Abstract
Objective
Transsphenoidal surgery is the procedure of choice in Cushing disease (CD), with immediate post-operative remission rates ranging between 59 and 94 % and recurrence rates between 3 and 46 %, both depending upon the definition criteria and the duration of the follow-up. Our aim was to assess the rate of remission, recurrence and persistence of the disease after the first treatment and to identify predictors of remission in the CD population of our center.
Methods
Retrospective cohort study of the patients diagnosed of CD and with follow-up in our center between 1974 and 2011. We analyzed 41 patients (35 women and 6 men) with a mean age at diagnosis of 34 ± 13 years. The mean follow-up was 14 ± 10 years (range 1–37 years) and the median of follow-up period was 6.68 years.
Results
Thirty-five (85.4 %) patients underwent transsphenoidal surgery as first treatment option. Histopathological evidence of a pituitary adenoma was registered in 17 (48.5 %) patients. Thirty-two (78 %) patients achieved disease remission after the first treatment, 21 (65.6 %) of them presented disease recurrence. Persistent disease was observed in 9 (22 %) patients. Twelve (29.3 %) subjects developed post-surgical adrenal insufficiency, 7 of which (70 %) achieved stable remission. Two parameters were found to be significant predictors of remission after the first treatment: age at disease diagnosis and the development of adrenal insufficiency (cortisol <3 μg/dl) in the immediate post-operative state.
Conclusions
We report a high recurrence rate, at least partially attributable to the long follow-up time. Early post-surgery adrenal insufficiency predicts remission. Hypopituitarism was also very prevalent, and strongly associated with radiotherapy. These results lead us to the conclusion that CD needs a life-long strict follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cushing’s disease (CD), although rare, is the most common cause of endogenous hypercortisolism, with an incidence ranging from 1.2 to 2 patients/million per year. It is associated with reduced life expectancy and quality of life, and with an increase in cardiometabolic risk that persists until several years after remission. The endogenous hypercortisolism causes an increase in morbidity through changes in body composition (central obesity, osteoporosis and sarcopenia), a prothrombotic state, impaired metabolic profile (dyslipidemia, insulin resistance and type 2 diabetes mellitus), and hypertension [1–3].
The most common cause of CD is the the ACTH-secreting pituitary microadenoma; nowadays, its surgical resection is the first choice of treatment for the control of hypercortisolism. In case of surgical failure or recurrence of the disease the second line of treatment may be a second surgical intervention, radiotherapy or bilateral adrenalectomy. Medical therapy is used for the control of hypercortisolism when remission is delayed or not achieved [1–3].
Transsphenoidal surgery (TSS) remains the procedure of choice with immediate post-operative remission rates ranging between 59 and 94 % in specialized centers. This wide range is due to the variability in defining remission in each study, the inclusion or not of macroadenomas, the number of the patients studied and the experience of surgical team [2, 4–19].
Recurrence rate of CD ranges between 3 and 46 %, depending both on the definition criteria and the duration of the follow-up. In different series, with various post-operative protocols, several factors are identified that can predict the evolution of CD. The most remarkable is postoperative hypocortisolism, identified by serum cortisol levels ranging from <1.8 to <5 mcg/dl in different studies, and a prolonged postoperatory suppression of the hypothalamic–pituitary–adrenal axis, which has been associated with a significant low rate of disease recurrence [4–20].
From this background on, we decided to perform a review of the patients with CD followed in our center from the 70’s to the present, in order to assess the rate of remission, recurrence and persistence of the disease after the first treatment; to evaluate the presence of co-morbidities before treatment and after remission; to identify predictors of remission; and to quantify the presence of hypopituitarism after several years of follow-up.
Materials and methods
Patients cohort
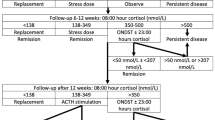
Retrospective cohort study of patients diagnosed of CD between 1974 and 2011 followed in the Endocrinology Department of the Hospital Clínic of Barcelona. Data were collected from the medical history records (Fig. 1).
