Purpose
To investigate the impact of a change in the proportions of lipid, surfactant and co-solvent on the solubilisation capacity of self-emulsifying formulations of danazol during in vitro dispersion and digestion studies and correlation with in vivo bioavailability in beagle dogs.
Methods
Formulations from within the phase diagram of the pseudo-ternary system composed of soybean oil:maisine 35-1 (1:1 w/w), Cremophor EL and ethanol were assessed in vitro on dispersion and digestion. The relative bioavailability of danazol after administration of a series of these formulations was also determined.
Results
All formulations formed microemulsions in the presence of water and no drug precipitation was observed on dispersion. In contrast, drug solubilisation was markedly affected by lipase-mediated digestion and a reduction in lipid (and increase in surfactant) content resulted in increased drug precipitation. Consistent with these data, the bioavailability of danazol decreased significantly when the lipid content in the formulations was reduced.
Conclusion
A rank-order correlation was observed between the patterns of solubilisation obtained during in vitro digestion and the in vivo performance of self-emulsifying formulations of danazol. In general a decrease in the lipid content and an increase in the proportions of surfactant and co-solvent resulted in reduced danazol bioavailability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The ability of lipid-based formulations to enhance the oral bioavailability of poorly water-soluble drugs has been recognised for many years (1,2). Although the rationale for such enhancement is not completely understood, it is commonly believed that increased luminal solubilisation and improved drug dissolution in the gastrointestinal tract (GIT) are the main mechanisms responsible for enhanced bioavailability. Increased drug solubilisation is achieved by the interaction of lipidic formulations and their digestion products with endogenous bile salts and phospholipids to form a range of vesicular and micellar species with enhanced solubilisation capacities in the intestine (3,4).
In recent years, there has been increasing focus on the utility of self-emulsifying lipid-based formulations to enhance the oral bioavailability of lipophilic drugs. However, despite the proven utility of these formulations and the fact that more than 40% of new drug candidates exhibit poor solubility in water (5) relatively few self-emulsifying lipid-based products (examples include cyclosporin A (Neoral®) and the protease inhibitors ritonavir (Norvir®), saquinavir (Fortovase®) and amprenavir (Agenerase®)) have been commercialised. The reasons underlying the lack of application of these technologies are not entirely clear, but likely reflect a limited knowledge of the formulation parameters responsible for good in vivo performance and the fact that few in vivo studies in humans have been reported in the literature when compared with conventional solid dosage forms. The lack of data describing useful in vitro tests that are predictive of in vivo performance has also hindered successful development of lipidic formulations.
The design of self-emulsifying lipid-based formulations has historically been driven by a knowledge of the solubility of a candidate drug in the dose form, the ease of dispersion of the formulation and the particle size of the resulting emulsion droplets (6–15). As a consequence, self-emulsifying formulations have commonly been assessed by simple dispersion tests in aqueous media coupled with particle size measurements to define the resulting dispersion. More recently, however, it has been suggested that additional assessment of the impact of lipid digestion on the solubilisation capacity of a lipid-based formulation is required to more accurately explain the in vivo performance of lipid-based formulations (16–21). Using these models, long-chain lipid digestion products have typically been shown to increase solubilisation in the GI milieu and enhance drug absorption more effectively than their medium-chain comparators (4,22–25). Although long-chain lipids appear to promote effective drug solubilisation in the GIT, drug solubility in formulations comprising large quantities of triglycerides is often limited. In recent years therefore, there has been a trend towards the design of self-emulsifying lipid-based formulations containing large amounts of hydrophilic surfactants (HLB>12) and co-surfactants or co-solvents in an attempt to increase drug loading capacity and to produce very fine dispersions (13,14,26,27). However, little is known regarding the nature of the colloidal structures produced by these systems in vivo and in particular whether they are equally capable of maintaining lipophilic drugs in solution during passage along the GIT when compared with similar formulations containing larger quantities of long-chain lipids.
Consequently in the current study, a series of self-emulsifying formulations containing the poorly water-soluble steroid, danazol [aqueous solubility <1 μg/ml, log P=4.53 (28)] have been investigated and the effects of changing the relative quantities of lipid, surfactant and co-solvent on drug solubilisation during in vitro dispersion and digestion examined. The bioavailability of danazol after oral administration of self-emulsifying formulations containing increasing quantities of surfactant and co-solvent to beagle dogs has subsequently been assessed in an attempt to correlate in vitro and in vivo behaviour. The current data confirm the utility of in vitro lipid digestion models to assist in the design of lipid-based formulations and suggest that formulations containing large quantities of at least some surfactants relative to the quantities of long-chain lipids may not provide sufficient solubilisation capacity in vivo.
MATERIALS AND METHODS
Materials
Danazol (pregna-2,4-dien-20-yno[2,3-d]isoxazol-17-ol) was kindly supplied by Sterling Pharmaceuticals (Sydney, Australia). Diazepam was from Alphapharm (Sydney, Australia). Soybean oil (C18 triglycerides), Cremophor EL (polyoxyl 35 castor oil), polyethylene glycol 400 (PEG 400), sodium taurodeoxycholate 99% (NaTDC) and porcine pancreatin (8×USP specifications activity) were from Sigma Chemical Co. (St Louis, MO, USA). Maïsine 35-1, a blend of long-chain mono- and diglyceride consisting primarily of linoleic acid (55%, C18:2), oleic acid (29%, C18:1) and palmitic acid (11%, C16:0), was a generous gift from Gattefossé (St Priest, France). Lecithin (approximately 60% pure phosphatidylcholine (PC) by HPTLC (2) from egg yolk) was a gift from Pharmacia LKB (Uppsala, Sweden), 4-bromophenylboronic acid (4-BPB) was obtained from Aldrich Chemicals Co. (St Louis, MO, USA) and 1 M sodium hydroxide (Titrisol), which was diluted to obtain 0.2 M NaOH titration solution, was purchased from Merck (Darmstadt, Germany). Water was obtained from a Milli-Q water purification system (Millipore, Bedford, MA, USA). All other chemicals and solvents were of analytical purity or high performance liquid chromatography (HPLC) grade, respectively.
