ABSTRACT
Purpose
Nonadherence to antipsychotic medications is a major obstacle preventing optimal outcomes for patients with schizophrenia. Extended release systems exist in the form of depot injections, but these formulations exhibit several disadvantages. To address these concerns, we previously demonstrated proof of concept for an antipsychotic implant containing risperidone and the biodegradable polymer poly(lactic-co-glycolic) acid (PLGA).
Methods
We build upon recently published data by utilizing a scalable single-screw extrusion system for the production of PLGA-risperidone implants. Implants were composed of 40% risperidone and 60% PLGA, with varying ratios of lactide to glycolide (50:50, 65:35, 75:25 or 85:15). Risperidone release was assessed in vitro and in vivo in rats, and Level A, B and C correlations (IVIVCs) attempted for all. Bioavailability was verified with locomotor testing
Results
Level B analysis yielded the greatest correlation between in vitro and in vivo data (R 2 = 0.9425), while Level C yielded the lowest (R 2 = 0.8336). Although, based on qualitative results, a Level A correlation was not achieved, it did produce an R 2 of 0.9261. Locomotor testing demonstrated that peak serum concentrations coincide with significant reductions in activity.
Conclusion
Data demonstrate the applicability of our modeling system and advance long-term, implantable antipsychotics toward clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Schizophrenia is a chronic and highly debilitating mental illness afflicting 1.1% of the U.S. population (1). Recent studies have estimated the U.S. economic burden of schizophrenia to be $63 billion, a cost that is disproportionately large compared to diseases of similar prevalence (2,3). Two major factors contributing to this excessive economic burden are lost income and frequent hospitalizations, secondary to the fact that schizophrenia remains a life-long disorder with a significant rate of relapse in a majority of patients (4). Although antipsychotic drugs have demonstrated therapeutic efficacy at improving clinical outcomes and reducing relapse rates, due to factors such as impaired cognition and lack of insight, medication nonadherence is a major obstacle in the proper treatment of schizophrenia (5). Studies have shown that nonadherence rates range from 24 to 74% and that nonadherent patients may be 4.89 times more likely to relapse and therefore be rehospitalized (6–9).
In an effort to reduce nonadherance, depot formulations of numerous antipsychotic drugs have been created, such as Haldol Decanoate. A major advantage of these formulations is that they have been associated with reduced relapse rates compared to oral formulations (10). In addition, depot injections bypass first-pass metabolism, permitting lower drug content to be administered with comparable therapeutic efficacy, thus reducing the risk of adverse events such as hepatotoxicity and hyperprolactinemia (11–14). Despite these advantages, depot formulations have a number of potential drawbacks. For instance, not all antipsychotic drugs are capable of being chemically synthesized into decanoate esters, the chemical form required for slow-release injections. In addition, depot injections can cause prolonged pain at the injection site, are irreversible and often require several days to reach therapeutic levels (15). To combat these problems while still maintaining the benefits of an extended-release system, we have proposed and demonstrated proof of concept of an implantable antipsychotic delivery system using the encapsulation matrix poly(lactic-co-glycolic acid) (PLGA) (16,17).
PLGA is an FDA-approved, biodegradable polymer that is physically strong and highly biocompatible (18,19). A number of medications have utilized PLGA or other biocompatible polymers to achieve extended release, including naltrexone, levodopa and ganciclovir (20–22). The atypical antipsychotic risperidone remains the most logical candidate for a PLGA-antipsychotic implant because it demonstrates high efficacy, tolerability in the subcutaneous space, lowest dose per implant size, stability at both physiological and low pHs, and has advantages, and disadvantages, relative to the side effect profiles of other agents (16,23–26). It was also the most frequently prescribed antipsychotic in 2002 and the second-most prescribed in 2003 and 2004, suggesting that it is chosen frequently by physicians and patients alike (IMS Database).
