Abstract
Objective To evaluate the efficiency of pharmaceutical care on the control of clinical parameters, such as fasting glycaemia and glycosylated haemoglobin in patients with Type 2 Diabetes mellitus. Setting This study was conducted at the Training and Community Health Centre of the College of Medicine of Ribeirao Preto, University of Sao Paulo, Brazil. Methods A prospective and experimental study was conducted with 71 participants divided in two groups: (i) pharmaceutical care group (n=40), and (ii) the control group (n=31). The distribution of patients within these groups was made casually, and the patients were monitored for 12 months. Main outcome measure: Values for fasting glycaemia and glycosylated haemoglobin were collected. Results Mean values of fasting glycaemia in the pharmaceutical care group were significantly reduced whilst a small reduction was detected in the control group at the same time. A significant reduction in the levels of glycosylated haemoglobin was detected in patients in the pharmaceutical care group, and an average increase was observed in the control group. Furthermore, the follow-up of the intervention group by a pharmacist contributed to the resolution of 62.7% of 142 drug therapy problems identified. Conclusion In Brazil, the information provided by a pharmacist to patients with Type 2 Diabetes mellitus increases compliance to treatment, solving or reducing the Drug Therapy Problem and, consequently, improving glycaemic control.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact of findings on practice
-
The frequent contacts with health professionals through pharmaceutical care regimens shows significant improvements in therapeutic practice such as reduced levels of fasting glycaemia and glycosylated haemoglobin in Type 2 Diabetes mellitus patients.
-
Information and care provided by pharmacists to patients with Diabetes mellitus Type 2 in Brazil improves compliance to treatment, and reduces the level of glycosylated haemoglobin.
Introduction
The prevalence of Diabetes mellitus in 2010 is estimated to reach 285 million individuals, 6.6% of the adult world population, and projections indicate that by 2030 the number will have increased to 438 million (7.8%), of which 90–95% will suffer from of Type 2 Diabetes mellitus (DM2)[1]. DM2 is a chronic and degenerative metabolic disorder characterised by alterations in the production and secretion of insulin or a defect in tissue sensitivity to the hormone or both [2].
Treatment of the disease involves changes in lifestyle, and if these changes do not lead to acceptable glycaemic control, disease care must be completed with the administration of oral antidiabetic drugs or insulin or both. According to the American Diabetes Association, care of the disease is related to patient education and primary attention received, meaning that an interdisciplinary health strategy may stimulate an active role in patient self-care process and promote DM2 control [3].
The pharmacist, as part of the healthcare team, must be in charge of Pharmaceutical Care (PC) which is defined by Hepler and Strand (1990) as “the responsible provision of drug therapy for the purpose of achieving the finite outcomes that improve a patient’s quality of life”[4]. In addition, by optimising pharmacotherapy, the professional pharmacist contributes, in collaboration with the members of the healthcare team, to the clinical improvement of the patient as well as to his or her quality of life [4, 5].
However, in developing countries such as Brazil, Mexico, Chile and Argentina, among others, published articles that address issues related to PC are scarce. It is therefore important to evaluate the role of the pharmacist in these countries in the context of the healthcare team and its final objective, namely the improvement of patient care [6]. In Brazil, the pharmacist works mainly in administration services, which includes activities related to the acquisition and inventory control of drugs. In addition, the practice of PC is not frequent in the public health system, and the pharmacist is involved in most cases only as a dispenser of drugs without providing guidance or pharmacotherapeutic follow-up.
The aim of this study was to evaluate the clinical impact of PC on patients with DM2, mainly considering the control of parameters such as fasting glycaemia and levels of glycosylated haemoglobin (HbA1c). Parallel to the pharmacotherapeutic follow-up, an intervention plan was developed to optimise drug use and adherence to the treatment to achieve DM2 control.