We included all patients with diagnosis and follow-up in our center and excluded patients referred only for specific procedures such as inferior petrosal sinus sampling (IPSS), in whom we lacked follow-up data. We analyzed 41 patients (35 women and 6 men) with a mean age at diagnosis of 34 ± 13 years (15–64). Thirty-five patients underwent transsphenoidal surgery as the first treatment. Bilateral adrenalectomy was employed as first line therapy in three patients diagnosed before 1980 and radiotherapy in other three diagnosed between 1980 and 1989.
Pre-surgical assessment
The diagnosis of endogenous hypercortisolism was confirmed by increased urinary free cortisol (UFC), loss of circadian rhythm (evidenced by high midnight cortisol levels measured in serum until 2007, and in salivary samples thereafter) and lack of suppression of cortisol secretion after either a single 1 mg dose, or 0.5 mg/6 h/48 h dexamethasone.
Diagnosis of ACTH-dependent hypercortisolism of pituitary origin was established following both the European Society of Endocrinology (ESE) and the endocrine society guidelines, by the 8 mg dexamethasone test.
Pituitary magnetic resonance imaging (MRI) was performed in most patients for tumor localization, except in some of the earlier cases in whom computed tomography (CT) was employed. Fifteen patients underwent IPSS; in all cases it confirmed the pituitary origin. IPSS indications were the absence of a tumor on MRI (normal MRI) in eight patients, an uncertain image in three patients, a partially empty sella in one patient, and a suspected ectopic origin in the remaining three. Differential diagnosis between pituitary and ectopic ACTH dependent Cushing syndrome was mainly based on the 8 mg DST, but all doubtful cases, inconclusive or suspicious of ectopic origin and patients with normal pituitary MRI underwent IPSS. All 14 IPSS (11 for negative MRI and 3 for suspected ectopic ACTH) confirmed the pituitary origin of ACTH.
Data on cardiometabolic comorbidities at diagnosis, namely obesity (body mass index ≥30 kg/m2), acute atherothrombotic events, hypertension, type 2 diabetes mellitus (DM2) and dyslipidemia were either obtained from the clinical history or deduced from the medical therapy with antihypertensive, oral antidiabetic or lipid-lowering drugs. Osteoporosis (defined by a T score less than –2.5 on lumbar densitometry), hypogonadism and other clinical symptoms considered to be secondary to the endogenous hypercortisolism were also registered.
Surgical approach
Due to the long period of time encompassed by our review (almost 40 years), procedures have evolved and changed. Furthermore, neurosurgical treatment in our cohort has been successively performed by two teams, one prior to 2003, and other from that year on. Surgery consisted in selective transsphenoidal adenomectomy in 31 patients, transsphenoidal hemi-hypophysectomy in three patients and hypophysectomy in one patient. Transsphenoidal endoscopic surgery was introduced since 2005. Moreover three patients underwent bilateral adrenalectomy as a first line treatment.
Post-surgical assessment
The mean follow-up of the serie was 14 ± 10 years (range 1–37 years) and the median of follow-up was 6.68 years. Patients were evaluated postoperatively at 48 h and 1 month, then every 3–4 months during the first year or till remission, every 6 months in the second year and annually thereafter. Comorbidities as defined above were registered all along follow-up.
Persistent disease was defined by the persistence after treatment of endogenous hypercortisolism, demonstrated by the high UFC levels, by the increased midnight salivary cortisol from 2007 on, and by the persistence of clinical features.
Remission was defined as either post-operative cortisol insufficiency with the need for glucocorticoid (GC) replacement treatment or normalization of hypercortisolism and recovery of the circadian rhythm of serum or salivary cortisol with normal functional tests excluding recurrence of the disease.
Recurrence of the disease was defined in most patients by the lack of suppression of cortisol after 1 mg dexamethasone and, in a few, after 0.5 mg/6 h for 48 h, together with elevated UFC and/or midnight salivary cortisol after a period of remission and by the reappearance of hypercortisolaemic features.
Moreover in every patient functional tests were performed, like low dose suppression test with DST 1 mg or 0.5 mg/6 h/2 days. In conclusion all patients underwent the same diagnostic tests, either to confirm remission, recurrence or persistence of disease.
-
Adrenal Insufficiency: has been defined by the presence of serum cortisol level below 3 mcg/dl.
-
Time of disease activity: time of exposure to hypercortisolism, arbitrarily considered from diagnosis to remission.
