Abstract
The involvement of multiple joints is common in osteoarthritis (OA), often referred to as generalized osteoarthritis (GOA). However, since research and practice mainly focus on a specific OA localization, the health status of patients with GOA is largely unknown. Therefore, we aimed to describe the clinical burden of GOA in terms of self-reported health-related quality of life (HRQoL) and activity limitations. In this cross-sectional study, individuals clinically diagnosed with GOA and referred to multidisciplinary treatment, completed questionnaires on socio-demographics, joint involvement, HRQoL (SF-36) and activity limitations (HAQ-DI). SF-36 physical (PCS) and mental component summary scores (MCS) were calculated using norm-based data. The patient’s specific most important activity limitations were linked to the International Classification of Functioning, Disability and Health. A total of 147 patients participated [85 % female; mean (SD) age 60 (8) years]. The majority (93 %) had symptomatic OA in both the upper and lower extremities. Predominant joints with symptomatic OA were the hands (85 %) and knees (82 %). Mean (SD) SF-36 PCS and MCS scores were 37 (7) and 48 (10), respectively, showing a broad impact of GOA on the physical component of health. The mean (SD) HAQ-DI score was 1.27 (0.50) indicating moderate to severe functional limitations. Activities concerning mobility and domestic life were considered most important activity limitations, especially walking. The results show a high clinical burden of GOA in terms of HRQoL and activity limitations. This study points to the need of developing non-pharmacological interventions for patients with GOA that should target on improving the physical component of health and mobility limitations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most prevalent chronic joint disease that can affect multiple joints [1]. The hands and the lower limb weight-bearing joints, i.e., the hip and knee are the most common sites of disease involvement [2]. Generalized osteoarthritis (GOA) is an important and widely accepted OA phenotype, describing the often polyarticular nature of OA [3–5]. The term GOA was first used by Kellgren and Moore in 1952 [6]. Since then multiple definitions of GOA have been suggested. However, a recently published review showed that there is still no widely accepted and validated definition of GOA [5]. Nevertheless, it has been suggested that individuals with GOA might represent a relatively large subgroup of patients with OA [7–9]. In knee OA populations, approximately 50 % of patients can be classified as GOA according to three different criteria sets [7].
Current research and clinical practice mostly examine OA populations for a specific localization of OA, without considering the involvement of multiple joints. As such, research on GOA is very limited. The impact of GOA on patient’s health status is therefore largely unknown. A few previous studies have examined the association between multiple joint involvement (e.g., joint pain comorbidity) and health outcomes in patients with hip and knee OA, showing poorer outcomes for pain, function and quality of life than in single joint OA [10–13]. However, in those studies, the nature of the additional musculoskeletal complaints is unknown and might be unrelated to OA. To the best of our knowledge, there are no studies that comprehensively assessed the health status of patients clinically diagnosed with GOA. So far, only one study assessed the impact of GOA on health status, showing that patients with GOA (radiographic OA in ≥2 joints) did not have a poorer quality of life than individuals with hip or knee OA only [14]. However, the limited sample size in that study (n = 30) prevents firm conclusions.
Improved understanding of the health status of patients with GOA is warranted considering the high prevalence of GOA and the lack of research. Information on the health status of patients with GOA might be used by clinicians and researchers to improve the management and quality of care for patients with GOA. Therefore, the aim of the current study was (1) to describe the clinical burden of patients clinically diagnosed with GOA in terms of self-reported health-related quality of life (HRQoL) and activity limitations and (2) to identify commonly reported, self-perceived activity limitations and participation restrictions in patients with GOA.
Method
Design
For this cross-sectional study, we used baseline data from a randomized clinical trial comparing the effectiveness of two multidisciplinary non-pharmacological treatment programs for patients with GOA, performed at the outpatient rheumatology departments of the Sint Maartenskliniek Hospitals in the Netherlands. Participants were allocated to either a multidisciplinary supervised group-based self-management program or a telephone-delivered self-management program. The complete study design has been described previously [15]. The Institutional Review Board of the Radboud University Medical Nijmegen Centre approved the study and all patients signed informed consent.
