ABSTRACT
Purpose
To determine distribution and deposition of Technosphere® Insulin (TI) inhalation powder and the rate of clearance of fumaryl diketopiperazine (FDKP; major component of Technosphere particles) and insulin from the lungs.
Methods
Deposition and distribution of 99mpertechnetate adsorbed onto TI immediately after administration using the MedTone® inhaler was quantified by gamma-scintigraphy. Clearance from the lungs was studied in a second experiment by serial bronchoalveolar lavage (BAL) after administration of TI inhalation powder and assay of the recovered fluid for FDKP and insulin.
Results
Following inhalation, ~60% of radioactivity (adsorbed on TI) emitted from the inhaler was delivered to the lungs; the remainder of the emitted dose was swallowed. Clearance from the lung epithelial lining fluid (ELF) of FDKP and insulin have a half-life of ~1 hour.
Conclusion
TI inhalation powder administered via the MedTone inhaler was uniformly distributed throughout the lungs; ~40% of the initial cartridge load reached the lungs. Insulin and FDKP are quickly cleared from the lungs, mainly by absorption into the systemic circulation. The terminal clearance half-life from the lung ELF, estimated from sequential BAL fluid measurements for both components, was ~1 hour. Since there is an overnight washout period, the potential for accumulation on chronic administration is minimal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Fumaryl diketopiperazine (FDKP) is a proprietary (MannKind Corporation, Valencia, CA, USA) novel excipient that is the primary component of Technosphere microparticles. FDKP is highly soluble in water at neutral and basic pH. Under acidic pH (<5.2), FDKP undergoes intermolecular self-assembly and crystallizes into Technosphere microparticles, which are highly porous (internal porosity of ~70%) with a median aerodynamic diameter of 2 to 2.5 μm (10% of the particles are <1 μm, 90% <5 μm), which is within the respirable range for particles (1,2). Adsorption of therapeutic agents, including peptides and proteins, such as insulin, glucagon-like peptide 1, and calcitonin, onto these microparticles produces dry powder formulations that, when dosed by oral inhalation, enable the delivery of that agent to the large absorptive area of the lung (1). Technosphere® Insulin (TI) inhalation powder (Afrezza®; MannKind Corporation, Valencia, CA, USA) is a dry powder formulation of recombinant human insulin adsorbed onto the Technosphere (FDKP) particles. The dry powder formulation is predominantly composed of insulin and FDKP (1:9 ratio by dry weight) with residual amounts of water and polysorbate 80. Upon inhalation using a breath-powered, unit-dose inhaler (MedTone®; MannKind Corporation, Valencia, CA, USA), the Technosphere microparticles dissolve rapidly at the physiological pH in the lungs, allowing absorption of insulin and FDKP into the systemic circulation with a time to maximum drug concentration (tmax) of 15 and 10 min, respectively (2).
It was hypothesized that upon inhalation (a) TI is distributed and deposited uniformly in both lungs and (b) both components of TI, insulin and FDKP, are rapidly absorbed into the systemic circulation, leading to rapid clearance from the lungs.
The ideal experimental design to study the distribution and clearance of a drug administered to the lungs would be to covalently label the drug with a tag that is visualized non-invasively. This method was not used for the following reasons. It requires at least two days to form TI inhalation particles from insulin plus Technosphere particles; therefore, TI is not amenable to a positron emission tomographic labeling. The use of a gamma label such as 125I on the insulin molecule would, following proteolysis, become labeled metabolite and no longer insulin. For the carrier, FDKP, the use of this gamma emitter attached to this small molecular weight compound would change the properties of the molecule and impact its ability to self-aggregate into the Technosphere particle. If particles form, their aerodynamics, ability to adsorb proteins, and rapid dissolution would also be affected. Because of these limitations, separate studies were designed to test each hypothesis.
To determine the distribution and deposition of TI in the lungs, nanoparticles (calculated mean particle size of 110 nm) of 99mTechnetium (99mTc) were adsorbed onto TI inhalation particles and were visualized after inhalation using gamma-scintigraphy. The amount of radioactivity in the oropharynx, lungs, and stomach was quantified using the output from the gamma camera and corrected for each subject using their attenuation factor for each anatomical segment.
