Abstract
Background Brazilians with type 2 diabetes require action to improve haemoglobin A1C levels considering the fact that approximately 73 % of them have poor glycaemic control. Evidence has shown the potential benefits of pharmaceutical care programs in type 2 diabetes patients. Objective To evaluate the effect of a pharmaceutical care program on blood glucose, blood pressure and lipid profile in hyperglycaemic patients undergoing drug treatment for type 2 diabetes. Setting Six primary care units of the Brazilian public health system, Ouro Preto, Brazil. Method An open, randomised, controlled clinical trial was conducted for 6 months. Subjects aged 18 years or older who were using oral antidiabetic medications and presenting haemoglobin A1C levels ≥7 % were randomly assigned to receive only usual health care or usual health care plus pharmaceutical intervention. Main outcome measure Haemoglobin A1C. Results A total of 129 subjects were enrolled, and 100 patients completed the study. Compared to the control group (n = 50), the intervention group (n = 50) showed a significant reduction of haemoglobin A1C (−0.6 vs 0.7 %, p = 0.001), fasting plasma glucose, total cholesterol, LDL cholesterol, triglycerides and systolic blood pressure and a significant increase in HDL cholesterol and the use of lipid-modifying agents and platelet aggregation inhibitors. Conclusions This study suggests that a pharmaceutical care program may provide important contributions to reduce haemoglobin A1C in type 2 diabetes patients. Moreover, the promotion of the rational use of drugs may be better achieved in a context of pharmaceutical care programs in Brazil.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Pharmaceutical care programs may contribute to the improvement of haemoglobin A1C and lipid profile in type 2 diabetes patients.
-
Pharmaceutical care programs developed for type 2 diabetes patients can have a positive impact on the quality of healthcare provided by the Brazilian public health system.
-
Pharmaceutical care programs can be an important strategy to identify and resolve drug therapy problems in primary care settings.
Introduction
Diabetes mellitus is a chronic metabolic disease that is presenting an increasing prevalence worldwide. In 2010, the worldwide prevalence of diabetes among individuals aged 20–79 years was estimated at 6.4 % [1]. In Brazil, the prevalence of diabetes in the population aged 30–79 is estimated at 7.6 % [2], of whom 90–95 % have type 2 diabetes [3]. In 2008, diabetes was the third leading cause of death in the Brazilian population [4]. Brazilians with type 2 diabetes require action to improve haemoglobin A1C levels considering the fact that approximately 73.0 % of them have poor glycaemic control [5].
The Brazilian public health system has an important role in the provision of health care for type 2 diabetes patients. Pharmacists are key elements in this process because of their potential to contribute to better results of drug therapy. In this context, pharmacists are expected to act in outpatient clinics, hospitals and community pharmacies to develop activities for the effectiveness and safety of drug use. In Brazil, the processes involving pharmacist practice are drug-centred, but this practice is undergoing a transition to a new patient-centred model following a discussion regarding pharmacist function that has emerged around the world [6].
Pharmaceutical care is a patient-centred model that consists of the responsible provision of drug therapy to achieve definite outcomes and to improve patient’s quality of life [7]. Some authors have noted that diabetes patients can benefit from pharmaceutical care programs and have a significant reduction of haemoglobin A1C levels [8–12]. Clinical trials evaluating pharmaceutical care programs for type 2 diabetes were conducted in Brazil. These studies demonstrated a significant reduction of haemoglobin A1C levels in patients assisted by the Brazilian public health system [13, 14]. Despite the potential benefits of pharmaceutical care in type 2 diabetes patients, some studies have limitations related to small sample size, nonrandomised design and lack of haemoglobin A1C evaluation [15]. Thus, studies on the impact of pharmaceutical care programs in primary care are relevant to evaluate the effect of this intervention on type 2 diabetes.
Aim of the study
This research was aimed at evaluating the effect of a pharmaceutical care program on blood glucose, blood pressure and lipid profile in hyperglycaemic patients undergoing drug treatment for type 2 diabetes in the Brazilian public health system.
Method
Study design and setting
The study was an open, randomised, controlled clinical trial with a 6-month patient follow-up conducted from April to September, 2010. The trial protocol was approved by the Research Ethical Committee, Federal University of Ouro Preto (CAAE 0037.0.238.000-029), and registered at clinicaltrials.gov (NCT01298726). The study settings were six primary health care units integrated into the Brazilian public health system in Ouro Preto, Brazil.