Establishment of the Pseudo-ternary Phase Diagram
The phase diagram of the pseudo-ternary system composed of long-chain lipid [soybean oil:maisine 35-1 (1:1 w/w)], Cremophor EL and absolute ethanol after dispersion (1 in 200 v/v) in water was established in the absence of drug and classified according to the efficiency of self-emulsification and the final appearance of the resultant emulsion. Each system was prepared by weighing the exact quantity of each excipient into a screw cap glass tube followed by vortexing to allow complete mixing. After overnight incubation at 37°C, non-isotropic mixtures were noted and discarded and isotropic mixtures were assessed for the efficiency of self-emulsification. The efficiency of self-emulsification was assessed using a USP II dissolution apparatus (Erweka, Germany). Each isotropic mixture (1 ml) was added dropwise to 200 ml of milli-Q water at 37°C. Gentle agitation was provided by a standard stainless steel dissolution paddle rotating at 60 rpm. The systems were assessed visually in terms of the rate of emulsification and the final appearance of the emulsion. Classification was stratified into systems that formed clear microemulsions or alternatively, systems that resulted in the formation of microemulsions which had a bluish white appearance. More detailed evaluation of specific systems was conducted as described below.
Preparation of the Drug Loaded Self-emulsifying Lipid-Based Formulations
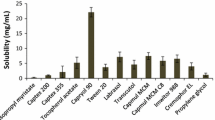
Specific compositions within the phase diagram were selected for more detailed evaluation using in vitro dispersion and digestion methodologies (Table I). In separate studies an additional series of formulations was also evaluated to examine the impact of changing the nature of the co-solvent from ethanol to PEG 400 and propylene glycol. In all cases, danazol was incorporated at 80% of its saturated solubility in the formulation (at 37°C) in order to maintain the thermodynamic activity constant across all formulations. Drug solubility in each excipient was assessed using standard methodologies (30). Solubility was defined as the value attained when at least three consecutive solubility samples varied by ≤5%. Approximately 5–10 g of each formulation was prepared by weighing the various proportions of Cremophor EL, long-chain lipid and danazol into a 50 ml beaker. The components were mixed at 50°C using a magnetic stirrer to facilitate drug solubilisation. The mixture was then cooled to ambient temperature before addition of the ethanol and further stirred to ensure homogeneity. Formulations were then transferred into screw cap glass vials and stored at 37°C to equilibrate overnight prior to evaluation.
In Vitro Evaluation
Drug Solubilisation During Formulation Dispersion
Dispersion studies were performed in 250 ml of 0.1 N HCl (pH 1.2) at 37°C using a USP II dissolution apparatus (Erweka, Germany). Gentle agitation was provided by a stainless steel dissolution paddle mounted immediately below the solution meniscus and operated at 100 rpm. A mass of formulation (1 g) was weighed onto a glass slide and introduced into the dissolution media. Aliquots (500 μl) of the dissolution media were then sampled at 0.5, 1, 2.5, 5, 10, 20, 30, 40, 50 and 60 min after introduction of the formulation and centrifuged for 15 min at 37°C and 3,500 rpm (Beckman GS-6R centrifuge, Beckman Instruments Inc., Fullerton, CA, USA). Samples of the supernatants obtained post centrifugation were assayed for danazol content by HPLC as described below. The mean particle size of the dispersed emulsion/microemulsion droplets present in the dissolution media was also assessed as described previously (31) using photon correlation spectroscopy (PCS) (Malvern Zetasizer 3000, Malvern Instrument, UK).
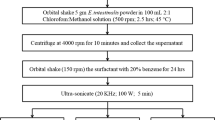
Drug Solubilisation During Formulation Digestion
In vitro digestion experiments were performed as previously described (29). Briefly, 1 g of self-emulsifying lipid-based formulation (containing danazol at 80% of its saturated solubility in the formulation) was dispersed in 36 ml of digestion buffer (50 mM TRIS maleate, 150 mM NaCl, 5 mM CaCl2. 2H2O, pH 7.5) containing 5 mM NaTDC and 1.25 mM PC [conditions broadly representative of fasted state intestinal conditions (32,33)]. Experiments were performed at 37°C in a stirred and thermostated glass vessel and were initiated by the addition of 4 ml of pancreatin extract containing 40,000 tributyrin units (TBU) of pancreatic lipase (final lipase concentration of 1,000 TBU per ml). Lipolysis was followed over 60 min using a pH-stat titration unit (Radiometer, Copenhagen, Denmark), which maintained the pH at 7.5. The fatty acids produced on lipolysis were titrated with 0.2 M NaOH. Aliquots (4.4 ml) were taken from the digestion medium at 5, 10, 15, 30, 45 and 60 min and lipolysis inhibitor (4-BPB, 9 μl of a 0.5 M solution in methanol per ml of digestion medium) immediately added to each sample to prevent further lipolysis (16,34). Samples were subsequently ultracentrifuged for 30 min at 37°C and 334,000×g (Optima XL-100 K centrifuge, SW-60 rotor, Beckman, Palo Alto, CA, USA) in order to separate the digests into an aqueous phase and a pellet phase. Samples obtained from each separated phase were assayed for danazol content by HPLC as described below.
Sample Preparation and HPLC Analysis of in vitro Dispersion and Digestion Samples
In the dispersion studies supernatant samples were simply diluted 1:1 (v/v) with acetonitrile prior to HPLC analysis. Samples of danazol in the pellets obtained from the digestion studies were first dissolved in 5 ml of chloroform:methanol (2:1 v/v) and subsequently diluted 1:10 (v/v) in acetonitrile prior to analysis by HPLC. Danazol containing aqueous phase samples were diluted 1:10 (v/v) with acetonitrile before HPLC analysis.