To determine the clearance of the components of TI from the lungs, the concentration of insulin and FDKP was measured in the bronchoalveolar lavage (BAL) fluid before and at various time points after inhalation of TI. A composite curve was then constructed based on the mean data from multiple subjects, which enabled the calculation of the insulin and FDKP elimination half-lives from the lung ELF.
MATERIALS AND METHODS
Study Conduct and Subject Consent
Both studies were approved by the ethics committee or institutional review board and conducted according to current International Conference on Harmonisation Guidelines for Good Clinical Practice, the Principles of the Declaration of Helsinki, and all other applicable national and local regulations. Written informed consent was obtained from each subject before initiating any study-related activity.
Preparation of 99mTc-Labeled Microparticles and Validation of Radiolabeling
Before labeling, three cartridges were randomly selected and the aerodynamic particle size distributions were determined using an Andersen Cascade Impactor (Mark II, Copley Scientific, Nottingham, UK) (3). The inhaler was attached to the impactor and the drug dispensed by a constant airflow through the device, which comprises a prefilter and eight sizing stages. The aerosol stream passes through each stage, and particles with the same inertia impact remain on a particular stage, while smaller particles pass onto the next impaction stage. Following powder discharge, the stages were then disassembled, the particle amount (by mass) deposited on the various stages, was measured, and the percentage of total mass deposited on all stages was calculated (4).
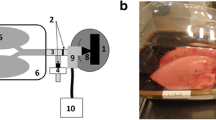
Ultrafine (nm) aerosol particles of 99mpertechnetate from a Mallinckrodt generator were passed into a nebulizer chamber containing TI inhalation powder. The TI inhalation powder and the 99mTc were allowed to “mix” for 60 sec as a nebulized cloud (4). The system was allowed to equilibrate to atmospheric conditions. The nebulized “mixing” and equilibration procedure was then repeated four more times. After the final equilibration, the powder was removed from the chamber and hand-filled into cartridges (5 mg/cartridge) using an S2 flow bench. The radioactivity (kBq) of every cartridge was measured using a gamma-scintillation counter to confirm that all cartridges contained an equal amount of radiolabeled material. The cartridges were stored at room temperature until inhalation, which was completed for all five subjects within 2 h of the radiolabeling procedure. Three cartridges were randomly selected, and the aerodynamic particle size distributions were determined as described above for the unlabeled material. Following powder discharge, the cascade impactor was disassembled, and the material deposited on each stage was analyzed for mass of material and radiolabel content. The percentage of total material on each stage was calculated for both radioactivity and mass (4). If the distribution of radioactivity and mass across all the stages was dissimilar, this would provide evidence that the radiolabel was not associated with the TI particles or the association was somehow dependent upon the TI aerodynamic particle size.
Determination of Distribution and Deposition of TI in Lungs
Healthy subjects (three males, two females; mean age 27 ± 1 years; mean BMI 23 ± 3 kg/m2) participated in the study. On the morning of the study day, each subject underwent pulmonary function testing (PFT), which included forced expiratory volume in 1 s (FEV1), inspiratory vital capacity (IVC), specific airway resistance (sRAW), mid-expiratory flows at 25%, 50% and 75% of forced vital capacity (MEF25%FVC, MEF50%FVC, MEF75%FVC, respectively) (5). One to 2 h before test article dosing, a standardized breakfast (500 kcal) was provided to mitigate the risk of hypoglycemia after the administration of TI. Subjects inhaled the 99mTc-TI inhalation powder from a single cartridge using the MedTone inhaler. Subjects were instructed to inhale fast and hard for 5 s and then hold their breath for another 5 s. This was done while seated with their back in front of a gamma camera (time point zero). Posterior views of oropharynx, lungs, and stomach were obtained at the end of the inhalation. Each image, starting at time zero, had an acquisition time of 1 min. A total of four images were obtained over the first 5 min after dosing. The radioactivity in the left lung, right lung, oropharynx, and stomach was quantified for each region after correction for background activity and tissue attenuation (using the standard attenuation technique, which considers the thickness of the subject’s chest and lung, stomach, and head to obtain individual attenuation factors) (4). All calculations of particle deposition (radioactivity) were based on the average of the first three images.
