Abstract
Purpose
In vitro lipid digestion models are commonly used to screen lipid-based formulations (LBF), but in vitro-in vivo correlations are in some cases unsuccessful. Here we enhance the scope of the lipid digestion test by incorporating an absorption ‘sink’ into the experimental model.
Methods
An in vitro model of lipid digestion was coupled directly to a single pass in situ intestinal perfusion experiment in an anaesthetised rat. The model allowed simultaneous real-time analysis of the digestion and absorption of LBFs of fenofibrate and was employed to evaluate the influence of formulation digestion, supersaturation and precipitation on drug absorption.
Results
Formulations containing higher quantities of co-solvent and surfactant resulted in higher supersaturation and more rapid drug precipitation in vitro when compared to those containing higher quantities of lipid. In contrast, when the same formulations were examined using the coupled in vitro lipid digestion – in vivo absorption model, drug flux into the mesenteric vein was similar regardless of in vitro formulation performance.
Conclusion
For some drugs, simple in vitro lipid digestion models may underestimate the potential for absorption from LBFs. Consistent with recent in vivo studies, drug absorption for rapidly absorbed drugs such as fenofibrate may occur even when drug precipitation is apparent during in vitro digestion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rate of passive drug absorption across the small intestine can be approximated using Fick’s Law. Under conditions of Fickian diffusion, the rate of absorptive drug flux is the product of drug permeability across the membrane and the drug concentration at the intestinal membrane surface. Thus, for a drug with fixed permeability, increasing drug concentration increases membrane flux and the maximal rate of flux is capped by drug solubility. Low drug solubility and dissolution in gastrointestinal (GI) fluids is therefore a potential limitation to effective drug absorption as it prevents the attainment of the high drug concentrations required to achieve maximal drug flux across the intestinal wall (1, 2).
In spite of this, there are an increasing number of drug candidates that exhibit low aqueous solubility, and where low solubility is a potential limitation to absorption. To address the limitation of low drug solubility, a range of formulation strategies (e.g., solid dispersions, cyclodextrins and salts) have been developed to enhance apparent solubility in the GI tract and to improve oral absorption (3). Lipid-based formulations (LBFs) provide one such approach to overcoming absorption limitations for poorly water-soluble drugs (PWSDs) (4, 5). LBFs promote absorption by presenting the drug to the GI tract in a solubilised form (thus removing the limitation to absorption presented by slow dissolution), increasing the solubilisation capacity of the GI fluids, and, in many cases, generating transiently supersaturated drug concentrations (5–8).
While a number of successful products have utilised LBFs for low solubility, wider application of this technology is limited by the lack of robust in vitro methods that can predict the extent by which LBF enhance drug absorption. As such, formulation efforts are driven, in large part, by the outcomes of in vivo preclinical testing (5, 9).
To assist understanding of the wide range of possible LBFs, Pouton proposed a Lipid Formulation Classification System (LFCS) (10, 11) in which formulations were assigned to one of four groups based on excipient composition. The LFCS allowed for the categorisation of LBFs via excipient composition, particle size and the likely significance of aqueous dilution and digestion on drug solubilisation and potentially, therefore, absorption within the small intestine.
Realising the importance of lipid digestion on the behaviour of LBFs in vivo, in vitro lipid digestion models have increasingly been employed to predict the likely impact of digestion by pancreatic enzymes and dispersion in bile fluids on formulation performance (12–16). These studies have been successful in highlighting the profound changes that are catalysed by lipid dispersion and digestion and have significantly improved our understanding of drug fate in LBFs within the GI tract. Correlations between drug solubilisation profiles during in vitro digestion and oral bioavailability have also been shown in a number of studies (6, 8, 17–19).
However, whilst the in vitro digestion model provides one means of assessing the likelihood of drug precipitation, it is a closed system, and does not fully represent conditions in vivo. Notably, it lacks the absorption sink that is present in vivo, and may therefore overestimate precipitation potential (20–22). Thus, where absorption is rapid, drug concentrations in the intestinal lumen may drop sufficiently rapidly that precipitation is avoided, even under conditions of significant initial supersaturation (23).
The work described herein was undertaken to explore a means by which an appropriate absorption sink could be added to the current in vitro digestion model. Previous studies have attempted to address this issue by (i) predigesting LBFs using the in vitro digestion model and then adding the digest to the acceptor chamber of a permeability model employing a cultured cell monolayer (24), (ii) assembling model micellar and vesicular systems designed to represent the digestion products formed from LBFs, and then perfusing these materials through a rat jejunum intestinal segment (25), or (iii) employing modelling approaches to simulate LBF digestion and supersaturation within an absorptive environment (26). These studies provide useful information as to the impact of formulation digestion on drug absorption, but do not relate in real time the rapid kinetic changes to formulation properties and drug solubilisation and saturation that occur during digestion, to drug flux across the absorptive membrane. The current model was developed to incorporate a means to accurately monitor lipid digestion in vitro and to simultaneously assess lipid/drug absorption in vivo. This allows for real time observations of formulation digestion and drug absorption. The advantage of this approach is that it provides a direct read-out of the impact of rapid changes to solubilisation (and supersaturation) on drug flux, using an absorption sink that is resistant to bile salt and has appropriately high surface area (unlike many cell culture systems).
Fenofibrate was employed as the model drug due to its low water-solubility and widespread use as a model BCS Class II drug in studies of oral absorption enhancement, in particular using LBFs (14, 21, 22, 27). Fenofibrate has a low aqueous solubility of less than 0.5 mcg/mL (28), is highly lipophilic (log P = 5.24) and is uncharged at physiological pH (29). Fenofibrate is also highly lipid-soluble (e.g., solubility in soybean oil is 79.9 mg/g (30)) allowing formulations with high drug loads and that are able to promote significant supersaturation on formulation dispersion and digestion.
Materials and Methods
Materials
Fenofibrate (2-[4-(4-chlorobenzoyl)phenoxy]-2-methylpropanoic acid isopropyl ester), fenofibric acid and meclofenamic acid were obtained from Sigma-Aldrich (St. Louis, MO). Captex® 300, a medium-chain triglyceride and Capmul® MCM, a blend of partially digested medium-chain glycerides, were donated by Abitec Corporation (Columbus, OH). Kolliphor® EL (polyoxyl 35 hydrogenated castor oil) was donated by BASF Corporation (Washington, NJ). Transcutol® HP (diethylene glycol monoethyl ether) was supplied by Gattefossé (St. Priest, France). Sodium taurodeoxycholate 95% (NaTDC), 4-bromophenylboronic acid (4-BPB) and porcine pancreatin extract (P7545, 8 x USP specifications activity) were all obtained from Sigma-Aldrich (St. Louis, MO). Phosphatidylcholine ((PC) Lipoid E PC S, approximately 99.2% pure, lecithin from egg) was obtained from Lipoid (Lipoid GmbH, Ludwigshafen, Germany). 1 M sodium hydroxide (NaOH), which was diluted to obtain 0.6 M NaOH titration solution, was purchased from Merck (Darmstadt, Germany). Water was obtained from a Milli-Q water purification system (Millipore, Bedford, MA). All other chemicals and solvents were of analytical purity or high performance liquid chromatography (HPLC) grade. Hypergrade solvents were used for UPLC-MS/MS analysis.