-
Exposure time before diagnosis/durations of symptoms before diagnosis: although we believe that it is a subjective parameter we have included it in the analysis. We considered the time from onset of symptoms to diagnosis.
To assess possible predictors of remission in our cohort, we divided it firstly into two groups; patients in remission versus patients with persistent disease after the first treatment. Thereafter we divided it into three groups: patients in remission after first treatment, patients in remission after two or more treatments and patients with persistent disease. Moreover, we anlysed the whole cohort by dividing it into groups according to time of disease activity: <5 years, between 5 and 10 years and over 10 years. Finally, we compared the last decade versus the previous period, in order to quantify changes between surgical teams and to evaluate changes in time.
Laboratory parameters
Hormonal analysis was performed in the hormonal laboratory of our center applying the standard procedures.
Statistical analysis
Quantitative data are presented as median and range, compared between groups with non-parametric test and ANOVA when more than two groups were involved. Categorical data are summarized as counts and percentages of subjects in each category and compared with Chi square or Fisher’s exact test. A logistic regression model was employed to identify predictors of remission. Statistical significance was set at a P value <0.05. Data were analyzed with the statistic software SPSS 17.
Results
Baseline data
Of the 41 patients included in the study, 35 (85.4 %) were females. The mean age at diagnosis was 34 ± 13 years (range 15–64 years). The most frequent clinical features were weight gain in 24 (58.5 %), hypogonadism in 20 (48.8 %) and hirsutism in 5 (12.2 %). The laboratory characteristicas were: UFC 336.9 ± 140.6 μg/24 h (NV: 20–100 μg/24 h), mean basal serum cortisol 26.6 ± 7.8 μg/dl (NV: 10–25 μg/dl), mean night serum cortisol 23 ± 9.8 μg/dl (NV: 2–10 µg/dl), serum ACTH 67.7 ± 38.26 pg/ml (NV: 10–60 pg/ml), mean serum cortisol after 1 mg overnight dexamethasone suppression test 14.3 ± 5.7 μg/dl (VN <1.8 μg/dl) and mean serum cortisol after 8 mg dexamethasone suppression test 6.3 ± 5.7 μg/dl (<50 % of baseline cortisol). Of all 38 pituitary images analyzed, 10 patients (24.4 %) had no visible adenoma on pituitary CT or MRI and three (7.3 %) had an empty sella. Six patients (14.6 %) had a macroadenoma and 19 (46.3 %) had a microadenoma. No pituitary images were available from three patients. The diagnosis of micro or macroadenoma was based on the pituitary imaging reports.
Treatment outcomes
Thirty-five (85.4 %) patients underwent transsphenoidal surgery as first treatment option, three patients underwent bilateral adrenalectomy and adjuvant pituitary radiotherapy and other three were initially treated with conventional 3D pituitary radiotherapy. These last six patients were diagnosed and treated before 1985.
Histopathological evidence of a pituitary adenoma was reported in seventeen (48.5 %) patients, while in 11 (31.4 %) cases histological findings were informed as normal pituitary. Seven out of the 11 patients with negative pituitary pathology had underwent IPSS, which confirmed the pituitary origin of ACTH production in all of them. IPSS had not been performed in the remaining four patients as all standard functional tests had been consistent with the central source, and they had a pituitary microadenoma on MRI.
Thirty-two (78 %) patients achieved disease remission after the first treatment; 21 (65.6 %) of them presented disease recurrence. Mean time to recurrence was 2.4 ± 1.7 years (range 0.5–5 years). Persistent disease was observed in 9 (22 %) patients. Twelve (29.3 %) subjects developed post-surgical adrenal insufficiency. Mean time to recovery of the hypothalamic–pituitary–adrenal axis was 20.8 ± 27.0 (0.5–84) months (Table 1).
Co-morbidities at diagnosis and after remission
The prevalence of co-morbidities at diagnosis was: hypertension in 17 (41.5 %) patients, DM2 in 6 (14.6 %), obesity in 29 (70.7 %), dyslipidemia in 18 (43.9 %), osteoporosis in 10 (24.4 %), osteopenia in 7 (17.1 %), hypogonadism in 20 (48.8 %) and hirsutism in 5 (12.2 %) patients. After remission of Cushing’s disease, the only significant change was observed in the rate of obesity, which was reduced from 29 of 41 initially to 15 of 35 (χ2: 5.98, *P: 0.014). Mean time of remission in patients who were evaluated was 11.7 ± 9.2 years (range 1–33 years).