Methods
Place of study
The Brazilian Public Health System provides free access to complete healthcare to all inhabitants in three levels of complexity: primary, secondary and tertiary. As a primary care, the population receives basic health services such as promotion of health education, prevention and surveys of disease spread. Professionals who provide this service include family physicians and nurses.
Diagnosis and treatment of many diseases are provided at the secondary care level by specially qualified physicians. In addition, other health professionals such as pharmacists, nurses, and nutritionists participate in the secondary level care. The two levels of care described above are offered to outpatients.
The tertiary care refers to diagnostic procedures and more complex treatments provided in the hospital to patients referred by professionals from the two first-levels, who require hospitalisation for a certain period, or else to emergency cases like accidents or sudden health problems.
This study was conducted between March 2006 and February 2007, at the Training and Community Health Centre of the College of Medicine of Ribeirao Preto, University of Sao Paulo, which is part of secondary care health centres provided nationwide by the Brazilian Public Health System. The research project was approved by the Committee on Ethics in Research of this Training and Community Health Centre according to the protocol number 0172/2006.
Inclusion Criteria
The patients referred to the PC service by physicians were the users of the Brazilian Public Health System and periodically attended at the Endocrinology Service of the Health Unit. They were 18-years-old or older and free of hepatotrophical viral diseases or human immunodeficiency virus—acquired immunodeficiency syndrome. All participants in the study signed the Terms of Informed Consent.
Study development
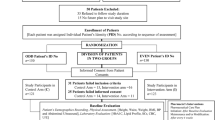
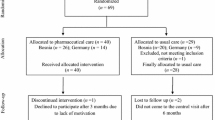
A prospective and experimental study was conducted with the patients regularly seen at the Endocrinology Unit (Standard Care), which identified patients who had difficulties in glycaemic control through biochemistry exams or those who did not take drugs as prescribed through self-report. The patients referred to the PC service (n = 71) were divided in two groups, the PC group (n = 40) in which participants received standard care and PC, and the control group (n = 31) who only received standard care. The distribution of patients in these groups was made casually. The groups had distinct numbers of patients, the PC group being larger than the control because according to the literature, the dropout rate could be as high as 40.0% in groups of patients followed by pharmacists [7, 8].
Results in the PC group were only considered for patients present at the monthly meetings at least seven times during the 12-month study. This number was considered as the minimum necessary to establish a good relationship between the pharmacist and patient. Strand et al. reported positive results in the identification and resolution of Drug Therapy Problems (DTP) in only four pharmaceutical consultations [9].
In the PC group, seven patients were excluded because one patient died, one moved to another city, two patients had changed Diabetes mellitus diagnostic status and three were enrolled in another health unit. The number of patients in the control group remained the same. They were only followed by their medical records, did not have to attend meetings at the PC service, and only had to keep their medical appointments.
The remaining 33 patients in the PC group and the 31 patients in the control group were asked by the endocrinologists of the Training and Community Health Centre to have clinical exams for fasting glycaemia and HbA1c every 4 months. In both groups, socio-demographical data collection (gender, age, schooling, marital status, family income, etc.), clinical evaluation (clinical diagnostic, length of DM2 pharmacological treatment, length of DM2 diagnosis, etc.), laboratory outcomes (fasting glycaemia and HbA1c) and the drug therapy prescribed were extracted from medical records by a clinical pharmacist. There was no contact between the clinical pharmacist and the participants of the control group.
The patients in the PC group had standard care and were followed up monthly by a single clinical pharmacist, who performed the data collection and the monitoring of these patients based on the Pharmacist’s Workup of Drug Therapy [9], which is a method of pharmaceutical care developed at the University of Minnesota, United States, by researchers Linda Strand and Charles Hepler.
Pharmaceutical records contained data on admission (social, demographical, economical and clinical data), follow-up (laboratory data and compliance test) and each patient’s intervention plan (an analysis of the situation of the patient and according to his/her problems and necessities, the establishment of a plan to solve them). Patient education was conducted individually according to his/her needs and knowledge of DM2 and its treatment [9]. It included questions about the drugs prescribed (name, indication, dosage and possible adverse events), and DM2 (complications and comorbidities), and all data supplied were registered in the pharmaceutical record.