PFT was repeated at the conclusion of the radioactivity scans. Serial blood samples were collected before and after TI administration and analyzed for serum glucose and insulin concentrations.
A ventilation scan was performed after completion of dosing, gamma imaging, and post-dose PFT. For the ventilation scan, while sitting in front of the gamma camera, the subjects were asked to breathe normally for 1 to 2 min while inhaling radioactive tracer gas (81mKrypton) from a gas generator (KryptoScan [61Rb/61mKr]–Generator, Mallinckrodt Medical GmbH, D-53773 Hennef, Germany) to define the gas distribution in the lungs for each subject.
The total (T) amount of 99mTc-TI inhalation powder in each cartridge was determined by direct measurement of radioactivity via scintillation counting.
The total amount of 99mTc-TI inhalation powder that was not delivered (Tndel) was calculated using the following formula:
where CPI is the post-inhalation residual radioactivity in the cartridge, DPI is the post-inhalation residual radioactivity in the device, and F is the post-TI administration radioactivity captured on a filter when the subject exhales.
The total amount of 99mTc-TI inhalation powder delivered to the subject (TD) was calculated using the following formula:
where T is the pre-inhalation total radioactivity in the cartridge, and Tndel is defined in Eq. 1. The amount of radioactivity detected in each of the organs (Rorgan) was the product of the direct measurement via the gamma camera and the attenuation factor for each of the organs and determined as per the following:
where R is the radioactivity measured by the gamma camera, and A is the individual’s attenuation factor for the organ/site of interest. The total amount of measured radioactivity (Tm), corrected with the attenuation factors, is the sum of Rorgan for all organs/sites \( \left( {{{\text{T}}_{\text{m}}} = \sum {\text{A}}*{\text{R}}} \right) \).
The percentage of delivered dose for each organ is \( \left( {{{\text{R}}_{\text{organ}}}/{{\text{T}}_{\text{m}}}} \right)*{1}00 \).
BAL Study (Clinical Trial.gov Identifier NCT00757367)
Since the Technosphere particles dissolve rapidly in the moist, pH-neutral environment of the lungs, 99mTc rapidly disassociates from the TI particles and its components. Thus, tracking radioactivity at time points beyond the first few minutes after inhalation would assess clearance from the lungs of the dissolved 99mTc only and not the actual radiolabeled 99mTc-TI particles. Therefore, the concentration of insulin and FDKP were measured in the BAL fluid at multiple time points following TI inhalation to determine their clearance from the lungs.
Another group of healthy adult volunteers (one female, three males in each of the three groups [N = 12], mean age 32 ± 7 years; mean BMI 26 ± 2 kg/m2) participated in this study and underwent two serial bronchoscopies (using flexible bronchoscope model P-10, Olympus America Inc, Melville, NY, USA) to collect samples of BAL fluid. Samples were collected from the right middle lobe during the first bronchoscopy and from the left lower lobe during the second bronchoscopy. All subjects received a single dose of 20-mg TI inhalation powder (60-U insulin) using the MedTone inhaler. Subjects were randomized to one of three groups. For group 1, BAL was performed at 0.5 and 6 h post-administration of the TI inhalation powder. For group 2, BAL was performed at 4 and 8 h post-administration of the TI inhalation powder. For group 3, BAL was performed at −0.5 (pre-dose) and 12 h post-dose. At each time point for each subject, two separate BALs with 50-ml aliquots of pre-warmed normal saline from the same lung segment were performed and treated as separate BAL fluid samples for analysis. The BAL fluid samples were stored on ice until centrifuged (within 1 h of collection), and the supernatant was stored frozen at −20°C until analysis.