Sample size
The sample size was calculated to detect a minimum difference of 1.1 % in haemoglobin A1C levels between groups using Minitab® software, version 15, with a statistical power of 80 % and a significance level of 5 %. Based on published data, a standard deviation of 1.9 % was considered in the calculation [9], resulting in 48 subjects for each group. A target sample size with 30 % more participants in the control and intervention groups was selected to ensure sufficient statistical power and to account for ‘drop-outs’ during the study. This percentage was derived according to the amount of participant loss described in two studies conducted in Brazil [16, 17].
Recruitment and randomisation
The participants included in the study were aged 18 years or older, of both genders, with post-prandial capillary glucose ≥180 mg/dL, as determined by a point of care device, and haemoglobin A1C ≥7 %. The participants had a prescription from the public health system of one or more oral antidiabetic medications prescribed at least 6 months prior to the beginning of the study. Pregnant women, nursing mothers and people with impaired physical mobility were excluded. Recruitment was conducted between January and March 2010. Patients were identified from a list provided by the primary care service. They were invited to participate in the study when the antidiabetic medications were dispensed by the pharmacy or during home visits performed by the health care team.
Patients were included if they fulfilled inclusion criteria, and they were subsequently randomly assigned to the intervention or control group using a list of random numbers generated by Minitab® software, version 15. Randomisation was stratified by each primary health care unit.
Data collection
Sociodemographic data, the duration of diabetes and lifestyle information were initially collected during interviews that occurred at the beginning and end of the study. The variables considered were age, gender, educational level and smoking habits. Information about weight and height was collected to calculate the body mass index (BMI). The drug list was investigated by prescription review and patient self-report. Prescribed and non-prescribed drugs were included, and the number of medications taken was calculated. The drugs were classified according to the anatomical therapeutic chemical (ATC) classification system [18]. The blood pressure was measured by an indirect method and oscillometric technique with a validated digital sphygmomanometer (Omron® HEM 742). Biochemical data included haemoglobin A1C, fasting plasma glucose, total cholesterol, HDL cholesterol, LDL cholesterol and triglycerides. The haemoglobin A1C level was determined by high-performance liquid chromatography. LDL cholesterol was not estimated if the triglycerides value was >400 mg/dL [19]. Blood pressure and biochemical data were determined in the first and last month of the study. The reference values for blood pressure and biochemical data were recommended by the American Diabetes Association (ADA) [20].
Control group
The participants in the control group received usual health care characterised by appointments with doctors, nurses, nutritionists or physiotherapists, without the participation of the research pharmacists. Pharmacy students from the Universidade Federal de Ouro Preto were involved in data collection. They were previously trained by the research pharmacists to obtain homogeneity among interviewers.
Intervention group
Two research pharmacists performed the intervention program based on the philosophical principles proposed by Cipolle et al. [21]. The researchers had 4 years of experience in community pharmacy, and they were trained in pharmaceutical care and diabetes management. The pharmaceutical care practice was developed with individual appointments scheduled once a month for 6 months. All of the procedures were standardised and documented. The patient’s needs were assessed, and drug therapy problems were identified based on the Pharmacotherapy Workup [21]. A care plan was designed for each patient focusing on actions to meet therapeutic goals, which included patient education and/or pharmacotherapy changes. Proposals for pharmacotherapy change were forwarded to physicians by letters for evaluation. Pharmacotherapy changes included drug introduction, replacement or withdrawal and dose increase or dose reduction, when necessary, aimed at improving effectiveness and safety.
Patient education consisted of verbal instructions about non-pharmacological issues and pharmacological treatments. Information about aetiology, pathophysiology, complications, treatment goals and the need of changes in diet and physical exercise was given to patients using a vocabulary suitable for the patients’ literacy level. Specific information about correct drug use was also provided.
The studied patients were educated on diabetes regarding risk factors for complications and the management of signs and symptoms. In respect to the use of antidiabetic medications, information about proper dosage, side-effects and drug storage was reinforced. Behavioural modification aspects were emphasised and included advice on self-monitoring glycaemic control, physical activity, diet and medication adherence.
Outcomes
The primary outcome was the serum level of haemoglobin A1C. A comparison among groups was also performed to investigate the impact of the intervention on other variables, such as fasting plasma glucose, total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides, systolic and diastolic blood pressure and the number of medications taken.