Danazol chromatography was conducted using a Beckman 126 Programmable Solvent Module, and a Beckman 168 Programmable detector (Beckman Coulter, Fullertone, CA, USA) and a waters 717 autosampler (Waters, MA, USA). A Waters symmetry C18 column (3.9×150 mm) (Waters, MA, USA) was maintained at 25°C using a Waters 038040 Column Heater Module (Waters, MA, USA). The mobile phase consisted of 60% (v/v) acetonitrile and 40% (v/v) milli-Q water. The flow rate was 1 ml/min. All samples were maintained at 10°C in the autosampler prior to injection of 50 μl. Detection of danazol was conducted by single wavelength monitoring at 286 nm.
The assay was validated by analysis of n=5 replicate standards made up at three different concentrations (0.5, 5, 50 μg/ml). Intra-assay variability was accurate to 101.6, 100.6 and 100.0% and precise to ± 3.1, 0.3 and 0.01% of 0.5, 5 and 50 μg/ml, respectively. Inter-assay variability was assessed over three separate days and was accurate to 105.2, 99.3 and 100.0% and precise to ± 5.2, 0.7 and 0.02% of 0.5, 5 and 50 μg/ml, respectively. The recovery of danazol spiked aqueous and pellet phases obtained from blank digests of pure soybean oil was 99.8±11.8 % (n=6).
Bioavailability Studies
Administration and Sampling
All experimental procedures were approved and performed in accordance with the guidelines of the local Institutional Animal Experimentation Ethics Committee. The study was conducted as a four-way crossover (7-day washout) in four male beagle dogs (13–23 kg). There were four different treatments, three consisting of self-emulsifying lipid-based formulations of danazol containing decreasing amounts of long-chain lipid [formulations F1, F2 and F3 containing 60, 37.5 and 18% soybean oil:maisine 35-1 (1:1 w/w), respectively] and one treatment consisting of a lipid free drug delivery system (formulation F4) (Table I). Formulations 1–4 were hand filled into air filled soft gelatin capsules 2 h prior to dosing as described previously (31). Each treatment was administered in two soft gelatine capsules (2×800 mg) with 50 ml water. Danazol was dosed at 80% of its saturated solubility in each formulation and the total dose administered with each treatment was 18.9 mg for F1, 25.8 mg for F2, 28.5 mg for F3 and 28.8 mg for F4. The dogs were fasted for at least 20 h prior to dosing. After dosing, animals remained fasted until 10 h post-dose, after which they were fed on a daily basis. Water was available ad libitum. Blood samples (3 ml), obtained from the cephalic vein either via an indwelling catheter or by individual venipuncture were collected pre-dose (−5 min) and at 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 10, 24, 32 and 48 h post-dosing into sterile tubes containing 5 mg of dipotassium EDTA. Plasma was separated by centrifugation for 15 min at 1,600×g and stored at −20°C prior to danazol analysis by HPLC as described below.
Plasma Sample Preparation
Calibration standards for danazol were prepared by spiking 1 ml aliquots of blank plasma with 100 μl of a 60:40 (v/v) acetonitrile:water solution containing 0.05, 0.10, 0.50, 1.0, 2.5 and 5.0 μg/ml danazol. This provided spiked plasma concentrations in the range of 5–500 ng/ml danazol. In order to compensate for the volume of the spiking solution added to plasma standards, 100 μl of 60:40 (v/v) acetonitrile:water was similarly added to the plasma samples obtained during the pharmacokinetic studies. One hundred microliters of an internal standard solution (20 μg/ml of diazepam prepared in 60:40 acetonitrile:water) was also added to each plasma sample or standard, the tubes vortexed for 1 min, and 6 ml n-hexane added. The tubes were then vortexed again for 1.5 min prior to centrifugation for 5 min at 3,500 rpm in a Beckman GS-6R refrigerated centrifuge. The organic phase was transferred into new tubes and the content evaporated to dryness under nitrogen at 30°C using an N-EVAP evaporator (Organomation, Berlin, MA, USA). The dried extracts were reconstituted with 100 μl of a 60:40 (v/v) acetonitrile:water solution, vortexed for 2 min, and centrifuged again for 5 min at 3,500 rpm (Beckman GS-6R centrifuge, Beckman Instruments Inc., Fullerton, CA, USA). The entire volume of the reconstituted material (100 μl) was transferred to limited volume autosampler vials and 50 μl injected onto the HPLC.
Unknown concentrations were determined by comparison of the unknown danazol:IS peak height ratio with a calibration curve of danazol:IS peak height ratio vs. danazol concentration constructed using the calibration standards. The plasma assay was validated by analysis of n=5 quality control samples containing 10, 100 and 500 ng/ml danazol in blank plasma on three consecutive days. Intra-assay variability was accurate to 104.4, 102.0 and 103.0% and precise to ±4.4, 2.0 and 3.0% of 10, 100 and 500 ng/ml, respectively. Inter-assay variability was accurate to 99.2, 99.1 and 101.1% and precise to ±0.8, 0.9 and 1.1% of 10, 100 and 500 ng/ml, respectively. The lower limit of quantification for the plasma assay (5 ng/ml) was determined by replicate analysis (n=4) of spiked plasma samples and defined as the lowest concentration at which appropriate accuracy and precision was obtained. At 5 ng/ml the assay was accurate to 106.4% and precise to 6.4%.
Danazol Plasma Sample Chromatography
Chromatography was conducted using a Beckman 126 Programmable Solvent Module, a Beckman 168 Programmable detector (Beckman Coulter, Fullertone, CA, USA) and a waters 717 autosampler (Waters, MA, USA). A Waters symmetry C18 column (3.9×150 mm) (Waters, MA, USA) was maintained at 25°C using a Waters 038040 Column Heater Module (Waters, MA, USA). The mobile phase consisted of a mixture of solvent A (10% v/v acetonitrile: 90% v/v milli-Q water) and solvent B (90% v/v acetonitrile:10% v/v milli-Q water). The flow rate was 1.2 ml/min. The initial percentage of solvent B was 50%. This was linearly increased to 60% over the first 2 min and was held at 60% solvent B for a further 13 min. After 15 min, the proportion of solvent B was increased to 90% over 5 min and was then held at 90% until 24 min. At this time, the gradient returned to 50% solvent B over 1 min. Total run-time was 30 min. All samples were maintained at 10°C in the autosampler prior to injection of 50 μl. Detection of danazol and the internal standard was conducted by single wavelength monitoring at 292 nm.
