Abstract
Purpose
The objective of this study was to assess the bioavailability and the sedative effect of a single-dose administration of an innovative oral solution of midazolam containing γ-cyclodextrins (ADV6209).
Methods
A bioavailability study with a standard two-sequences, two-periods, and crossover design was conducted. Subjects randomly received 15 mg of ADV6209 by oral route followed by 5 mg of the reference drug (midazolam hydrochloride intravenous solution (Hypnovel®, Roche) by intravenous route or vice versa. Blood samples were drawn at different time points to measure midazolam and its metabolite α-hydroxymidazolam concentrations. Non-compartmental pharmacokinetic methods were used to calculate main pharmacokinetic parameters and absolute bioavailability.
Results
Caucasian healthy subjects (n = 12) were included in the study. ADV6209 had a bioavailability of 39.6%. The oral elimination half-life with ADV6209 was slightly shorter than with the reference i.v. form (2.66 h versus 2.99 h). The sedative effect was observed 27.5 ± 15.5 min after oral administration for a duration of 48.5 ± 35.4 min. Double peak phenomenon was observed in 5 patients.
Conclusions
Cyclodextrins have little impact on midazolam oral bioavailability and the pharmacokinetics parameters of midazolam formulation ADV6209 are close to those reported previously.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sedation and cooperation of children are needed to ease minor surgery (e.g. laceration repairs, dental surgery) or anesthesia induction [1]. Due to its short pharmacokinetic half-life (around 2 h), its hypnotic, and its myorelaxant properties, midazolam is commonly used for moderate sedation especially in the pediatric population [2]. Additional benefits may result from moderate sedation with a benzodiazepine such as midazolam, like a better control of post-operative behavioral disturbances, [3] due in part to the anterograde amnesia it can induce [4]. In the pediatric setting, it is generally recommended to avoid unpleasant routes of administration such as intravenous (iv), where the oral route of administration is preferred [5]. The usual dosage of oral midazolam for moderate sedation in children ranges between 0.25–1 mg/kg [5, 6] As no licensed oral solution is available in most European countries, it is usual to administer midazolam intravenous solution orally, however it exhibits a strong bitterness, which can cause children to spit out the dose or trigger nausea and vomiting, hampering its utilization [7]. Sometimes extemporaneous preparations are made by mixing the intravenous solution with a fruit juice or syrup, but they are not always well controlled in terms of solubility and stability.
In order to address this lack of available licensed oral formulation, an innovative oral liquid formulation ready to use was previously proposed (ADV6209) [8]. This oral solution, aiming at treating children from the age of 6 months, was developed to facilitate dose adjustments according to the children’s weight. Palatability concerns were addressed as recommended by the EMA. For that purpose, the intense sweetener sucralose that exhibits a bitter masking effect [9], an orange aroma, and a cyclodextrin were used [10]. γ-cyclodextrin offers the advantage that it can decrease midazolam bitterness and enhance its aqueous solubility, by forming an inclusion complex with the drug [8]. Additionally, we reported that the addition of γ-cyclodextrin or randomly methylated β-cyclodextrins could improve the stability of midazolam in the formulation conferring an additional benefit to the use of cyclodextrins [11]. The impact of cyclodextrins on the oral pharmacokinetics of drugs depends mainly on the physicochemical properties of the guest compound. It is for example well known that cyclodextrins, by solubilizing lipophilic drugs, could enhance their bioavailability [12]. For example another benzodiazepine, diazepam, has been demonstrated to lead to increased bioavailability when complexed with cyclodextrins and administered orally to rabbits or humans [12]. However, the absolute bioavailability of midazolam using an orally administered midazolam:γ-cyclodextrin complex has to our knowledge, never been previously reported.
A pharmacokinetic study was done in healthy adults in order to determine the main pharmacokinetic parameters, including the absolute oral bioavailability, of the industrially optimized 0.2% midazolam solution containing γ-cyclodextrin (ADV6209). Sedation scores, safety and tolerability were also assessed before pursuing the development of this oral formulation for use in children.