Previous authors have noted a paucity of published IVIVC data for implantable drug delivery systems (27). However, correlation analysis for oral medications has long been established and widely accepted (28). To address this gap, the current study attempts level A, B and C in vitro–in vivo correlations (IVIVCs) and demonstrates behavioral effects of PLGA-risperidone implants produced via a scalable single-screw extrusion system. According to the United States Pharmacopeia (USP), IVIVC levels decrease in acceptability and preference from A to C (29). In this paper, we will present all three levels so as to portray comprehensive models and release characteristics. Level C IVIVC utilizes a single-point relationship between in vitro and in vivo data, such as dissolution at a given time and maximum serum concentration (C max), respectively. Level B correlations rely on statistical moment analyses and compare mean dissolution time (MDT) in vitro with mean residence time (MRT) in the body. Even though this level correlation, like Level C, is dependent upon one single variable, it is generally considered valuable when performing extended release studies. Finally, Level A analyses are point-to-point comparisons between in vitro and in vivo release. Our data provide further evidence for the feasibility of a long-term PLGA-risperidone delivery system and advance this concept toward application in a clinical setting.
MATERIALS AND METHODS
Implant Fabrication
Cylindrical implants were fabricated from a PLGA Medisorb biodegradable polymer (Lakeshore Biomaterials, Birmingham, AL) and risperidone (supplied by the NIMH drug synthesis program). PLGA pellets were ground into powder using an electronic crushing mill (IKA Laboratory Equipment, Wilmington, NC) and collected after sifting through a 500 µm sieve (Daigger Lab Equipment & Supplies, Vernon Hills, IL). Based on previously published results, drug load was fixed at 40% by mass, and polymer composition was varied as a function of lactide-to-glycolide ratio (16). The different polymers used were 50:50, 65:35, 75:25 and 85:15 (molar ratio of lactide:glycolide) PLGA. Drug and polymer mixtures were extruded into rod-shaped implants using a single-screw Microtruder at approximately 100°C (RCP 0375, Randcastle Extrusion Systems, Inc., Cedar Grove, NJ). Microtruder parameters included 3/8″ screw and 0.078″ die diameters. Negative control rods with 0% risperidone by mass were fabricated in the same fashion. Following fabrication, half of all implants placed in vitro and all implants placed in vivo were gamma sterilized by Steris Isomedix Services (Morton Grove, IL). Sterilization parameters included an average exposure time of 164 min and an absorbed dose of between 4.8 and 5.1 kGy. Half of all in vitro implants remained non-sterilized for the assessment of potential effects of the sterilization procedure on release profiles.
Drug Dosage
In humans, daily risperidone dosages range from two to 16 mg/ kg, with motor side effects increasing in a linear fashion given doses above 6 mg/ kg (30). Based on this clinical data and the effects of chronic risperidone administration in rats, we chose a daily estimated drug dose of 3 mg/ kg (31–33). Total drug load was calculated based on a 400-g animal for a total duration of either 30 (for 50:50 implants) or 150 days (for all other implants), resulting in risperidone doses of 36 or 180 mg, respectively. Each implant was then cut to a length of 1–2.5 cm, and a total mass of 90 to 450 mg (based on 40% drug load by mass).
In Vitro Release Studies
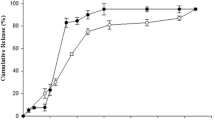
In vitro dissolution data was collected for all four implant types so that we could assess the potential effects of lactide-to-glycolide ratio (polymer composition) on risperidone release. The in vitro dissolution method has been previously validated using a variety of compounds (16,17,34,35). This method is based on but not identical to those employed by the USP. Assay accuracy was 87.6 ± 4%, and assay precision was 97.4 ± 1.6%. Three replicates of each implant type were placed in separate amber, light-safe bottles containing phosphate-buffered saline (PBS) (200 ml for 50:50 implants; 2,400 ml for all others; pH 7.4) and onto a shaker (40 rpm, 37°C). The volume in the in vitro system was adjusted in proportion to the amount of drug released so as to ensure against solution saturation with drug. Two-hundred-µl aliquots were removed from each bottle for analysis by UV spectrophotometry (Bio-Tek Instruments, Inc., Winooski, VT). Risperidone concentration was read at 280 nm and quantified relative to a standard curve, which ranged from 0.0019 to 0.25 mg/ ml. Two-hundred µl of fresh PBS were added back to each bottle following analyses to maintain constant volume. Samples were assessed approximately every other day until release closely approached optimal levels, at which time they were assessed weekly (time 0, 3 h, 6 h, days 1, 2, 3, 4, 7, 9, 11, 14, 16, 18, 21, 23, 25, 28, 30, 32, 35, 36, 39, 42, 50, 56, 63, 70, 77, 84, 92, 98, 106 and 112). Drug stability under these conditions has been previously demonstrated (16). These studies also revealed no significant differences in daily release values between sterilized and non-sterilized implants.