In addition, the pharmacist performed verbal and written orientations related to the control of the disease, compliance to therapeutic treatment, appropriate nutrition and correct use of drugs including the method of insulin application. The pharmacist also worked in association with other health professionals, and additional interventions were performed, such as adjustment of drug dose, modification of the drug therapy (addition or withdrawal), and modification of diet plan and care of the diabetic foot. The patients were also referred to specialists (ophthalmologists, cardiologists and others) when there was need for these procedures. The pharmacist in charge was then able to analyse the patient’s condition and plan the PC with clear and defined aims to obtain satisfactory clinical results, besides identifying or preventing DTP or both. Laboratory determinations of fasting glycaemia and HbA1c helped evaluate clinical conditions of patients during consultations.
At the same time, controls received only standard care provided by the endocrinology unit, consisting of appointments every 4 months, whose procedures were registered in the patient records and could consist of alterations in the prescribed drugs, requests for laboratory exams, general information about patient health and referrals to specialists.
Compliance
Compliance to the therapeutic regimens was verified by the Morisky–Green test that consists of the following questions:
-
(1)
Do you ever forget to take your medicine?
-
(2)
Are you careless at times about taking your medicine?
-
(3)
When you feel better, do you sometimes stop taking your medicine?
-
(4)
Sometimes if you feel worse when you take the medicine, do you stop taking it?
According to the protocol of the Morisky-Green test, patients are considered adherent to the treatment when they get a maximum score of four points, and non-adherent when they get three points or less [10].
Drug Therapy Problem
DTP were classified according to the Pharmacist’s Workup of Drug Therapy [9]. This model may be applied to all individuals, independent of the number of pathological diagnoses, and can be used besides treating noncompliance to pharmacological treatments such as DTP.
Cardiovascular risk
At the consultation, the patient was also evaluated for cardiovascular risks by applying the Framingham Cardiac Risk Score, which deals with the following variables: age, gender, total cholesterol level, high density lipoprotein cholesterol, blood arterial pressure, diabetes status and smoking. The variables described above are stratified into categories that receive absolute numerical values. The sum of these values defines a patient’s cardiovascular risk as the probability of occurrence of cardiovascular events in the next 10 years as a percentage. Criteria defined by the Framingham Cardiac Risk Score were applied to determine patient risk as well as the odds for cardiovascular events [11].
Statistical analysis
The results were assessed using continuous variables represented as the mean ± standard deviation and the Student’s t-test was used for independent and paired data analysis. Statistical significance was set at P < 0.05. Analyses were performed using the Software GraphPad Instat® and Statgraphics®.
Results
The population of this study consists of poorly educated individuals, with low family income and inconsistent health care. The most significant difference between the groups was the number of careers that are necessary to help manage DM2 in the control group. In general, both control and pharmaceutical care groups were similar regarding demographical data (Table 1).
The clinical values of fasting glycaemia and HbA1c, and the Framingham Cardiac Risk Scores for both groups of patients were obtained. The PC group had significantly lower levels of fasting glycaemia and HbA1c at the completion of the study. However, there was no significant difference in the decreases of Framingham Cardiac Risk Scores in both groups (Table 2).
Compliance to the therapeutic regimen was verified during the study. After 12 pharmaceutical consultations, the average scores obtained from the Morisky–Green test in the PC group was higher when compared to the score measured at start of the study (Fig. 1). This result indicates an increase in compliance to the pharmacological treatment during the course of the study.
For patients in the PC group, DTP was identified and resolved during the study period, with the lack of compliance to the pharmacological treatment being the most prevalent issue. In addition, modifications to the therapeutic plans of the PC group such as dosage adjustments or addition or withdrawal of prescribed drugs were suggested by the pharmacist when necessary (Table 3). Seventy-three percent of the suggestions made were accepted by the physician.