Blood samples were drawn at 30 min and immediately before inhalation of TI powder (time [t] = 0), and then at 15, 25, 55, 115, 175, 235, 295, 355, and 475 min post-administration. A drop of this blood was used to determine glucose concentration (glucose meter) and the value used to adjust the glucose infusion rate as necessary to maintain blood glucose between 80 and 150 mg/dL. The remainder of the sample was allowed to clot, and the sera were stored frozen at −20°C until analyzed for insulin and FDKP concentrations.
FDKP concentrations were determined in serum and BAL fluid using a sensitive and specific, validated liquid chromatography-tandem mass spectrometry method (1–10,000 ng/ml with dilutions, serum; 10–10,000 ng/ml with dilutions for BAL). Serum insulin concentration was measured by electrochemiluminescent immunoassay utilizing the Roche E170 autoanalyzer (Roche Diagnostics, Indianapolis, IL, USA) with a validated range for quantification from 0.5 to 400 μU/ml. Insulin concentrations in BAL fluid were determined with a commercially available ELISA (incorporating polyclonal antibodies; human insulin ELISA kit, Linco, Millipore, St. Charles, MO, USA) with a validated range with dilutions of 2 to 10,000 μU/ml.
A blood sample was obtained 5 min before each bronchoscopy to determine blood urea concentration. The ratio of concentration of urea in blood (UreaBlood) to that in the BAL fluid (UreaBAL) was used to correct for the dilution effects inherent within the BAL procedure (6) by using the following equation modified from Gotfried et al. (7):
where Concinsulin/FDKP is the concentration of insulin or FDKP in the epithelial lining fluid (ELF) or BAL fluid.
RESULTS
Deposition and Distribution of the 99mTc-Labeled TI Inhalation Particles
Five healthy subjects participated in the study. All five subjects had normal lung function tests at baseline (FEV1, IVC, sRAW, MEF25%FVC, MEF50%FVC, and MEF75%FVC). There were no clinically meaningful changes in any of the PFT parameters post-dose relative to pre-dose.
The aerodynamic particle-size distribution, as measured by cascade impactor, remained comparable before and after the radiolabeling of the TI particles (Fig. 1), indicating that no appreciable change in particle size occurred upon 99mTc radiolabeling. The distribution of radioactivity closely matched the weight distribution. There appeared to be some preference of the 99mTc nanoparticles to associate with the smaller TI particle sizes (μm), which led to a small increase in specific activity with decreased TI particle size. However, given the minimal radioactivity in the fractions less than 0.65 microns (no indication of free 99mTc nanoparticles [0.11 μm]), the data would indicate essentially quantitative association with TI particles.
Distribution of particle sizes from the Andersen Cascade Impactor as assessed by the percentage of total mass (pre- and post-labeling) and the percentage of total radioactivity (post-labeling) on individual stages. The aerodynamic particle size normally defined as the respirable fraction is between 0.5 and 5.8 μm (12).
Administration of the 99mTc adsorbed onto TI particles to healthy subjects via the MedTone inhaler resulted in the particles being homogeneously deposited in both lungs, as shown in a representative scintigraph (Fig. 2). Approximately 20% of the amount loaded into the cartridge was found deposited in the oropharynx (Table I) after inhalation (8). This material would subsequently be swallowed into the gastrointestinal tract (Fig. 2, white areas). The left image on Fig. 2 represents the 81mKrypton gas ventilation scan for this individual (8). The distribution of the 99mTc-labeled TI is similar to the gas distribution seen with the 81mKrypton gas.
The mean amount of Technosphere particles emitted from the device was ~65%, based on the difference of the initial radioactivity minus the residual activity left in the inhalation device and cartridge after administration. The measurement of the radioactivity by the gamma camera and the use of the appropriate attenuation factors for the different anatomical sections (4) provided the ability to quantify the distribution of the Technosphere particles immediately after inhalation. Table I shows the distribution based on the percentage of the original dose in the cartridge and as a percentage of the calculated total delivered material. A mean of ~60% of the emitted dose reaches the lungs with minimal difference between the left and right lung. The remainder is swallowed and enters the gastrointestinal tract.