Fenofibrate Lipid-Based Formulations
Formulations were constructed, using the LFCS as a guide, to illustrate differences in in vitro formulation performance. Formulations were assembled such that they covered Type IIIA, Type IIIB and Type IV formulations as defined by LFCS as these are more commonly employed than e.g., Type I or Type II formulations. For comparison, an aqueous suspension formulation of fenofibrate was also prepared by suspending crystalline fenofibrate in digestion buffer (composition described in the in vitro digestion model section). Details of the composition of the formulations are given in Table I.
Formulation Preparation
Drug-free lipid formulations were prepared by weighing the various components (see Table I) directly into clean screw-capped glass vials. Vials were sealed, vortex-mixed and stored at 37°C for at least 24 h to ensure homogeneity.
Fenofibrate was incorporated into LBFs at a constant drug loading (60 mg/g). This loading was chosen to represent ~40% of saturated solubility in the formulations and to provide a loading that led to appropriate differences in in vitro behaviour based on the in vitro digestion test. The required mass of fenofibrate was weighed directly into clean screw-capped glass vials and drug-free lipid formulation was added up to the target mass loading. Vials were sealed, vortex-mixed and stored at 37°C to equilibrate overnight prior to testing. Drug solubility in each of the formulations was assessed using standard methodologies as previously described, and all experiments were performed in triplicate (31). Solubility was defined as the value attained when at least three consecutive solubility sample values varied by less than 5%. For fenofibrate, this was typically achieved between 24 and 48 h.
In Vitro Digestion Model
Drug Solubilisation During LBF Dispersion and Digestion
In vitro digestion experiments were undertaken using previously reported conditions and equipment, with some modifications (12–14). The experimental set-up consisted of a PHM290 MeterLab pH stat titration unit (Radiometer, Copenhagen, Denmark) and a thermostatically controlled jacketed glass reaction vessel (Metrohm AG, Herisau, Switzerland) that was used to keep the LBFs and digestion medium at a constant temperature (37°C). The contents within the vessel were mixed continuously using a magnetically stirred cylindrical rod, and the pH of the digestion media was monitored using a combined pH Ag/AgCl electrode (Radiometer), coupled to a 10 mL ABU901 autoburette (Radiometer). The in vitro digestion apparatus is depicted as the glass reaction vessel in Fig. 1.
The lipid-based formulation (1.1 g) was dispersed in 40 mL of digestion buffer, comprising 2 mM Tris-maleate, 1.4 mM CaCl2·2H20 and 150 mM NaCl, adjusted to pH 6.5, supplemented with 3 mM NaTDC and 0.75 mM PC.
During a 15 min dispersion phase the formulation was dispersed within the digestion medium and the pH manually adjusted to 6.5 using small volumes of NaOH or HCl solution where needed. Samples (1 mL) were removed after 5, 10 and 15 min dispersion and promptly centrifuged (6708 g, MiniSpin, Eppendorf AG, Hamburg, Germany) for 10 min to separate any drug precipitate from the aqueous solution. Samples (100 μL) from the post-centrifugation aqueous phase were diluted 10–100 fold with acetonitrile, prior to further centrifugation (10 min, 21,100 g, 20°C, Fresco 21 Heraeus, Thermo Scientific, Osterode, Germany) and analysis for fenofibrate content by HPLC, as described below.
After the 15 min dispersion phase, digestion was initiated by addition of 4 mL of pancreatin extract containing pancreatic lipase and other pancreatic enzymes. The pancreatin extract was freshly prepared prior to each in vitro digestion experiment by mixing 1 g of pancreatin powder with 5 mL digestion buffer and ~20 μL of 5.0 M NaOH solution to establish the target pH 6.5. The enzyme suspension was centrifuged (2880 g, 5°C, Eppendorf 5804R, Hamburg, Germany) for 10 min. Four millilitre pancreatin extract contained ~40,000 tributyrin units (TBU) (1000 TBU per mL of digest). The duration of the digestion experiment was 60 min and during this period the pH of the digest was continuously monitored and maintained at 6.5 by the pH-stat titration unit (Radiometer). The pH stat automatically added 0.6 M NaOH to the digestion vessel in response to decreasing pH in order to maintain the set point at pH 6.5. Samples (1 mL) were taken throughout the digestion phase (t = 5 min intervals over 60 min). Samples taken during digestion were inhibited by the addition of 5 μl of 1.0 M 4-BPB (in methanol) and processed as described for dispersion samples, prior to analysis for fenofibrate content by HPLC.
Determination of Drug Solubility in the Aqueous Pre-Digestion Phase
The solubility of crystalline fenofibrate in dispersed blank drug free LBFs was evaluated to allow estimation of drug supersaturation during formulation dispersion. Triplicate samples of the aqueous phase were removed after 10 min dispersion of drug-free LBFs. Excess crystalline fenofibrate was added and the samples were incubated at 37°C. Samples were taken at 1 h time intervals, centrifuged (21,000 g, Heraeus Fresco 21) at 37°C for 10 min and fenofibrate concentration determined by HPLC. Equilibrium solubility was defined as the mean solubility value across the three consecutive incubation sample time points and varied less than 5%.
Determination of Drug Solubility in Aqueous Post-Digestion Phase
The solubility of crystalline fenofibrate in the aqueous phase generated post digestion of blank LBFs was evaluated after 5, 15, 30 and 60 min digestion to allow estimation of drug supersaturation during formulation digestion. Digestion conditions for the blank drug free formulations were as described above, and samples were centrifuged and the aqueous phase removed to enable determination of drug solubility in triplicate. Crystalline fenofibrate was added in excess to the LBF digestion media and incubated at 37°C. At each time point samples were centrifuged at 37°C for 10 min (21,000 g, Heraeus Fresco 21). As with previous studies from our laboratory (8), a decrease in drug solubility was seen over 24 h for many of the formulations. The apparent solubility of fenofibrate in the aqueous post-digestion phases was defined as the mean solubility value obtained over at least two time points, where the change in solubility was less than 5% (usually 2–3 h incubation).
Assessment of Supersaturation
The ability for the LBF to initiate and maintain supersaturation during dispersion and digestion was expressed using the supersaturation ratio (SR) calculated using Eq. 1. SR values were determined from the solubilised fenofibrate concentrations obtained from the dispersion and digestion samples at each time point divided by the apparent drug solubility in the aqueous phase pre- and post-digestion of drug free LBF at the same time point.
Supersaturation ratio values were then plotted against dispersion and digestion time to provide an indication of changes to thermodynamic activity of the drug during dispersion and digestion. To capture the extent of supersaturation of each LBF across the digestion testing period, the area under the supersaturation-time curve (AUC) for each individual LBF between 0 and 60 min was calculated using the trapezoidal rule.
HPLC Quantification of Fenofibrate in Formulations and In Vitro Digestion Samples
Fenofibrate HPLC analyses were conducted using a Waters Alliance 2695 Separation Module and a Waters 486 tuneable Absorbance Detector, (Waters Alliance Instruments, Milford, MA). A reverse phase C18 column (3.9 × 150 mm, Waters Symmetry) was maintained at room temperature and mobile phase (80% (v/v) acetonitrile: 20% Milli-Q water plus 0.1% (v/v) formic acid) was pumped at a flow rate of 1 mL/ min. UV detection of fenofibrate was at 286 nm. The injection volume was 50 μL. The assay was validated by analysis of n = 5 quality control (QC) samples at three different concentrations on three separate days. The QC standards were prepared at low (1 mcg/mL), medium (12.5 mcg/mL) and high (50 mcg/mL) concentrations. Intra-assay variability was accurate to 95.6, 99.9 and 98.2% and precise to ± 1.4, 1.9 and 1.7% of 1.0, 12.5 and 50.0 mcg/mL. Inter-assay variability was assessed over three separate days and was accurate to 99.4, 100.6 and 97.4% and precise to ±1.76, 1.44 and 1.56% at 1.0, 12.5 and 50 μg/mL.