Discussion
Approximately 33.0% of patients with diabetes in the United States receive health education [12, 13]. In the majority of the developing countries, however, this practice is less frequent. In this context, the pharmacist, in association with other health professionals, has plenty to contribute to improve the care supplied to patients with diabetes [14], mainly by addressing issues relevant to PC.
In this study, the mean fasting glycaemia values were significantly reduced in the PC group when comparing levels at the start and finish of the study, whilst only a small reduction was detected in the control group at the same time (Table 2). Similar studies reported a reduction of 9.1% (14.4 mg/dl) and 66.0 mg/dl in the fasting glycaemia levels of diabetic patients assisted by a programme of pharmaceutical care [15, 16]. The result in the PC group of this study had clinical relevance because the final fasting glycaemia values were close to the ones recommended by the American Diabetes Association for Diabetes mellitus patients, which are 90.0–130.0 mg/dl3. In addition, lower standard deviations at the completion of the study demonstrated that patients in the PC group had a smaller number of hypoglycaemia and hyperglycaemia episodes, that is, a smaller variation in fasting glycaemia levels, thus optimising control of DM2. However, the change in the outcome measurements for fasting glycaemia calculated for each patient (final value minus initial value) and the mean difference between the groups was not statistically significant.
The recommended values for HbA1c by the American Diabetes Association are lower than 7.0% [3]. At the start of the study, both the PC and the control groups had values of HbA1c higher than 7.0%, demonstrating the inadequate control of blood glucose levels. In this study, after 12 months, there was a statistically significant reduction in HbA1c values in the PC group, whereas in the control group, there was a slight increase (Table 2). In addition, the change in the outcome measurements for HbA1c was calculated for each patient (final value minus initial value), and the mean difference between the groups was statistically significant (Table 2). Thus, the PC contributed effectively to glycaemic control. The clinically relevant reduced HbA1c values were much closer to the recommended ones of the American Diabetes Association, and confirmed decreases of 0.9%, 1.4% and 0.7% points as reported by other authors [17–19]. Other studies showed values with higher reductions such as 2.2% and 1.9% points [11, 20]. Some other studies considered that pharmaceutical services did not result in an appreciable reduction in HbA1c levels [21, 22].
According to the United Kingdom Prospective Diabetes Study, for each 1.0% point reduction in HbA1c levels, diabetic individuals have a 35.0% lower risk of microvascular complications, as determined in a follow-up period of 8.4 years [23]. The reduced follow-up period in the present study prohibited any conclusions pertaining to microvascular complications in the subjects studied.
Compliance with pharmacological treatment leads to adequate glycaemic control [3, 24], which retards or prevents complications or comorbidities or both associated with DM2 [3]. Through the Morisky–Green test, an appreciable increase in compliance was observed in the PC group (Fig. 1). However, according to Carvalho et al., 100% compliance is very hard to attain because the everyday lives of patients are directly affected by the proposed treatments. The same authors conclude that risk factors leading to reduced compliance with pharmacological treatment are emotional interference, education, family income, and unfavourable job conditions [25]. Previous studies have considered that complex therapeutic plans and difficulty in understanding medical prescriptions probably are contributing factors in the reduced compliance to pharmacological treatment in DM2[26, 27]. Taken together, all of these factors may characterise the profiles of patients in this study, but the results showed that health education, orientation, and systematic and adequate follow-up of the therapeutic regimen during PC increased compliance, thus facilitating attainment of the expected clinical results.
Reports from the World Health Organization indicate that in developed countries, more than half of the individuals do not correctly use drugs and that this number is even higher in developing countries [28]. During this study, 142 DTP were identified. Noncompliance with treatment was the most prevalent, followed by adverse drug reactions and the need for additional drug therapy (Table 3).