Major cardiovascular events (stroke, myocardial infarction, pulmonary thromboembolism) were registered in three patients: one patient had a stroke at the time of CD diagnosis; one suffered a myocardial infarction and other one had a stroke, both after CD remission.
Overall lethality index was 7.3; 75 % (2/3) being females. Death causes were neoplasia in two patients, one of sigma adenocarcinoma and the other one of lymphoma, both after long term remission and the third patient in the early postoperative state of a reintervention for an invasive macroadenoma.
Predictors of remission of Cushing’s disease
One parameter was found to be a statistically significant predictor of remission after the first treatment: the development of adrenal insufficiency in the immediate postoperative state [*P: 0.03 Exp (B) 0.129 CI 0.02–00.8]. Another parameter found was age at disease diagnosis, although at the limit of statistically significance [P: 0.05 Exp (B) 1.08 CI 0.9–1.1].
When we subdivide the cohort of patients in a group with active disease, another one cured after the first treatment intent and a third one cured after several treatments, we observe differences between these groups in terms of duration of symptoms, levels of morning and midnight serum cortisol at baseline, and the time of follow-up (Table 2). Interestingly, if we divide the cohort according to the time of disease activity there are no significant differences between groups (Table 3).
No statistically significant differences were observed when we divided the cohort in two groups according to the year of diagnosis and treatment, and compare the last decade with the years before.
Hypopituitarism rates
Hypopituitarism rate is high in our cohort. At least one hormone deficiency is present in 22 (53.7 %) patients, including corticotropin deficit in 18 (43.9 %) patients; gonadotropin deficit in 12 (29.3 %); somatotropin deficit in 14 (34.1 %) and thyrotropin deficit in 14 (34.1 %) patients. When considering only patients in remission, hypopituitarism rate is 60.6 % and panhypopituitarism in 33.3 %. Corticotropin deficit was observed in 17 (51.5 %) patients, gonadotropin deficit in 10 (30.3 %); somatotropin deficit in 11 (33.3 %) and thyrotropin deficit in 12 (36.4 %). Patients who have received radiotherapy had more hypopituitarism 17/20 versus 7/14 (P: 0.05).
Discussion
The present study was designed to describe and investigate recurrence rates and potential contributing factors to recurrence in a large cohort of patients with CD treated in our centre and with a prolonged follow-up. This is one of the longest follow up studies underwent so far.
Our population presented a clear female predominance, with a male to female ratio of 1:5.8, quite higher than previously described series that range from 1:2 to 1:13 [3, 21]. The mechanisms involved in gender differences in CD are unknown; however, estrogen responsiveness of corticotroph adenoma tissue has been implicated [22, 23].
The most frequently registered co-morbidities at diagnosis were obesity, hypogonadism and hypertension. Our data on clinical features present at diagnosis support previous findings [3].
Mortality was slightly lower in our series than in older meta-analyses [24] and other recent reported series a [25, 26], maybe due to the fact that there was no cardiovascular death. To note, that in our cohort the prevalence of cardiovascular events from diagnosis to post-remission follow-up is low. This may be due to the retrospective nature of our analysis, as minor thromboembolic events, like peripheral thrombosis, may be underrated in medical files, even though we cannot consider that mortality has been underrated.
Nevertheless, cardiovascular clinical morbidity and mortality is lower than in the other series reported in the literature. Although the small simple size could be the argue, this results make us speculate that this could be due to the low global cardiovascular mortality reported in the nord-spanish Mediterranean regions as compared with other European populations [27].
The observed remission rate after the first treatment was of 78 %, with disease recurrence in 65.6 % of our patients. Remission rates, persistence and recurrence in the literature, are of 59–90, 10–24 and 5–22 % respectively [4–20]. Therefore, when we compare with the data from our serie, our remission rate is in the low average range. When considering only patients with a diagnosis and treatment in the last 10 years, our remission rate increases to 85.7 %, fact that can be warranted by the advance in the transsphenoidal surgery approach.