Solid-State Analysis of Precipitated Material (Pellet Phase) Using Polarized Light Microscopy
Selected digestion pellets from the Type IV0:50:50 LBF, containing precipitated fenofibrate, were carefully removed from the polypropylene centrifuge tubes, transferred onto a microscope slide and analysed using a Zeiss Axiolab microscope (Carl Zeiss, Oberkochen, Germany) equipped with crossed polarising filters. Images were recorded using a Canon PowerShot A70 digital camera (Tokyo, Japan). Pellets were analysed within 3 h of sampling to minimise any changes in drug solid state properties due to storage.
Single Pass Rat Jejunum Intestinal Perfusion
Animals
All animal studies were performed in accordance with the Australian and New Zealand Council for the Care of Animals on Research and Teaching guidelines and approved by the institutional animal experimentation ethics committee (Monash Institute of Pharmaceutical Science – Monash University).
Male Sprague–Dawley rats weighing 300–330 g were fasted overnight (12–18 h) prior to surgery and were anaesthetised by subcutaneous injection (1.0 mL/kg) of anaesthetic cocktail I (37.3 mg/mL ketamine, 9.8 mg/mL xylazine, 0.4 mg/mL acepromazine in saline) with subsequent doses (0.44 mL/kg) of cocktail II (90.0 mg/mL ketamine, 0.9 mg/mL acepromazine in saline) every hour thereafter (32). The rats were maintained under general anaesthesia for the duration of the experiment. At the end of all experiments, rats were euthanized via an intravenous or intracardiac injection of sodium pentobarbitone (100 mg).
Surgical Procedures
A midline incision was made in the abdomen to expose the small intestine. Two small incisions were made by electro cautery approximately 10 cm apart in the jejunum and cannulated with elbow tube polypropylene fittings. The segment was flushed with saline to remove intestinal contents. The mesenteric vein draining the isolated region of the jejunum was exposed by blunt dissection and cannulated to allow for the determination of the mass of drug absorbed (Fig. 1). The externalised jejunum section was kept moist and maintained at 37°C throughout the experiment using a heated pad and a heated light source and experiments were performed in a perfusion cabinet. To maintain a consistent blood supply, donor blood was infused throughout the experiment via a cannula in the jugular vein. To facilitate this the jugular vein was cannulated as previously described (32).
Assessment of Absorptive Flux Using the In Vitro Lipid Digestion – In Vivo Absorption Model
Animals were allowed to equilibrate after surgery for 30 min. During this time, heparinized donor rat blood (5 Units/mL) was infused via the right jugular vein at a rate of 0.3 mL/min using an infusion pump (Pump 11, Harvard Apparatus, Holliston, MA). During the initial 30 min equilibration period, blood from the cannulated mesenteric vein was continuously collected for reinfusion. Fresh heparinised donor blood was also collected by cardiac puncture from donor rats under isoflurane anaesthesia. Saline at 37°C was pumped through the jejunum segment during the equilibration period, and outflowing perfusate was directed to waste.
The contents of the in vitro digestion vessel, including drug, digesting LBF, digestion media and pancreatic enzyme were pumped through the jejunum using a peristaltic pump (Pump P-1, Pharmacia Biotech, Amersham Biosciences, Piscataway, NJ) (Fig. 1). Prior to initiating the digest infusion, the LBF was dispersed for 15 min. After this dispersion, digestion was initiated by addition of pancreatic enzyme (as described in detail above) and simultaneously the inlet tubing for the rat jejunum perfusion was switched from saline to the in vitro digestion vessel. The flow rate of LBF digestion medium through the jejunum was set to 0.4 mL/min, to enable the contents of the in vitro digestion model to reach the jejunum segment shortly after initiation of digestion (<2 min).
Samples (0.5 mL) were taken from the thermostat-jacketed glass reaction vessel (as described above) to enable the measurement of fenofibrate drug concentrations during dispersion and digestion. Samples were also taken from the tubing post-jejunum to enable measurement of fenofibrate drug concentrations in the digestion medium following passage through the jejunum. Samples were processed and analysed by HPLC as above. Blood from the cannulated mesenteric vein was collected over 5 min intervals into 1.5 mL polypropylene tubes. The volume of blood collected was determined by weighing the collection tubes before and after mesenteric blood collection. Plasma was separated from whole blood by centrifugation (6708 g, MiniSpin) for 5 min, and stored at −80°C until sample analysis.
Where the aqueous suspension formulation of fenofibrate was perfused into the jejunum segment, the peristaltic pump was unable to transfer the suspension effectively and homogenously. To overcome this difficultly the ‘in vitro digestion’ of the suspension (i.e., in digestion buffer under identical conditions to the LBFs) was therefore run to completion (60 min, to allow for complete digestion of PC in the digestion buffer) and the contents transferred from the digestion vessel to a 30 mL syringe. The contents of the syringe were then manually perfused through the jejunum at the same flow rate as the peristaltic pump (0.4 mL/min).
Validation of Jejunum Membrane Integrity in Absorption Model
To validate the integrity of the jejunum membrane during perfusion of in vitro digestion media containing lipid digestion products and bile acids, radiolabelled permeability markers for passive transcellular (antipyrine) and paracellular (mannitol) transport routes were employed. The apparent permeability coefficients of antipyrine (3.12 × 10−5 cm/s) and mannitol (1.25 × 10−6 cm/s) were consistent with previously reported data (33–35), providing confidence that the perfusate has no deleterious effects on membrane integrity over the period of the experiment.
Quantification of Fenofibric Acid in Plasma from In Situ Perfusion Experiments by UPLC-MS/MS
Plasma Sample Preparation
Calibration standards for fenofibric acid were prepared by spiking 100 μL aliquots of blank rat plasma with 10 μL ACN solution containing 1–150 μg/mL fenofibric acid. This provided plasma standards in the concentration range of 40–5000 ng/mL fenofibric acid. Meclofenamic acid (150 μg/mL in ACN) was used as an internal standard (IS), where 10 μL was added to each 100 μL plasma sample or standard. The tubes were vortexed, and 180 μL ACN was added (an additional 10 μL ACN was added to unknown plasma samples to give a total 300 μL volume). The tubes were vortexed again and centrifuged for 10 min at 21,100 g (20°C, Fresco 21 Heraeus). The supernatant was removed and centrifuged again and the supernatant was transferred into autosampler vials to be injected onto the LC-MS/MS. Unknown concentrations were determined by comparison to the calibration standards.