Participants
Recruitment to the study took place between January 2010 and March 2013. During an outpatient visit, patients clinically diagnosed with GOA and referred by their rheumatologist for treatment were invited for a screening visit with an occupational therapist, physical therapist and researcher to consider eligibility to participate in the trial. Patients were eligible when meeting all of the following inclusion criteria: (1) aged ≥18 years; (2) having objective signs of OA in at least two joint areas on the basis of the patient’s medical file (objective signs included: malalignment, crepitation, limited range of motion, palpable osteophytes/nodules or radiographic signs including the presence of joint space narrowing and/or osteophytes); (3) having clinical symptoms in ≥3 out of 8 joint areas; (4) being limited in the performance of daily activities [Health Assessment Questionnaire Disability Index (HAQ-DI) score >0.5]; and (5) being motivated to alter your lifestyle and willing to participate in a group. Excluded were patients who were as follows: (1) diagnosed with another rheumatic disease; (2) awaiting surgery; (3) already participated unsuccessfully in a self-management program; (4) having psychosocial problems interfering with the scope of the treatment program (on the basis of clinical judgment of a physical therapist and occupational therapist); (5) incapable of coming to the hospital; or (6) unable to write and or understand the Dutch language.
Data collection
Prior to the start of the treatment programs, all patients completed a standardized set of health-related patient-reported outcome measures to assess socio-demographic characteristics, fatigue, joint involvement, activity limitations and HRQoL. Socio-demographic characteristics included age, sex, education, marital status and occupation. Height and weight were recorded to calculate the body mass index (BMI). Fatigue was measured with the “subjective fatigue” subscale of the checklist individual strength (CIS; score range 8–56 points, scores of ≥35 represent severe fatigue [16]).
Joint involvement
To identify the localization of symptomatic OA in eight joint areas [i.e., feet (including ankles), knees, hips, lumbar spine, neck, shoulders, elbows and hands (including wrists)], the following question was assessed in the baseline questionnaire: “In which of these joints do you experience symptoms (pain/stiffness) for more than half of the time?” The locations of symptoms were identified by each patient on a paper manikin, which permitted the identification of symptom locations on either side of the body [17]. In addition, objective signs of OA and its localization were registered by the first author by screening each patient’s medical file.
Health-related quality of life
Health-related quality of life was measured with the Short Form 36 Health Survey (SF-36), a widely used generic questionnaire that comprises eight areas of health status: physical functioning, physical role limitations, bodily pain, general health, vitality, social functioning, emotional role limitations and mental health [18]. Additionally, the SF-36 comprises two summary scores: the physical component summary (PCS) and the mental component summary (MCS). We used SF-36 scores of the Dutch general population to standardize the scores of the patients in the current study in order to apply the norm-based scoring whereby we adjusted for age [19, 20]. All scores were standardized to a mean (SD) of 50 (10). Lower scores represent worse health status.
Activity limitations measured with the HAQ-DI
Participants completed the Dutch consensus HAQ-DI [21]. The HAQ-DI measures difficulties with the performance of 20 daily activities retrospectively over the preceding week with four response categories: no difficulty (0), some difficulty (1), much difficulty (2) and unable to do (3). The activities are classified into eight categories with two or three activities each: dressing and grooming, arising, eating, walking, personal hygiene, reaching, gripping and usual activities (i.e., shopping, doing chores, getting in and out of a car) [22]. The highest scores of each category are summed and averaged resulting in a disability index ranging from 0 to 3, where scores of 0–1 are generally considered to represent mild to moderate disability, 1–2 moderate to severe disability and 2–3 severe to very severe disability [22]. We did not correct HAQ-DI scores for using assistive devices.
Activity limitations and participation restrictions measured with the patient-specific complaints questionnaire (PSK)
The PSK was administered by an occupational therapist with the aim to elicit activity limitations and participation restrictions that are specific and relevant to the individual patient [23]. Patients were asked to identify the three most important activities, currently difficult to perform because of their GOA. No list of activities was used to allow patients freedom in their responses. In addition, patients rated the severity of each activity on a 10 cm visual analogue scale (VAS; 0 = no difficulty, 10 = impossible) [23]. Patient-specific approaches to measure functional limitations have been shown to be reliable, valid and responsive in patients with several musculoskeletal conditions [23, 24]. These activity limitations were then linked to the Activities and Participation component of the International Classification of Functioning, Disability and Health (ICF) [25]. This component describes a person’s functional status whereby Activities refer to the execution of specific tasks and Participation refers to the involvement in life situations. The ICF categories of the Activities and Participation component are designated by the letter d, followed by a numeric classification that indicates the chapter and specific category within the ICF classification. In the current study, each activity limitation was systematically linked to the most precise ICF category (third or fourth level) independently by three assessors (SK, DK and JG) using established linking rules [26]. In case of disagreement, agreement was established through a consensus meeting. When a patient reported different activity limitations or participation restrictions within the same PSK item, different ICF categories were identified. This process resulted in a list of ICF codes on different levels of the ICF within the area of Activities and Participation.