While the rate of persistence of the disease after the first treatment is similar to the series described, our recurrence rate after the first curative treatment is higher (21/32), reaching 60 % of the study population, and being therefore one of the highest described so far, probably due to the long period of time and follow up of our cohort. If we consider only the last 10 years, the recurrence rate decreases to 42.9 %. Patients with either persistent or recurrent CD underwent further treatments, such as a second transsphenoidal surgery and/or radiotherapy, and even bilateral adrenalectomy in selected cases. CD recurred along follow-up in 32 of the patients with remission after their first treatment. Early adrenal insufficiency is a significant predictor of remission; 75 % of the patients with early adrenal insufficiency achieved stable remission, while this was present only in 23 % of the patients with recurrence of the disease.
The identification of factors predictive of postoperative clinical outcomes is important for both patients’ counselling and to guide further management. Previously suggested predictors of remission and cure of CD include age at diagnosis, presence of hypertension or diabetes [3, 24], early and 6-week postoperative serum cortisol [20, 28, 29], early postoperative serum ACTH [9], ACTH response to CRH testing [30], postoperative metyrapone [31], desmopressin testing [32], low-dose dexamethasone testing [33], identification of tumor at surgery and an adenoma histology positive for corticotropinoma [29, 34]. Our study confirmed the previous findings on the predictive value of a low early postoperative serum cortisol and probably the age at diagnosis. The limited statistical power of this second factor may be due to the small number of the sample.
Recent data have suggested that positive preoperative MRI findings are associated with a higher chance of achieving initial remission [19]. However, our data support previous work in which preoperative MRI findings are not predictive of long term cure [35].
Following pituitary surgery, careful ongoing expert endocrine assessment is mandatory. Relapse incidence increases as follow-up extends, and also as endocrine assessment becomes more thorough [5, 36]. In our cohort, follow-up time was associated with a higher rate of relapse, the longer the follow-up the greater the chance of relapse. But reassessing all the follow-up data, our conclusion is that our results are partly due to the relatively long follow-up. In our view, the main reason of the early recurrence was the surgical outcome of the study population. Considering only the last 10 years, the recurrence rate drops to 42 % and a there was also a decrease in the number of negative pituitary pathologic studies. We can conclude that our surgical results have improved in recent years, although the comparison did not reach statistical significance.
The overall rate of hypopituitarism observed in our series was 53.7 %, significantly higher when compared to other studies [3, 20]. Panhypopituitarism was observed in 29.3 %. Isolated corticotropin deficit was observed in 43.9 %, somatotropin and thyrotropin in 34.1 % and gonadotropin in 29.3 %, in concordance with data found in the literature. The high rate of hypopituitarism is possibly due to the multiple treatments that many of these patients have undergone due to the disease recurrence or persistence.
The retrospective nature of our study, covering a time span of about 35 years, is its main limitation, as it implies great difficulties in obtaining complete medical records, variations along the years in definitions of disease activity, changes in procedures and protocols, and even in the surgical team. On the other hand, it may allow to achieve better understanding of the long-term course of this complex disease.