Methods
Study Design
A monocentric randomized bioavailability study with a standard two-sequence two-period crossover design was conducted. The study was approved by the west regional independent ethics committee (CPP Ouest, France) and registered (EudraCT 2012–003047-30). Written informed consent was obtained from all subjects. The study population consisted of healthy non-smoking adult subjects, women or men, aged 18–55 years, with a BMI of 18.5–25 kg/m2, without major medical history or chronic conditions.
Two treatments were investigated; the innovative 0.2% midazolam solution containing γ-cyclodextrin [8] (ADV6209) as the test formulation and an already marketed midazolam hydrochloride intravenous solution (Hypnovel®, Roche) as the reference formulation. Eligible subjects were enrolled and randomly assigned to one of the two sequences to receive 15 mg of the test formulation orally then 5 mg of the reference formulation by intravenous route or vice versa. Based on the short half-life of the product, there was a washout period of at least three days between the two treatment periods, Blood samples were drawn just before and 5, 10, 15, 20, 30, 40, 50 min and 1, 1.5, 2, 4, 6, 9 and 12 h after administration. Plasma concentration of midazolam and its main active metabolite, α-hydroxymidazolam, were determined using a validated LC-MS/MS method with a limit of quantification (LOQ) of 0.100 ng/ml for both analytes.
Study Endpoints
Individual pharmacokinetic parameters were determined for midazolam and α-hydroxymidazolam. Non-compartmental methods were used to determine the area under the curve from 0 to the last time point (AUC 0 → Tlast ), the area under the curve extrapolated to infinity (AUC 0 → ∞), the maximal concentration (C max ), the time to reach maximal concentration (T max ), the terminal elimination rate constant (λ z ), the terminal half-life (T 1/2), and the absolute bioavailability (F) [13]. Area under the curve was determined with the method of linear interpolation using the trapezoidal rule. The terminal elimination rate constant (λ z ) was determined by a log-linear regression using the last three time-points. In order to determine λ z and then extrapolate AUC 0 → Tlast to infinity (i.e. to determineAUC 0 → ∞), the adjusted coefficient of determination of the log-linear regression (Adj. R2) had to be greater than 0.8, otherwise data were not used for statistical purposes. Individual ratios AUC 0 → ∞/AUC 0 → Tlast had also to be greater than 0.8 to determine bioavailability. Midazolam dose (D) normalised parameters, AUC 0 → ∞/D , AUC 0 → Tlast /D, and C max /D, and metabolic ratio (MR) (ratio of AUC 0 → ∞ values of midazolam and α-hydroxymidazolam) were also calculated.
Sedation was assessed using two different sedation scales: a visual analog scale for alertness (VAS) [14] and the observer’s assessment of alertness/sedation (OAAS) scale [15]. The OAAS score was rated by the investigator at 11 time points (just before treatment and 15, 30, 40, 50 min and 1, 1.5, 2, 4, 9 and 12 h after administration) and the VAS alertness score was rated by the subject at 10 time points (just before treatment and 15, 30, 40 min and 1, 1.5, 2, 4, 9 and 12 h after administration). Subjects with OAAS score ≤ 17 were considered sedated [16].
For safety evaluation purposes, the subjects were physically examined and monitored (oxyhemoglobin saturation, diastolic and systolic blood pressure, heart rate, respiratory rate, temperature) just before and after administrations, and regularly thereafter until 12 h after administration. Routine laboratory tests were performed and any adverse events were noted.
Statistical Analysis
Standard descriptive analyses of pharmacokinetic and pharmacodynamic data were performed. Unless otherwise stated, data were represented as mean ± standard deviation. Analysis of variance (ANOVA) was performed on AUC 0 → ∞/D, AUC 0 → Tlast /D, and C max /D to detect the presence of period effect, a carry-over effect, and a direct drug effect. [13].