UPLC-MS/MS Conditions for Fenofibric Acid Quantification
Analysis of fenofibric acid in plasma was conducted using a LCMS-8030 triple quadruple mass spectrometer (Shimadzu, Kyoto, Japan), including a LC-20AD binary pump, a SiL-30AC refrigerated autosampler, a mobile phase vacuum degassing unit (DGU-20A5), and a temperature-controlled column compartment (CTO-20A), coupled to a triple quadruple mass spectrometric (MS) detector equipped with an electrospray ionization source. The autosampler was maintained at 4°C and the column was heated to 40°C. A Phenomenex Kintex C18 column (50 × 2.1 mm, 2.6 μm, Torrance, CA) was used for chromatographic separation. Samples were eluted using gradient elution at a flow rate of 0.25 mL/min. Mobile phase A was Milli-Q water plus 0.1% (v/v) formic acid. Mobile phase B was acetonitrile. The initial percentage of mobile phase B was 50% and increased to 95% over 3.7 min where it was held at 95% for 1.2 min. After 4.9 min solvent B decreased to 30% over 0.5 min and returned to 50% by the end of the 6.4 min run time to re-establish equilibrium.
The MS conditions were as follows: drying gas flow, 3 L/min; nebulizing gas flow, 1 L/min; drying gas temperature, 300°C; heat block temperature, 200°C and CID gas, 230 kPa. Selected-ion monitoring was accomplished at m/z 317.05 > 231.00 for fenofibric acid and m/z 296.00 > 242.95 for the internal standard meclofenamic acid. The first quadruple (Q1) and third quadruple (Q3) of the mass spectrometer were set at 15 and 26 V, respectively. The collision energy was 12 V. The chromatographic data were acquired using the LabSolutions LCMS Version 5.4 software package for LCMS-8030. Calibration curves and regression parameters were calculated by least-squares linear regression analysis using a weighting factor of 1/concentration2.
The assay was validated by analysis of n = 4 spiked plasma QC standards on three separate days. The QC standards were prepared at low (40 ng/mL), medium (312.5 ng/mL) and high (5000 ng/mL) concentrations. Intra-assay variability was accurate to 102.1, 101.6 and 97.6% and precise to ± 2.0, 4.9 and 2.7% of 40, 312.5 and 5000 ng/mL, respectively. Inter-assay variability was assessed over three separate days and was accurate to 107.5, 108.0 and 91.3% and precise to ±11.4, 5.7 and 3.8% at 40, 312.5 and 5000 ng/mL.
Blood: Plasma Ratio Determination of Fenofibric Acid
The blood:plasma ratio for fenofibric acid was determined by spiking 0.5 mL of whole blank blood and blank plasma with known amounts of fenofibric acid to achieve low (50 ng/mL), medium (200 ng/mL) and high (2000 ng/mL) concentrations. Whole blank blood was centrifuged as above and plasma separated. Protein precipitation was achieved in the same manner as that used for plasma from mesenteric blood collected during the in situ perfusion experiments. Drug concentration was assayed by LC-MS/MS as above. Blank plasma samples spiked with known amounts of fenofibric acid were subsequently processed in the same manner. The blood:plasma ratio was calculated from the ratio of the concentration of drug measured in spiked plasma to the drug concentration measured in plasma separated from spiked whole blood. The blood:plasma ratio for fenofibric acid was 0.67 ± 0.04 (mean ± SD, n = 9). The mean blood:plasma ratio was subsequently used to convert plasma concentrations to blood concentrations in mesenteric blood, enabling quantification of total fenofibric acid transport into mesenteric blood.
Statistical Analysis
Statistically significant differences were assessed using one-way ANOVA with Tukey post-test for multiple comparisons at a significance level of α = 0.05. All statistical analysis was performed using GraphPad Prism version 6.05 for Windows (GraphPad Software, La Jolla, CA).
Results
In Vitro Evaluation of Lipid-Based Formulation Performance
Fenofibrate Solubility in Formulations
The equilibrium solubility of fenofibrate in the three formulations examined was similar (Fig. 2). The LBFs employed for the in vitro lipid digestion – in vivo absorption experiments contained fenofibrate at a constant drug load (60 mg/g). The fenofibrate saturation levels in the formulations therefore varied slightly and are annotated as percentages in Fig. 2.
Fenofibrate Solubilisation During Formulation Dispersion and Digestion
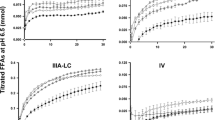
During in vitro dispersion and digestion experiments, the concentrations of fenofibrate solubilised in the aqueous phase of the in vitro digestion were determined every 5 min (Fig. 3). Samples were removed either directly from the digestion vessel or after perfusion through the jejunum. The equilibrium solubility of fenofibrate in the dispersed and digested aqueous phase was also measured and is shown as the dotted line in Fig. 3.
Drug solubilisation profiles of fenofibrate (60 mg/g drug loading) pre- (filled symbols) and post- (open symbols) perfusion of the jejunum during dispersion and digestion of the three LBFs [mean ± SD (n = 3)]. Greyed panel represents the dispersion stage. The dotted line indicates fenofibrate solubility in the aqueous colloidal phase produced by dispersion and digestion of drug free LBF.
Solubilised fenofibrate concentrations in the aqueous phase post-jejunum were lower than drug concentrations in the digestion vessel, most likely due to absorption of drug. Total drug concentrations (solubilised plus precipitated), however, were similar suggesting that the vessel contents (including suspended drug) were successfully transported through the model via the peristaltic pump.
For the Type IIIA60:40:0 formulation, fenofibrate was maintained in a solubilised state during dispersion and for a period of up to 15–20 min during digestion. After approximately 20 min, precipitation occurred and the solubilised drug concentration dropped toward the apparent drug solubility in the aqueous post-digest phase. In contrast to the concentrations of solubilised drug measured during the kinetic in vitro digestion experiment, apparent drug solubility in the digesting formulation (depicted by the dotted line) dropped almost instantly at t = 0. As such the solubilised drug concentrations were supersaturated for ~15–20 min post-digestion.
For the Type IIIB20:60:20 formulation, a similar solubilisation profile was observed although drug was maintained in a stable supersaturated state for slightly less time (~15 min) before precipitation was initiated and drug concentrations dropped to levels similar to the apparent drug solubility at ~30 min.
The Type IV0:50:50 formulation was unable to maintain fenofibrate in a solubilised state for any significant period of time during the in vitro test, and the solubilised concentration dropped rapidly on formulation dispersion. In this case, little difference was seen in equilibrium drug solubility in the colloids formed on dispersion and digestion of the formulation. The lack of impact of digestion most likely reflects the lack of glyceride lipid in the formulation and the lower digestibility of the surfactant and co-solvent contained in the Type IV formulation. Characterisation of the precipitate formed on dispersion and digestion of the Type IV formulation, using polarised light microscopy, confirmed the presence of crystalline fenofibrate (see Fig. 4).
Solubilised fenofibrate concentrations could not be determined by HPLC analysis after introduction of the aqueous suspension formulation into the digestion vessel, suggesting that the concentration of solubilised fenofibrate was less than 1 mcg/mL throughout the experiment. Total fenofibrate concentrations (i.e., solubilised plus suspended) were also measured in the digestion media and were essentially unchanged throughout the in vitro digestion test.
The differences in fenofibrate solubilisation on dispersion and digestion of the three LBFs examined are shown in Fig. 5a and suggest the potential for discrimination of in vivo formulation performance based on solubilisation. The area under the solubilised fenofibrate drug concentration versus time profile for each LBF is given in Fig. 5b, providing an overall rank in exposure to solubilised drug (Type IIIA > Type IIIB > Type IV).
