Abstract
Background Medication errors are avoidable events that may occur at any stage of the medication use process. Implementing a clinical pharmacist is one strategy that is believed to reduce the number of medication errors. Pediatric patients, who are more vulnerable to medication errors due to several contributing factors, may benefit from the interventions of a pharmacist. Aim of the review To qualitatively and quantitatively evaluate the impact of clinical pharmacist interventions on medication error rates for hospitalized pediatric patients. Methods PubMed, EMBASE, Cochrane Controlled Trials Register and Google Scholar search engines were searched from database inception to February 2020. Study selection, data extraction and quality assessment was conducted by two independent reviewers. Observational and interventional studies were included. Data extraction was done manually and the Crowe Critical Appraisal Tool was used to critically appraise eligible articles. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated using a random-effects model for rates of medication errors. Results 19 studies were systematically reviewed and 6 studies (29,291 patients) were included in the meta-analysis. Pharmacist interventions involved delivering educational sessions, reviewing prescriptions, attending rounds and implementing a unit-based clinical pharmacist. The systematic review indicated that the most common trigger for pharmacist interventions was inappropriate dosing. Pharmacist involvement was associated with significant reductions in the overall rate of medication errors occurrence (OR 0.27; 95% CI 0.15 to 0.49). Conclusion Pharmacist interventions are effective for reducing medication error rates in hospitalized pediatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
A clinical pharmacist caring for pediatric patients can reduce the rates of medication errors.
-
Direct pharmacist involvement in education, direct patient care, therapeutic drug monitoring, drug distribution oversight and quality improvement have been demonstrated to reduce the rates of medication errors in pediatric patients.
-
Dosing errors are the most common medication errors occurring in hospitalized pediatric patients.
Introduction
Patient safety is one of the core goals in all healthcare systems and is a key step to ensure the provision of a high-quality care to patients [1]. Medication errors (ME) and preventable adverse drug events (ADEs) can take place in any healthcare system and can lead to patient harm [2]. Medication errors encompasses all events that could occur at any stage of the medication use process including prescribing, transcribing, dispensing, administering and monitoring a medication. On the other hand, preventable ADEs are injuries resulting from medication use and may sometimes be a result of medication errors [3].
Pediatric patients are more prone to experience a medication error in a health care setting, and when such events occur, these errors have three times the potential to cause direct patient harm as compared to adult patients [4, 5]. Factors such as complex dosing, varying growth and development processes, availability and accuracy of dosage forms, the use of off-label formulations, limited physiologic reserves to buffer potential overdose errors, and variable communication capabilities all contribute to additional risks for medication errors in this population[4, 6,7,8]. These factors highlight the need for pediatric-specific prevention strategies for reducing medication errors and preventable ADEs.
Several strategies have been investigated to reduce the occurrence of these events in health care settings. One such strategy is the implementation of a clinical pharmacist within the ward. The clinical pharmacist’s role has been evolving over the past decades as a healthcare practitioner who has expertise in appropriate safe and effective medication use [9]. Several systematic reviews and meta-analyses have indicated that a clinical pharmacists’ interventions may reduce medication errors and preventable ADEs in hospitalized patients, including events that could lead to actual harm before reaching the patients. In addition, these interventions improved the quality of care provided to patients and reduced the overall cost of health which enhanced the efficiency of healthcare [10,11,12,13,14,15]. However, the majority of these studies focus on having a clinical pharmacist intervening with adult patients. Therefore, it is essential to study the effect of a clinical pharmacist caring for pediatric patients, given that they are more vulnerable to medication errors.
Aim of the review
The aim of this systematic review and meta-analysis is to evaluate the impact of clinical pharmacist interventions on reducing medication errors and preventable ADEs for pediatric patients in hospital settings and evaluate the overall quality of the available evidence.
Method
This systematic review and meta-analysis follows the recommendations by the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines and the Cochrane Handbook guidelines, to ensure inclusion of relevant information. The protocol of the study is registered with the International Prospective Register of Systematic Reviews (PROSPERO)—CRD42019126541[16].
Scope and search strategy
A Systematic review of published works was conducted to evaluate the role of pharmacist intervention on medication errors for inpatient pediatric patients. The following electronic databases were searched from inception until February 2020 to identify eligible articles: Ovid MEDLINE®, EMBASE, The Cochrane Database of Systematic Reviews, and Google Scholar. In addition, reference lists of the resulted systematic review articles were manually searched to locate additional relevant articles that were not identified through the database search.