For pharmacodynamic analyses, either data corresponding to the test formulation alone, or a set of combined data corresponding to test and reference formulation together were used. The relationship between plasma concentrations of midazolam or the sum of midazolam and α-hydroxymidazolam for each time point and the corresponding OAAS score was analyzed by linear regression. The relationship between plasma concentrations and the corresponding sedation state (sedated or not sedated, OAAS score = 17 as cut-off) was analyzed by logistic regression for each time point. A previously described logistic model was applied to determine the EC50 – the plasma concentration at which the predicted probability of a positive response is 50%. Statistical analysis and graphs were produced using SAS® (8.0) software and R (3.2.2) software and results were considered to be significant if p value was <0.05.
Results
Healthy Caucasian men (n = 6) and women (n = 6) were enrolled in the crossover study. The mean age of the subjects was 43.9 ± 8.6 years, the mean weight was 62.9 ± 11.0 kg, and the mean BMI was 22.6 ± 1.7 kg/m2.
Pharmacokinetics
Mean pharmacokinetics parameters are summarized in Table I . Regarding ADV6209, λ z AUC 0 → ∞ could not be determined for midazolam in 4 (33%) subjects and for α-hydroxymidazolam in 3 (25%) subjects as adj. R2 of the terminal log linear regressions were too small. The test formulation produced a mean midazolam plasma peak concentration of 113 ± 51.1 ng/ml, 20 to 120 min (median 35 min) after administration. Its absolute bioavailability ranged between 16.3 and 52.4% (mean 39.4%) and the metabolic ratio ranged between 13.8 and 69.1% (mean 38.7%). Mean pharmacokinetic profiles are depicted in Figs. 1 and 2 alongside both sedation scores.
(From top to bottom) plasma concentration profiles of midazolam (black solid line) and α-hydroxymidazolam (red dashed line) on logarithmic scale and normal scale, OAAS score, and change from baseline of VAS score obtained after oral administration of 15 mg of ADV6209, versus time (common time axis; mean, sd)
(From top to bottom) plasma concentrations profiles of midazolam (black solid line) and α-hydroxymidazolam (red dashed line) on logarithmic scale and normal scale, OAAS score, and change from baseline of VAS score obtained after intravenous administration of 5 mg of reference formulation, versus time (common time axis; mean, sd)
No carry-over effect or period effect was observed by the ANOVA analysis for the midazolam pharmacokinetic parameters AUC 0 → ∞/D (p = 0.48 and p = 0.25 respectively), AUC 0 → Tlast /D (p = 0.16 and p = 0.19 respectively), and C max /D (p = 0.12 and p = 0.73 respectively). A treatment effect was detected (p < 0.0001 for all three parameters) meaning that the variation of mean pharmacokinetic parameters observed between both sequences or periods was only due to the nature of the treatment.
Pharmacodynamics
Mean OAAS scores and VAS scores are depicted in Fig. 1 (for ADV6209) and Fig. 2 (for the iv formulation), alongside midazolam and α-hydroxymidazolam pharmacokinetic profiles.
All subjects were sedated (OAAS score ≤ 17) at least at one time-point after administration of ADV6209, two subjects were never sedated (OAS/S score > 17) after administration of the reference formulation. Considering the OAAS scores of the subjects for whom sedation was achieved, sedation began 27.5 ± 15.5 min after oral administration and lasted 48.5 ± 35.4 min with ADV6209. All subjects were completely alert 4 h after administration. The maximum mean sedation levels were observed between 30 and 60 min after oral administration (OAAS scores 15.7 to 15.9). The VAS alertness scores corroborated these results with a maximum score 60 min after oral administration of midazolam (VAS score 52.76 ± 21.5).
Pharmacokinetic/Pharmacodynamic Relationships
The time profiles of both sedation scores were consistent with that of the mean midazolam plasma concentrations. However, linear regression analysis of OAAS scores showed poor linear correlation of sedation with midazolam and midazolam + α-hydroxymidazolam concentrations for the combined dataset (y = −20.1 + 0.0535 x, R2 = 0.437, p < 0.05 and y = −20.1 + 0.0422 x, R2 = 0.4, p < 0.05, respectively).