In vitro evaluation (drug solubilisation and supersaturation) of the three LBFs incorporating fenofibrate at 60 mg/g drug loading (Type IIIA  , Type IIIB
, Type IIIB  , Type IV
, Type IV  ) during digestion and dispersion testing [mean ± SD (n = 3–4)]. Panel (a): Overlaid drug solubilisation profiles (mg/mL) for the three LBFs during in vitro dispersion and digestion. The grey panel represents the dispersion stage. Panel (b): Calculated AUC of solubilised drug concentration over time (from Panel a) during the digestion stage (time = 0–60 min) for each LBF. Panel (c): Supersaturation ratios (calculated using Eq. 1 from solubilised drug and apparent drug solubility data) vs. dispersion and digestion time. The dispersion stage is depicted by the grey panel. Panel (d): Overall thermodynamic activity of drug during digestion of each LBF (calculated using the AUC of the supersaturation ratio versus time figure in Panel c). * Statistically significant difference (p < 0.05).
) during digestion and dispersion testing [mean ± SD (n = 3–4)]. Panel (a): Overlaid drug solubilisation profiles (mg/mL) for the three LBFs during in vitro dispersion and digestion. The grey panel represents the dispersion stage. Panel (b): Calculated AUC of solubilised drug concentration over time (from Panel a) during the digestion stage (time = 0–60 min) for each LBF. Panel (c): Supersaturation ratios (calculated using Eq. 1 from solubilised drug and apparent drug solubility data) vs. dispersion and digestion time. The dispersion stage is depicted by the grey panel. Panel (d): Overall thermodynamic activity of drug during digestion of each LBF (calculated using the AUC of the supersaturation ratio versus time figure in Panel c). * Statistically significant difference (p < 0.05).
Supersaturation ratios at each 5 min time point were also calculated using Eq. 1. These ratios are plotted against dispersion and digestion time in Fig. 5c to provide an indication of the thermodynamic activity of drug during dispersion and digestion of each formulation. In a similar manner to the analysis undertaken to quantify overall exposure to solubilised drug, the area under the curve (AUC) for drug supersaturation ratios over time was also calculated (Fig. 5d). The Type IIIA and Type IIIB LBFs had similar supersaturation ratio AUC values, whereas the supersaturation ratio AUC for the Type IV formulation was lower over the 60 min post digestion period.
Coupled In Vitro Lipid Digestion – In Vivo Absorption Evaluation
Fenofibrate is a prodrug and is metabolised to fenofibric acid in vivo by non-specific esterases in the tissue and plasma (36–38). After oral administration, hydrolysis to fenofibric acid is sufficiently rapid that only fenofibric acid can be identified in the systemic circulation (39). Consistent with these previous data, in the current studies, fenofibrate could not be detected in the mesenteric blood (data not shown). Fenofibric acid concentrations in mesenteric blood were therefore used to quantify fenofibrate absorption.
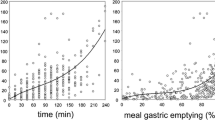
In many single pass intestinal perfusion protocols, the rate of disappearance from the luminal perfusate is used to estimate drug permeability. However, this approach assumes that steady state flux is reached during perfusion. In the current experiments where the solubilised drug concentrations were deliberately allowed to change over time in order to better reflect events stimulated by digestion, the calculation of a permeability co-efficient is not possible. Instead drug flux into the mesenteric vein was measured directly and compared to drug solubilisation in the perfusate.
Fenofibric Acid Drug Flux into Mesenteric Vein
Fenofibric acid flux into the mesenteric blood after perfusion of the digesting LBFs is shown in Fig. 6. In spite of the differences seen in drug solubilisation and supersaturation during the in vitro digestion (Fig. 5a), in the presence of the absorption sink, fenofibric acid drug flux was similar regardless of the LBF employed. A notable increase in fenofibric acid drug flux was, however, seen from the LBFs when compared to the aqueous suspension formulation of crystalline fenofibrate.
Fenofibric acid drug flux assessment from the in vitro lipid digestion – in vivo absorption model of the three LBFs incorporating fenofibrate at 60 mg/g drug loading (Type IIIA  , Type IIIB
, Type IIIB  , Type IV
, Type IV  ) and crystalline fenofibrate suspension (
) and crystalline fenofibrate suspension ( ) [mean ± SEM (n = 3–4)]. Panel (a): Overlaid fenofibric acid drug flux appearance into the mesenteric vein profiles (mcg/5 min/ 10 cm2) from the three digesting LBFs loaded with fenofibrate and crystalline fenofibrate aqueous suspension. Panel (b): Calculated AUC of fenofibric acid flux over time (from Panel a) during perfusion (time = 5–60 min) for each LBF and suspension.
) [mean ± SEM (n = 3–4)]. Panel (a): Overlaid fenofibric acid drug flux appearance into the mesenteric vein profiles (mcg/5 min/ 10 cm2) from the three digesting LBFs loaded with fenofibrate and crystalline fenofibrate aqueous suspension. Panel (b): Calculated AUC of fenofibric acid flux over time (from Panel a) during perfusion (time = 5–60 min) for each LBF and suspension.
Discussion
The current study aimed to develop a unique model for evaluating drug absorption from digestible LBFs, and to use the model to better understand the influence of formulation digestion, drug solublisation, supersaturation and precipitation on the rate and extent of drug absorption from LBFs. The data suggest, at least for the PWSD fenofibrate, that efficient drug flux across the absorptive membrane may be achievable, even when drug solubilisation is not maintained at ‘maximal’ levels for extended periods during formulation dispersion and digestion.
The lack of an absorption sink has been acknowledged as a limitation of in vitro dissolution tests for many years. This limitation is also apparent for in vitro digestion testing protocols for LBFs, where differences in formulation performance are typically ascribed to differences in drug solubilisation during formulation dispersion and digestion. In contrast to closed in vitro dissolution or digestion models, the presence of a high surface area absorption sink in the small intestine is likely to reduce solubilised drug concentrations, lowering the drivers of drug supersaturation and precipitation. Several attempts have therefore been made to develop models where dissolution (or solubilisation during lipid digestion) can be assessed in the presence of an absorption sink. These include simple systems where an immiscible oil layer is overlaid over the dissolution fluid (40–42) through to highly complex model intestinal systems such as the TNO Simulated Gastro-intestinal Tract (TIM-1) from TNO Nutrition and Food Research (Zeist, The Netherlands) (43). Immiscible oil layers are of limited use during studies conducted in the presence of bile acids since the oil layer becomes emulsified and partitioning of bile acids into the oil layer is likely to alter the structure of the solubilised species. Complex models such as the TIM-1 can be impractical since the resources required may be beyond that of most research groups. Focus has therefore been directed towards relatively simple models where lipid digestion models are used in sequence with in vitro permeability models (24). Dissolution models coupled to Caco-2 cell permeability models have been employed to good effect to explore drug absorption from traditional formulations (44–46), but the sensitivity of the Caco-2 monolayer to high concentrations of bile salts and fatty acids makes them less easily applied to digesting LBFs. A further limitation is the very limited surface area that can be created in a typical in vitro permeability system, when compared to the complex architecture of the small intestine.
In the current studies we chose to couple the in vitro lipid-digestion model directly to an in situ permeability model in an intact rat. The model was chosen since it overcomes the issues of tolerability to bile and lipid concentrations and presents a high surface area with an intact intestinal microclimate (47). Cannulation of the mesenteric vein also enabled direct assessment of drug transport into the blood (48). The complexity of the experimental model employed dictates that it is not suitable as a screening tool. Rather, it was developed here to allow more detailed examination of the mechanisms that drive drug absorption from LBFs and to inform better interpretation of the data that can be obtained with relatively simple lipid digestion models.