The following Medical Subject Headings [MeSH] and keywords were incorporated using ‘OR’: ‘pediatric(s), ‘child’, ‘children’, ‘neonate’, ‘infant(s)’, ‘adolescent(s)’. These were combined with the following using ‘AND’: ‘pharmacist(s)’, ‘Pharm* intervention’. The results from this search were combined with the following using ‘AND’: ‘medication errors’, ‘prescribing error’, ‘preventable adverse drug reaction’, ‘medication discrepancy’, ‘inappropriate prescribing’, ‘safe prescribing’, ‘mistake’. The result of this search was limited further to ‘English language’ and ‘Human species’.
Study selection and eligibility criteria
Studies were considered for inclusion if the primary focus was the assessment of medication errors as expressed as a rate or percentage. Appropriate study settings included hospital environments with a clear designation of including pediatric patients. A clear intervention directly involving a clinical pharmacist was necessary for inclusion. Only articles published in English were included. Editorials, commentaries or case-studies were excluded.
Study selection
Potential articles were first screened by title and abstract. EndNote X8® (2019 Clarivate) was used to remove duplicates and organize the reference list. Those that were of potential relevance were read independently by 2 authors to determine whether they met the inclusion criteria. Discrepancies were reviewed by study authors.
Data extraction
Two authors independently extracted study data using a standardized form which included the study authors and year, country, study design, hospital unit, study population characteristics, pharmacist intervention, and outcomes obtained for medication errors. Discrepancies were reviewed by study authors.
Quality assessment
Quality of the included articles was assessed using Crowe Critical Appraisal Tool (CCAT) version 1.4 [17, 18]. This tool was selected as it was anticipated from other systematic reviews that studies included would have significantly different methodologies. The CCAT is divided into 8 categories and 22 items. Each item has multiple descriptors for ease of appraisal with each category receiving its own score on a 6 point scale (0–5). An overall score for each study can be expressed out of a total score of 40 points. Two independent raters assessed each study. Discrepancies were resolved after discussion between authors. Intraclass correlation coefficient (ICC) was calculated using IBM SPSS® statistical software version 22 to measure the consistency between the two raters in order to insure reliability.
Statistical analysis
Studies that reported a similar primary outcome measure with a numerical difference between medication errors for pre- and post-intervention were included in the meta-analysis. Meta-analysis was conducted using Cochrane Review Manager Software (RevMan 5.3; Nordic Cochrane Centre, Copenhagen, Denmark). A random-effects model was used to estimate the pooled odds ratios (ORs) for the primary analyses as heterogeneity is expected owing to the different settings (departments within the hospital) and different types of pharmacist intervention. Together with 95% confidence intervals (CIs), ORs and weighted mean differences were derived for dichotomous variables. Statistical heterogeneity among studies was evaluated using I2 and P values.
Results
Identification and selection of studies
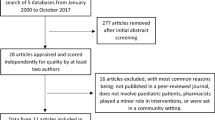
The electronic search yielded 598 citations and 8 additional records were identified from reference lists of included studies. After removal of duplicates, a total of 559 title and abstracts were screened for inclusion. A total of 67 full articles were screened of which 19 were included in this review. (Figure 1).
Characteristics of included studies
Major characteristics of the included studies are presented in Tables 1 and 2 for studies that showed numerical difference and studies that reported types of errors respectively. Of the 19 studies included, 11 were retrospective or prospective cohort studies [8, 19,20,21,22,23,24,25,26,27,28], 6 before-after studies [4, 29,30,31,32,33] and two cross–sectional observational studies [9, 34]. Most of the studies were conducted in the USA (n = 5) [8, 19, 21, 22, 24] followed by Spain (n = 3) [9, 23, 30], Netherlands (n = 2) [27, 31], Egypt (n = 2) [4, 33], one multicenter study across Europe [28] and one each from Canada[26], Brazil [34], Malaysia [32], India [25], Pakistan[29] and Saudi Arabia [20]. Only four studies were confined to multicenter [8, 23, 24, 28]. The majority of studies involved various hospital departments (n = 8) [8, 19, 21, 22, 24, 26,27,28] and three each from a neonatal intensive care unit (NICU) [25, 30, 31] and general medical ward [20, 29, 32]. Only two studies were conducted in the pediatric intensive care unit (PICU) [4, 34] and one in the pediatric surgery department [33], while the remaining two did not specify the hospital ward or unit [9, 23]. The two main pharmacist interventions were educational sessions (n = 5) [29,30,31,32,33] and review/validation of medication orders (n = 5) [9, 21, 23, 26, 27]. There were three studies for implementing a unit-based clinical pharmacist [19, 24, 28] and applying multiple interventions, such as combining monitoring medication orders and attending rounds [4, 8, 34], two studies for attending rounds [22, 25] and one study for implementing medication safety program designed and filled by pharmacist [20].