Pharmacokinetic Data Analysis
The peak plasma concentrations (C max) and the time for their occurrence (T max) were noted directly from the individual plasma concentration vs. time profiles. The area under the plasma concentration vs. time profiles (AUC 0−10) was calculated by the linear trapezoidal method. Because the danazol plasma concentrations were typically below the limit of quantification of the assay at 24, 32 and 48 h post-dose, accurate determination of the terminal elimination rate constant and (\(AUC^{{0 - \infty }}\)) was not possible. However, the danazol plasma concentrations at 10 h were low, and therefore the extrapolated AUC (\(AUC^{{10 - \infty }}\)) was expected to contribute only a minor proportion of the total AUC (\(AUC^{{0 - \infty }}\)). Relative bioavailability comparisons were therefore performed using (\(AUC^{{0 - 10}}\)).
Statistically significant differences were determined by ANOVA followed by Tukey’s test for multiple comparisons at a significance level of α=0.05. All statistical analysis was performed using SPSS for windows version 11.5.0. (SPSS Inc, Chicago, IL, USA).
RESULTS
Formulation Characteristics
The miscibility and self-emulsification behaviour of the Cremophor EL/soybean oil:maisine 35-1 (1:1 w/w)/ethanol mixtures is summarized in Fig. 1. When initial combinations of components were assembled, it became apparent that many combinations of components were not miscible at 37°C therefore precluding further examination. These systems are shown in white in the phase diagram to the right of the broken line. It is apparent that below 60% w/w Cremophor EL and in presence of >10% w/w long-chain lipid these systems were relatively poorly miscible. For those combinations that were miscible, it is further apparent that efficient self-emulsification only occurred when the amount of Cremophor EL was above 30% w/w. Incorporation of danazol in the placebo formulations did not modify the properties of self-emulsification.
Pseudo-ternary phase diagram for a self-emulsifying drug delivery system composed of long-chain lipids [soybean oil: maisine 35-1 (1:1 w/w)], Cremophor EL and absolute ethanol diluted 1:200 v/v in water. Isotropic combinations that formed clear microemulsions and microemulsions with a bluish-white appearance are represented in light grey and dark grey respectively. The white area represents combinations of components that were not miscible (right side of the dotted line) and combinations that were miscible but did not emulsify efficiently in the presence of water (left side of the dotted line). Combinations that were subsequently investigated in vitro are numbered from 1 to 9 (refer to Table I).
In Vitro Evaluation
Dispersion and Particle Size
Formulations of various compositions in terms of the ratio of lipid to surfactant and the percentage of included co-solvent were selected from within the domains of isotropy and self-emulsification in the ternary phase diagram (Fig. 1 and Table I) and these specific compositions examined in more detail. All the formulations, with the exception of formulations 2, 7 and 8 dispersed rapidly (within 1 min) (Fig. 2) to form microemulsions with emulsion droplets sizes <80 nm (Table I). Formulations 2, 7 and 8 contained relatively high quantities of Cremophor EL (>50% w/w) and low quantities of ethanol (<10% w/w) and formed a viscous gel that slowly dissolved over time, presumably reflecting a difficulty in water penetration of the gel phase (35,36) (Fig. 2). Although F2 and F8 contained similar ratios of lipid to surfactant, the inclusion of 7.5% w/w ethanol significantly improved the dispersion properties of F2 when compared with F8 (zero ethanol). The ease of dispersion was therefore facilitated by the incorporation of co-solvent (i.e., ethanol) and the size of the resulting emulsion droplets was slightly reduced by the incorporation of greater quantities of surfactant (Table I: F1 vs. F5, F6, F7 or F8), although in all cases the differences were small. Once effective dispersion was achieved all the formulations maintained the drug in a solubilised state in simulated gastric media (i.e., no precipitation was evident), even in the absence of lipid and in the presence of relatively high quantities of water miscible co-solvent (F4) (Fig. 2).
Dispersion profiles for self-emulsifying lipid-based formulations F2 (open circle), F7 (open triangle) and F8 (filled circle) [mean ± SD (n=3)] and average dispersion profile for formulations F1, F3, F4, F5, F6 and F9 (inverted filled triangle) in simulated gastric media (0.1 N HCl) [mean ± SD (n=18)]. Formulations F1, F3–F6 and F9 displayed almost identical dispersion profiles and were therefore plotted together as the mean of all data points to improve the clarity of the figure.
Digestion Studies
In contrast to the dispersion studies, the ability of many of the formulations to prevent danazol precipitation was markedly affected by lipid digestion. Under the digestion conditions employed here, fatty acids were liberated (and titrated) rapidly, and maximal rate of digestion was observed in the first 5–10 min of the experiment. Fatty acid production had slowed dramatically by 60 min in all cases, and no residual oil phase was apparent on ultracentrifugation of the digestion media. Consistent with previous results (37) release of fatty acids from the lipid free formulation (F4) was also observed, suggesting that the ethoxylated glycerides present in Cremophor EL were digested by pancreatic lipase-colipase. Analysis of the danazol content of the aqueous and pellet phases obtained by ultracentrifugation of the digestion media revealed that a reduction in the lipid content of the formulation from 60 to 40% w/w long-chain lipids resulted in a dramatic reduction in solubilisation capacity of the digested formulation with only 48% of the dose remaining in the aqueous phase (F8) when compared with 92% of the dose when 60% w/w long-chain lipid was present in the formulation (F5) (Fig. 3). The incorporation of up to 10% w/w ethanol did not affect the solubilisation capacity of formulations containing similar ratios of lipid to surfactant with 92 and 83% of the dose remaining in solution for F5 and F9 respectively and 48% of the dose remaining in solution for both F8 and F2 (Fig. 4). However, an increase in the percentage of ethanol to 18% (F3) and 35% (F4) w/w in the formulation, in combination with a reduction in the lipid content, resulted in significantly increased drug precipitation. Most noticeably, the lipid-free formulation (F4) containing 35% w/w ethanol and 65% w/w Cremophor EL retained only 22% of the dose in the aqueous phase post digestion. To examine the impact of a change to the nature of the co-solvent employed, the composition of F3 was modified and ethanol was replaced by PEG 400 (F3-PEG) or propylene glycol (F3-PG). The data in Table II suggest that both F3-PEG and F3-PG containing 64% w/w Cremophor EL, 18% w/w long-chain lipid and 18% w/w of PEG 400 or propylene glycol respectively, effectively prevented drug precipitation on dispersion, but displayed similar solubilisation and precipitation profiles on digestion to that observed with F3 containing 18% w/w ethanol (Table II).
