Abstract
Objective Antibiotics may frequently be prescribed on the basis of vague diagnoses, possibly resulting in unnecessary antimicrobial resistance. Our aim is to map general practitioners’ (GPs’) decision-making for common infections, exploring their diagnostic basis for antibiotic prescriptions. Setting General practice in Iceland. Method Ten in-depth qualitative interviews with, and three observations of, GPs in 1995. Diagnostic issues extracted and analysed. In 2006, eight GPs commented on analysis and updated (email/telephone). Main outcome measure Diagnostic variability and reasons for prescribing antibiotics, consistency or changes over time. Results Wide variations were uncovered in diagnostic procedures, although each GP remained consistent through time. Some GPs had developed “rules-of-thumb”. They often balanced risks against issues like money, time, need for the workforce (perceived importance of the patient’s job), client’s need for job/earnings (perceived ability to afford a sick day) and doctor-patient relationship (risk of refusal adversely affecting the relationship). Perceptions of risk varied from focusing on resistance development to focusing on possible harm from untreated infections, also ranging between considering both to worrying about neither. Changes over time were not prominent but included increased point-of-care testing and the perception by GPs that patients were increasingly willing to “wait and see”. Conclusions Large variability and individuality characterized the GPs’ diagnostic procedures, contrasted by consistency through time. If modification of diagnostic routines is needed, provision of “scientific facts” and technological aids is insufficient. A prerequisite for changing practice is GPs’ acceptance of accuracy of information and of reliability, applicability, and relevance of technology, for physician and/or patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact of findings on practice
-
GPs’ diagnostic procedures vary between individuals and between infections.
-
GPs’ diagnostic procedures are relatively resistant to changes over time.
-
GPs only change diagnostic procedures if they consider themselves to have adequate information, indicating that change is beneficial.
Introduction
Liberal prescribing of antibiotics poses a threat to public health due to its link with increasing antimicrobial resistance [1]. Antibiotic prescriptions are frequently less evidence-based than best-practice requires [2] and often issued presumptively, sometimes over the telephone [3]. Diagnoses are frequently not recorded, missing, or uncertain [4, 5], and vary from one physician to another [6]. Diagnosis is expected to create a rational basis for therapy or prognosis [7] but can also reflect the physician’s special interest in the particular disease/problem, views regarding the physician-role (expected to diagnose), or need to label the problem (communication-tool) [5]. Considering the magnitude of antibiotic prescribing in general practice and claims of unnecessarily liberal prescribing, a thorough understanding of GPs’ diagnostic decision-making is a necessary foundation for successful interventions to improve prescribing [8].
Diagnostic and therapeutic options change rapidly over time, as changes in the availability of medicines and diagnostic tools occur. However, knowledge of GPs’ decision-making and changes/conservatism associated with it remains limited. Qualitative research methods are useful for revealing important, unanticipated issues and understanding in-depth the phenomenon under study [9], but such studies of GPs’ diagnostic procedures for infections seem scarce, as indicated by limited results from search for such literature.
Aim
To understand the use of evidence by GPs in the diagnostic process preceding antibiotic prescribing, and explore changes over time in this diagnostic process.
Methods
In 1995 ten Icelandic GPs were interviewed for ¾–2 h each (semi-structured interviews, Appendix 1). Three of them were observed at work before the interviews, for 3–10 h each, to see them work under different conditions. The initial observations served the twofold purpose of aiding in the construction of the interview guide and illustrating the extent of frankness and openness in the interviews. Two informants from group practices (one rural practice, the other urban) and one informant serving in a solo practice in a large distant rural area, were observed. The observation focus was on GP-patient consultations where antibiotics and/or infections were discussed, including telephone-consultations.