Statistical analysis
Descriptive statistics were used to describe the main characteristics of the study population and to explore comparability between the participants and eligible patients. Mean (SD) SF-36 subscale and component summary scores were calculated to identify the patient’s health status. The mean (SD) total HAQ-DI score as well as mean (SD) HAQ-DI scores of each HAQ-DI category were calculated to identify the patient’s functional status. Additionally, we assessed for each HAQ-DI category, the percentage of patients that reported to have either no/some difficulty (score 0 or 1) or much difficulty (score 2 or 3) with performing everyday activities. The most commonly reported activity limitations and participation restrictions by patients with GOA were identified by analyzing the frequencies of the assigned ICF categories from the PSK. All statistical analyses were performed using STATA 10.1.
Results
Patient characteristics
In total, 236 patients were considered eligible to participate in the study of whom 158 (67 %) agreed to. Main reasons for patients not to participate was having a preference for the multidisciplinary group-based treatment (n = 46; 59 %) or lacking confidence toward the telephone-delivered treatment (n = 24; 31 %). No differences were found between the group of eligible patients and the participants with regard to age, whereas there were relatively less women in the group of eligible patients (72 vs. 85 %, p = 0.01). Of the 158 participants, 11 were lost before the first measurement (i.e., provided no data), meaning that 147 patients were included in the analysis of the current study. Characteristics of the study population are summarized in Table 1.
Joint involvement
The median number of self-reported joint areas with symptomatic OA was 5 (interquartile range 4–6), and the median number of joint areas with objective signs of OA was 2 (interquartile range 2–3). The majority of patients (n = 136; 93 %) had symptomatic OA in both the upper half (neck, shoulder, elbow and hand) and lower half (lumbar spine, hip, knee and foot) of the body. The prevalence of self-reported and objective signs of OA for each joint area is depicted in Fig. 1. The predominant joints with symptomatic OA were the hands (n = 125; 85 %) and knees (n = 121; 82 %), whereas symptoms in the elbow joints were the least often reported (n = 41; 28 %). The predominant joints with objective signs of OA were also the hands (n = 114; 78 %) and knees (n = 78; 53 %) as recorded in the patient’s medical files, whereas objective OA signs in the elbows were the least often recorded (n = 3; 2 %). We found the combination of hand and knee OA to be most common, both self-reported (n = 106; 72 %) as well as recorded in the medical files (n = 58; 39 %).
Percentages of symptomatic and objective signs of OA for each joint area. The light gray bars represent the percentage of self-reported symptomatic OA, the gray bars represent the percentage of objective OA signs as recorded in the patient’s medical files, and the dark gray bars represent the percentage of both self-reported symptoms and objective signs of OA
Health-related quality of life
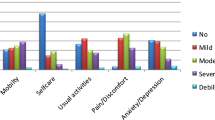
Mean scores for the PCS, MCS and subscales of the SF-36 are presented in Fig. 2. Mean (SD) PCS and MCS scores were 37.4 (6.9) and 47.8 (10.5), respectively. Mean (SD) scores were worst for the subscales physical function, physical role limitations, bodily pain and vitality, i.e., 37.4 (7.7), 39.0 (8.3), 40.0 (6.6) and 40.3 (5.5), respectively. Highest scores were obtained for the subscales mental health and emotional role limitations, i.e., 47.7 (8.6) and 45.4 (12.0).
Activity limitations measured with the HAQ-DI
The mean (SD) total HAQ-DI score for the total study population was 1.27 (0.50), indicating moderate to severe activity limitations [22]. One hundred and eleven patients (76 %) obtained a HAQ-DI score ≥1. The analysis of the HAQ-DI categories revealed that patients in the current study reported the greatest amount of difficulty with performing activities in the categories usual activities (i.e., shopping, doing chores, get in and out of a car) and reaching (i.e., bending down to pick up clothing from the floor, reach and get down a 5 pound object from above your head). Mean HAQ-DI scores for these categories were 1.61 and 1.58, respectively (Fig. 3). More than half of the patients reported to have “much difficulty” with performing these activities. Patients reported the least amount of difficulty with performing activities in the category dressing and grooming (dress yourself and shampoo your hair) as this category obtained the lowest mean (SD) HAQ-DI score, i.e., 0.86 (0.66). Thirteen percent of the patients reported to have “much difficulty” with performing these activities.