Solubilisation profile of danazol during in vitro digestion of ethanol-free self-emulsifying formulations F5 (filled square), F6 (inverted filled triangle), F7 (filled triangle) and F8 (filled circle) containing 60, 55, 50 and 40% (w/w) long-chain lipid respectively [mean ± SD (n=3)]. In these binary formulations the remaining proportion of the formulations was Cremophor EL.
Solubilisation profile of danazol after in vitro digestion of self-emulsifying formulations F1 (open triangle), F2 (inverted open triangle), F3 (open square), F4 (open circle), F5 (filled circle), F8 (filled triangle) and F9 (filled square) containing increasing quantity of co-solvent [mean ± SD (n=3)]. Formulations that were subsequently assessed in vivo are shown with open symbols.
Bioavailability Data
The mean plasma concentration vs. time profiles for danazol (data normalized to a 15 mg dose) following oral administration of F1–F4 are shown in Fig. 5. Danazol plasma concentrations were typically below the limit of quantification of the assay at 24 and 48 h post dose and as such data have been truncated to 10 h to aid comparison of C max and T max. The corresponding mean pharmacokinetic parameters for all formulations, are tabulated in Table III. The terminal half-lives (t 1/2) for all treatments were consistent and in the range reported previously for beagle dogs [2.7±1.4 h (38)]. The plasma profile of danazol after oral administration of F1 was also consistent with that reported in a previous study (24), providing further confidence in the validity of the data obtained.
Mean plasma concentration vs. time profiles [mean ± SEM (n=4)] for danazol (normalized to a 15 mg dose) after oral administration to beagle dogs of (open triangle) formulation F1 (containing 60% w/w lipid and 10% w/w ethanol), (inverted open triangle) formulation F2 (containing 37.5% w/w lipid and 7.5% w/w ethanol), (filled square) formulation F3 (containing 18% w/w lipid and 18% w/w ethanol) and (filled circle) the lipid-free formulation F4 (containing 35% w/w ethanol) (2×800 mg soft gelatin capsules).
A clear distinction in terms of relative bioavailability and C max was observed between the formulations, and the bioavailability of danazol after administration of F1 (containing 60% long-chain lipid) was approximately two fold higher than that of F2 (containing 37.5% long-chain lipid and 7.5% ethanol) and F3 (containing 18% long-chain lipid and 18% ethanol), and three times higher than that of the lipid free formulation (F4). No significant differences in bioavailability were seen between F2 and F3.
DISCUSSION
In an attempt to better predict the relative in vivo performance of lipid-based formulations, in vitro lipid digestion models have recently been developed (17,21,22,39), and utilised to more effectively reflect the solubilisation conditions that exist in vivo and to identify the formulation parameters responsible for efficient in vivo performance. Using this approach, we have previously shown that a self-emulsifying drug delivery system containing long-chain lipids (LC-SMEDDS) appears to more effectively promote the oral bioavailability of danazol when compared with a similar formulation comprising medium-chain lipids (24). Furthermore, no difference in the bioavailability of danazol was observed after oral administration of a simple long-chain triglyceride solution (LCT-solution) when compared with a LC-SMEDDS formulation, despite both formulations displaying significant differences in terms of dispersibility. These data suggested that the nature of the lipid phase (at least in terms of long vs medium-chain lipids) was more important for bioavailability enhancement when compared with the degree of dispersion of the formulation. However, these studies were conducted using fixed ratios of formulation components, and to that point we had little understanding as to the potential impact of a change to the proportions of lipid, surfactant and co-surfactant/co-solvent on the in vivo performance of self-emulsifying lipid-based formulations.
The current studies were therefore conducted to compare the in vivo performance of self-emulsifying formulations comprising varying ratios of lipid to surfactant and increasing quantities of co-solvent and to confirm the utility of in vitro lipid digestion models to predict the in vivo formulation differences.
All the formulations investigated dispersed spontaneously in aqueous media to form microemulsions with particle sizes below 80 nm (Table I). The solubilisation capacity of the formulations was not affected by dilution in aqueous media as shown by the absence of drug precipitation on dispersion in simulated gastric media (Fig. 2). A Cremophor EL concentration of 30% w/w or above was required to provide for efficient self-emulsification (Fig. 1) and a higher relative proportion of Cremophor EL also resulted in increased drug loads (Table II) (as poorly water-soluble drugs with an intermediate partition coefficient (2<Log P<4) generally display higher affinities for non-ionic surfactants when compared to natural oils). At Cremophor EL contents above 50% w/w (in the absence of co-solvent), however, the formation of viscous gels delayed self-emulsification (although these systems did eventually produce very clear dispersions with very small particle sizes (<50 nm)). The formation of gel-like structures during the dispersion of lipid-based formulations has previously been observed by Pouton in systems comprising Tween 85 and Miglyol 840 when the quantity of surfactant was >50% w/w (40) and also by Wakerley (41) in mixtures of Tagat TO and medium-chain glycerides, again at higher surfactant contents. In the current studies the ease of emulsification was increased by the inclusion of ethanol into the formulation (Fig. 2). The ease of emulsification of self-emulsifying formulations has been suggested to be associated with the formation of liquid crystals at the interface of the oil/surfactant mixture and water, resulting from water penetration into the oil/surfactant blend (35,42,43). Self-emulsification is subsequently thought to occur via fracture of the liquid crystals leading to droplet formation under gentle agitation (41,42,44). Inclusion of co-solvents and/or co-surfactants in the formulations may therefore facilitate improved self-emulsification by enhancing the ability of the aqueous phase to penetrate into the liquid crystals formed (45,46).