In 2006, the eight informants still alive were re-interviewed after being contacted by phone and agreeing to comment on an analysis of the first round of interviews. Three informants were re-interviewed over the telephone for 15–20 min each and five by e-mail (ranging from short correspondence to detailed back-and-forth correspondence). The re-established contact and re-interviewing (interview-guide in Appendix 1) served a triple purpose:
-
to validate the analysis of diagnostic practices
-
to identify changes in practice over the decade
-
to obtain views on supplementary questions
In 1995, informants were selected to reflect variation in: age (32–67, +11 years 2006), professional experience (1–36 years, +11 years 2006), gender (two female informants, in 1995 and 2006), practice organisation (two working in a solo practice, in 1995 and 2006), employment (contractors/employed 2/8 in 1995 and 0/8 in 2006), geographical area (three rural in 1995 and 2006), specialization (Sweden/Canada/not 6/1/3 in 1995, Sweden/Canada/Iceland 6/1/1 in 2006). Amongst those Icelandic physicians who completed specialist training, the most common country for this specialization was Sweden, followed by Canada. In 1995 a specialization program was set up in Iceland. Addition of informants continued until saturation, the last two interviews did not provide new insights. The project had ethical committee approval and informants gave informed verbal consent.
Detailed field-notes were taken during the observations and the interviews were transcribed verbatim, with the exception of one interview in which permission to audio-record was refused; this was handled like field notes. Issues associated with diagnosis were extracted and analysed in a grounded theory style, both from observations and interviews, by open coding, axial coding, and selective coding [10]. One author coded, and another verified the coding. In the first round of analysis, this was student-supervisor coding-verifying process, with the supervisor ensuring that the PhD student coded appropriately. In the second round, when there was a smaller volume of data, the same persons acted as coder and verifier as in the first round.
The findings were validated in several ways: method triangulation, combining observations and interviewing did not reveal any obvious contradictions between observed behaviour and informants’ descriptions of diagnostic behaviour. Sensitive, even embarrassing issues were observed, and also openly brought up by informants. We also asked the informants for comments/verification of analysis. Our method of doing so a decade after initial data collection has, to our knowledge, not been reported in the literature. Our team, consisting of an Icelandic pharmacist, a Danish pharmacist and an Icelandic physician, provides insider and outsider-views on prescription decisions in general practice in Iceland—yet another approach to validation [11].
Results
Wide variations in diagnostic procedures emerged from the informants’ descriptions, confirmed by observations (the three observed physicians had quite different approaches), although the individual GPs remained remarkably consistent from the first to the second round of data collection. A necessary starting point for examining changes versus consistency is knowledge of the diagnostic practices as observed, and described by the informants, in 1995. The knowledge gained by analysing the data from 1995 is grouped into themes (the analysis that was sent to the informants). The themes are: diagnostic practices, individual physician’s antibiotic policy (including risk perception) and balancing of issues, with the addition of consistency and changes from first to second round of data collection, as analysed by comparing first and second round. Quotes from the informants A–J (referring to first to tenth informant) are numbered Q1–Q13.
Diagnostic practices
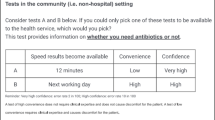
Table 1 illustrates the variety of diagnostic procedures. Sometimes the “diagnosis” was merely a suspicion. Patient complaints or anamnesis (the medical history of the patient) could also constitute the “diagnostic” basis. Indicators of aetiology (varying in reliability) could play a role: many informants had theories about the causative organism, for example based on the colour of liquid from the middle ear, patient’s occupation (Q1), or a cystitis sufferer’s age (Q2).
Q1: “we are a bit in connection with the basic industries here and there seems.. to be.. for example, this is just a feeling really, but I get many fishermen with.. who get hooks in their bodies and.. which of course is dirty in itself but penicillin seems to work well for that, these slime-bacteria. Then again here in the countryside where one knows that there is, well.. yes at least clean soil, clean soil bacteria […….] other people, let’s say here from the local meat industry or something, some floors, someone falls on to the floor, and opens a wound, […….] then I go over to staphylococcus medicines” GP F
Q2: “young women who lead an active sex life…[….] one knows that there is saprophyticus” GP B
A diagnosis could also be based on clinical features, or results from point-of-care tests/aids. The informants were practical about laboratory use, C-reactive protein (CRP) and X-ray, only using such diagnostic aids if they thought the results from these would be useful to them. A couple of informants described increasing use of laboratory tests and X-ray in the second round of data collection.