Midazolam EC50 values of 53.8, 61.9 and 57.8 ng/ml were obtained from logistic regression analyses for the test formulation, the reference formulation, and for the combined dataset, respectively (Fig. 3). Among all pharmacokinetic time-points (test formulation and reference formulation) for which an OAAS score was determined, the median concentration of midazolam and midazolam + α-hydroxymidazolam that produced sedation was 63.2 ng·ml−1, IC 95% [55.1–71.3] and 76.1 ng·ml−1, IC 95% [64.4–87.8] (Fig. 4).
Probability of being sedated (OAAS ≤17) according to midazolam concentrations after oral administration of 15 mg of ADV6209 (top), after intravenous administration of 5 mg of reference formulation (middle) and for both dataset combined (bottom), with actual state of sedation according to midazolam concentration (●) and EC50 (red) depicted on all three graphs (common concentration axis)
Safety
No clinically relevant changes were observed in hemodynamic parameters (blood pressure and heart rate), ECG time intervals, oxyhemoglobin saturation, and routine laboratory tests. No serious adverse events were observed during the study.
Discussion
The pharmacokinetic profile of orally administered midazolam:γ-cyclodextrin complex solution (ADV6209) is similar to that of orally administered midazolam solutions or tablets previously described in the literature (Table II). As evidenced by the standard deviations of pharmacokinetic parameters, the pharmacokinetics of midazolam showed high inter-individual variability, most likely reflecting differences of drug-metabolizing enzyme levels, which is characteristic following administration of this drug via the oral route [17]. Elimination half-life (T 1/2 = 2.66 h) was within the range of previous findings for adults (Table II). Administration of ADV6209 resulted in an average oral bioavailability of 39.4% with a very broad range (F = 16.3–52.4%). These results were within the range of previous findings for oral administration of midazolam alone to adult subjects (F = 20.9 to 48.4%) (Table II) or to pediatric patients (F = 27.0 to 36.0%) [18, 19] and demonstrate that cyclodextrins have little or no impact on midazolam bioavailability. Drug absorption is a continuous process of dissolution and permeation and cyclodextrins are known to enhance bioavailability of lipophilic drugs by solubilizing them [12] without changing their intrinsic ability to permeate lipophilic membranes [20]. In solution, midazolam exists both in a lipophilic close ring form and in a hydrophilic open ring form which are in equilibrium. The amount of open ring form impacts its solubility and is influenced by pH [21]. At acidic pH, as in the stomach, the solubility of midazolam is optimal as a high amount of open ring form is present. Regarding the biopharmaceutical classification system (BCS) midazolam is considered highly soluble and highly permeable (i.e. BCS class I drug) at the doses administered and at gastric pH values [22]. Accordingly, and based on our observations, solubilizing midazolam with cyclodextrins to form a pharmaceutical solution is unlikely to enhance its solubility in gastric fluids at the doses generally administered. Thus its oral bioavailability is not likely to be modified as for truly lipophilic drugs (i.e. BCS class II drugs) [23]. First pass metabolism by enterocytes and hepatocytes remains the main factor limiting the bioavailability of midazolam [24] as illustrated by the difference between the metabolic ratios obtained after intravenous administration (mean 13.4%) and after oral administration (mean 38.7%).
Pharmacokinetic profiles of the test formulation showed a double-peak phenomenon (a 2nd peak 1 h after the 1st peak and approximately 2 h after administration) and the second peak was clearly visible in 5 subjects (Fig. 5). This phenomenon has been previously observed with oral administration of midazolam or other benzodiazepines [25] and appears to be more pronounced with higher (15 mg) oral doses [26] of midazolam than with lower (≤ 5 mg) doses [27, 28]. Usually the double peak phenomenon results from enterohepatic recirculation, delayed gastric emptying, or variability of absorption of the drug in the different regions of the gut [29]. We already know that BCS class I drugs may have their pharmacokinetics altered by gastric emptying [30] and that delayed gastric emptying may produce a double peak phenomenon [31]. We also know that midazolam could induce a delayed gastric emptying [32]. In the present study, double-peaks are believed to be related to a delayed gastric emptying in some subjects. Although we could not formally exclude the role of γ-cyclodextrins in a possible sequestration/release phenomenon, it is unlikely due to the rapid hydrolysis of γ-cyclodextrin by pancreatic and salivary amylases [33] and because of the small association constant of the midazolam:γ-cyclodextrin complex (K = 283 M−1) [8]. A larger association constant and a poor in vivo dissolution of the drug:cyclodextrin complex are generally needed to sequester a drug inside cyclodextrins [34]. Caution should be taken regarding the concomitant use of drugs affecting gastric emptying such as prokinetics or medications that delay gastric emptying, as they are likely to significantly alter the pharmacokinetic profile of midazolam. The impact of this double-peak phenomenon on the sedation state seems to be minimal as no subjects were sedated 4 h after oral administration of 15 mg of midazolam.