BAL Study
The urea-corrected insulin and urea-corrected FDKP concentrations and percentages of the initial mean concentration (30 min) in the lungs are presented in Table II and graphically in Figs. 3 and 4 (9,10). The inhaled insulin is rapidly cleared from the lungs, with concentrations falling below the limit of quantification (2 μU/ml) by 12 h. FDKP is similarly cleared rapidly from the lung and is also near the limit of quantification (10 ng/ml) in most samples by 12 h.
Using the slope of the log mean values from 4 h post-dosing and beyond (see Figs. 3 and 4, insert), the calculated terminal half-life for insulin and FDKP in the lungs is ~1 h based on the BAL sampling. The corresponding mean serum insulin and FDKP concentration-time profiles are presented in Fig. 5.
DISCUSSION
When the 99mTc-TI inhalation powder is administered using the MedTone® breath-powered, high-resistance inhaler, the mean amount of Technosphere particles emitted from the inhaler in this study was ~65%, based on the difference of the initial radioactivity minus the residual activity left in the inhalation device after administration. Approximately 60% of the emitted dose is delivered to the lungs with a homogeneous distribution bilaterally throughout the lungs. The remaining ~40% of the emitted material is not bioavailable as it is ultimately swallowed and enters the gastrointestinal tract, where neither the insulin nor the carrier molecule (FDKP) is absorbed (11). Although the plasma was analyzed for insulin, the low dose administered (due to radioactivity exposure limit) and the meal prior to dosing made it impossible to accurately determine the contribution of the exogenously administered insulin to the total insulin concentration.
Technosphere particles are highly porous, crystalline microparticles with a median diameter of ~2 to 2.5 μm (10% of the particles are <1 μm, 90% <5 μm). Particles with aerodynamic particle size between 0.5 and 5.8 μm are considered in the respirable range and well suited for deposition into the distal lungs (12). The aerodynamic size distribution of the radiolabeled TI powder via the Andersen Cascade Impactor, as measured by weight, was comparable to the particle size of the unlabeled TI inhalation powder and the majority of material within the respirable range. While there were small differences in the distribution of radioactivity and weight on the individual plates after labeling, the percentage of total for both weight and radioactivity across the respirable fraction (0.5–5.8 μm) is comparable. Additionally, <0.2% radiolabeled material was in the 0 to 0.43-μm stage, indicating that the radioactivity was associated with the TI inhalation powder and not free 99mTc radioactivity. Although it is theoretically possible that the nanoparticles agglomerated to more than 110 nmeter, their original size during the labeling process, this has not been seen in any other study we have conducted using this methodology.
The MedTone inhaler is a breath-powered device. As the subject inhales from the mouthpiece of the inhaler, the inspiratory effort and inhaler-supplied flow resistance create an air flow through the system, as described by the Bernoulli principle. A limitation of the study was that the inspiratory flow or the pressure drop during the inhalation of TI powder was not measured. In a study evaluating the inspiratory flow profile in subjects with diabetes, peak flow rates achieved through the MedTone system averaged ~26.4 ± 6.06 L/min (13). Furthermore, as the scintigraphy planar images are only two-dimensional, the limitation of the analysis is the lack of resolution to determine precise depth of deposition within the peripheral airways/distal airways of the lungs (i.e., terminal conducting bronchioles vs. acinus/alveolar regions).