Activity limitations measured with the PSK
The total number of self-perceived activity limitations and participation restrictions obtained with the PSK was 440 (one patient mentioned only two limitations). These were linked to 463 ICF codes within the area of Activities and Participation of the ICF (d-codes), comprising 30 unique ICF categories. Of these 463 codes, 316 (68 %) pertained to the chapter mobility (d4), 85 (18 %) to domestic life (d6), 27 (6 %) to community, social and civic life (d9) and 19 (4 %) to self-care (d5). The remaining codes pertained to the chapters major life areas (d8), learning and applying knowledge (d1) and general tasks and demands (d2). Patients reported a broad spectrum of activity limitations and participation restrictions. The ten most frequently reported GOA-related activity problems and participation restrictions with corresponding ICF codes and mean (SD) severity scores are presented in hierarchical order in Table 2. Activities concerning mobility (d4) and domestic life (d6) were most frequently mentioned as being important activity limitations by patients with GOA; walking (d450) was most commonly reported. The category moving around (d455) can be further specified to the fourth level of the ICF as all activities in this category concerned climbing stairs (d4551). The severity of the activity limitations and participation restrictions were all above 6.0 with the highest score of 7.3 (on a 10 points scale) for caring for household objects (d650).
Discussion
This is the first study that comprehensively describes the health status of patients clinically diagnosed with GOA. The results show that GOA has a broad impact on the physical component of health. Furthermore, the majority of our patients were moderate to severely impaired in performing daily activities. Patients reported a broad spectrum of important activity limitations and participation restrictions; activities concerning mobility and domestic life were considered as most important activity limitations, especially walking. In addition, more than half of the patients reported having “much difficulty” with activities such as shopping or doing chores and activities concerning reaching. These results offer starting points for clinicians and researchers to improve treatment programs for patients with GOA tailored to their needs and problems.
The present study showed that patients with GOA experience a markedly reduced quality of life, reflecting a high clinical burden. In particular, the physical component of health was affected. The observed level of physical health in the present study is comparable to that of patients with chronic, inflammatory arthritis such as rheumatoid arthritis (RA) [27, 28]. Mental health was less affected compared to physical health in our study sample. One previous study assessed the PCS and MCS scores in a relatively small number of patients with GOA (n = 30) [14], showing comparable scores as obtained in the current study. Our results indicate that effective interventions for GOA should be developed focussing on improving the physical component of health.
Patients in this study were moderately to severely impaired in performing daily activities as reflected by a mean HAQ-DI score of 1.27. This score is considerably higher than the average HAQ-DI score of 0.50 observed in Dutch patients with symptomatic OA at multiple joint sites participating in the Genetics, Arthrosis and Progression (GARP) study [29]. In another study among Dutch patients with OA (localization not specified) visiting an outpatient rheumatology department, a mean HAQ-DI score of 1.00 was reported [30]. Considering the abovementioned, it seems that the functional status of patients with GOA is more affected compared to other Dutch OA populations. Comparisons are, however, hampered by the fact that the patients in the current study were a selected group of patients with functional disability who were referred to multidisciplinary treatment. However, since our study population represents patients seeking help, this is probably the most interesting group for clinicians.
Understanding the nature of GOA-related activity limitations and participation restrictions might be important to develop treatment targets tailored to the patients’ needs and problems. The results of the PSK showed that our patients reported a broad spectrum of activity limitations and participation restrictions. Activities involving the lower extremities were considered to be the most important activity limitations, especially walking. This finding cannot be explained by a predominance of lower limb OA by our patients, but might be due to a high impact of mobility limitations on a patient’s well-being. Moreover, self-care limitations were rarely reported as being important activity limitations. This is in contrast with the ICF core sets for OA in which self-care activities are assumed to be key issues for patients with OA [31]. Dressing is even one out of three ICF categories of the brief core set for OA representing activities that minimally should be addressed when measuring disability in clinical studies [31, 32]. Only one of these three activities was identified as an important activity limitation in our study. This discrepancy might be due to that we restricted patients to identify only three activity limitations. Nonetheless, our results point to the need of developing effective interventions to improve mobility, especially walking.