Of the noncompliance problems, 63.6% were resolved. Strand et al. were able to resolve 88.0% of their DTP cases whilst Rao et al. were successful in 81.0% of cases identified [9, 29]. The total number of problems resolved in this study (62.7%) was lower than those reported by others, but it produced a significant improvement in the clinical results of the PC group. The identification of DTP is an important tool of PC, and solving the DTP improves the control of DM2.
The risk for cardiovascular events is four times higher in DM2 patients compared to the general population. About half of deaths in DM2 patients are related to cardiovascular complications [30]. In the present study, cardiovascular risk was evaluated by the Framingham Cardiac Risk Score, and there was no significant difference in the decrease of risk in both groups (Table 2). However, results in the PC group were more outstanding especially if it is considered that the average age in the control group was 5 years lower. Furthermore, the results were even better when compared to Oliveira et al. who dealt with a population ten years younger with a similar DM2 diagnostic statistics. It should be considered that age is a risk factor in the Framingham Cardiac Risk Score [31].
The findings of this study demonstrate that structured pharmaceutical services emphasising therapeutic monitoring solve DTP, promote health education and if inserted in a healthcare team, can promote significant results in the management of DM2.
The limitations of this study are related to the population sample size, which is considered small when compared to others studies [17, 18]. In addition, patient selection was not random, and the nature of the intervention did not permit blinding of the pharmacist. In addition, the short duration of the study prevents incidence evaluation of micro- and macrovascular complications, an important factor to be considered.
Conclusion
The management of DM2 patients involves comprehensive clinical control including several factors, starting from changes in lifestyle and including correct pharmacological therapy. In this study, frequent contact with a pharmacist through PC services increased compliance to therapy due to adjustments of drugs' dosages, prevented or resolved DTP and, consequently, improved the glycaemic control in patients with DM2. In addition, these findings contribute to the growing information in the literature that supports the development of clinical interventions and health policies in developing countries, stimulating the academic training of clinical pharmacists who are competent to act in healthcare teams.
References
International Diabetes Federation. Diabetes Atlas. 4th ed. Brussels: International Diabetes Federation; 2009. 100p. (ISBN - 13: 978-2-930229-71-3). Available: http://www.diabetesatlas.org/content/diabetes.
World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. Geneva: World Health Organization; 2006. 52p. (ISBN - 92-4-159493-4). Available: http://www.idf.org/webdata/docs/WHO_IDF_definition_diagnosis_of_diabetes.pdf.
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2009;32(1):S13–61.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43.
Hasegawa GR. Enhancing patients’ understanding of drug therapy. Am J Health Syst Pharm. 2004;61(23):2503.
Pereira LRL, Freitas O. The evolution of pharmaceutical care and the prospect for the Brazil. Braz J Pharm Sci. 2008;44(4):601–12.
Castro MS, Chemello C, Pilger D, Junges F, Bohnen L, Zimmerman LM, et al. Pharmaceutical care in the management of patients with hypertension. Braz J Hypertens. 2006;13(3):198–202.
Lyra-Júnior DP, Kheir N, Abriata JP, Rocha CE, Santos CB, Pelá IR. Impact of pharmaceutical care interventions in the identification and resolution of drug-related problems and on quality of life in a group of elderly outpatients in Ribeirão Preto (SP), Brazil. Ther Clin Risk Manag. 2007;3(6):989–98.
Strand LM, Cipolle RJ, Morley PC, Frakes MJ. The impact of pharmaceutical care practice on the practitioner and the patient in the ambulatory practice setting: twenty-five years of experience. Curr Pharm Des. 2004;10(31):3987–4001.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of self-reported measure of medication adherence. Med Care. 1986;24(1):67–74.
D’agostinho RB, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: result of a multiple ethnic groups investigation. JAMA. 2001;286(2):180–7.
Beckles GL, Engelgau MM, Narayan KM, Herman WH, Aubert RE, Williamson DF. Population-based assessment of the level of care among adults with diabetes in the US. Diabetes Care. 1998;21(9):1432–8.