Quality of included studies
Two raters appraised each of the 19 studies, which resulted in 38 independent CCAT evaluations, the total score ranged from 16 to 35.5 out of 40. ICC showed a range of 0.948–0.997 for all studies which indicates high similarity between raters, thus excellent reliability (Table 3) [35]. The overall assessment mean for all studies was 27.87 out of 40 points with standard deviation of 6.04. Within the CCAT the sections the highest scores were for preliminary (4.18/5) and introduction (4.11/5), while the lowest were for ethics (2.89/5) and sampling (2.58/5). The mean scores by study and domain are summarized in Table 3.
Types of medication errors that prompted pharmacist interventions
Nineteen studies were included in this analysis. Of this, 13 studies had wrong dose as one of the three most common reasons for intervention [4, 9, 20, 21, 23,24,25,26,27,28, 30, 33, 34], reported as inappropriate dosing including overdosing or underdosing. Wrong drug was one of the top three causes for intervention in four articles which resulted in recommending an alternative therapy [22,23,24, 26]. Another type of error that also led to modification of therapy was for drug interaction and was among the three top reasons for pharmacist involvement in two studies [20, 25]. Three studies reported missing information (e.g. weight or date of birth) [9, 21, 22], inappropriate formulation [23, 26, 27], and wrong frequency [4, 29, 31] among the most common three triggers for intervention. Six studies rated the severity of pharmacist interventions: three showed that most interventions were moderate [4, 25, 31], and two were severe [9, 23]. One study revealed that out of 616 preventable errors, only 120 were harmful [8]. Five studies reported the acceptance rate of pharmacist interventions, of this, four studies showed an acceptance rate more than 55% [9, 23, 25, 27]. The remaining study showed acceptance rate of 83% without changing regimen [28].
Studies reporting quantitative outcomes of pharmacist interventions
Seven studies were included in this analysis. Six before-after studies were included in this analysis as they reported the number of medication errors pre and post intervention [4, 29,30,31,32,33]. One cohort study was excluded because it reported the results in error per patient-days [19]. Of the six studies included in the meta-analysis, five implemented an educational sessions designed and delivered by pharmacist to nurses and physicians [29, 30, 32, 33]. Five of six studies showed significant reduction (P < 0.0001) in the incidence of medication errors [4, 29,30,31,32]. The pooled OR (n = 29 291 patients) across all studies was 0.27 (95% CI 0.15 to 0.49). However, the results of these studies are substantially heterogeneous (Fig. 2). The impact of the unit-based pharmacist implemented in the cohort study, which measured the total serious medication errors (SMEs) and SMEs/1000 patient-days, was significant for the SMEs/1000 patient-days from the intensive care unit (ICU) (P < 0.01). However, there was no significant difference for the total SMEs in the ICU and for the total SMEs and SMEs/1000 patient-days in the surgical and medical wards [19].
Discussion
This systematic review and meta-analysis investigated the impact of clinical pharmacist interventions on medication error rates in hospitalized pediatric patients. It provides a comprehensive overview and analysis of the most common types of errors that lead to pharmacist interventions and their significance grade (mild, moderate, severe) as well as the rate of acceptance of the pharmacists’ recommendations. Previous studies and reviews demonstrated the importance of clinical pharmacists with pediatric patients’ management. Benefits highlighted included: identifying drug related problems, recommending suitable medications, improve medication use and reduce medication related costs as well as reduce medication errors [36, 37]. Similar benefits were also observed with interventions targeted at adult population medication error prevention [10,11,12,13,14,15]. Such findings highlight that pharmacist’s involvement is essential to reduce medication errors regardless of the population involved.