The in vitro digestion profiles of the fenofibrate formulations examined were largely consistent with what has been described previously (14, 49). The Type IV LBF (that comprised only hydrophilic formulation components, i.e., co-solvent and surfactant), had the highest solubilisation capacity for fenofibrate in the pre-concentrated undiluted state (Fig. 2). Solubilisation capacity, however, was rapidly lost during dispersion due to excipient miscibility with GI fluids (Fig. 3 – Type IV). The rapid loss in solubilisation capacity resulted in transient supersaturation and return of solubilised drug concentrations to values approaching equilibrium. In contrast, for both the more lipid-rich Type IIIA and IIIB formulations, drug solubilisation was maintained as the formulation was dispersed, and precipitation was only evident sometime after initiation of digestion. Comparing the Type IIIA and Type IIIB formulations, the larger quantities of lipid in the Type IIIA formulation appeared to further prolong drug solubilisation. Consistent with previous studies (50), therefore, increasing the quantity of lipid (rather than surfactant or co-solvent) in the formulation reduced drug precipitation on formulation dispersion and digestion. This likely reflects the formation of microemulsion or emulsion droplets on dispersion of the Type III formulations, where the larger lipid core of the colloids produced enhances drug solubilisation when compared to the micellar solution formed on dispersion of the Type IV formulation. Although the lipids and surfactants employed in the current formulations are all digestible, the impact of digestion was most profound for the formulations including greater quantities of glyceride lipids (i.e., the Type III formulations) rather than surfactant. The impact of digestion on the Type IV formulation was low.
The net effect of changes to the formulation on dispersion and digestion was that fenofibrate solubilisation was similar (and higher) after dispersion and digestion of the Type III formulations and lower from the Type IV formulation. These differences were magnified at early time points and limited at later time points. Across the two Type III formulations, the Type IIIA formulation, that contained the slightly higher quantities of lipid, resulted in slightly (but not significantly) better drug solubilisation when compared to the Type IIIB formulation.
In contrast to the in vitro solubilisation data, however, the absorptive drug flux data obtained from the same LBFs was remarkably similar. Thus, in spite of the three formulations maintaining very different total solubilised drug concentrations over the period of the intestinal perfusion, similar quantities of drug were absorbed. Some correlation is evident between total solubilised drug and total absorptive flux, however, the differences in flux were very small and variable, decreasing confidence in the power of the correlation.
The total quantity of drug perfused into the intestinal segment was the same for all formulations. Since drug flux into the mesenteric vein was similar for all LBF, it might be argued that drug flux was simply dependent on total drug (i.e., precipitated plus solubilised) perfused into the intestine, rather than the quantity of drug that was in solution. The data obtained for the aqueous suspension formulation of crystalline fenofibrate, however, argue against this suggestion and show that when formulated as a suspension at the same dose, the degree of absorptive flux is markedly lower. Delivery of the drug in combination with the LBF was therefore a requirement for increased drug absorption.
Whilst correlation of solubilised drug concentrations with drug flux is intuitive, more careful consideration of the likely mechanism of absorption suggests that the driving force for drug permeability across the absorptive membrane is not solubilised drug, but rather the free drug concentration that is in equilibrium with the solubilised reservoir (51). Thus, the solubilised drug concentration within the small intestine is the sum of drug within intestinal colloidal species plus drug in free solution, with these two drug forms being in rapid equilibrium. Drug in free solution is the form that is available for partitioning into and across the enterocyte, and when this occurs, drug partitions from the colloidal phase into free solution to maintain equilibrium between these two environments (17).
The free concentration is dictated by the thermodynamic activity of the system, where the thermodynamic activity of drug is equal to the product of the total concentration and the activity coefficient. In a simple solubilised system, the activity and activity co-efficient are quantitatively the same as the free concentration and the free fraction, respectively (52). The relationship between the solubilised concentration and the free concentration is defined by the micellar partition coefficient (or colloid partition co-efficient for non-micellar systems). At the solubility limit, the concentration of free drug equals the drug solubility in the intermicellar phase – i.e., the media employed minus the solubilising species. This is approximately the same as the solubility in the buffer employed to conduct the experiments. The free drug concentration at the solubility limit is therefore approximately the aqueous solubility, and at all solubilised drug concentrations below the solubility limit the free drug concentration is reduced. In the alternate scenario, where drug concentrations are above the equilibrium solubility limit (i.e., supersaturation), the free concentration in equilibrium with the supersaturated solubilised reservoir is higher than the solubility limit (making the assumption that the micellar/colloid partition coefficient is unaltered).
From this discussion it is evident that the driver of drug flux across the membrane might more accurately be estimated from the thermodynamic activity of drug in solution or the free concentration, rather than the total solubilised concentration. Direct measurement of the free concentration of drug in a rapidly changing kinetic environment is impractical since almost all methods require some time to separate free from bound drug (e.g., dialysis, polymer partitioning, centrifugation, etc.). A relative indicator of free concentration, however, may be obtained from a measurement of the degree of saturation or supersaturation of the colloids present in the GI tract at any one time. Thus, the degree of saturation or supersaturation is expected to be directly related to changes in free concentration. Taking this approach, the degree of supersaturation of all the examined formulations was calculated by taking the ratio of the measured solubilised concentration of fenofibrate during the digestion experiments and the apparent solubility of fenofibrate in the colloids present in the lipid digest at the same time point. This data is shown in Fig. 5c. By analogy with the data in Fig. 5a and b for total solubilised drug, taking the area under the saturation curve provides an indication of relative total exposure of free drug (Fig. 5d).
The trends in free drug exposure show that during dispersion, the Type IV formulation results in a transient spike in thermodynamic activity, due to a rapid loss in solubilisation capacity and a slight delay in precipitation. In contrast, the Type III formulations were not significantly supersaturated on dispersion (and therefore little precipitation was evident). On initiation of digestion, the solubilisation capacity of the Type III formulations dropped (dashed line in Fig. 3), but precipitation was not immediate. As such a period of supersaturation was maintained for ~15–30 min followed by a drop in concentration back towards equilibrium solubility. In contrast, the Type IV formulation lost solubilisation capacity on dispersion and was relatively unaltered by digestion. The net effect of these changes therefore was that the Type IV formulation might be expected to generate higher free concentrations on dispersion that decay rapidly, whereas the Type III formulations are expected to maintain free concentrations around the solubility limit on dispersion, followed by a jump in free concentration/supersaturation for a 15–30 min period following initiation of digestion, followed ultimately to a drop towards the solubility limit after digestion is initiated.
Taking the AUC of the saturation/supersaturation curve from zero to 60 min (i.e., the period of infusion), suggests that total exposure in free drug terms was highest for the Type IIIB formulation followed by Type IIIA followed by Type IV. But, this was not consistent with the in situ perfusion flux data that instead showed limited differences in drug exposure in the portal blood, regardless of formulation. The flux data are, however, highly consistent with a number of recent in vivo studies for fenofibrate using similar LBFs, where differences in bioavailability were not evident, in spite of differing in vitro digestion behaviour in the rat (20), Landrace pig (22) and mini pig (21). The ultimate read out from the in vitro lipid digestion – in situ absorption model (flux into mesenteric blood) therefore appears to be consistent with previous in vivo bioavailability studies, i.e., fenofibrate absorption seems to be relatively insensitive to the nature of the LBF employed, but is notably improved by formulation as a LBF when compared to administration as a suspension.