No informant used the whole range of the diagnostic procedures, shown in Table 1, although an informant could require extensive evidence for some infections but could consider the patient’s description as sufficient evidence for others. Hence, evidence requirements varied widely, depending on the infection and/or GP, sometimes on the patient. Some informants assumed that chronic urinary tract infection (UTI) sufferers would recognise the symptoms themselves, while others felt an examination was necessary. Some GPs used rapid streptococcus tests routinely, others considered them unreliable (due to possibility of false negative or the possibility of the patient being a healthy streptococcus carrier with a viral infection), or found the expiry date of the test kits too unfavourable to buy the bulk packages available at the price offered. The informants described the use of these tests as increasing in second round of data collection. Some GPs considered children’s fighting or crying to complicate the diagnosing of otitis media (Q3), others considered a baby’s cry to indicate pain, and hence helpful in diagnosing.
Q3: “One has to go easy on the child or the person one is examining, because if he/she starts to cry then there can come such a redness and swelling in the ear”. GP B
Distinguishing between bronchitis and pneumonia was described as difficult (Q4).
Q4: “the rough stethoscope sounds more even, rather in bronchitis but the crepetations are normally just one sided, one can say, in the pneumonia. Well, except if it is broncho-pneumonia then there can be rough stethoscope sounds on both sides.. and then of course the pain tells me.. tells one a lot, you see, the pain in pneumonia if it is pneumonia with chest pain”. GP H
Several seemingly unproven or vaguely proven diagnostic procedures were reported. One informant described how smell and appearance of a urine sample indicated the type of bacteria. Another claimed, without further specification, to be able to “see it on the tongue” (no further description) when “diagnosing” tonsillitis, a skill that another informant referred to by quoting research confirming it (Q5).
Q5: “On the one hand I consider whether the patient has fever. If he doesn’t have fever then I am much more reluctant, really, to treat it.. secondly it depends a lot on how many or severe symptoms there are like pain or sheen or soreness and sometimes.. I see a throat that I can just state to anybody that there is overwhelming likelihood that there is streptococcus.. it is a bit more difficult to describe it, it’s an oedema that is a bit special there are bleedings, like tiny bleedings and there are, well, certain signs that one little by little in fact connects and, but this is of course something that cannot be easily proven although research exists that has shown that if doctors see pictures” GP J
A “general upper respiratory tract infection” was described: a very ill patient presenting with symptoms of flaming red throat, coating on the tongue or throat, headache, bone aches, and general malaise. One informant divided infections into long lasting infections with vague symptoms, suited for culture, and severe infections of short duration, requiring quick action (Q6).
Q6: “It is there somewhere in-between usually because if people for example have relatively vague symptoms but rather longstanding then you preferably take a culture and check whether they need antibiotics, on the other hand people with severe symptoms, not to mention kids, have high fever and it seems to me, the clinic, that I see such, I think perhaps there is a suspicion of a bacterial infection, then I prescribe antibiotics to them before, without necessarily taking a culture” GP D
Perceptions of risk and individual GPs’ antibiotic policy
The physicians’ diagnostic routines depended to some extent on their perception of risk. If they thought that withholding treatment could harm the patient, and perhaps also that resistance risk was overrated, they required less evidence to prescribe than if they thought resistance was a real threat, and perhaps also that infections were often a self-limiting condition. Their risk perceptions covered all the above range, and varied from seeing and trying to balance between both/all threats to focusing on one side or stating not to have any particular risk concerns. The GPs’ policy could range from vague ideas to detailed “rules-of-thumb” (broadly applicable principles but not strictly accurate or reliable for every situation). A restrictive attitude was frequently formed under the influence of an older, “guru” type colleague. Inexperienced GPs were often influenced by older colleagues, often resulting in the younger GPs’ adoption of their behaviours/practices without evaluation of the procedures. Influences towards a more liberal prescribing could be caused by the GP having observed serious consequences of untreated infections, perhaps coupled with beliefs about resistance problems being irrelevant to general practice. The informants talked about socialisation into “the Swedish system” (restrictive/narrow spectrum prescribing), but scepticism about the Swedish policy also occurred (Q7).
Q7: “So it is, well, some influence from reading English and American [medical] literature, and then this old Swedish is sitting somewhere in the subconscious, so it is somewhere in between” GP D
Balancing the issues, including uncertainty
Many of the GPs described “rules-of-thumb”, for example, to “localize the infection”, to “treat on the slightest suspicion”, or to exert “diplomatic resistance” (Q8).