References
Steffensen C, Bak AM, Rubeck KZ, Jorgensen JO (2010) Epidemiology of Cushing’s syndrome. Neuroendocrinology 92(Suppl 1):1–5
Alexandraki K, Kaltsas G, Isidori A, Storr H, Grossman A (2013) Long-term remission and recurrence rates in Cushing’s disease: predictive factors in a single-centre study. Eur J Endocrinol 168(4):639–648
Hassan-Smith Z, Sherlock M, Wiebke Arlt R, Ayuk J, Stewart P (2012) Outcomes of Cushing’s disease following transsphenoidal Surgery in a single center over 20 years. J Clin Endocrinol Metab 97(4):1194–1201
Rees DA, Hanna FW, Davies JS, Mills RG, Vafidis J, Sacanlon MF (2002) Long-term follow-up results of transsphenoidal surgery for Cushing’s disease in a single centre using strict criteria for remission. Clin Endocrinol 56(4):541–551
Atkinson AB, Kennedy A, Wiggam MI, McCance DR, Sheridan B (2005) Long-term remission rates after pituitary surgery for Cushing’s disease: the need for long-term surveillance. Clin Endocrinol 63(5):549–559
Tritos NA, Biller BM, Swearingen B, Management of Cushing’s disease (2011) Nature Reviews. Endocrinology 7(5):279–289
Czepielewski MA, Rollin GA, Casagrande A, Ferreira NP (2007) Criteria of cure and remission in Cushing’s disease: an update. Arq Bras Endocrinol Metabol 51(8):1362–1372
Chen JC, Amar AP, Choi S, Singer P, Couldwell WT, Weiss MH (2003) Transsphenoidal microsurgical treatment of Cushing’s disease: postoperative assessment of surgical efficacy by application of an overnight low-dose dexamethasone suppression test. J Neurosurg 98(5):967–973
Flitsch J, Knappe UJ, Lüdecke DK (2003) The use of postoperative ACTH levels as a marker for successful transsphenoidal microsurgery in Cushing’s disease. Zentralblatt für Neurochirurgie 64(1):6–11
Hammer GD, Tyrrell JB, Lamborn KR, Applebury CB, Hannegan ET, Bell S, Rahl R, Lu A, Wilson CB (2004) Transsphenoidal microsurgery for Cushing’s disease: initial outcome and long-term results. J Clin Endocrinol Metab 89(12):6348–6357
Hoffmann BM, Fahlbusch R (2006) Treatment of Cushing’s disease: a retrospective clinical study of the latest 100 cases. Front Horm Res 34:158–184
Rollin G, Ferreira NP, Czepielewski MA (2007) Prospective evaluation of transsphenoidal pituitary surgery in 108 patients with Cushing’s disease. Arq Bras Endocrinol Metabol 51(8):1355–1361
Pouratian N, Prevedello DM, Jagannathan J, Lopes MB, Vance ML, Laws ER Jr (2007) Outcomes and management of patients with Cushing’s disease without pathological confirmation of tumor resection after transsphenoidal surgery. J Clin Endocrinol Metab 92(9):3383–3388
Hofmann BM, Hlavac M, Martinez R, Buchfelder M, Müller OA, Fanhlbusch R (2008) Long-term results after microsurgery for Cushing’s disease: experience with 426 primary operation over 35 years. J Neurosurg 108(1):9–18
Prevedello DM, Pouratian N, Sherman J, Jane JA, Vance ML, Lopes MB, Laws ER Jr (2008) Management of Cushing’s disease: outcome in patients with microadenoma detected on pituitary magnetic resonance imaging. J Neurosurg 109(4):751–759
Patil CG, Prevedello DM, Lad SP, Vance ML, Thorner MO, Katznelson L, Laws ER Jr (2008) Late recurrence of Cushing’s disease after initial successful transsphenoidal surgery. J Clin Endocrinol Metab 93(2):358–362
Jagannathan J, Smith R, DeVroom HL, Vortmeyer AO, Stratakis CA, Nieman LK, Oldfield EH (2009) Outcome of using the histological pseudocapsule as a surgical capsule in Cushing’s disease. J Neurosurg 111(4):531–539
Valassi E, Biller BM, Swearingen B, Pecori Giraldi F, Losa M, Mortini P, Hayden D, Cavagnini F, Klibanski A (2010) Delayed remission after trassphenoidal surgery in patients with Cushing’s disease. J Clin Endocrinol Metab 95(2):601–610
Ciric I, Zhao JC, Du H, Findling JW, Molitch ME, Weiss RE, Refetoff S, Kerr WD, Meyer J (2012) Transsphenoidal surgery for Cushing’s disease: experience with 136 patients. Neurosurgery 70(1):70–81
Costenaro F, Rodrigues T, Rollin G, Ferreira N, Czepielewski M (2013) Evaluation of Cushing’s disease remission after transs phenoidal surgery based on early serum cortisol dynamics. Clin Endocrinol. doi:10.1111/cen.12300