What is less clear is an explanation for the lack of correlation between drug flux and either total solubilised drug or free drug in the in vitro lipid digestion apparatus. A number of possible explanations are apparent. Firstly, where intestinal permeability is high, the required solubility needed to drive drug flux across the absorptive membrane may be sufficiently low that even very low free drug concentrations are able to promote absorptive flux. Under this circumstance, relatively small differences in thermodynamic activity may have little impact on absorption. Second, the suggestion that thermodynamic activity (or total solubilised drug) drives drug flux across the membrane and therefore absorption, assumes that the nature of the solubilised species produced by digestion of individual formulations has little impact on absorption (other than effects on solubilisation and thermodynamic activity) and acts only as a passive reservoir. It remains possible that different species may promote differing patterns of absorption, even at the same thermodynamic activity. For example, significant differences in particle size may change diffusion rates across the unstirred water layer (UWL), and previous studies have shown that the presence of lipids in the formulation may drive differences in supersaturation at the absorptive membrane due to lipid absorption (25). Finally, the surfactants and lipids commonly included in LBF may alter the biochemical barrier properties of intestinal wall, including the activity of efflux pumps and metabolic enzymes. Differences in the extent by which different formulations manipulate these properties may also prevent correlation between in vitro solubilisation and in vivo absorption profiles. These possibilities are the subject of ongoing investigation.
Conclusion
This work demonstrates the feasibility of using a coupled lipid digestion apparatus and single pass rat jejunum intestinal perfusion model to improve understanding of drug absorption from digesting LBFs in vivo. The model allows the simultaneous measurement of solubilised drug concentrations during a controlled lipid digestion experiment and drug flux into the mesenteric vein resulting from intestinal exposure to the same lipid digestion media. The model provides a means to better probe the interplay between drug solubilisation, supersaturation, precipitation and absorption for LBF. Consistent with previous in vivo studies, the studies described here using LBF of the PWSD fenofibrate, suggest that LBF significantly enhance drug absorption when compared to traditional suspension formulations, but that differences in in vitro drug solubilisation may not directly correlate with in vivo absorption, at least for highly permeable drugs such as fenofibrate.
Abbreviations
- 4-BPB:
-
4-bromophenylboronic acid
- AUC:
-
Area under the curve
- GI:
-
Gastrointestinal
- HPLC:
-
High performance liquid chromatography
- LBF:
-
Lipid-based formulation
- LFCS:
-
Lipid Formulation Classification System
- NaTDC:
-
Sodium taurodeoxycholate
- PC:
-
Phosphatidylcholine
- TBU:
-
Tributyrin units
- UPLCMS/MS:
-
Ultra performance liquid chromatography – tandem mass spectrometer
References
Amidon GL, Lennernas H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification - the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12(3):413–20.
Lipinski CA, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev. 2001;46(1–3):3–26.
Williams HD, Trevaskis NL, Charman SA, Shanker RM, Charman WN, Pouton CW, et al. Strategies to address low drug solubility in discovery and development. Pharmacol Rev. 2013;65(1):315–499.
Charman SA, Charman WN, Rogge MC, Wilson TD, Dutko FJ, Pouton CW. Self-emulsifying drug delivery systems: formulation and biopharmaceutic evaluation of an investigational lipophilic compound. Pharm Res. 1992;9(1):87–93.
Porter CJH, Trevaskis NL, Charman WN. Lipids and lipid-based formulations: optimizing the oral delivery of lipophilic drugs. Nat Rev Drug Discov. 2007;6(3):231–48.
Cuine JF, McEvoy CL, Charman WN, Pouton CW, Edwards GA, Benameur H, et al. Evaluation of the impact of surfactant digestion on the bioavailability of danazol after oral administration of lipidic self-emulsifying formulations to dogs. J Pharm Sci. 2008;97(2):995–1012.
Porter CJH, Pouton CW, Cuine JF, Charman WN. Enhancing intestinal drug solubilisation using lipid-based delivery systems. Adv Drug Deliv Rev. 2008;60(6):673–91.
Anby MU, Williams HD, McIntosh M, Benameur H, Edwards GA, Pouton CW, et al. Lipid digestion as a trigger for supersaturation: evaluation of the impact of supersaturation stabilization on the in vitro and in vivo performance of self-emulsifying drug delivery systems. Mol Pharm. 2012;9(7):2063–79.
Chen X-Q, Gudmundsson OS, Hageman MJ. Application of lipid-based formulations in drug discovery. J Med Chem. 2012;55(18):7945–56.
Pouton CW. Lipid formulations for oral administration of drugs: non-emulsifying, self-emulsifying and ‘self-microemulsifying’ drug delivery systems. Eur J Pharm Sci. 2000;11:S93–8.
Pouton CW. Formulation of poorly water-soluble drugs for oral administration: physicochemical and physiological issues and the lipid formulation classification system. Eur J Pharm Sci. 2006;29(3–4):278–87.
Williams HD, Sassene P, Kleberg K, Bakala-N’Goma JC, Calderone M, Jannin V, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 1: method parameterization and comparison of in vitro digestion profiles across a range of representative formulations. J Pharm Sci. 2012;101(9):3360–80.
Williams HD, Anby MU, Sassene P, Kleberg K, Bakala-N’Goma J-C, Calderone M, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations. 2. The effect of bile salt concentration and drug loading on the performance of type I, II, IIIA, IIIB, and IV formulations during in vitro digestion. Mol Pharm. 2012;9(11):3286–300.
Williams H, Sassene P, Kleberg K, Calderone M, Igonin A, Jule E, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 3: understanding supersaturation versus precipitation potential during the in vitro digestion of type I, II, IIIA, IIIB and IV lipid-based formulations. Pharm Res. 2013:1–18.
Williams HD, Sassene P, Kleberg K, Calderone M, Igonin A, Jule E, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 4: proposing a new lipid formulation performance classification system. J Pharm Sci. 2014;103(8):2441–55.
Bakala-N’Goma JC, Williams HD, Sassene PJ, Kleberg K, Calderone M, Jannin V, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations. 5. Lipolysis of representative formulations by gastric lipase. Pharm Res. 2015;32(4):1279–87.
Kaukonen AM, Boyd BJ, Charman WN, Porter CJH. Drug solubilization behavior during in vitro digestion of suspension formulations of poorly water-soluble drugs in triglyceride lipids. Pharm Res. 2004;21(2):254–60.
Fatouros DG, Mullertz A. In vitro lipid digestion models in design of drug delivery systems for enhancing oral bioavailability. Expert Opin Drug Metab Toxicol. 2008;4(1):65–76.
Larsen AT, Sassene P, Mullertz A. In vitro lipolysis models as a tool for the characterization of oral lipid and surfactant based drug delivery systems. Int J Pharm. 2011;417(1–2):245–55.
Do TT, Van Speybroeck M, Mols R, Annaert P, Martens J, Van Humbeeck J, et al. The conflict between in vitro release studies in human biorelevant media and the in vivo exposure in rats of the lipophilic compound fenofibrate. Int J Pharm. 2011;414(1–2):118–24.