Q8: “the person [wants] antibiotics from you, even under the worst of circumstances, where I am practically sure that he does not need them, then, by giving.. people antibiotics, “you want antibiotics, you get antibiotics, but I think you might have coped with this without getting antibiotics”, it has nevertheless, or the experience is.. I feel like this has some influence next time. It all seeps in, you see, so I think this is.. that is why I [think] this diplomacy is important, you see, people always getting to know my opinion, but I let them decide.. you see, the final decision is theirs. ….. […] … this diplomatic resistance, it gives positive results.” GP K
Nevertheless, they all strayed from their “rules-of-thumb” approach if they felt their patient’s case was special. Such straying seemed to cause some dismay/discomfort. A GP could require considerable evidence in diagnosing a particular infection for one particular patient and treat another one on the basis of the slightest suspicion, occasionally contradicting his own general policy.
Every GP mentioned uncertainty in the decision-making, regarding their own clinical abilities (Q9), quality of certain tests, distrust of science, and the dilemma of balancing need for evidence against physician’s, patient’s or society’s resources. A few informants expressed uncertainty without discomfort.
Q9: “this is a very personal style, you see. It is really, what we are taught is that for sinusitis this treatment is needed and such things, sinusitis can be diagnosed with this.. with X-ray.. and then perhaps when one gets more secure in the clinic, then they can allow themselves a bit more.. then this is also personal.. how much demands.. confirm the diagnosis” GP C
Experiences contradicting “scientific facts” were described. Resistance was by some considered a minor problem, unconfirmed by own experience.
The physicians took the diagnostic precision only to the point of reaching a conclusion regarding treatment, only ordering cultures to identify bacteria or determine a susceptibility pattern if they considered results useful for treatment decisions (Q10). This was mainly to save the patients from inconvenience and cost (Q11).
Q10: “Cultures were taken to search for these pneumococci and check whether they were multi-resistant, something like that, …. I never understood this, I thought it would be just as good not to know this, what decided it was in fact just whether this responded to something or nothing” GP J
Q11: “I don’t take cultures very often, you see. It is perhaps.. also because.. when one is under such a pressure as we are here.. one relatively quickly starts skipping tests that do not make any difference and just, then it is also now the way that people themselves have to pay 1500 krónur for this and then perhaps 600 krónur for the consultation or 1000 if it is in the evening” GP J
They did not order cultures under time constraints and/or when limited laboratory access rendered results useless. They did not see patients if they felt confident that the patient knew the symptoms and their meaning, or other reasons (trusting the patients to describe symptoms sufficiently accurately and/or long travelling distance and/or previous similar/identical incidences) made decisions final, but when considering extensive evidence necessary, they met the patient, verified clinical signs, and if still vacillating, order identification/susceptibility tests. The more restrictive physicians (less willing to prescribe) generally felt they needed evidence, compromising only if they considered the delays in treatment too risky. The more liberal physicians (more willing to prescribe) felt they needed the evidence when dealing with persistent infections but, generally, not in other cases. The elderly physician, prescribing on the “slightest suspicion”, only required extensive evidence for sinusitis, where he used X-rays. Considering sinusitis relatively unresponsive to treatment, he diagnosed very precisely to justify a non-prescription solution.
A minority of informants was genuinely concerned about risk of antimicrobial resistance and it seemed to be something the informants had heard/read about rather than experienced. The majority ranked other issues higher in importance: physician-patient relationship, own resources (time), society’s/patient’s resources (money), society’s needs (workforce, i.e., perceived importance of the patient’s job) or patient’s daily-life needs. The emphasis on the patient’s perceived daily-life needs and physician-patient relationship was reinforced in second round as described below, in the physicians’ discussion of the patients’/parents’ increasing acceptance of waiting and seeing.
Development and consistency over time
The eight informants in 2006 generally agreed that the analysis was an accurate description of the diagnostic work as it had been in 1995, and basically still was. A few minor changes were mentioned, such as the above mentioned increasing use of rapid streptococcus tests, although such tests were still considered by some to be insufficiently reliable. The physicians used the same arguments as they had employed 11 years earlier. Increasing use of “stix” (reagent indicator strips), laboratory tests and X-ray was also mentioned by a couple of informants.