The EC50 calculated for the test formulation was close to previously reported values obtained using the same sedation scale in young children and adolescents (EC50 = 51.4 ng/ml) [16]. As shown in Fig. 4 , midazolam concentrations were distributed according to the discrete variable “sedation state” and there were only 8.3% and 9.1% of subjects with a concentration above the EC50 but not sedated for the test formulation and for the combined dataset, respectively. The active metabolite of midazolam may significantly contribute to the effects of the parent compound, which could explain the lower midazolam EC50 observed with ADV6209 when compared to the reference form, the former presenting a higher metabolic ratio.
The poor linear correlation between sedation scores and midazolam plasma concentrations could partly be due to the fact that a slight counter-clockwise hysteresis was observed, most probably resulting from a dispositional delay [35].
Conclusion
The use of cyclodextrins with midazolam presents an interesting option for specific pediatric pharmaceutical formulation purposes (e.g. pharmaceutical solubilization, aqueous stability enhancement, and palatability improvement through bitter taste masking).
The results of this phase I study are supportive of carrying out PK and PD studies in children. As expected for BCS class I drugs, cyclodextrins do not appear to alter pharmacokinetic parameters of midazolam. Therefore, the doses generally recommended in children with other oral formulations should be respected for pediatric use of the present oral solution.
Abbreviations
- λ z :
-
Terminal elimination rate constant
- AUC 0 → ∞ :
-
Area under the concentration-time curve from zero up to infinity with extrapolation of the terminal phase
- AUC 0 → Tlast :
-
Area under the concentration-time curve from 0 up to the last time point
- C max :
-
Observed maximum plasma concentration after administration
- D :
-
Dose administered
- EC50 :
-
Plasma concentration at which the predicted probability of a positive response is 50%
- iv:
-
Intravenous
- LOQ:
-
Limit of quantification
- F :
-
Absolute bioavailability
- MR :
-
Metabolic ratio
- OAAS:
-
Observer’s assessment of alertness/sedation scale
- R2 :
-
Coefficient of determination
- T 1/2 :
-
Terminal half-life
- T max :
-
Time to reach C max
- VAS:
-
Visual analogue scale
References
Pacheco GS, Ferayorni A. Pediatric procedural sedation and analgesia. Emerg med Clin North am. 2013;31:831–52.
Nordt SP, Clark RF. Midazolam: a review of therapeutic uses and toxicity. J Emerg med. 1997;15:357–65.
Cox RG, Nemish U, Ewen A, Crowe M-J. Evidence-based clinical update: does premedication with oral midazolam lead to improved behavioural outcomes in children? Can J Anesth. 2006;53:1213–9.
Kain ZN, Hofstadter M, Mayes LC, Krivutza D, Alexander G, Wang S-M, et al. Midazolam: effects on amnesia and anxiety in children. Anesthesiology. 2000;93:676–84.
Kupietzky A. Evaluation of oral or rectal midazolam as conscious sedation for pediatric patients in oral surgery. Pediatr Dent. 1993;15:237–41.
De Wildt SN, Kearns GL, Hop WCJ, Murry DJ, Abdel-Rahman SM, Van Den Anker JN. Pharmacokinetics and metabolism of oral midazolam in preterm infants. Br J Clin Pharmacol. 2002;53:390–2.
McCann ME, Kain ZN. The management of preoperative anxiety in children: an update. Anesth Analg. 2001;93:98–105.