Since the radiolabel was not covalently bound to the particles, and the particles themselves dissolve almost immediately after delivery to the lungs, it is not possible to use the scintigraphy analysis to determine the clearance of insulin and FDKP from the lungs. Analysis of BAL fluid after administration of 60 U of TI inhalation powder (approximately the mean of the meal time doses used in the phase three program) was used to determine the rate of disappearance from the lungs. The volume of lavage fluid recovered is variable, leading to differential dilution within the recovered BAL fluid. The ratio of urea concentration in BAL fluid to the serum urea concentration can be used to normalize the insulin and FDKP concentrations since, with urea being freely permeable, the concentration within the serum and epithelial lining fluid is assumed to be the same (6,7). It has been well established that the insulin and FDKP serum tmax are between 9 and 15 min (2,14) as opposed to the 45 to 60 min for other inhaled insulins (15,16). Due to experimental design, the earliest time of bronchoscopy post-inhalation was deemed to be 30 min. As expected, the peak concentrations in the lungs were the first time point. The initial high concentration found in the lungs rapidly decreases as both insulin and FDKP are absorbed into the systemic circulation, from which the latter is excreted unchanged in the urine (11). The clearance from the lung ELF, as measured by serial BAL, is quite rapid with an apparent terminal half-life of ~1 h for insulin and the carrier FDKP. Both insulin and FDKP concentrations in BAL fluid were at the lower limits of quantification by 12 h, which was <0.3% of the value at 30 min post-inhalation. In comparison, the amount of insulin remaining in BAL fluid at 12 h after inhalation of another inhaled insulin (Exubera), which has a serum tmax of ~55 min (16) and are the only data reported for an inhaled insulin, was estimated to be ~8% of the last dose (17). This methodology is only minimally invasive, but does not measure components taken up by the cells of the lungs. Lombry and colleagues instilled FITC-insulin into the lungs of rats and, following serial sacrifices, looked at uptake by the cells of the lungs by confocal microscopy (18). They showed FTIC-insulin in and around cells of the lungs at 30 min, but not within the alveolar macrophages, and no indication of the label by 6 h post-instillation. This is consistent with the results presented here.
Because of the limited blood sampling taken within this study, extensive serum pharmacokinetic analysis could not be performed. However, the data as reported are consistent with what has been reported in other pharmacokinetic and pharmacokinetic/pharmacodynamic studies where extensive blood sampling was conducted (2,11,14). The serum half-life of FDKP from this study (approximately 140 min) is equivalent to the 150 min half-life reported after IV administration (11), indicating that serum clearance is not absorption dependent.
CONCLUSION
TI inhalation powder administered via the MedTone inhaler is uniformly distributed throughout the lungs with ~40% of the initial cartridge load reaching the lungs. The components of TI inhalation powder―insulin and FDKP—are quickly cleared from the lungs, mainly by absorption into the systemic circulation. The clearance half-life from the lung ELF, as measured by serial BAL, for insulin and FDKP was demonstrated to be ~1 h. Since there is an overnight washout period, the potential for accumulation on chronic administration is minimal.
Abbreviations
- Tc:
-
99mTechnetium
- AUC0–t :
-
area under the insulin concentration-time curve from 0 to time t
- BAL:
-
bronchoalveolar lavage
- ELF:
-
epithelial lining fluid of the lungs
- FDKP:
-
fumaryl diketopiperazine
- FEV1 :
-
forced expiratory volume in 1 s
- IVC:
-
inspiratory vital capacity
- MEF25%FVC :
-
mid-expiratory flow at 25% of forced vital capacity
- MEF50%FVC :
-
mid-expiratory flow at 50% of forced vital capacity
- MEF75%FVC :
-
mid-expiratory flow at 75% of forced vital capacity
- PFT:
-
pulmonary function testing
- sRAW :
-
specific airway resistance
- T:
-
total amount of radioactivity in the cartridge
- TI:
-
Technosphere Insulin
- tmax :
-
time to maximum observed drug concentration
- Tndel :
-
total amount of 99mTc-TI inhalation powder that is not delivered to the body
REFERENCES
Leone-Bay A, Grant M. Technosphere technology: a platform for inhaled protein therapeutics. ONdrugDelivery. 2006:11–18. Available from: www.Ondrugdelivery.com.
Richardson PC, Boss AH. Technosphere® Insulin technology. Diab Technol Ther. 2007;9 Suppl 1:S65–72.
United States Pharmacopeia–National Formulary (USP–NF). Aerosols, Nasal Sprays, Metered-Dose Inhalers, and Dry Powder Inhalers <601>. The United States Pharmacopeia USP 29; The National Formulary NF 24 through First Supplement. Rockville, MD: U.S.P.C. Inc.
Dunbar C, Scheuch G, Sommerer K, DeLong M, Verma A, Batycky R. In vitro and in vivo dose delivery characteristics of large porous particles for inhalation. Int J Pharm. 2002;245(1–2):179–89.
