Abstract
Recent reports suggest declines in the age-specific risk of Alzheimer’s dementia in higher income Western countries. At the same time, investigators believe that worldwide trends of increasing mid-life modifiable risk factors [e.g., cardiovascular disease (CVD) risk factors] coupled with the growth of the world's oldest age groups may nonetheless lead to an increase in Alzheimer’s dementia. Thus, understanding the overlap in neuroanatomical profiles associated with CVD risk factors and AD may offer more relevant targets for investigating ways to reduce the growing dementia epidemic than current targets specific to isolated AD-related neuropathology. We hypothesized that a core group of common brain structural alterations exist between CVD risk factors and Alzheimer’s dementia. Two co-authors conducted independent literature reviews in PubMed using search terms for CVD risk factor burden (separate searches for ‘cardiovascular disease risk factors’, ‘hypertension’, and ‘Type 2 diabetes’) and ‘aging’ or ‘Alzheimer’s dementia’ with either ‘grey matter volumes’ or ‘white matter’. Of studies that reported regionally localized results, we found support for our hypothesis, determining 23 regions commonly associated with both CVD risk factors and Alzheimer’s dementia. Within this context, we outline future directions for research as well as larger cerebrovascular implications for these commonalities. Overall, this review supports previous as well as more recent calls for the consideration that both vascular and neurodegenerative factors contribute to the pathogenesis of dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
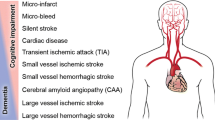
The relationship between vascular disease and Alzheimer’s dementia has been discussed for decades (de la Torre, 2010; Jellinger, 2010; Kalaria, 2010), with work from bench to bedside (de la Torre, 2010) attempting to elucidate the interplay of vascular dysfunction and dementia (see de la Torre, 2018 for review). As part of this larger corpus, it has been documented that mid-life, and to a lesser extent, late-life cardiovascular disease (CVD) risk factors increase the risk for and development of dementia including Alzheimer’s dementia (Beauchet et al., 2013; Bendlin et al., 2010; Li et al., 2016; Raz, Knoefel and Bhaskar, 2016; Suzuki et al., 2019; Tolppanen, Solomon, Soininen and Kivipelto, 2012). In fact, CVD risk factors are no longer seen as more relevant to vascular dementia as once thought, but rather reflective of cerebrovascular alterations that may not only contribute to Alzheimer’s dementia (Nelson, Sweeney, Sagare and Zlokovic, 2016), but may also be seen as a common etiology shared among all dementias (Raz et al., 2016). Yet drug development and recent NIA-AA research criteria for Alzheimer’s disease (Jack Jr. et al., 2018) continue to focus primarily on amyloid- or tau-based biomarkers despite the fact that they may not reflect the complete picture of neuropathological alterations present in individuals with Alzheimer’s dementia at death (Kapasi, DeCarli and Schneider, 2017; Yarchoan et al., 2012). For example, over 230 different combinations of neuropathologies that have been reported to date (Boyle et al., 2018). Thus, considering the potential overlap of brain structural alterations associated with CVD risk factors and Alzheimer’s dementia may offer relevant, more inclusive, targets for drug development and clinical trials, including trials of already available drugs on the market for CVD risk factor management (e.g., Sprint Mind Investigators for the SPRINT Research Group et al., 2019).
The two-hit vascular hypothesis for Alzheimer’s disease (Zlokovic, 2011) includes CVD risk factors as part of ‘hit one’ that leads to the blood-brain barrier dysfunction and reduced cerebral blood flow that precedes dementia, with ‘hit two’ characterized by an increase in beta-amyloid amplifying neuronal dysfunction, neurodegeneration and disease. As such, we reviewed the literature for commonalities between grey and white matter as well as subcortical structural alterations associated with CVD risk factors and Alzheimer’s dementia to better understand the structural commonalities of regional vulnerabilities associated with the early stages of disease. More specifically, two co-authors conducted independent literature reviews in PubMed using search terms for CVD risk factor burden (separate searches for ‘cardiovascular disease risk factors’, ‘hypertension’, and ‘Type 2 diabetes’) and ‘aging’ or ‘Alzheimer’s dementia’ with either ‘grey matter volumes’ or ‘white matter’. We hypothesized that our review of studies reporting regionally localized results would reveal a set of overlapping brain structural alterations across studies of CVD risk factors and Alzheimer’s dementia. Results of this review are placed within the larger context of the relationship between vascular disease and Alzheimer’s dementia. Additionally, we discuss future directions for structural neuroimaging research strategies incorporating commonalities across CVD risk factors and Alzheimer’s dementia for a more holistic approach to understanding cognitive aging and dementia. Lastly, we describe the larger cerebrovascular implications of this work. It is our belief that only within this more integrated framework to brain aging, i.e., one that considers a more complete picture of the neuroanatomical alterations associated not only with Alzheimer’s dementia but also CVD risk factors and how they relate to real-world cognitive outcomes, will we be able to move beyond increasingly isolated and unsuccessful clinical trials to slow and ultimately stop risk for and development of Alzheimer’s dementia.