Despite the heterogeneity of studies included in this meta-analysis the overall aggregate effect of pharmacist’s interventions demonstrated a significant beneficial outcome in reducing the odds of medication errors by 73%. Interventions that showed most benefit include correcting prescribing errors (dosing errors, units of measurement, route, and frequency) [29, 30]. Previous studies highlight that most medication errors occur during the prescribing process [36, 38]. Therefore, it is very important to include pharmacists in clinical ward rounds with prescribers. This gives the pharmacists the opportunity to prevent prescribing errors in the first place and therefore reduce the delays which happen when trying to correct these errors later.
The focus of this review was the hospital setting, since medication errors are more likely to occur within a tertiary healthcare setting compared to primary settings. Moreover, the role of pharmacists in preventing medication errors in hospital settings can have a far more benefit as compared to clinics and community settings due to the nature of complex patients received in hospitals as compared to other settings [39,40,41]. Nonetheless, it is important to investigate the role of pharmacists in preventing medication errors in other settings separately and highlight whether the same magnitude of benefit can be observed.
The main pharmacist intervention found in our study was educational sessions done by pharmacists to other healthcare providers, mainly nurses and physicians. In addition, reviewing or validating orders and implementing a unit-based clinical pharmacist were among the most common interventions in this systematic review. A previous systematic review that focused on ICU patients showed that the most common intervention was implementing a pharmacist within the medical team which is one of the top interventions in our study [10].
The main strength in this meta-analysis is that up to our knowledge this is the first review to numerically assess the impact of pharmacist interventions on medication error rates for pediatric patients in hospital settings. In addition, the systematic review included studies from different countries in various parts of the world which could enhance the generalizability of outcomes. The use of the CCAT offered further insight into the studies included in this analysis as the general quality of data between studies could be compared. The CCAT was selected in this analysis as it has been found to be more reliable than an informal appraisal of various research studies. The uniform manner of appraisal offered through the CCAT has been found to almost eliminate the rater effect with no substantial subject matter knowledge effect [42].
This study has some limitations that should be addressed. First, the overall quality of all components was 27.87 out of 40 which is considered moderate. This was mainly due to poor reporting of sampling and ethics approval as those two domains had the lowest overall ranking within the CCAT. Although sampling is essential to minimize the risk of selection bias, ethics disclosure does not introduce any particular type of bias to the study, thus do not affect the internal validity of the review. Moreover, the included studies were published in peer reviewed journals, a majority of which require ethical disclosure prior to publication. Second, some of the studies included a combination of pharmacist interventions, thus it cannot be guaranteed which intervention caused the reduction in medication errors. Significant heterogeneity in the studies included in the meta-analysis was identified which might be due to many reasons including, the variation in the implemented pharmacist interventions in addition to the method of detecting medication errors and the definition of medication discrepancy varied from one study to another. Moreover, some studies have reported results as medication errors and others as preventable ADRs. Lastly, this systematic review identified studies published between 1987 and 2018. With this wide range of dates, it is likely that clinical pharmacist practice and understanding of medication errors has changed over this time frame. As such, the outcomes from earlier conducted studies may report different outcomes compared to more recent studies due to practice changes and changes to the context of general healthcare.
Future studies should focus on evaluating the role of pharmacist interventions on medication errors in outpatient settings. This will allow for a better insight to the pharmacist impact in society and will enable the healthcare system to identify the areas or settings in which more attention and improvements are required. Furthermore, subgroup analysis of the outcomes of the current study might be required in order to examine the impact of a pharmacist on particular types of errors such as prescribing errors or administration errors; it will be beneficial to overcome this heterogeneity.
Conclusion
Medication errors remain to be of great concern especially when it comes to the pediatric population. Prescribing errors including inappropriate dosing and selecting inappropriate medications were the main medication errors reported within the included articles. Pharmacist interventions play an important role in reducing medication errors in the pediatric population. These interventions include educational sessions, review/validation of medication orders, and implementing a ward-based pharmacist or a medication safety program involving a pharmacist [20]. Overall, the findings from this review support the implementation of a clinical pharmacist in order to reduce the occurrence of medication errors in pediatric patients.