In Vivo Studies
Animals
For pharmacokinetic analyses and behavioral studies, 50 male Sprague-Dawley rats (weighing approximately 300 g upon arrival) were obtained from Charles River Laboratories (Wilmington, MA). Of these rats, 15 each were given implants containing either 50:50, 65:35 or 75:25 PLGA, and five were given 85:15. Within each group of 15, 12 animals received 40% risperidone implants, and three received negative controls; of the five 85:15 PLGA implants, four were composed of 40% risperidone and one PLGA alone. An n of 12 was chosen for the 50:50, 65:35 and 75:25 implants based on Institutional Animal Care and Use Committee (IACUC) restrictions on blood collection frequency per animal. Thus, within each group of 15 were three rotating groups of four experimentally treated and one control-treated animal(s). Because samples were taken with less frequency from animals given 85:15 implants, they were not subject to such restrictions. Rats were housed two per cage and acclimated to the housing facility for 1 week prior to implantation, after which each animal was housed singly. Water and standard rodent chow were available ad libitum. All protocols were approved by the IACUC and were in compliance with University Laboratory Animal Resources (ULAR) guidelines.
Implant Insertion
All animals received either 40% risperidone or negative control implants. Subjects were anesthetized with isoflurane, and skin was shaved prior to cleaning the area with betadine and alcohol. Implants were placed in the subcutaneous space on the dorsal surface with a 10-gauge trochar (Innovative Research of America, Sarasota, FL), and the implant site was closed with a single stitch. All methodologies for implant insertion were consistent with previously published procedures in mice (16). Animals were monitored throughout the course of the study for severe weight loss, signs of distress and adverse reactions at the implant site. No subjects exhibited any of the aforementioned changes following the procedure.
Release Studies
To evaluate implant release profiles in vivo, 1-ml samples of blood were collected once (for 85:15 PLGA implants) or twice (50:50, 65:35 and 75:25 implants) per week until serum concentrations returned to basal levels (4 h, day 1, 3, 7, 10, 14, 17, 21, 24, 28, 31, 35, 43, 45, 49, 52, 57, 60, 63, 66, 70, 77, 84, 87, 91, 94, 98, 101, 105 and 112). Samples were obtained via lateral tail vein blood collection. Previous studies from our group have demonstrated mass balance in implants removed from mice at various intervals (16). Samples (40% risperidone n = 4; negative control n = 1 per time point) were centrifuged for 35 min at 3,500 RPM, leaving at least 200 µl of serum for analysis. Centrifugation was performed in 10-ml glass BD Vacutainer venous blood collection tubes containing no additives or silicon. Solid phase extraction (SPE) and subsequent HPLC analyses were conducted on serum samples according to previously published methodologies (16). Assay accuracy was 95.1 ± 0.9%, and assay precision was 98.0 ± 0.9%.