Thomas N, Richter K, Pedersen TB, Holm R, Mullertz A, Rades T. In vitro lipolysis data does not adequately predict the in vivo performance of lipid-based drug delivery systems containing fenofibrate. AAPS J. 2014;16(3):539–49.
Griffin BT, Kuentz M, Vertzoni M, Kostewicz ES, Fei Y, Faisal W, et al. Comparison of in vitro tests at various levels of complexity for the prediction of in vivo performance of lipid-based formulations: case studies with fenofibrate. Eur J Pharm Biopharm. 2014;86(3):427–37.
Bevernage J, Brouwers J, Annaert P, Augustijns P. Drug precipitation–permeation interplay: supersaturation in an absorptive environment. Eur J Pharm Biopharm. 2012;82(2):424–8.
Dahan A, Hoffman A. The effect of different lipid based formulations on the oral absorption of lipophilic drugs: the ability of in vitro lipolysis and consecutive ex vivo intestinal permeability data to predict in vivo bioavailability in rats. Eur J Pharm Biopharm. 2007;67(1):96–105.
Yeap YY, Trevaskis NL, Porter CJH. The potential for drug supersaturation during intestinal processing of lipid-based formulations may be enhanced for basic drugs. Mol Pharm. 2013.
Stillhart C, Imanidis G, Griffin BT, Kuentz M. Biopharmaceutical modeling of drug supersaturation during lipid-based formulation digestion considering an absorption sink. Pharm Res. 2014;31(12):3426–44.
Stillhart C, Imanidis G, Kuentz M. Insights into drug precipitation kinetics during in vitro digestion of a lipid-based drug delivery system using in-line Raman spectroscopy and mathematical modeling. Pharm Res. 2013;30(12):3114–30.
Vogt M, Kunath K, Dressman JB. Dissolution enhancement of fenofibrate by micronization, cogrinding and spray-drying: comparison with commercial preparations. Eur J Pharm Biopharm. 2008;68(2):283–8.
Munoz A, Guichard JP, Reginault P. Micronised fenofibrate. Atherosclerosis. 1994;110(SUPPL):S45–8.
Persson L, Porter CH, Charman W, Bergström CS. Computational prediction of drug solubility in lipid based formulation excipients. Pharm Res. 2013:1–13.
Khoo S-M, Humberstone AJ, Porter CJH, Edwards GA, Charman WN. Formulation design and bioavailability assessment of lipidic self-emulsifying formulations of halofantrine. Int J Pharm. 1998;167(1–2):155–64.
Johnson BM, Chen W, Borchardt RT, Charman WN, Porter CJH. A kinetic evaluation of the absorption, efflux, and metabolism of verapamil in the autoperfused rat jejunum. J Pharmacol Exp Ther. 2003;305(1):151–8.
Singhal D, Ho NFH, Anderson BD. Absorption and intestinal metabolism of purine dideoxynucleosides and an adenosine deaminase-activated prodrug of 2′,3′-dideoxyinosine in the mesenteric vein cannulated rat ileum. J Pharm Sci. 1998;87(5):569–77.
Cao J, Chen X, Liang J, Yu X-Q, Xu A-L, Chan E, et al. Role of P-glycoprotein in the intestinal absorption of glabridin, an active flavonoid from the root of glycyrrhiza glabra. Drug Metab Dispos. 2007;35(4):539–53.
Masaoka Y, Tanaka Y, Kataoka M, Sakuma S, Yamashita S. Site of drug absorption after oral administration: assessment of membrane permeability and luminal concentration of drugs in each segment of gastrointestinal tract. Eur J Pharm Sci. 2006;29(3–4):240–50.
Chapman MJ. Pharmacology of fenofibrate. Am J Med. 1987;83(5, Supplement 2):21–5.
Caldwell J. The biochemical pharmacology of fenofibrate. Cardiology. 1989;76 Suppl 1:33–41.
Weil A, Caldwell J, Strolin-Benedetti M. The metabolism and disposition of fenofibrate in rat, guinea pig, and dog. Drug Metab Dispos. 1988;16(2):302–9.
Lovin I, Albu F, Tache F, David V, Medvedovici A. Solvent and salting effects on sample preparation for the determination of fenofibric acid in human plasma by HPLC-DAD. Microchem J. 2003;75(3):179–87.
Niebergall PJ, Patil MY, Sugita ET. Simultaneous determination of dissolution and partitioning rates in vitro. J Pharm Sci. 1967;56(8):943–7.
Gibaldi M, Feldman S. Establishment of sink conditions in dissolution rate determinations. Theoretical considerations and application to nondisintegrating dosage forms. J Pharm Sci. 1967;56(10):1238–42.
Shi Y, Gao P, Gong Y, Ping H. Application of a biphasic test for characterization of in vitro drug release of immediate release formulations of celecoxib and its relevance to in vivo absorption. Mol Pharm. 2010;7(5):1458–65.
Minekus M, Marteau P, Havenaar R. A multi-compartmental dynamic computer-controlled model simulating the stomach and small intestine. ATLA Altern Lab Anim. 1995;23:197–209.
Kataoka M, Masaoka Y, Yamazaki Y, Sakane T, Sezaki H, Yamashita S. In vitro system to evaluate oral absorption of poorly water-soluble drugs: simultaneous analysis on dissolution and permeation of drugs. Pharm Res. 2003;20(10):1674–80.
Ginski MJ, Polli JE. Prediction of dissolution–absorption relationships from a dissolution/Caco-2 system. Int J Pharm. 1999;177(1):117–25.
Buch P, Langguth P, Kataoka M, Yamashita S. IVIVC in oral absorption for fenofibrate immediate release tablets using a dissolution/permeation system. J Pharm Sci. 2009;98(6):2001–9.
Corrigan OI, Gubbins RH, O’Driscoll CM. Estimation of absorption parameters from the non-steady-state phase in the rat gut perfusion model. J Pharm Pharmacol. 2003;55(4):487–93.
Stappaerts J, Brouwers J, Annaert P, Augustijns P. In situ perfusion in rodents to explore intestinal drug absorption: Challenges and opportunities. Int J Pharm. 2015;478(2):665–81.
Mohsin K. Design of lipid-based formulations for oral administration of poorly water-soluble drug fenofibrate: effects of digestion. AAPS PharmSciTech. 2012;13(2):637–46.
Cuine JF, Charman WN, Pouton CW, Edwards GA, Porter CJH. Increasing the proportional content of surfactant (Cremophor EL) relative to lipid in self-emulsifying lipid-based formulations of danazol reduces oral bioavailability in beagle dogs. Pharm Res. 2007;24(4):748–57.
Simmonds WJ. The role of micellar solubilization in lipid absorption. Aust J Exp Biol Med Sci. 1972;50(4):403–21.
Boyd BJ, Porter CJH, Charman WN. Using the polymer partitioning method to probe the thermodynamic activity of poorly water-soluble drugs solubilized in model lipid digestion products. J Pharm Sci. 2003;92(6):1262–71.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors would like to thank Mr Doron Gafni for drawing of the model schematic. Funding support from the Monash University Institute of Graduate Research (MIGR) is gratefully received.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crum, M.F., Trevaskis, N.L., Williams, H.D. et al. A new in vitro lipid digestion – in vivo absorption model to evaluate the mechanisms of drug absorption from lipid-based formulations. Pharm Res 33, 970–982 (2016). https://doi.org/10.1007/s11095-015-1843-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-015-1843-7