Statistical analysis
Data were registered by double entry using the Excel® program, version 2007. All of the data were analysed with the IBM Statistical Package for Social Sciences (SPSS) software, version 18.0. Descriptive statistical methods were used to compare control and intervention groups. The Kolmogorov–Smirnov test evaluated the normality of the variables. The Pearson’s Chi-squared test or Fisher’s exact test were used to compare categorical variables. Quantitative variables were assessed using Student’s t test or the Mann–Whitney U test when indicated. A multiple linear regression analysis was used to determine the variables that could explain the variation in blood glucose, assuming haemoglobin A1C as the dependent variable and the quantitative and categorical variables with p < 0.20 in the univariate analysis as independent variables. To estimate the regression coefficients, the method of a generalised estimating equation was used with a compound symmetry structure for the covariance matrix due to the dependence data structure.
Results
Participants
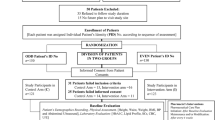
A total of 129 subjects were enrolled in the study. Among them, 50 out of 65 subjects in the intervention group and 50 out of 64 subjects in the control group completed the study. Figure 1 depicts the patient flowchart. The participants who did not complete the study had similar characteristics as those who completed the study in relation to age, sex, education level and haemoglobin A1C levels. The percentage of patients who dropped out of the study was similar between control and intervention groups (p = 0.552). Sociodemographic data, smoking status, length of diabetes, blood pressure and biochemical data are presented in Table 1. Both groups exhibited similar characteristics (p > 0.05), except for systolic blood pressure.
Outcomes
Comparing the intervention group with the control group at the end of the trial, there was a significant improvement in the biochemical data and systolic blood pressure. No significant difference in BMI or diastolic blood pressure was found (Table 1).
The predictors of changes in haemoglobin A1C were the level of fasting plasma glucose and the allocation of participants to the intervention group only. The regression model results showed the following: (1) at baseline, the participants of the intervention group had average haemoglobin A1C levels 3.5 % higher than the control group; (2) after 6 months, the intervention group had average haemoglobin A1C levels 4.0 % lower than the control group; (3) an increase of 10 mg/dL in fasting plasma glucose resulted in an average increase of 2.0 % in the haemoglobin A1C level (Table 2).
Impact on drug use
All medications used by both groups are detailed in Table 3. Approximately 80 % of the patients’ drug list included antihypertensive agents, antidiabetic drugs, lipid-modifying agents or platelet aggregation inhibitors. The average number of drugs taken by the control group remained the same throughout the trial (5.2 vs 5.2), whereas the intervention group showed an increase from 5.7 to 6.9 (p < 0.001) medications per participant. The specific drug classes whose use was significantly increased in the intervention group included lipid-modifying agents and platelet aggregation inhibitors. No significant difference was found in the average number of antihypertensive and antidiabetic drugs used by both groups at the end of the study.
Drug therapy problems
The average number of drug therapy problems in the intervention group at baseline was 6.7. Drug therapy problems included 3.8 % of needs for additional drug therapy, 21.2 % of unnecessary drug therapy, 30.8 % of ineffective drug, 22.7 % of dosage too low, 6.5 % of adverse drug reactions, 1.2 % of dosage too high and 13.8 % of noncompliance. The average number of drug therapy problems at the end of the study was significantly reduced to 5.0 (p < 0.001). Drug therapy problems at the end of the study were 9.2 % of needs additional drug therapy, 7.7 % of unnecessary drug therapy, 45.6 % of ineffective drug, 21.8 % of dosage too low, 1.2 % of adverse drug reactions, 2.8 % of dosage too high and 11.7 % of noncompliance.
Discussion
In the current study, a pharmaceutical care program showed favourable results in the control of type 2 diabetes, as determined by a significant decrease in the average level of haemoglobin A1C. The intervention also led to the improvement of other parameters, such as fasting plasma glucose, lipid profile and systolic blood pressure. Our study contributed to the identification of needs for additional drug therapy, which resulted in an increase in the use of prescribed drugs, such as simvastatin and acetylsalicylic acid. These positive results were obtained through the provision of a patient-centred approach and education strategies in the intervention group.
Other studies have been carried out in different settings to evaluate pharmaceutical care programs focused on type 2 diabetes. These studies found a reduction in haemoglobin A1C ranging from 0.5 to 1.0 % [9–11, 13]. A study performed by Stratton et al. [22] demonstrated that each reduction of 1 % in haemoglobin A1C is associated with a decrease of 21 % in the risk of death related to diabetes, 14 % in the risk of myocardial infarction and 37 % in the risk of microvascular complications. Our findings show that a pharmaceutical care program in primary care may provide contributions to the control of glycaemic levels and the prevention of clinical complications.