American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med. 1995;152:1107–36.
Rennard S, Basset G, Lecossier D, O’Donnell K, Pinkston P, Martin P, et al. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol. 1986;60(2):532–8.
Gotfried M, Danzinger L, Rodvold K. Steady-state plasma and intrapulmonary concentrations of leofloxin and ciprofloxin in healthy human subjects. Chest. 2001;119(4):1114–22.
Pfützner A, Sommerer K, Meyer T, Haussermann S, Flacke F, Steiner S, et al. Lung distribution of radiolabeled Technosphere/Insulin. Diabetes. 2003;52 Suppl 1:A107 [abstract 459-P].
Cassidy J, Marino M, Amin N, Gotfried M, Baughman R, Gray M, et al. Lung deposition and absorption of AFRESA (Technosphere Insulin) [abstract 433-P]. Diabetes. 2009;58 Suppl 1:A115.
Gotfried M, Cassidy J, Marino M, Amin N, Baughman R, Gray M, et al. Lung deposition and absorption of insulin from Technosphere insulin [abstract 955]. Diabetologia. 2009;52 Suppl 1:S375.
Potocka E, Cassidy J, Haworth P, Heuman D, van Marle S, Baughman R. Pharmacokinetic characterization of the novel pulmonary delivery excipient fumaryl diketopiperazine. J Diab Sci Technol. 2010;4(5):1164–73.
Okamoto H, Todo H, Iida K, Danjo K. Dry powders for pulmonary delivery of peptides and proteins. Inhaled Insulin: Lung Deposition and Clearance. 2002;20:71–82.
Smutney CC, Friedman EM, Polidoro JM, Amin N. Inspiratory efforts achieved in use of the Technosphere® Insulin inhalation system. J Diab Sci Technol. 2009;3(5):1–8.
Rave K, Potocka E, Boss AH, Marino M, Costello D, Chen R. Pharmacokinetics and linear exposure of AFRESA™ compared with the subcutaneous injection of regular human insulin. Diab Obes Metab. 2009;11(7):715–20.
Muchmore D, Silverman B, de la Pena A, Tobin J. The AIR® inhaled insulin system: system components and pharmacokinetics/glucodynamic data. Diab Technol Ther. 2007;9 Suppl 1:S41–7.
Rave K, Bott S, Heineman L, Sha S, Becker R, Willaviza S, et al. Time action profile of inhaled insulin in comparison with subcutaneously injected insulin lispro and regular human insulin. Diabetes Care. 2005;28(5):1077–82.
Brain J, Finch G, Riese R, Schwartz P, Teeter J. Trough insulin levels in bronchoalveolar lavage following inhalation of human insulin (Exubera®) in patients with diabetes mellitus [abstract A53]. Am J Resp Crit Care Med. 2008;177:A616.
Lombry C, Edwards D, Preat V, Vanbever R. Alveolar macrophages are a primary barrier to pulmonary absorption of macromolecules. Am J Physiol Lung Cell Mol Physiol. 2004;286(5):L1002–8.
ACKNOWLEDGMENTS
The authors extend their appreciation to Dr. Andreas Pfützner, University of Applied Sciences, Bingen, Germany, the principal investigator, and the staff at Inamed, Gauting, Germany, for the excellent conduct of the radiolabeled study; the research coordinators at Pulmonary Associates, Phoenix, AZ, USA, and the Endoscopy Department of John C. Lincoln North Mountain Hospital, Phoenix, AZ, USA, for conducting a quality bronchoscopy study; and the staffs at BARC, Lake Success, NY, USA (serum insulin), and QPS, Newark, DE, USA (serum and BAL FDKP and BAL insulin), for their excellent bioanalytical analysis of the samples; and Sungita Patel, who excelled as the clinical monitor for the BAL study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cassidy, J.P., Amin, N., Marino, M. et al. Insulin Lung Deposition and Clearance Following Technosphere® Insulin Inhalation Powder Administration. Pharm Res 28, 2157–2164 (2011). https://doi.org/10.1007/s11095-011-0443-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-011-0443-4