Sherlock M, Ayuk J, Tomlinson JW, Toogood AA, Aragon Alonso A, Sheppard MC, Bates AS, Stewart PM (2010) Mortality in patients with pituitary disease. Endocr Rev 31(3):301–342
Pecori GF, Moro M, Cavagnini F (2003) Gender related differences in the presentation and course of Cushing’s disease. J Clin Endocrinol Metab 88(4):1554–1558
Chaidarun SS, Alexander JM (1998) A tumor-specific truncated estrogen receptor splice variant enhances estrogen-stimulated gene expression. Mol Endocrinol 12(9):1355–1366
Clayton RN, Raskauskiene D, Reulen RC, Jones PW (2011) Mortality and morbidity in Cushing’s disease over 50 years in Stroke-on-Trent UK: audit and meta-analysis of literature. J Clin Endocrinol Metab 96(3):632–642
Ntali G, Asimakopoulou A, Siamatras T, Komninos J, Vassiliadi D, Tzanela M, Tsagarakis S, Grossman AB, Wass JA, Karavitaki N (2013) Mortality in Cushing’s syndrome: systematic analysis of a large series with prolonged follow-up. Eur J Endocrinol 169(5):715–723
Yaneva M, Kalinov K, Zacharieva S (2013) Mortality in Cushing’s syndrome: data from 386 patients from a single tertiary referral center. Eur J Endocrinol 169(5):621–627
Müller-Nordhorn J, Binting S, Roll S, Willich SN (2008) An update on regional variation in cardiovascular mortality within Europe. Eur Heart J 29(10):1316–1326
Esposito F, Dusick JR, Cohan P, Moftakhar P, McArthur D, Wang C, Swerdloff RS, Kelly DF (2006) Clinical review: early morning cortisol levels as a predictor of remission after transsphenoidal surgery for Cushing’s disease. J Clin Endocrinol Metab 91(1):7–13
Martino J, Acebes JJ, Montanya E, Masuet C, Brell M (2007) Analysis of early prognostic factor for Risk of treatment failure in Cushing’s disease treated by trans-sphenoidal pituitary surgery. Med Clin 128(9):330–332
Nishizawa S, Oki Y, Ohta S, Yokota N, Yokoyama T, Uemura K (1999) What can predict postoperative “endocrinological cure” in Cushing’s disease? Neurosurgery 45(2):239–244
Alwani RA, de Herder WW, van Aken MO, van den Berge JH, Delwel EJ, Dallenga AH, De Jong FH, Lamberts SW, van der Lely AJ, Feelders RA (2010) Biochemical predictors of outcome of pituitary surgery for Cushing’s disease. Neuroendocrinology 91(2):169–178
Losa M, Bianchi R, Barzaghi R, Giovanelli M, Mortini P (2009) Persistent adrenocorticotropin response to desmopresin in the early postoperative period predicts recurrence of Cushing’s disease. J Clin Endocrinol Metab 94(9):3322–3328
McCance DR, Gordon DS, Fannin TF, Hadden DR, Kennedy L, Sheridan B, Atkinson AB (1993) Assessment of endocrine function after transsphenoidal surgery for Cushing’s disease. Clin Endocrinol 38(1):79–86
Acebes JJ, Martino J, Masuet C, Montanya E, Soler J (2007) Early postoperative ACTH and cortisol as predictors of remission in Cushing’s disease. Acta Neurochir 149:471–479
Salevane S, Gatta B, Pecheur S, San-Galli F, Visot A, Lasjaunias P, Roger P, Berge J, Young J, Tabarin A, Chanson P (2007) Pituitary magnetic resonance imaging findings do not influence surgical outcome in adrenocorticotropin-secreting microadenomas. J Clin Endocrinol Metab 89(7):3371–3376
Dimopoulou C, Schopohl J, Rachinger W, Buchfelder M, Honegger J, Reincke M, Stalla GK (2014) Long-term remission and recurrence rates after first and second transsphenoidal surgery for Cushing’s disease: care reality in the Munich Metropolitan Region. Eur J Endocrinol 170(2):283–292
Conflict of interest
The authors have nothing to declare. The present work has no financial sponsorship. The authors are staff members of the public entities Hospital Clinic, CIBERDEM, IDIBAPS and University of Barcelona.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. A. Hanzu and I. Halperin have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Aranda, G., Enseñat, J., Mora, M. et al. Long-term remission and recurrence rate in a cohort of Cushing’s disease: the need for long-term follow-up. Pituitary 18, 142–149 (2015). https://doi.org/10.1007/s11102-014-0567-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0567-8