The intervention group showed improved lipid profiles compared with the control group. These results are in line with previous studies [9, 11, 23]. Fornos et al. [9] found a significant reduction only for total cholesterol and LDL cholesterol levels, without significant changes in triglycerides and HDL cholesterol levels. In contrast, Clifford et al. [11] did not find a significant change in the total cholesterol, HDL cholesterol or triglycerides. Regarding blood pressure, we found a significant reduction in systolic blood pressure. Other studies revealed heterogeneity in the impact of pharmaceutical care programs on blood pressure [9, 10, 15–17, 23]. The interpretation of our results related to the secondary outcomes should take into account that the study sample size and the statistical power may not be sufficient to assess these variables. Further studies would be useful to evaluate the contributions of pharmaceutical care programs to predict the long-term risk of cardiovascular events.
Although biochemical data and systolic blood pressure showed better results in the intervention group than the control group, the magnitude of this improvement was not sufficient to attain the values recommended by the ADA [20]. These results may be explained by the 6-month period of study, which may not have been enough to promote the achievement of therapeutic goals. Additional factors possibly involved in the impact of intervention should be addressed: no prompt access to medical appointments, drug shortages, heterogeneity in clinical procedures, medication non-adherence and the lack of integration between pharmacists and physicians.
Pharmaceutical care should be developed from the perspective of integrated actions in health care [24]. In that sense, it is essential that this practice occurs within an organisation that promotes multidisciplinary teamwork characterised by a mutual relationship involving interactions among different healthcare professionals [25]. Cooperative and coordinated work is fundamental for the resolution of problems in health care. Thus, there is an urgent need to foster teamwork in primary health care units, aiming to harmonise procedures and provide suitable interventions that benefit patients under complex drug therapy.
The main cause of death in patients with type 2 diabetes is cardiovascular diseases. As the prevalence of type 2 diabetes continues to increase rapidly, the optimal control of cardiovascular risk factors should be considered as a priority. There is evidence that the use of lipid-lowering medication and platelet aggregation inhibitors contributes to the control of some of these risk factors. The increase in the use of these drugs in the intervention group may prevent patients from undergoing cardiovascular events. In contrast, the maintenance of the average number of drugs taken by the patients in the control group might reflect the behaviour of some physicians not initiating or intensifying pharmacotherapy when necessary, which is referred to in the literature as clinical inertia [26–28].
The favourable results in this study can be attributed to not only changes in pharmacotherapy but also the provision of proper education on pharmacological and non-pharmacological treatments. However, additional efforts should be made to resolve the remaining drug therapy problems of the patients in the intervention group.
The strengths of our study are the design of a randomised controlled trial to evaluate the performance of a pharmaceutical care program to improve clinical results in patients with type 2 diabetes and the measurement of diverse surrogate outcomes in the primary health care system of a developing country. We also described the impact of this program on the reduction of drug-related problems, the identification of needs for additional therapy and the introduction of new medications.
There are some limitations to be mentioned. First, we examined surrogate outcomes instead of endpoint outcomes. Investigations specially designed to study the role of a pharmaceutical care program on endpoint outcomes would better explain the real impact of this intervention on type 2 diabetes patient care. Second, in respect to participant loss, the small sample size may explain the non-significant difference between groups and such difference could not be trivial in large randomised clinical trials. Third, the study was relatively short to allow the inference that the improvement of biochemical levels and blood pressure would be intensified or maintained longer. Additionally, as the control group participants had access to laboratory results at baseline, they may have improved self-care and sought medical attention, which could minimise the effect of the intervention provided in this study. Regarding data collection, it cannot be assumed that there was strong and significant concordance between pharmacists and pharmacy students in the measurements. Finally, our observations could not be generalised to the Brazilian public health system as a whole because the number of pharmacists who perform pharmaceutical care is still small, and these professionals are not specifically qualified for patient follow-up.
Conclusion
In conclusion, this study suggests that a pharmaceutical care program may provide important contributions to reduce haemoglobin A1C levels in type 2 diabetes patients. Moreover, the promotion of the rational use of drugs may be better achieved in the context of pharmaceutical care programs. Patient-centred actions in primary care could be an important strategy to improve the quality of healthcare provided by the Brazilian public health system.
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14.
Malerbi DA, Franco LJ. Multicenter study of the prevalence of diabetes mellitus and impaired glucose tolerance in the urban Brazilian population aged 30–69 years. The Brazilian Cooperative Group on the Study of Diabetes Prevalence. Diabetes Care. 1992;15:1509–16.
Sociedade Brasileira de Diabetes (SBD). Diretrizes da Sociedade Brasileira de Diabetes. [cited 2012 18 Jul]; Available from: http://www.diabetes.org.br/attachments/diretrizes09_final.pdf.