In Vitro–In Vivo Correlations (IVIVCs)
For the most basic Level C IVIVCs, we calculated the following in vitro parameters: time required to dissolve 50% (T 50%) and 63.2% (T 63.2%) of drug (relative to maximum observed) and cumulative dissolution at day 24 (D 24 d). In vivo parameters included in this analysis were maximum serum drug concentration (C max) and corresponding time to maximum concentration (T max). All calculations were based upon composite, average concentration-time profiles for a given implant type. For Level B moment analyses, true mean dissolution time (MDT) in vitro was estimated using the equation
where M ∞ is the asymptotic amount of drug that is dissolved, based on the assumption of complete release (36). ABC is the area under the cumulative dissolution profile calculated using the trapezoidal rule. The trapezoidal rule was also used to calculate in vivo area under the concentration-time curve (AUC) from zero to infinity, or in this case back down to zero. Mean residence time of the drug could then be determined according to the equation
where AUMC is equal to the first moment of the concentration-time curve. To carry out Level A analyses, we first followed the Wagner-Nelson method to determine fraction absorbed from in vivo plasma concentrations, assuming a one-compartment model. The following equation was utilized for each assayed time point:
where C P is equal to plasma drug concentration at time t, and k e represents the elimination constant calculated based on plasma risperidone levels following intravenous (IV) administration in rats. Wagner-Nelson absorption fractions were then compared to plasma density functions (PDFs) calculated via the Weibull distribution function
where α and β were determined for each implant type based on the minimum squared difference between plasma drug concentration and the Weibull fit (Fig. 1). All four implant types exhibited correlations greater than 99%, thus confirming the accuracy of these two in vivo modeling systems. Finally, fractional in vivo release derived from the Weibull distribution was compared to in vitro release at identical time points. Pearson correlation coefficients were then calculated for each implant ratio.
Modeled in vivo release profiles for 50:50, 65:35, 75:25 and 85:15 PLGA/ risperidone implants. All modeling was performed according to the “IVIVC” subsection of “Materials and Methods”. A release ratio, or fractional absorption value, of one represents the maximum observed serum drug concentration according to the modeling system. The profiles show that, as expected, release was delayed as the proportion of lactide to glycolide increased.
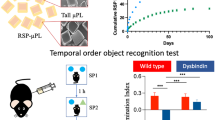
Locomotor Testing
The effects of continual risperidone treatment on locomotor activity were assessed for 30 min in animals that received 65:35 or 75:25 PLGA implants (65:35 drug-treated n = 6–7; 75:25 drug-treated n = 4–7; control n = 4–6). Testing was performed on days 11, 25, 42, 53, 67, 81, and 95. Single animals were placed in opaque holding containers (19.5′ l × 13′ w × 15.75′ h) containing fresh bedding, and TopScan recording software (Clever Systems, Inc., Reston, VA) was used to document and measure locomotor activity as previously published (37). Containers were cleaned with 100% ethanol, and bedding was changed after each animal was removed. Locomotor activity was assessed approximately once every 2 weeks. Individual one-way analyses of variance (ANOVAs) were performed on data gathered at each time point. For the purpose of analyses, animals were divided into three groups according to the following implant types: negative controls (65:35 and 75:25 pooled), 65:35 PLGA-risperidone, and 75:25 PLGA-risperidone. To identify differences between negative control and 40% risperidone implants, significant results were subsequently submitted to Fisher LSD post hoc analyses using Statistica 6.1 (Statsoft, Inc., Tulsa, OK).
RESULTS
IVIVC Models
As Fig. 1 shows, we first modeled in vivo drug release for each of the four implant types observed. These profiles demonstrate that 50:50, 65:35, 75:25 and 85:15 implants reached complete release on, approximately, days 35, 63, 84 and 112, respectively. From these and our in vitro data, we were then able to perform Level C IVIVCs and calculate the following parameters: in vitro D 24 days, T 50% and T 63.2%, and in vivo C max and T max (Fig. 2A & B). As expected, such correlations confirmed that an increase in the proportion of lactide in PLGA temporally extended release profiles and decreased daily release values. This relationship was determined based on results showing that T 50%, T 63.2%, and T max increased with increasing lactide concentration and, inversely, that D 24 d and C max decreased (Table I). Linear correlations, displayed in Fig. 2, demonstrate that in vitro results in our Level C analyses were least predictive of in vivo outcomes (R 2 = 0.8336–0.9167). Level B analysis revealed the highest level of predictability of the two lower-level correlations (R 2 = 0.9425). Such results suggest that, as anticipated, analysis between mean dissolution time (MDT) and mean residence time (MRT) is more desirable than between other temporal parameters. Level A analysis was performed on composite data from all four implant types, yielding an R 2 value of 0.9261 (Fig. 3) (F(1, 126) = 1578.88, p < 0.0000001). However, based on the qualitative pattern of this fit, we conclude that a level A correlation was not achieved.