Several informants described the patients’ acceptance of the “wait and see” approach (minimum 24 h lag-time between obtaining the prescription and starting treatment for otitis media) as increasing, and one informant linked this change specifically to changed attitudes among young people (Q12).
Q12: “it is an enormous change, because [11 years ago] the mothers just came, and intended to get an antibiotic, at all costs, but now on the other hand, they put ambition into well, absolutely want to wait, and absolutely want to avoid using penicillin if possible” GP C
The informants considered this change in attitudes to have made their work much easier. One informant mentioned that recent research indicated the majority of these infections to be viral. Two informants mentioned that it would be useful to have a clear picture of the bacteria flora.
The informants considered other aspects of diagnosing and prescribing to be basically unchanged for themselves and colleagues, but possibly not for specialists from a different field (Q13).
Q13: Colleagues’ prescriptions generally are just fine, with some exceptions, for example some single paediatricians have tended quite a bit to prescribe, and I understand it partly that they are afraid of prescribing too little if it should lead to death. Vaccination against meningococcus and haemophilus reduces the risk though.” GP I
Responding to the specific questions about changes in prescriptions, none considered their habits to have changed, although one mentioned an increased tendency to allow “lung patients” to have antibiotics in stock. A couple of informants also mentioned a slightly decreasing tendency to treat bronchitis, linking the change to media focus on antimicrobial resistance.
Discussion
Our method of checking consistency, by sending an analysis of 11 year-old data to the informants for commenting has advantages and disadvantages. By doing so, we may have influenced their responses to the new questions. However, most of them had already reported in the initial phone conversations (prior to seeing the analysis of the data) that their procedures were relatively unchanged. It is unlikely that this consistency reporting has been based on wanting to be seen as consistent, considering the development in diagnostic procedures and range of antibiotics, and the criticism of liberal prescribing aired in the mass media on a regular basis since 1995. Re-interviewing with a similar interview guide instead of getting comments on the analysis was possible, but the interviewer presented herself as a PhD student in 1995, whereas she could not have done so in 2006, a fact that could have influenced responses in re-interviewing. The interviews in 2006 were shorter than in 1995, but the analysis of the 1995 interviews created the basis for these interviews which previously did not exist. The informants may have forgotten some changes in behaviour, but their responses to specific questions compared to responses regarding similar issues in 1995 did not suggest this. However, there was some uncertainty about the timing of events (such as referring to something that happened before 1995 as if it had happened later). The informants themselves mentioned the few changes that they considered to have happened. If they had specifically wanted to be seen as up to date in their procedures, or restrictive in prescribing, they might have elaborated more on changes.
Our informants used a practical “common sense” approach [12] to diagnosis and discussed the impact of patient factors (the patient’s type of job, the patient’s expected ability to pay for tests etc.) on their decision-making. The study confirms the individuality and variability revealed in GPs’ prescribing behaviours [13, 14], as also applying to diagnostic behaviour, but reveals a remarkable consistency over time in each individual GP’s diagnostic procedures.
We uncovered large variations in diagnostic procedures between GPs, and in individual GP’s diagnostic practices for different diagnoses. Reasons for such individuality could be: fear of missing something or of catastrophic consequences of restrictive prescribing, reacting to social pressure or ’negotiating’, being the main interface between biomedical concepts and lay beliefs about illness [15].
Our informants are not alone in the extended use of own senses in diagnosing. Assigning predictive value to colour of nasal discharge or sputum when suspecting sinusitis has been described [16]. Examination of the eardrum is a key component in GPs’ diagnosis of acute otitis media [17], although its appearance might not predict the clinical course [18]. Physicians’ concerns regarding rapid streptococcus tests are known from the literature [19]. A practical approach towards use of cultures was also found in Canadian studies, where GPs usually prescribed antibacterials for sore throat before getting results of a culture and when limited access to laboratories could play a role [20, 21]. Our informants’ uncertainty about their clinical observations, laboratory tests and scientifically proven facts agrees with research indicating that diagnoses in general practice often are less certain than in hospitals, and sometimes based more on signs and symptoms than tests [22, 23]. Microbiological diagnosis for infections in the community is rarely available at the time of prescribing, often not at all and the aetiology is variable, even mixed [4, 24], which underlines GPs need for user-friendly, up-to-date information on susceptibility trends [24]. Patient demand and limited resources are also known to hinder GPs in living up to their own ideals [8]. Creation of rules-of-thumb or mindlines (collectively reinforced, internalized tacit guidelines), as shortcuts to tacit knowledge, may be a reaction to time pressure [13, 25, 26].
