.org/10.2165/00019053-199304050-00006
Leggett S, van der Zee-Neuen A, Boonen A et al (2016) Test-retest reliability and correlations of 5 global measures addressing at-work productivity loss in patients with rheumatic diseases. J Rheumatol 43:433–439. https://doi.org/10.3899/jrheum.141605
Bellamy N, Wilson C, Hendrikz J (2011) Population-based normative values for the Western Ontario and McMaster (WOMAC) Osteoarthritis Index: Part I. Semin Arthritis Rheum 41:139–148. https://doi.org/10.1016/j.semarthrit.2011.03.002
Chuang-Stein C (1992) Summarizing laboratory data with different reference ranges in multi-center clinical trials. Drug Inf J 26:77–84. https://doi.org/10.1177/009286159202600108
Kropf LL, Madeira M, Neto LV et al (2013) Functional evaluation of the joints in acromegalic patients and associated factors. Clin Rheumatol 32:991–998. https://doi.org/10.1007/s10067-013-2219-1
Biermasz NR, Pereira AM, Smit JW, Romijn JA et al (2005) Morbidity after long-term remission for acromegaly: persisting joint-related complaints cause reduced quality of life. J Clin Endocrinol Metab 90:2731–2739. https://doi.org/10.1210/jc.2004-2297
Johnson VL, Hunter DJ (2014) The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol 28:5–15. https://doi.org/10.1016/J.BERH.2014.01.004
Claessen KMJA, Canete AN, de Bruin PW et al (2017) Acromegalic arthropathy in various stages of the disease: an MRI study. Eur J Endocrinol 176:779–790. https://doi.org/10.1530/EJE-16-1073
Layton MW, Fudman EJ, Barkan A et al (1988) Acromegalic arthropathy. Characteristics and response to therapy. Arthritis Rheum 31:1022–1027
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported
Ethical approval and informed consent
The study was conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethic Committee of the coordinating institution (GR-2008-1137632), and all patients gave a written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fatti, L.M., Cangiano, B., Vitale, G. et al. Arthropathy in acromegaly: a questionnaire-based estimation of motor disability and its relation with quality of life and work productivity. Pituitary 22, 552–560 (2019). https://doi.org/10.1007/s11102-019-00966-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00966-8