Harris MI. Medical care for patients with diabetes. epidemiologic aspects. Ann Intern Med. 1996;124(1):117–22.
Campbell RK. Role of the pharmacist in diabetes management. Am J Health Syst Pharm. 2002;59(9):S18–21.
Clifford RM, Davis WA, Batty KT, Davis TM. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the fremantle diabetes study. Diabetes Care. 2005;28(4):771–6.
Coast-senior EA, Kroner BA, Kelley CL, Trilli LE. Management of patients with type 2 diabetes by pharmacist in primary care clinics. Ann Pharmacother. 1998;32(6):636–41.
Davidson MB, Karlan VJ, Hair TL. Effect of a pharmacist-managed diabetes care program in a free medical clinic. Am J Med Qual. 2000;15(4):137–42.
Maccord AD. Clinical impact of a pharmacist-management diabetes mellitus drug therapy management service. Pharmacotherapy. 2006;26(2):248–53.
Anaya JP, Rivera JO, Lawson K, Garcia J, Luna JJ, Ortiz M. Evaluation of pharmacist-managed diabetes mellitus under a collaborative drug therapy agreement. Am J Health Syst Pharm. 2008;65(19):1841–5.
Rothman R, Malone R, Bryant B, Horlen C, Pignone M. Pharmacist-led, primary care-based disease management improves hemoglobin HbA1c in high-risk patients with diabetes. Am J Med Qual. 2003;18(2):51–8.
Irons BK, Lenz RJ, Anderson SL, Wharton B, Habeger B, Anderson G. A retrospective cohort analysis of the clinical effectiveness of a physician-pharmacist collaborative drug therapy management diabetes clinic. Pharmacotherapy. 2002;22(10):1294–300.
Odegard PS, Goo A, Hummel J, Williamas KL, Gray SL. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Ann Pharmacother. 2005;39(3):433–40.
United Kingston Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes (UKPDS 38). BMJ. 1998;317(7160):703–13.
Chiu YW, Chang JM, Lin LI, Chang PY, Lo WC, Wu LC, et al. Adherence to a diabetic care plan provides better glycemic control in ambulatory patients with type 2 diabetes. Kaohsiung J Med Sci. 2009;25(4):184–92.
Carvalho CV, Duarte DB, Merchán-Hamann E, Bicudo E, Laguardia J. Predictors of compliance with highly active antiretroviral therapy in Brasilia, Distrito Federal, Brazil, 1999–2000. Cad Saude Publica. 2003;19(2):593–604.
Odegard OS, Gray SL. Barriers to medication adherence in poorly controlled diabetes mellitus. Diabetes Educ. 2008;34(4):692–7.
Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ. 2007;33(6):1014–29.
World Health Organization. Adherence to long-term therapies: Evidence for action. Geneva: WHO publications; 2003. 211p. (ISBN – 92-4-154599-2). Available: http://apps.who.int/medicinedocs/en/d/Js4883e/.
Rao D, Gilbert A, Strand LM, Cipolle RJ. Drug therapy problems found in ambulatory patient populations in Minnesota and South Australia. Pharm World Sci. 2007;29(6):647–54.
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and non-diabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–34.
Oliveira DS, Tannus LR, Matheus AS, Corrêa FH, Cobas R, Cunha EF, et al. Evaluation of cardiovascular risk according to Framingham criteria in patients with type 2 diabetes. Arq Bras Endocrinol Metabol. 2007;51(2):268–74.
Acknowledgments
The authors would like to thank all the patients who participated in this study.
Funding
The study was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borges, A.P.S., Guidoni, C.M., Ferreira, L.D. et al. The Pharmaceutical care of patients with type 2 diabetes mellitus. Pharm World Sci 32, 730–736 (2010). https://doi.org/10.1007/s11096-010-9428-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-010-9428-3