The appropriateness of increasing X-ray use for diagnosis is not known. Informants in a Belgian study, who considered diagnoses for respiratory tract infections to be uncertain, questioned the value and feasibility of technical investigations such as blood or sputum analysis and X-ray [23], which also has been described as risky [4].
Our informants considered patient expectations to have changed. A significant association has been found between general practitioners’ presumptions about patient expectations and real patient expectations [27], although contradictory results also exist [21]. A relationship between physician prescribing habits and parental knowledge has been found [28] and physicians have connected propaganda in the media with parental change in attitudes towards antibiotics for their children [29]. The media coverage in Iceland might explain patients’/parents’ increasing willingness to wait and see, as a mass media campaign has been found to have a role in changing antimicrobial prescribing practice[30].
Our informants’ statements of only subtle changes in their decision-making do not fully agree with trends in antibiotic prescribing in Iceland [31], possibly due the low number of informants or to changes in specialist-prescribing (as indicated by our informants). The methods used in this project aimed at in-depth understanding, not at statistical reliability. Therefore, our analysis is not meant to explain changes in magnitude of prescribing.
In spite of many theories on implementing changes in physician-behaviour, it still seems a difficult task. Magic bullet strategies, assuming a critical moment of change might miss the point, as the dominant process may, in agreement with our study be stability and continuity [32]. The hypothesis about consistency being the dominant process is reinforced by the fact that a work on national guidelines started shortly after the initial interviews. The first guidelines were published in 1997 [33], and the guideline work is still ongoing [34].
The ideal for diagnostic procedures, evidence based medicine (EBM), a 4-step procedure of formulating a clear clinical question, searching the literature, critically appraising evidence, and implementing useful findings in clinical practice [35] or a stepwise diagnostic reasoning based on background knowledge, everyday knowledge, non-verbal communication, and clinician’s feelings [36] are possible procedural options. The non-verbal communication and the clinician’s feelings do not seem to be included in the EBM approach, although clearly identifiable in our study. Framing a problem can be complex in general practice and adapting EBM to the GPs knowledge of the patient’s complaint threshold is also an issue [36]. Therefore, it remains complicated to use the EBM approach in daily practice, and more training in managing uncertainty might be needed [37].
Conclusion
A high degree of variability and individuality characterised the GPs’ procedures, although the individual GP remained remarkably consistent throughout the 11 years. If interventions into GPs’ diagnostic routines are considered necessary, bombarding them with “scientific facts” and technological aids is unlikely to suffice to change their deeply-rooted practices. Individual GP’s reality and perspectives must also be taken into account. Prerequisites for change are that: GPs’ accept the information as being correct, the technology as reliable and acceptable to patients, and the information and technology as practical and applicable in their own practice.
Notes
In 1995 there were discussions about referrals from a GP, for granting patient’s access to specialists in other fields. These discussions had created a tug-of-war between GPs and specialists
References
Friedman CR, Srinivasan A. Public health responses to antimicrobial resistance in outpatient and inpatient setting, Chapter 16. In: Wax RG, Lewis K, Salyers AA, Taber H, editors. Bacterial resistance to antimicrobials, 2nd ed. Boca Raton: CRC Press; 2008. ISBN 978-0-8493-9190-3.
O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, et al.. Educational outreach visits: effects on professional practice and health care outcomes (Review). Reprint of a Cochrane review, published in The Cochrane Library 2008(3). http://apps.who.int/rhl/reviews/CD000409sp.pdf. Accessed on 7 May 2010.
Björnsdóttir I, Hansen EH. Telephone prescribing of antibiotics: general practitioners’ views and reflections. Eur J Pub Health. 2001;11(3):260–3.