It has recently been suggested that assessment of the impact of lipid digestion on the solubilisation capacity of lipid-based formulations might more accurately explain the in vivo performance of lipid-based formulations (18,19,24). Consequently, the impact of digestion by pancreatic lipase/colipase on the solubilisation capacity of F1–F9 was also investigated. In contrast to the patterns of solubilisation observed on dispersion where no difference between the formulations was observed (Fig. 1), the ability of the formulations to provide efficient drug solubilisation during lipase-mediated digestion was markedly affected by a change in the ratio of lipid to surfactant and co-solvent. Indeed, a reduction in relative lipid content resulted in a significant loss of solubilisation capacity of the colloidal species formed post digestion (Fig. 3). The substitution of large quantities of the lipid phase with ethanol also resulted in significant drug precipitation (Fig. 4: F8 vs F3, F4). In contrast, the incorporation of up to 10% w/w ethanol did not seem to affect the solubilisation capacity of the formulations (Fig. 4: F2 vs F8 and F9 vs F5). Interestingly, the nature of the co-solvent did not appear to impact on the post digestion solubilisation capacity of the lipidic formulations, even those containing a significant proportion of co-solvent (Table II).
In an attempt to confirm the impact of changing the relative proportion of lipid, surfactant and co-solvent on drug bioavailability and to compare the in vitro and in vivo end-points, F1–F4 (containing 60, 37.5, 18 and 0% w/w lipid) were administered to beagle dogs. Consistent with the digestion data (Fig. 4), the plasma profiles in Fig. 5 and the pharmacokinetic parameters in Table III reveal a decrease in oral bioavailability as the quantity of long-chain lipid present in the formulation was reduced and the amount of surfactant and/or co-solvent increased.
Cremophor EL and ethanol therefore facilitate the emulsification process and contribute to the formation of very fine dispersions, but do not appear to enhance the solubilisation capacity in an intestinal environment as significantly as long-chain lipids. [It should be acknowledged however that surfactants, including Cremophor EL, may have additional beneficial effects on the intestinal absorption of compounds where bioavailability is limited by P-glycoprotein (47-49)]. In agreement with these data, Porter et al. previously failed to observe a significant difference in danazol bioavailability after administration of a long-chain lipid solution (LCT-sol) and a long-chain lipid self-emulsifying drug delivery system (LC-SMEDDS) equivalent to F1 (24). These studies suggest that precipitation in the GIT is prevented by drug solubilisation in the micellar systems formed by incorporation of lipid digestion products into endogenous bile salts/phospholipid mixed micelles and that water soluble (e.g., ethanol) and amphiphilic (e.g., surfactants) components are less capable of enhancing the solubilisation capacity of these systems (at least post-digestion) when compared with more non polar material (i.e., lipids). This is consistent with previous studies that have shown that the solubility of danazol is greatly enhanced in simulated intestinal medias containing long-chain fatty acids and monoglycerides when compared with intestinal medias containing only bile salts and phospholipids (4,50); and that the patterns of solubilisation of danazol can be correlated with the concentration of long-chain fatty acids and monoglycerides present in the aqueous phase of in vitro models of lipid digestion (19). Surprisingly in the latter study a correlation was not evident for probucol (Log P≈10) suggesting that the process is, at least to some extent, drug specific.
Although lipid digestion products have been shown to play a major role in the solubilisation of lipophilic drugs via the formation of mixed micelles, little is known as to the mechanism by which non-ionic surfactants interact with bile salts mixed micelles and the possible effect of lipase-mediated digestion on their solubilisation capacity. In this regard, the poor solubilisation capacity observed for Cremophor EL may reflect its apparent susceptibility to lipase-mediated digestion (as suggested by the release of fatty acids observed on in vitro digestion of F4 (containing 65% w/w Cremophor EL and 35% w/w ethanol)). The hydrolysis of Cremophor EL by pancreatic lipase/colipase has previously been reported by Sek et al. (37) and might result in the production, post digestion, of colloidal species with reduced solubilisation capacity when compared with the colloidal species formed on dispersion of the formulations under non digesting conditions.
In conclusion, the data obtained in these studies highlight the importance of consideration of the effect of lipid digestion on drug solubilisation and drug disposition in the GIT and confirm the utility of in vitro lipid digestion models to assist in the design of lipid-based formulations. More specifically the data suggest that the inclusion of high quantities of Cremophor EL and co-solvent in an attempt to increase drug load in the formulations and to facilitate rapid emulsification and the production of small particle size dispersions may lead to a reduction in oral bioavailability. Conversely, it appears that higher quantities of long-chain lipid more effectively prevent drug precipitation in the GIT and lead to greater increases in oral bioavailability. The data also suggest that non-ionic surfactants such as Cremophor EL may be susceptible to lipase-mediated digestion and that this in turn may affect their capacity to enhance solubilisation in vivo. The potential impact of lipase-mediated digestion on the solubilisation capacity of non-ionic surfactants is currently under investigation.
References
A. J. Humberstone and W. N. Charman. Lipid-based vehicles for the oral delivery of poorly water soluble drugs. Adv. Drug Deliv. Rev. 25:103–128 (1997).
T. Gershanik and S. Benita. Self-dispersing lipid formulations for improving oral absorption of lipophilic drugs. Eur. J. Pharm. Biopharm. 50:179–188 (2000).
M. Lindstrom, H. Ljusberg-Wharen, and K. Larsson. Aqueous lipid phases of relevance to intestinal fat digestion and absorption. Lipids 16:749–754 (1981).
G. A. Kossena, B. J. Boyd, C. J. H. Porter, and W. N. Charman. Separation and characterization of the colloidal phases produced on digestion of common formulation lipids and assessment of their impact on the apparent solubility of selected poorly water-soluble drugs. J. Pharm. Sci. 92:634–648 (2003).