References
Campino A, Lopez-de-Heredia MC, Lopez-Heredia I, Valls ISA. Medication errors in a neonatal intensive care unit. Influence of observation on the error rate. Acta Paediatr. 2008;97(11):1591–4.
New England Quality Innovation Network-Quality Improvement Organization. Adverse drug events—What do we really mean? United States: Centers for Medicare & Medicaid Services. [cited 2020 Apr 7]. Available from: http://doh.hpc.go.th/data/HA2018/ADR_ADE.pdf.
Morimoto T, Gandhi TK, Seger AC, Hsieh TC, Bates DW. Adverse drug events and medication errors: detection and classification methods. Qual Saf Health Care. 2004;13(4):306–14.
Alagha HZ, Badary OA, Ibrahim HM, Sabri NA. Reducing prescribing errors in the paediatric intensive care unit: an experience from Egypt. Acta Paediatr. 2011;100(10):e169–74.
Costello JL, Torowicz DL, Yeh TS. Effects of a pharmacist-led pediatrics medication safety team on medication-error reporting. Am J Health-Syst Pharm. 2007;64(13):1422–6.
Poole RL, Carleton BC. Medication errors: neonates, infants and children are the most vulnerable. JPPT. 2008;13(2):65–7.
Doherty C, Mc Donnell C. Tenfold medication errors: 5 years’ experience at a university-affiliated pediatric hospital. Pediatrics. 2012;129(5):916–24.
Fortescue EB, Kaushal R, Landrigan CP, McKenna KJ, Clapp MD, Federico F, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003;111:722–9.
Fernández-Llamazares CM, Calleja-Hernandez MA, Manrique-Rodriguez S, Pérez-Sanz C, Duran-García E, Sanjurjo-Saez M. Impact of clinical pharmacist interventions in reducing paediatric prescribing errors. Arch Dis Child. 2012;97(6):564–8.
Wang T, Benedict N, Olsen KM, Luan R, Zhu X, Zhou N, et al. Effect of critical care pharmacist’s intervention on medication errors: a systematic review and meta-analysis of observational studies. J Crit Care. 2015;30(5):1101–6.
Manias E, Williams A, Liew D. Interventions to reduce medication errors in adult intensive care: a systematic review. Br J Clin Pharmacol. 2012;74(3):411–23.
Cohen V, Jellinek SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: a systematic review. Am J Health-Syst Pharm. 2009;66(15):1353–61.
Maidment ID, Lelliott P, Paton C. Medication errors in mental healthcare: a systematic review. Qual Saf Health Care. 2006;15(6):409–13.
Noormandi A, Karimzadeh I, Mirjalili M, Khalili H. Clinical and economic impacts of clinical pharmacists’ interventions in Iran: a systematic review. Daru. 2019;27(1):361–78.
Keers RN, Williams SD, Cooke J, Walsh T, Ashcroft DM. Impact of interventions designed to reduce medication administration errors in hospitals: a systematic review. Drug Saf. 2014;37(5):317–32.
Pawluk S, Hussain T, Naseralallah L. The effect of clinical pharmacist interventions on reducing medication errors in pediatric patients: a systematic review. PROSPERO 2019; CRD42019126541. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019126541.
M C. Crowe Critical Appraisal Tool (v1.4): Conchra; 2011 [cited 2020 Apr 7]. Available from: https://conchra.com.au/2015/12/08/crowe-critical-appraisal-tool-v1-4/.
Crowe M, Sheppard L. A general critical appraisal tool: an evaluation of construct validity. Int J Nurs Stud. 2011;48(12):1505–16.
Kaushal R, Bates DW, Abramson EL, Soukup JR, Goldmann DA. Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health-Syst Pharm. 2008;65(13):1254–60.
Abuelsoud NN. Improving medication safety through implementation of medication error reporting systems in different medical specialities. J Pharm Pract Res. 2018;48(6):537–42.
Christiansen SR, Morgan JA, Hilmas E, Shepardson A. Impact of a prescription review program on the accuracy and safety of discharge prescriptions in a pediatric hospital setting. JPPT. 2008;13(4):226–32.
Cunningham KJ. Analysis of clinical interventions and the impact of pediatric pharmacists on medication error prevention in a teaching hospital. JPPT. 2012;17(4):365–73.