McGavock H, Webb CH, Johnston GD, Milligan E. Drug marketing: the most powerful external influence on prescribing. In: McGavock H, et al., editors. The prescribing jigsaw. Belfast: Drug Utilisation Research Unit, Queen’s University; 1998.
Wick A. The importance of diagnosis in general practice. Schweiz Rundsch Med Prax. 1993;82:68–76.
Kaplan RM. Uncertainty, variability, and resource allocation in the health care decision process, Chapter 14. In: Friedman HS, Silver RC, editors. Foundations of health psychology. New York: Oxford University Press; 2007. ISBN: 978-0-513959-4.
Gyssens IC, Kullberg BJ. Improving the quality of antimicrobial drug use can result in cost containment. Pharm World Sci. 1995;17(5):163–7.
Henriksen K, Hansen EH. The threatened self: general practitioners’ self-perception in relation to prescribing medicine. Soc Sci Med. 2004;59(1):47–55.
Bradley C. Insights from qualitative research are needed to improve GP prescribing. Eur J Gen Pract. 2002;8:3–4.
Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park: Sage Publications; 1990.
Janesick V. The choreography of qualitative research design: minutes, improvisations and crystallization. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2000. p. 379–99.
Hansen EH. Rationality and common sense in Danish drug therapy. J Soc Adm Pharm. 1988;5(3/4):105–13.
Björnsdóttir I. Studies in prescribing of antibiotics in Iceland: a qualitative and quantitative approach. Copenhagen: The Royal Danish School of Pharmacy, Department of Social Pharmacy, 1999.
Wigton RS, Darr CA, Corbett KK, Nickol DR, Gonzales R. How do community practitioners decide whether to prescribe antibiotics for acute respiratory tract infections? J Gen Intern Med. 2008;23(10):1615–20. doi:10.1007/s11606-008-0707-9.
Howie JGR. Some non-bacteriological determinants and implications of antibiotic use in upper respiratory tract illness. Scand J Infect Dis Suppl. 1983;39:68–73.
Fahey T. Bronchitis and sinusitis, Chapter 4.1. In: Gibson PG, editor. Evidence-based respiratory medicine. Oxford: Blackwell Publishing; 2005. ISBN: 978-0-7279-1605-1.
Sundberg M. Optical methods for tympanic membrane characterisation. Linköping studies in science and technology dissertation no. 1173. Linköping: Linköping University; 2008. ISBN 978-91-7393-933-1.
Appelman CLM, Claessen JQPJ, Touw-Otten FWMM, Hordijk GJ, de Melker RA. Severity of inflammation of tympanic membrane as predictor of clinical course of recurrent acute otitis media. BMJ. 1993;306:895.
Reid MC, Lane DA, Feinstein AR. Academic calculations versus clinical judgments: practicing physicians’ use of quantitative measures of test accuracy. Am J Med. 1998;104:374–80.
McIsaac WJ, Goel V. Sore throat management practices of Canadian family physicians. Fam Pract. 1997;14:34–9.
Paluck E, Katzenstein D, Frankish CJ, Herbert CP, Milner R, Speert D, Chambers K. Prescribing practices and attitudes toward giving children antibiotics. Can Fam Physician. 2001;47:521–7.
Howie JG. Diagnosis: the Achilles heel? J R Coll Gen Pract. 1972;22(118):310–5.
Coenen S, van Royen P, Vermeire E, Hermann I, Denekens J. Antibiotics for coughing in general practice: a qualitative decision analysis. Fam Pract. 2000;17(5):380–5.
Finch R. Bacterial resistance: the clinical challenge. Clin Microbiol Infect. 2002;8(Suppl 3):21–32.
Andre M, Borgquist L, Molstad S. Use of rules of thumb in the consultation in general practice: an act of balance between the individual and the general perspective. Fam Pract. 2003;20(5):514–9.
Gabbay J, le May A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ. 2004;329(7473):1013.
Cockburn J, Pit S. Prescribing behaviour in clinical practice: patients’ expectations and doctors’ perceptions of patients’ expectations: a questionnaire study. BMJ. 1997;315(7107):520–3.
Arason VA, Sigurdsson JA, Kristinsson KG, Getz L, Gudmundsson S. Otitis media, tympanostomy tube placement, and use of antibiotics. Cross-sectional community study repeated after five years. Scand J Prim Health Care. 2005;23(3):184–91.