This study has some potential limitations that should be addressed. In this study, we used a pragmatic definition of GOA in the absence of a widely accepted and validated definition. In the literature, the threshold number of affected joints as well as the localization of involved joints has been described differently [5]. Besides, previous GOA definitions mainly rely on radiographic findings independent of clinical symptoms, whereas symptoms are likely to be more important in functional outcomes [33]. We are one of the first that defined GOA from a clinical rather than a radiographic perspective. Second, due to pragmatic reasons, we were not able to systematically obtain radiographs of all joint areas of each participant. Since we recorded objective signs of OA on the basis of information available in the patient’s medical file, it is conceivable that there is an underestimation of the number of joint areas with objective OA in our study population. Another limitation is that we did not assess comorbidities in this study population. The presence of comorbidities might have influenced the reported functional limitations and quality of life.
In conclusion, we generated empirical data showing a high clinical burden in terms of HRQoL and activity limitations in patients clinically diagnosed with GOA. This study contributes to the understanding of the deprived health status of individuals with GOA which is warranted considering the high prevalence of GOA and the lack of research on GOA. The results point to the need of developing effective interventions for patients with GOA to improve the physical component of health and to improve mobility, especially walking. Moreover, the broad spectrum of activity limitations underlines that treatment should be individualized according to the problems of the individual patient.
References
Bijlsma JW, Berenbaum F, Lafeber FP (2011) Osteoarthritis: an update with relevance for clinical practice. Lancet 377:2115–2126
Petersson IF, Jacobsson LT (2002) Osteoarthritis of the peripheral joints. Best Pract Res Clin Rheumatol 16:741–760
Bierma-Zeinstra SM, Verhagen AP (2011) Osteoarthritis subpopulations and implications for clinical trial design. Arthritis Res Ther 13:213
Felson DT (2010) Identifying different osteoarthritis phenotypes through epidemiology. Osteoarthritis Cartilage 18:601–604
Nelson AE, Smith MW, Golightly YM, Jordan JM (2014) “Generalized osteoarthritis”: a systematic review. Semin Arthritis Rheum 43:713–720
Kellgren JH, Moore R (1952) Generalized osteoarthritis and Heberden’s nodes. Br Med J 1:181–187
Forestier R, Francon A, Briole V, Genty C, Chevalier X, Richette P (2011) Prevalence of generalized osteoarthritis in a population with knee osteoarthritis. Joint Bone Spine 78:275–278
Gunther KP, Sturmer T, Sauerland S, Zeissig I, Sun Y, Kessler S, Scharf HP, Brenner H, Puhl W (1998) Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: the Ulm Osteoarthritis Study. Ann Rheum Dis 57:717–723
Min JL, Meulenbelt I, Riyazi N, Kloppenburg M, Houwing-Duistermaat JJ, Seymour AB, Pols HA, van Duijn CM, Slagboom PE (2005) Association of the frizzled-related protein gene with symptomatic osteoarthritis at multiple sites. Arthritis Rheum 52:1077–1080
Hoogeboom TJ, den Broeder AA, Swierstra BA, de Bie RA, van den Ende CH (2012) Joint-pain comorbidity, health status, and medication use in hip and knee osteoarthritis: a cross-sectional study. Arthritis Care Res (Hoboken.) 64:54–58
Hoogeboom TJ, den Broeder AA, de Bie RA, van den Ende CH (2013) Longitudinal impact of joint pain comorbidity on quality of life and activity levels in knee osteoarthritis: data from the Osteoarthritis Initiative. Rheumatology (Oxford) 52:543–546
Perruccio AV, Power JD, Evans HM, Mahomed SR, Gandhi R, Mahomed NN, Davis AM (2012) Multiple joint involvement in total knee replacement for osteoarthritis: effects on patient-reported outcomes. Arthritis Care Res (Hoboken.) 64:838–846
Suri P, Morgenroth DC, Kwoh CK, Bean JF, Kalichman L, Hunter DJ (2010) Low back pain and other musculoskeletal pain comorbidities in individuals with symptomatic osteoarthritis of the knee: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken.) 62:1715–1723