Marçon F, Mathiron D, Pilard S, Lemaire-Hurtel AS, Dubaele JM, Djedaini-Pilard F. Development and formulation of a 0.2% oral solution of midazolam containing γ-cyclodextrin. Int. J. Pharm. 2009;379:244–50.
Ley JP. Masking bitter taste by molecules. Chemosens Percept. 2008;1:58–77.
Walsh J, Cram A, Woertz K, Breitkreutz J, Winzenburg G, Turner R, et al. Playing hide and seek with poorly tasting paediatric medicines: do not forget the excipients. Adv. Drug Deliv Rev. 2014;73:14–33.
Mathiron D, Marçon F, Dubaele J-M, Cailleu D, Pilard S, DjedaÏni-pilard F. Benefits of methylated cyclodextrins in the development of midazolam pharmaceutical formulations. J Pharm Sci. 2013;102:2102–11.
Carrier RL, Miller LA, Ahmed I. The utility of cyclodextrins for enhancing oral bioavailability. J Control Release. 2007;123:78–99.
Chow S-C, Liu J. Design and analysis of bioavailability and bioequivalence studies. Third Edition: CRC Press; 2008.
Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br J med Psychol. 1974;47:211–8.
Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, et al. Validity and reliability of the Observer’s assessment of alertness/sedation scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244–51.
Brosius KK, Bannister CF. Oral midazolam premedication in preadolescents and adolescents. Anesth Analg. 2002;94:31–6.
Tateishi T, Watanabe M, Nakura H, Asoh M, Shirai H, Mizorogi Y, et al. CYP3A activity in European American and Japanese men using midazolam as an in vivo probe. Clin Pharmacol Ther. 2001;69:333–9.
Payne K, Mattheyse FJ, Liebenberg D, Dawes T. The pharmacokinetics of midazolam in paediatric patients. Eur J Clin Pharmacol. 1989;37:267–72.
Reed MD, Rodarte A, Blumer JL, Khoo KC, Akbari B, Pou S, et al. The single-dose pharmacokinetics of midazolam and its primary metabolite in pediatric patients after oral and intravenous administration. J Clin Pharmacol. 2001;41:1359–69.
Másson M, Loftsson T, Másson G, Stefánsson E. Cyclodextrins as permeation enhancers: some theoretical evaluations and in vitro testing. J Control Release. 1999;59:107–18.
Gerecke M. Chemical structure and properties of midazolam compared with other benzodiazepines. Br J Clin Pharmacol. 1983;16(Suppl 1):11S–6S.
Amidon GL, Lennernäs H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm res. 1995;12:413–20.
Loftsson T. Cyclodextrins and the biopharmaceutics classification system of drugs. J Incl Phenom Macrocycl Chem. 2002;44:63–7.
Thummel KE, O’Shea D, Paine MF, Shen DD, Kunze KL, Perkins JD, et al. Oral first-pass elimination of midazolam involves both gastrointestinal and hepatic CYP3A-mediated metabolism. Clin Pharmacol Ther. 1996;59:491–502.
Wang Y, Roy A, Sun L, Lau CE. A double-peak phenomenon in the pharmacokinetics of alprazolam after oral administration. Drug Metab Dispos. 1999;27:855–9.
Guo T, Mao G-F, Xia D-Y, Su X-Y, Zhao L-S. Pharmacokinetics of midazolam tablet in different Chinese ethnic groups. J Clin Pharm Ther. 2011;36:406–11.
Schwagmeier R, Alincic S, Striebel HW. Midazolam pharmacokinetics following intravenous and buccal administration. Br J Clin Pharmacol. 1998;46:203–6.
Belle DJ, Callaghan JT, Gorski JC, Maya JF, Mousa O, Wrighton SA, et al. The effects of an oral contraceptive containing ethinyloestradiol and norgestrel on CYP3A activity. Br J Clin Pharmacol. 2002;53:67–74.
Godfrey KR. Arundel P a, dong Z, Bryant R. Modelling the double peak phenomenon in pharmacokinetics. Comput. Methods Programs Biomed. 2011;104:62–9.
Wu CY, Benet LZ. Predicting drug disposition via application of BCS: transport/absorption/ elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm res. 2005;22:11–23.