J. R. Robinson. Semi-solid formulations for oral drug delivery. B.T. Gattefosse 89:11–13 (1996).
S. A. Charman, W. N. Charman, M. C. Rogge, T. D. Wilson, F. J. Dutko and C. N. Pouton. Self-emulsifying drug delivery systems: formulation and evaluation of an investigational lipophilic compound. Pharm. Res. 9:87–93 (1992).
N. H. Shah, M. T. Carjaval, C. I. Patel, M. H. Infeld, and A. W. Malick. Self-emulsifying drug delivery systems (SEDDS) with polyglycolyzed glycerides for improving in vitro dissolution and oral absorption of lipophilic drugs. Int. J. Pharm. 106:15–23 (1994).
D. J. Hauss, S. E. Fogal, J. V. Ficorilli, C. A. Price, T. Roy, A. A. Jayaraj, and J. J. Keirns. Lipid-based delivery systems for improving the bioavailability and lymphatic transport of a poorly water-soluble LTB4 inhibitor. J. Pharm. Sci. 87:164–169 (1998).
J. Y. Kim and Y. S. Ku. Enhanced absorption of indomethacin after oral or rectal administration of a self-emulsifying system containing indomethacin to rats. Int. J. Pharm. 194:81–89 (2000).
H.-J. Kim, K. A. Yoon, M. Hahn, E.-S. Park, and S.-C. Chi. Preparation and in vitro evaluation of self-microemulsifying drug delivery systems containing Idebenone. Drug Dev. Ind. Pharm. 26:523–529 (2000).
T. R. Kommuru, B. Gurley, M. A. Khan, and I. K. Reddy. Self-emulsifying drug delivery systems (SEDDS) of coenzyme Q10: formulation development and bioavailability assessment. Int. J. Pharm. 212:233–246 (2001).
C.-K. Kim, Y.-J. Cho, and Z.-G. Gao. Preparation and evaluation of biphenyl dimethyl dicarboxylate microemulsions for oral delivery. J. Control. Release 70:149–155 (2001).
B. K. Kang, J. S. Lee, S. K. Chon, S. Y. Jeong, S. H. Yuk, G. Khang, H. B. Lee, and S. H. Cho. Development of self-microemulsifying drug delivery systems (SMEDDS) for oral bioavailability enhancement of simvastatin in beagle dogs. Int. J. Pharm. 274:65–73 (2004).
P. Li, A. Ghosh, R. F. Wagner, S. Krill, Y. M. Joshi, and A. T. M. Serajuddin. Effect of combined use of nonionic surfactant on formation of oil-in-water microemulsions. Int. J. Pharm. 288:27–34 (2005).
J.-Y. Hong, J.-K. Kim, Y.-K. Song, J.-S. Park, and C.-K. Kim. A new self-emulsifying formulation of itroconazole with improved dissolution and oral absorption. J. Control. Release 110:332–338 (2006).
J.-P. Reymond and H. Sucker. in vitro model for ciclosporin intestinal absorption in lipid vehicles. Pharm. Res. 5:673–676 (1988).
K. J. MacGregor, J. K. Embleton, J. E. Lacy, E. A. Perry, L. J. Solomon, H. Seager, and C. W. Pouton. Influence of lipolysis on drug absorption from the gastro-intestinal tract. Adv. Drug Deliv. Rev. 25:33–46 (1997).
C. J. H. Porter and W. N. Charman. in vitro assessment of oral lipid based formulations. Adv. Drug Deliv. Rev. 50:S127–S147 (2001).
N. H. Zangenberg, A. Mullertz, H. G. Kristensen, and L. Hovgaard. A dynamic in vitro lipolysis model. II: evaluation of the model. Eur. J. Pharm. Sci. 14:237–244 (2001).
H. Ljusberg-Wahren, F. S. Nielsen, M. Brogard, E. Troedsson, and A. Mullertz. Enzymatic characterization of lipid-based drug delivery systems. Int. J. Pharm. 298:328–332 (2005).
A. Dahan and A. Hoffman. Use of a dynamic in vitro lipolysis model to rationalize oral formulation development for poor water soluble drugs: correlation with in vivo data and the relationship to intra-enterocyte processes in rats. Pharm. Res. 23:2165–2174 (2006).
L. Sek, C. J. H. Porter, A.-M. Kaukonen, and W. N. Charman. Evaluation of the in-vitro digestion profiles of long and medium chain glycerides and the phase behaviour of their lipolytic products. J. Pharm. Pharmacol. 54:29–41 (2002).
C. J. H. Porter, A. M. Kaukonen, A. Taillardat-Bertschinger, B. J. Boyd, J. M. O’Connor, G. A. Edwards, and W. N. Charman. Use of in vitro lipid digestion data to explain the in vivo performance of triglyceride based lipid formulations for the oral administration of poorly water-soluble drugs: studies with Halofantrine. J. Pharm. Sci. 93:1110–1121 (2004).
C. J. H. Porter, B. Boyd, A. M. Kaukonen, G. A. Edwards, and W. N. Charman. Susceptibility to lipase-mediated digestion reduces the oral bioavailability of danazol after administration as a medium chain lipid-based microemulsion formulation. Pharm. Res. 21:1405–1412 (2004).
J. O. Christensen, K. Schultz, B. Mollgaard, H. G. Kristensen, and A. Mullertz. Solubilisation of poorly water-soluble drugs during in vitro lipolysis of medium- and long-chain triacylglycerols. Eur. J. Pharm. Sci. 23:287–296 (2004).
M. Devani, M. Ashford, and D. Q. M. Craig. The emulsification and solubilisation properties of polyglycolysed oils in self-emulsifying formulations. J. Pharm. Pharmacol. 56:307–316 (2004).
R. Subramanian, R. Subhabrata, S. K. Ghosal, R. Bhadra, and S. P. Moulik. Formulation design of self-emulsifying drug delivery systems for improved oral bioavailability of celecoxib. Biol. Pharm. Bull. 27:1993–1999 (2004).