Moe RH, Grotle M, Kjeken I, Hagen KB, Kvien TK, Uhlig T (2013) Disease impact of hand OA compared with hip, knee and generalized disease in specialist rheumatology health care. Rheumatology (Oxford) 52:189–196
Hoogeboom TJ, Stukstette MJ, de Bie RA, Cornelissen J, den Broeder AA, van den Ende CH (2010) Non-pharmacological care for patients with generalized osteoarthritis: design of a randomized clinical trial. BMC Musculoskelet Disord 11:142
Vercoulen JH, Swanink CM, Fennis JF, Galama JM, van der Meer JW, Bleijenberg G (1994) Dimensional assessment of chronic fatigue syndrome. J Psychosom Res 38:383–392
van den Hoven LH, Gorter KJ, Picavet HS (2010) Measuring musculoskeletal pain by questionnaires: the manikin versus written questions. Eur J Pain 14:335–338
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MA, te Velde A, Verrips E (1998) Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 51:1055–1068
Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 33:AS264–AS279
Boers M, Jacobs JW, Vliet Vlieland TP, van Riel PL (2007) Consensus Dutch health assessment questionnaire. Ann Rheum Dis 66:132–133
Bruce B, Fries JF (2003) The Stanford health assessment questionnaire: dimensions and practical applications. Health Qual Life Outcomes 1:20
Beurskens AJ, de Vet HC, Koke AJ, Lindeman E, van der Heijden GJ, Regtop W, Knipschild PG (1999) A patient-specific approach for measuring functional status in low back pain. J Manipulative Physiol Ther 22:144–148
Rosengren J, Brodin N (2012) Validity and reliability of the Swedish version of the Patient Specific Functional Scale in patients treated surgically for carpometacarpal joint osteoarthritis. J Hand Ther 26:53–61
International Classification of Functioning, Disability and Health: ICF (2001) Geneva, Switzerland: World Health Organization. Available at http://www.who.int/classifications/icf/en/
Cieza A, Brockow T, Ewert T, Amman E, Kollerits B, Chatterji S, Ustun TB, Stucki G (2002) Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med 34:205–210
Rupp I, Boshuizen HC, Roorda LD, Dinant HJ, Jacobi CE, van den Bos G (2006) Course of patient-reported health outcomes in rheumatoid arthritis: comparison of longitudinal and cross-sectional approaches. J Rheumatol 33:228–233
Wolfe F, Michaud K, Li T, Katz RS (2010) EQ-5D and SF-36 quality of life measures in systemic lupus erythematosus: comparisons with rheumatoid arthritis, noninflammatory rheumatic disorders, and fibromyalgia. J Rheumatol 37:296–304
Bijsterbosch J, Scharloo M, Visser AW, Watt I, Meulenbelt I, Huizinga TW, Kaptein AA, Kloppenburg M (2009) Illness perceptions in patients with osteoarthritis: change over time and association with disability. Arthritis Rheum 61:1054–1061
van Groen MM, ten Klooster PM, Taal E, van de Laar MA, Glas CA (2010) Application of the health assessment questionnaire disability index to various rheumatic diseases. Qual Life Res 19:1255–1263
Dreinhofer K, Stucki G, Ewert T, Huber E, Ebenbichler G, Gutenbrunner C, Kostanjsek N, Cieza A (2004) ICF Core Sets for osteoarthritis. J Rehabil Med 44:75–80
Oberhauser C, Escorpizo R, Boonen A, Stucki G, Cieza A (2013) Statistical validation of the brief International Classification of Functioning, Disability and Health Core Set for osteoarthritis based on a large international sample of patients with osteoarthritis. Arthritis Care Res (Hoboken.) 65:177–186
Nelson AE, Elstad E, DeVellis RF, Schwartz TA, Golightly YM, Renner JB, Conaghan PG, Kraus VB, Jordan JM (2013) Composite measures of multi-joint symptoms, but not of radiographic osteoarthritis, are associated with functional outcomes: the Johnston County Osteoarthritis Project. Disabil Rehabil 36:300–306
Acknowledgments
We would like to thank all the participants of this study. Furthermore, we are grateful to Sylvia Karsenbarg and Dennis Konhuurne en Jasper Geerts for their contribution in the data collection.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuperus, N., Vliet Vlieland, T.P.M., Mahler, E.A.M. et al. The clinical burden of generalized osteoarthritis represented by self-reported health-related quality of life and activity limitations: a cross-sectional study. Rheumatol Int 35, 871–877 (2015). https://doi.org/10.1007/s00296-014-3149-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-014-3149-1