Brasil. Saúde Brasil 2009: uma análise da situação de saúde e da agenda nacional e internacional de prioridades em saúde. [cited 2012 18 Jul]; Available from: http://portal.saude.gov.br/portal/arquivos/pdf/29_11_10_saude_brasil_web.pdf.
Mendes ABV, Fittipaldi JAS, Neves RCS, Chacra AR, Moreira ED. Prevalence and correlates of inadequate glycaemic control: results from a nationwide survey in 6,671 adults with diabetes in Brazil. Acta Diabetol. 2010;47:137–45.
World Health Organization. The role of the pharmacist in the health care system. Vancouver, Canada; 1997. [cited 2012 18 Jul]; Available from: www.opas.org.br/medicamentos/site/UploadArq/who-pharm-97-599.pdf.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–43.
Turnacilar M, Sancar M, Apikoglu-Rabus S, Hursitoglu M, Izzettin FV. Improvement of diabetes indices of care by a short pharmaceutical care program. Pharm World Sci. 2009;31:689–95.
Fornos AJ, Andrés NF, Andrés JC, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006;28:65–72.
Krass I, Armour CL, Mitchell B, Brillant M, Dienaar R, Hughes J, et al. The pharmacy diabetes care program: assessment of a community pharmacy diabetes service model in Australia. Diabet Med. 2007;24:677–83.
Clifford RM, Davis WA, Batty KT, Davis TM. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2005;28:771–6.
Correr CJ, Melchiors AC, Fernandes-Llimós F, Pontarolo R. Effects of a pharmacotherapy follow-up in community pharmacies on type 2 diabetes patients in Brazil. Int J Clin Pharm. 2011;33:273–80.
Neto PRO, Marusic S, Lyra-Júnior DP, Pilger D, Cruciol-Souza JM, Gaeti WP, et al. Effect of a 36-month pharmaceutical care program on coronary heart disease risk in elderly diabetic and hypertensive patients. J Pharm Pharmaceut Sci. 2011;14:249–63.
Borges AP, Guidoni CM, Ferreira LD, de Freitas O, Pereira LR. The pharmaceutical care of patients with type 2 diabetes mellitus. Pharm World Sci. 2010;32:730–6.
Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67:547–57.
Correr CJ, Pontarolo R, Wiens A, Rossignoli P, Melchiors AC, Radominski R, et al. Economic evaluation of pharmacotherapeutic follow-up in type 2 diabetes mellitus patients in community pharmacies. Arq Bras Endocrinol Metab. 2009;53:825–33.
Cid AS. Avaliação da efetividade da atenção farmacêutica no controle da hipertensão arterial. Dissertação (Mestrado em Ciências Farmacêuticas). Universidade Federal de Ouro Preto, Ouro Preto; 2008.
World Health Organization. ATC/DDD Index 2010. [cited 2012 18 Jul]; Available from: http://www.whocc.no/atc_ddd_index/.
Friedewald WT, Levi RI, Fredrickson DS. Estimation of the concentration of low density lipoproteins cholesterol in plasma without use of the ultracentrifuge. Clin Chem. 1972;18:499–502.
American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(Suppl. 1):S11–61.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the clinician’s guide. 2nd ed. New York: McGraw-Hill; 2004.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–12.
Fera T, Bluml BM, Ellis WM. Diabetes ten city challenge: final economic and clinical results. J Am Pharm Assoc. 2009;49(3):383–91.
Ivama AM, Noblat L, De Castro MS, De Oliveira NVBV, Jaramillo NM, Rech N. Consenso Brasileiro de atenção farmacêutica. Brasília: PAHO/WHO; 2002.
Peduzzi M. Multiprofessional healthcare team: concept and typology. Rev Saúde Pública. 2001;35:103–9.
Grant RW, Buse JB, Meigs JB. Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change. Diabetes Care. 2005;28:337–42.
Zafar A, Davies M, Azhar A, Khunti K. Clinical inertia in management of T2DM. Prim Care Diabetes. 2010;4:203–7.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Acknowledgments
The authors would like to thank the teachers and students of Education Program for Health Work and the pharmacists who contributed to this research.
Funding
The study was supported by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) and Universidade Federal de Ouro Preto.
Conflicts of interest
The authors have no conflict of interest with regard to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mourão, A.O.M., Ferreira, W.R., Martins, M.A.P. et al. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharm 35, 79–86 (2013). https://doi.org/10.1007/s11096-012-9710-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9710-7