Level B and C IVIVCs for all four risperidone implant types. Level C IVIVCs depicting in vivo D 24 days (A) or T max (B) and C max or either T 50% or T 63.2% , in vitro. These analyses yielded the lowest degrees of correlation, with R 2 values between 0.8336 and 0.9167. C Level B analysis depicting Mean Residence Time (MRT) in vivo versus Mean Dissolution Time (MDT) in vitro produced a higher R 2 of 0.9425.
Locomotor Testing
The effects of chronic risperidone treatment on locomotor activity were evaluated in rats that received 65:35 or 75:25 PLGA implants. One-way ANOVAs on data collected from animals that had either negative control implants or either formulation of risperidone revealed significant differences on days 25, 42 and 53 (day 25: F(2, 13) = 9.14, p = 0.003; 42: F(2, 13) = 4.34, p = 0.036; 53: F(2, 16) = 4.89, p = 0.022). Post hoc analyses showed that rats given risperidone implants mixed with 65:35 PLGA exhibited significantly reduced locomotor activity compared to negative controls on all 3 days (day 25: p = 0.003, MS = 9774E3, df = 13; 42: p = 0.012, MS = 9039E3, df = 13; 53: p = 0.016, MS = 2545E4, df = 16). Rats treated with 75:25 PLGA-risperidone implants exhibited a trend toward decreased activity on day 42 (p = 0.079, MS = 9039E3, df = 13) and a significant reduction on day 53 (p = 0.011, MS = 2545E4, df = 16). An ANOVA on day 67 revealed a trend toward significance (F(2, 15) = 2.65, p = 0.1), and post hoc analyses demonstrated that rats with 75:25 PLGA-risperidone implants still displayed significantly reduced activity (p = 0.036, MS = 2745E4, df = 15). This trend in the ANOVA still existed on day 81 (F(2, 16) = 3.37, p = 0.060), but the difference between 75:25 PLGA-risperidone-implanted rats and negative controls was no longer statistically significant (p = 0.055, MS = 3318E4, df = 16) (Fig. 4B). In Fig. 4, we display both serum drug concentration and change in locomotor activity. Regression analysis showed that values for locomotor activity and serum concentrations were significantly correlated among test groups (F(1,12) = 8.84, p < 0.012).
A Serum concentrations and B locomotor activity for rats treated with either 65:35 or 75:25 PLGA-risperidone implants. As the figure shows, peak serum drug concentrations and the largest decreases in locomotor activity generally occur at the same time, though this is more evident for 75:25 implants. Error bars represent mean ± SEM. Asterisks indicate significant reductions in activity relative to control-treated animals (p ≤ 0.05), and cross indicates a trend toward a reduction (p ≤ 0.1). Values for locomotor activity and serum concentrations were significantly correlated among test groups (F(1,12) = 8.84, p < 0.012).
DISCUSSION
The current paper utilizes a scalable single-screw extrusion method for the production of a novel long-term antipsychotic release system. Implants were produced by creating a uniform mixture of the popular antipsychotic risperidone and different compositions of the matrix polymer poly(lactic-co-glycolic acid) (PLGA). Implants were then sterilized and analyzed both in vitro and in vivo to assess the accuracy of our in vitro modeling system. Three different level correlations were performed based on the data gathered: Levels C, B and A. Level C and B correlations rely on the comparison of single in vitro and in vivo parameters, while Level A analysis is based directly upon each of the assayed time points. Level A analysis is therefore able to account for both qualitative patterns of release and their temporal positioning.
One of the greatest concerns when creating IVIVCs for implant formulations is the burst effect, in which a high concentration of drug is released during a short period of time. Such a burst generally occurs within 24 h of either in vitro or in vivo placement, but may also occur later after, for instance, a certain threshold of solvent is absorbed by the implant. Several studies have sought to minimize this burst, and it appears that surface extraction and surface-preferential crosslinking are two particularly effective methods for achieving this goal (38). Additionally, several manufacturing variables, such as solute size, drug partitioning and drying time, can effect release characteristics (39). The burst effect was not observed for any of our implant types, though, as anticipated, there was a period of increased release around T 50%. This increase was greatest for 50:50 implants and decreased with increasing lactide concentration (Fig. 1).