Fernandez-Llamazares CM, Pozas M, Feal B, Cabanas MJ, Villaronga M, Hernandez-Gago Y, et al. Profile of prescribing errors detected by clinical pharmacists in paediatric hospitals in Spain. Int J Clin Pharm. 2013;35(4):638–46.
Folli HL, Poole RL, Benitz WE, Russo JC. Medication error prevention by clinical pharmacists in two children’s hospitals. Pediatrics. 1987;79(5):718–22.
Khan SN, Joseph S, Sasidharan P, Faap A. A study of clinical pharmacist initiated interventions for the optimal use of medications in a neonatal intensive care unit (NICU) of a tertiary care hospital in South India. Int J Pharm Sci. 2015;8:1.
Koren G, Reich A, Hales B. Use of clinical pharmacists to prevent medication errors in children. J Pharm Technol. 1991;7(6):219–21.
Maat B, Au YS, Bollen CW, van Vught AJ, Egberts TCG, Rademaker CMA. Clinical pharmacy interventions in paediatric electronic prescriptions. Arch Dis Child. 2013;98(3):222–7.
Prot-Labarthe S, Di Paolo ER, Lavoie A, Quennery S, Bussieres JF, Brion F, et al. Pediatric drug-related problems: a multicenter study in four French-speaking countries. Int J Clin Pharm. 2013;35(2):251–9.
Ahmed T, Haq N, Rehman M, Nasim A. The impact of pharmacist intervention on medication errors in a teaching hospital Quetta, Pakistan. Value Health. 2016;19(7):A630.
Campino A, Lopez-Herrera MC, Lopez-de-Heredia I, Valls-i-Soler A. Educational strategy to reduce medication errors in a neonatal intensive care unit. Acta Paediatr. 2009;98(5):782–5.
Chedoe I, Molendijk H, Hospes W, Van den Heuvel ER, Taxis K. The effect of a multifaceted educational intervention on medication preparation and administration errors in neonatal intensive care. Arch Dis Child Fetal Neonatal Ed. 2012;97(6):F449–55.
Chua S-S, Choo S-M, Sulaiman CZ, Omar A, Thong M-K. Effects of sharing information on drug administration errors in pediatric wards: a pre-post intervention study. Ther Clin Risk Manag. 2017;13:345–53.
Fawaz MG, Sabri NA, Albaghdady AA, Malek FAA. Detection and prevention of medication errors in the operating rooms of a pediatric surgery department in Egypt. Int J Pharm Sci Rev Res. 2017;42(2):100–6.
Okumura LM, da Silva DM, Comarella L. Relation between safe use of medicines and clinical pharmacy services at pediatric intensive care units. Rev Paul Pediatr. 2016;34:397–402.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63.
Drovandi A, Robertson K, Tucker M, Robinson N, Perks S, Kairuz T. A systematic review of clinical pharmacist interventions in paediatric hospital patients. Eur J Pediatr. 2018;177(8):1139–48.
Sanghera N, Chan P-Y, Khaki ZF, Planner C, Lee KKC, Cranswick NE, et al. Interventions of hospital pharmacists in improving drug therapy in children: a systematic literature review. Drug Saf. 2006;29(11):1031–47.
Ghaleb MA, Barber N, Franklin BD, Yeung VW, Khaki ZF, Wong IC. Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;40(10):1766–76.
Smith M, Giuliano MR, Starkowski MP. In Connecticut: improving patient medication management in primary care. Health Aff (Millwood). 2011;30(4):646–54.
Simpson SH. The roles we have as hospital pharmacists. Can J Hosp Pharm. 2017;70(1):3–4.
Mossialos E, Naci H, Courtin E. Expanding the role of community pharmacists: policymaking in the absence of policy-relevant evidence? Health Policy. 2013;111(2):135–48.
Crowe M, Sheppard L, Campbell A. Camparison of the effects of using the crowe critical appraisal tool versus informal appraisal in assessing health research: a randomised trial. Int J Evid Based Healthcare. 2011;9(4):444–9.
Acknowledgements
None
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naseralallah, L.M., Hussain, T.A., Jaam, M. et al. Impact of pharmacist interventions on medication errors in hospitalized pediatric patients: a systematic review and meta-analysis. Int J Clin Pharm 42, 979–994 (2020). https://doi.org/10.1007/s11096-020-01034-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01034-z