Kristinsson KG. Modification of prescribers’ behavior: the Icelandic approach. Clin Microbiol Infect. 1999;5(Suppl 4):S43–7.
Lambert MF, Masters GA, Brent SL. Can mass media campaigns change antimicrobial prescribing? A regional evaluation study. J Antimicrob Chemother. 2007;59(3):537–43. doi:10.1093/jac/dk1511.
Anonymous. Use of drugs in Iceland 1996-2005. Icelandic Ministry of Health. http://www.heilbrigdisraduneyti.is/media/Lyfjamyndir/Notkun_lyfja_a_Islandi_1996-2005.pdf. Accessed 7 May 2010.
Armstrong D. Clinical autonomy, individual and collective: the problem of changing doctors’ behaviour. Soc Sci Med. 2002;55(10):1771–7.
Publications and reports (In Icelandic = Rit og skýrslur). The Directorate of Health (Landlæknisembættið). http://www.landlaeknir.is/Utgafa/Ritogskyrslur. Accessed 7 May 2010.
Clinical guidelines (In Icelandic = Klínískar leiðbeiningar). The Directorate of Health (Landlæknisembættið). http://www.landlaeknir.is/Kliniskarleidbeiningar. Accessed 7 May 2010.
Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem-solving. BMJ. 1995;310:1122–6.
Forde R. Competing conceptions of diagnostic reasoning: is there a way out? Theor Med Bioeth. 1998;19(1):59–72.
Fargason CA Jr, Evans H, Ashworth CS, Capper SA. The importance of preparing medical students to manage different types of uncertainty. Acad Med. 1997;72:688–92.
Acknowledgments
We thank our informants for the participation and Maxine Ingalls, RN, for proofreading.
Funding
Research is a part of our duties within our ordinary paid jobs. This research was done within that scope.
Conflicts of interest
We have no conflicts of interests to declare.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Original guide = questions asked in 1995
-
Years in general practice?
-
What is your view regarding use of antibacterials? (on the slightest suspicion, only when based on cultures or somewhere in-between)
-
How do you prescribe for sore throat? (symptoms, treatment) For sinusitis? For infections in the respiratory tract? For UTI? For dermatological infections? Other infections?
-
For children? (probe for otitis here) Elderly people? Women versus men?
-
Usability and disadvantages of specific antibiotics? (groups)
-
Recall the last 10 [antibiotic prescriptions]. Any uncomfortable?
-
Do patients press? If yes, what do you think the reason is? (certain types??)
-
Time pressure?
-
Telephone prescriptions. How decided?
-
Fear of resistance problems?
-
Laboratory facilities in the town?
-
Cost to patient?
-
Composition of wages?
-
The secretary/the telephone lady?
-
Co-operation between the physicians?
-
(The referral case?)Footnote 1
-
Co-operation with pharmacy?
-
Anything you would like to add, - or anything I forget to ask about?
Supplementary questions = questions asked in 2006
-
How have your prescribing habits regarding the most common infections changed during these 10–11 years from the initial interview?
-
(common infections: otitis, sinusitis, sore throat, UTIs, pneumonia, dermatological infections)
-
If changes—why do you think the changes occurred?
-
Have there been changes in your prescribing of azithromycin, ciprofloxacin and doxycyklin (official sales statistics indicate changes in the use of these drugs)
-
What is your view regarding the development in resistance to antibiotics?
-
What is your opinion regarding the authorities’ response to that development?
-
What is your view regarding your prescribing habits for antibiotics?
-
Do you think your prescribing is on a suitable level, or is your antibiotic prescribing on a level that you consider unfortunate in some way?
-
Why?
-
What is your view regarding your colleagues’ prescribing of antibiotics?
-
Is their prescribing on a suitable level, or is it unfortunate in some way?
-
Why?
Rights and permissions
About this article
Cite this article
Björnsdóttir, I., Kristinsson, K.G. & Hansen, E.H. Diagnosing infections: a qualitative view on prescription decisions in general practice over time. Pharm World Sci 32, 805–814 (2010). https://doi.org/10.1007/s11096-010-9441-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-010-9441-6