Such a period of high drug release could be managed in a variety of different ways. First, a depot injection of risperidone (which is generally administered once every 2 weeks) could be concurrently administered when patients are first treated with a set of implants. This would provide the appropriate dosage of drug during the relatively low level of release throughout the first 14 days of treatment. Additionally, because risperidone release from these implants is dependent upon the ratio of lactide to glycolide in the PLGA polymer, one would be able to alter release patterns by simply modifying that ratio. For instance, by using a PLGA mixture with a greater percentage of glycolide than lactide, maximal risperidone release could potentially be achieved closer to the date of implantation (day 0). If release from such implants were not too rapid, then this could negate the need for a supplementary depot injection. Previous studies have demonstrated similar release profiles with haloperidol, as well as how release profiles vary for different drugs from PLGA matrices (34,35). Future studies could address the extent to which the IVIVC models in the current study apply to other drugs and polymeric systems.
By combining all four of the implants studied in this paper, we could theoretically achieve release with only two peaks in drug concentration over the course of about 4 months. This ratio of peaks and troughs per time period is in stark contrast to that given daily oral administration, in which two peaks are observed within only 2 days. The continual release demonstrated by our implants provides several advantages over antipsychotics currently on the market. One of the key advantages is that nonadherence is the major hurdle preventing the optimal treatment of patients with schizophrenia. The implants described in this paper could improve adherence by providing a mechanism for patients to make their treatment decisions with their physician during periods of health, rather than having to make a daily choice, which can be particularly difficult during periods of symptom exacerbation (17). Because antipsychotic treatment is associated with decreased rates of relapse, prolonged periods of health would aid in the reduction of patient hospitalization and loss of function. Improved patient outcomes would also reduce the burden of medication monitoring and associated stressors for patients’ families and society as a whole.
CONCLUSION
In this report we have demonstrated the accuracy of our in vitro modeling system by performing IVIVCs of different polymer ratio implants and subsequent behavioral testing. We hope that such pharmacokinetic analyses advance this concept one step closer toward clinical relevancy, as there is undoubtedly a need within the mental health community for improved treatment options and outcomes.
REFERENCES
Siegel SJ, Dankert M, Phillips JM. Psychosis and schizophrenia (chapter 55). In: Waldman S, Terzic A, editors. Pharmacology and therapeutics: principles to practice. Philadelphia: Elsevier; 2008.
Wu EQ et al. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66(9):1122–9.
Rice DP. The economic impact of schizophrenia. J Clin Psychiatry. 1999;60 Suppl 1:4–6. discussion 28–30.
Crown WH et al. Hospitalization and total medical costs for privately insured persons with schizophrenia. Adm Policy Ment Health. 2001;28(5):335–51.
Kane JM. Utilization of long-acting antipsychotic medication in patient care. CNS Spectr. 2006;11(12 Suppl 14):1–7. quiz 7–8.
Lieberman JA et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23.
Gilmer TP et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161(4):692–9.
Robinson D et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56(3):241–7.
Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull. 1995;21(3):419–29.
Schooler NR. Relapse and rehospitalization: comparing oral and depot antipsychotics. J Clin Psychiatry. 2003;64 Suppl 16:14–7.
Melkersson K. Differences in prolactin elevation and related symptoms of atypical antipsychotics in schizophrenic patients. J Clin Psychiatry. 2005;66(6):761–7.
Melkersson KI, Hulting AL, Brismar KE. Elevated levels of insulin, leptin, and blood lipids in olanzapine-treated patients with schizophrenia or related psychoses. J Clin Psychiatry. 2000;61(10):742–9.
Ozcanli T et al. Severe liver enzyme elevations after three years of olanzapine treatment: a case report and review of olanzapine associated hepatotoxicity. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(6):1163–6.
Benazzi F. Risperidone-induced hepatotoxicity. Pharmacopsychiatry. 1998;31(6):241.
Yadalam KG, Simpson GM. Changing from oral to depot fluphenazine. J Clin Psychiatry. 1988;49(9):346–8.
Rabin C et al. In vitro and in vivo demonstration of risperidone implants in mice. Schizophr Res. 2008;98(1–3):66–78.