V. Bakatselou, R. C. Oppeneim, and J. B. Dressman. Solubilization and wetting effects of bile salts on the dissolution of steroids. Pharm. Res. 8:1461–1469 (1991).
L. Sek, C. J. H. Porter, and W. N. Charman. Characterisation and quantification of medium chain and long chain triglycerides and their in vitro digestion products, by HPTLC coupled with in situ densitometric analysis. J. Pharm. Biomed. Anal. 25:651–661 (2001).
G. A. Kossena, W. N. Charman, B. J. Boyd, D. E. Dunstan, and C. J. H. Porter. Probing drug solubilization patterns in the gastrointestinal tract after administration of lipid-based delivery systems: a phase diagram approach. J. Pharm. Sci. 93:332–348 (2004).
S.-M. Khoo, A. J. Humberstone, C. J. H. Porter, G. A. Edwards, and W. N. Charman. Formulation design and bioavailability assessment of lipidic self-emulsifying formulations of Halofantrine. Int. J. Pharm. 167:155–164 (1998).
D. W. Hay, M. J. Cahalane, N. Timofeyeva, and M. C. Carey. Molecular species of lecithins in human gallbladder bile. J. Lipid Res. 34:759–768 (1993).
W. C. Duane, R. L. Ginsberg, and L. J. Bennion. Effects of fasting on bile acid metabolism and biliary lipid composition in man. J. Lipid Res. 17:211–219 (1976).
J. E. Staggers, O. Hernell, R. J. Stafford, and M. C. Carey. Physical-behavior of dietary and biliary lipids during intestinal digestion and absorption. 1. Phase behavior and aggregation states of model lipid systems patterned after aqueous duodenal contents of healthy adult human beings. Biochemistry 29:2028–2040 (1990).
M. J. Groves and D. A. de Galindez. The self-emulsifying action of mixed surfactants in oil. Acta Pharm. Suec. 13:361–372 (1976).
R. N. Gursoy and S. Benita. Self-emulsifying drug delivery systems (SEDDS) for improved oral delivery of lipophilic drugs. Biomed. Pharmacother. 58:173–182 (2004).
L. Sek, B. J. Boyd, W. N. Charman, and C. J. H. Porter. Examination of the impact of a range of Pluronic surfactants on the in vitro solubilisation behaviour and oral bioavailability of lipidic formulations of atovaquone. J. Pharm. Pharmacol. 58:809–820 (2006).
L. Erlich, D. Yu, D. A. Pallister, R. S. Levinson, D. G. Gole, P. A. Wilkinson, R. E. Erlich, L. E. Reeve, and T. X. Viegas. Relative bioavailability of danazol in dogs from liquid-filled hard gelatin capsules. Int. J. Pharm. 179:49–53 (1999).
N. H. Zangenberg, A. Mullertz, H. G. Kristensen, and L. Hovgaard. A dynamic in vitro lipolysis model. I: controlling the rate of lipolysis by continuous addition of calcium. Eur. J. Pharm. Sci. 14:115–122 (2001).
C. W. Pouton. Self-emulsifying drug delivery systems: assessment of the efficiency of emulsification. Int. J. Pharm. 27:335–348 (1985).
M. G. Wakerley. Self-emulsifying drug delivery systems based on nonionic surfactant-oil mixtures, Ph.D. Thesis, University of Bath, 1989.
M. J. Groves and R. M. A. Mustafa. Measurement of the ‘spontaneity’ of self-emulsifiable oils. J. Pharm. Pharmacol. 26:671–681 (1974).
D. Q. M. Craig, S. A. Barker, D. Banning, and S. W. Booth. An investigation into the mechanisms of self-emulsification using particle size analysis and low frequency electric spectroscopy. Int. J. Pharm. 114:103–110 (1995).
M. Groves, R. M. A. Mustafa, and J. E. Carless. Phase studies of mixed phosphated surfactants, n-hexane and water. J. Pharm. Pharmacol. 26:616–623 (1974).
P. P. Constantinides. Lipid microemulsions for improving drug dissolution and oral absorption: physical and biopharmaceutical aspects. Pharm. Res. 12:1561–1572 (1995).
P. P. Constantinides and J.-P. Scalart. Formulation and physical characterization of water-in-oil microemulsions containing long- versus medium-chain glycerides. Int. J. Pharm. 158:57–68 (1997).
M. M. Nerurkar, P. S. Burton, and R. T. Borchardt. The use of surfactants to enhance the permeability of peptides through caco-2 cells by inhibition of an apically polarized efflux system. Pharm. Res. 13:(1996).
M. Martin-Facklam, J. Burhenne, R. Ding, R. Fricker, G. Mikus, I. Walter-Sack, and W. E. Haefeli. Dose-dependent increase of saquinavir bioavailability by the pharmaceutic aid cremophor EL. Br. J. Clin. Pharmacol. 53:576–581 (2002).
K. Bogman, Y. Zysset, L. Degen, G. Hopfgartner, H. Gutmann, J. Alsenz, and J. Drewe. P-glycoprotein and surfactants: effect on intestinal talinolol absorption. Clin. Pharmacol. Ther. 77:24–32 (2005).
V. H. Sunesen, B. L. Pedersen, H. G. Kristensen, and A. Müllertz. in vivo in vitro correlations for a poorly soluble drug, danazol, using the flow-through dissolution method with biorelevant dissolution media. Eur. J. Pharm. Sci. 24:305–313 (2005).
Acknowledgments
Funding from Capsugel, division of Pfizer, is gratefully acknowledged. We also thank Dr. Karen White for technical assistance with the bioavailability study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuiné, J.F., Charman, W.N., Pouton, C.W. et al. Increasing the Proportional Content of Surfactant (Cremophor EL) Relative to Lipid in Self-emulsifying Lipid-based Formulations of Danazol Reduces Oral Bioavailability in Beagle Dogs. Pharm Res 24, 748–757 (2007). https://doi.org/10.1007/s11095-006-9194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9194-z