Oberle RL, Amidon GL. The influence of variable gastric emptying and intestinal transit rates on the plasma level curve of cimetidine; an explanation for the double peak phenomenon. J Pharmacokinet Biopharm. 1987;15:529–44.
Inada T, Asai T, Yamada M, Shingu K. Propofol and midazolam inhibit gastric emptying and gastrointestinal transit in mice. Anesth Analg. 2004;99:1102–6.
De Bie ATH, Van Ommen B, Bär A. Disposition of [14C]γ-Cyclodextrin in germ-free and conventional rats. Regul Toxicol Pharmacol. 1998;27:150–8.
Stella V. Mechanisms of drug release from cyclodextrin complexes. Adv Drug Deliv rev. 1999;36:3–16.
Koopmans R, Dingemanse J, Danhof M, Horsten GP, van Boxtel CJ. Pharmacokinetic-pharmacodynamic modeling of midazolam effects on the human central nervous system. Clin Pharmacol Ther. 1988;44:14–22.
Allonen H, Ziegler G, Klotz U. Midazolam kinetics. Clin Pharmacol Ther. 1981;30:653–61.
Brill MJE, van Rongen A, Houwink API, Burggraaf J, van Ramshorst B, Wiezer RJ, et al. Midazolam pharmacokinetics in morbidly obese patients following semi-simultaneous oral and intravenous administration: a comparison with healthy volunteers. Clin Pharmacokinet. 2014;53:931–41.
Greenblatt DJ, Abernethy DR, Locniskar A, Harmatz JS, Limjuco RA, Shader RI. Effect of age, gender, and obesity on midazolam kinetics. Anesthesiology [internet]. 1984;61:27–35. Available from. http://www.ncbi.nlm.nih.gov/pubmed/6742481
Heizmann P, Eckert M, Ziegler WH. Pharmacokinetics and bioavailability of midazolam in man. Br. J. Clin. Pharmacol. 1983;16 Suppl 1:43S–49S.
Hohmann N, Kocheise F, Carls A, Burhenne J, Haefeli WE, Mikus G. Midazolam microdose to determine systemic and pre-systemic metabolic CYP3A activity in humans. Br J Clin Pharmacol. 2015;79:278–85.
Lee J-I, Chaves-Gnecco D, Amico JA, Kroboth PD, Wilson JW, Frye RF. Application of semisimultaneous midazolam administration for hepatic and intestinal cytochrome P450 3A phenotyping. Clin Pharmacol Ther. 2002;72:718–28.
Mandema JW, Tuk B, Steveninck AL van, Breimer DD, Cohen AF, Danhof M. Pharmacokinetic-pharmacodynamic modeling of the central nervous system effects of midazolam and its main metabolite alpha-hydroxymidazolam in healthy volunteers. Clin Pharmacol Ther 1992;51:715–728.
Smith MT, Eadie MJ, Brophy TO. The pharmacokinetics of midazolam in man. Eur J Clin Pharmacol. 1981;19:271–8.
Tsunoda SM, Velez RL, von Moltke LL, Greenblatt DJ. Differentiation of intestinal and hepatic cytochrome P450 3A activity with use of midazolam as an in vivo probe: effect of ketoconazole. Clin Pharmacol Ther. 1999;66:461–71.
ACKNOWLEDGEMENTS AND DISCLOSURES
Advicenne Pharma financed this study. Dr. Fauchoux provided and cared for study subjects and collected data and Dr. Patat provided scientific advice for study conduct.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guittet, C., Manso, M., Burton, I. et al. A Two-way Randomized Cross-over Pharmacokinetic and Pharmacodynamic Study of an Innovative Oral Solution of Midazolam (ADV6209). Pharm Res 34, 1840–1848 (2017). https://doi.org/10.1007/s11095-017-2193-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2193-4




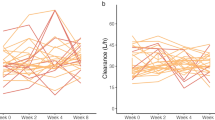




 ) and oral values with ADV6209 formulation (
) and oral values with ADV6209 formulation ( )
)