Siegel SJ et al. Surgically implantable long-term antipsychotic delivery systems for the treatment of schizophrenia. Neuropsychopharmacology. 2002;26(6):817–23.
Kitchell JP, Wise DL. Poly(lactic/glycolic acid) biodegradable drug-polymer matrix systems. Methods Enzymol. 1985;112:436–48.
Schakenraad JM et al. In vivo and in vitro degradation of glycine/DL-lactic acid copolymers. J Biomed Mater Res. 1989;23(11):1271–88.
Sharon AC, Wise DL. Development of drug delivery systems for use in treatment of narcotic addiction. NIDA Res Monogr. 1981;28:194–213.
Sabel BA et al. Levodopa delivery from controlled-release polymer matrix: delivery of more than 600 days in vitro and 225 days of elevated plasma levels after subcutaneous implantation in rats. J Pharmacol Exp Ther. 1990;255(2):914–22.
Okada H, Toguchi H. Biodegradable microspheres in drug delivery. Crit Rev Ther Drug Carrier Syst. 1995;12(1):1–99.
Janssen PA et al. Pharmacology of risperidone (R 64 766), a new antipsychotic with serotonin-S2 and dopamine-D2 antagonistic properties. J Pharmacol Exp Ther. 1988;244(2):685–93.
Davis JM, Chen N, Glick ID. A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry. 2003;60(6):553–64.
Nasrallah HA. The roles of efficacy, safety, and tolerability in antipsychotic effectiveness: practical implications of the CATIE schizophrenia trial. J Clin Psychiatry. 2007;68 Suppl 1:5–11.
Brown CS et al. Atypical antipsychotics: Part II: adverse effects, drug interactions, and costs. Ann Pharmacother. 1999;33(2):210–7.
Iyer SS, Barr WH, Karnes HT. Profiling in vitro drug release from subcutaneous implants: a review of current status and potential implications on drug product development. Biopharm Drug Dispos. 2006;27(4):157–70.
Amidon GL et al. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12(3):413–20.
United States Pharmacopeial Convention. The United States pharmacopeia. The national formulary, United States Pharmacopeial Convention: Rockville, Md., p. v.
Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151(6):825–35.
Naiker DV et al. Dose determination of haloperidol, risperidone and olanzapine using an in vivo dopamine D2-receptor occupancy method in the rat. Eur J Pharmacol. 2006;540(1–3):87–90.
Tarazi FI, Zhang K, Baldessarini RJ. Long-term effects of olanzapine, risperidone, and quetiapine on dopamine receptor types in regions of rat brain: implications for antipsychotic drug treatment. J Pharmacol Exp Ther. 2001;297(2):711–7.
Moran-Gates T et al. Effects of risperidone on dopamine receptor subtypes in developing rat brain. Eur Neuropsychopharmacol. 2007;17(6–7):448–55.
Metzger KL et al. Pharmacokinetic and behavioral characterization of a long-term antipsychotic delivery system in rodents and rabbits. Psychopharmacology (Berl). 2007;190(2):201–11.
Siegel SJ et al. Effect of drug type on the degradation rate of PLGA matrices. Eur J Pharm Biopharm. 2006;64(3):287–93.
Rinaki E, Dokoumetzidis A, Macheras P. The mean dissolution time depends on the dose/solubility ratio. Pharm Res. 2003;20(3):406–8.
Halene TB et al. Assessment of NMDA receptor NR1 subunit hypofunction in mice as a model for schizophrenia. Genes Brain Behav. 2009;8:661–75.
Huang X, Chestang BL, Brazel CS. Minimization of initial burst in poly(vinyl alcohol) hydrogels by surface extraction and surface-preferential crosslinking. Int J Pharm. 2002;248(1–2):183–92.
Huang X, Brazel CS. On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release. 2001;73(2–3):121–36.
ACKNOWLEDGEMENTS
Funding provided by NIMH Grant 5R01MH074672-04.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amann, L.C., Gandal, M.J., Lin, R. et al. In Vitro–In Vivo Correlations of Scalable PLGA-Risperidone Implants for the Treatment of Schizophrenia. Pharm Res 27, 1730–1737 (2010). https://doi.org/10.1007/s11095-010-0152-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0152-4