Literature Review
Neuroimaging of Grey Matter and Subcortical Structures
Cardiovascular Disease Risk
Studies examining composite CVD risk factor burden scores that incorporate multiple risk factors such as hypertension, Type 2 diabetes mellitus, smoking, hypercholesterolemia, and obesity, report relationships between increased CVD risk factor burden and decreased regional grey matter and subcortical structures (Table 1, Column A). For example, increased CVD risk factor burden was associated with decreased frontal and more posterior regional brain volumes as well as hippocampal volumes across participants between the fourth to eight decades of life (Cardenas et al., 2012; Debette et al., 2011; Gonzales et al., 2017; Lamar et al., 2015; Leritz et al., 2011). A review of the literature by Friedman and colleagues further confirms that in individuals without a history of overt cardiovascular disease, the presence of CVD risk factors is associated with these same structural brain changes (Friedman et al., 2014). Lastly, cumulative CVD risk factor burden has also been associated with a reduction of subcortical volumes in the hippocampus, and several subcortical structures including the nucleus accumbens, caudate, putamen, pallidum, and thalamus (Cox et al., 2019). While composite CVD risk factor burden scores are useful in conceptualizing cumulative risk, they do not reveal the separate contributions of individual CVD risk factors such as hypertension and diabetes mellitus to grey matter structural alterations in the aging brain.
Mid-life CVD risk factors including hypertension and diabetes mellitus have been linked to late-life alterations in whole brain as well as regional grey matter and subcortical structures, with less, albeit still robust, evidence suggesting late-life CVD risk factors are also associated with late-life structural alterations (see Table 1, Column A and Friedman et al., 2014 for review). For example, hypertension has been associated with cross-sectional differences and increased rates of change in whole brain atrophy in older adults (Firbank et al., 2007; Wiseman et al., 2004) as well as specific hippocampal vulnerability (Firbank et al., 2007; Wiseman et al., 2004). In a qualitative review of approximately 30 studies conducted in mid- to late-life adults (i.e., 45 to 80 years of age), hypertension as well as higher blood pressure in individuals without hypertension were associated with reductions in frontal, parietal, and temporal lobe volumes as well as hippocampal volumes (Beauchet et al., 2013). More recently, an analysis of approximately 10,000 mid- to late-life participants in the UK Biobank revealed that hypertension was linked to alterations in global brain outcomes as well as regionally specific alterations within the frontal and temporal lobes and subcortical structures including the pallidum, accumbens, thalamus, putamen, hippocampus, and amygdala (Cox et al., 2019). A recent study in the mid-life CARDIA cohort confirmed the basal ganglia-thalamic signature of elevated blood pressure exposure (Jenkins et al., 2020).
Many of these same results have been reported for mid- and late-life adults with diabetes mellitus (see Table 1, Column A; and Moulton, Costafreda, Horton, Ismail and Fu, 2015 for review). Diabetes mellitus has been associated with decreased whole brain volumes, particularly grey matter volumes (Bryan et al., 2014; Reitz et al., 2017); an association recently highlighted in a systematic review (Wu, Lin, Zhang and Wu, 2017). Additionally, work detailing cerebral localization of diabetes mellitus associates has reported reductions within frontal and temporal regions, in the presence of mid- (e.g., Bruehl et al., 2009; Moran et al., 2013) as well as late-life diabetes mellitus (e.g, Erus et al., 2015; Kumar et al., 2008), although, more severe diabetes mellitus has been associated with smaller volumes of all lobes (Schneider et al., 2017). Regional implications of longer duration diabetes mellitus include middle and inferior frontal gyri, precentral and posterior cingulate cortices, as well as middle and inferior temporal cortices in young-old to older adults (Erus et al., 2015; Moran et al., 2013). There are also multiple reports of associations between diabetes mellitus and volumetric reductions in the limbic system (Erus et al., 2015) including the hippocampus (Cui, Abduljalil, Manor, Peng and Novak, 2014; Moran et al., 2013; Reitz et al., 2017; Roberts et al., 2014; Y. W. Zhang et al., 2015), the amygdala, as well as subcortical structures including the putamen (Cox et al., 2019; D. Cui et al., 2019), the caudate, thalamus, and nucleus accumbens (Chen et al., 2017; Cox et al., 2019). Thus, CVD risk factors combined or in isolation have been associated with reductions in several of the same brain regions, some of which are also implicated in risk for and development of Alzheimer’s dementia as outlined below.
Alzheimer’s Dementia Risk and Development
Initial studies as well as more recent work investigating risk for and development of Alzheimer’s dementia point to the importance of key brain regions to cognitive decline and incident dementia (Table 1, Column B). For example, volume loss in the hippocampus is either associated with or predictive of Alzheimer’s dementia (Apostolova et al., 2010; den Heijer et al., 2010; Fox et al., 1996; Zeifman et al., 2015). Furthermore, longitudinal staging of brain structural alterations suggest that early in the development of the disease, there is atrophy of the hippocampus and subsequent atrophic changes in the amygdala (Eskildsen et al., 2013). In fact, loss of hippocampal and amygdala volume along with volume loss within the posterior cingulate gyrus, the inferior parietal lobe and the superior frontal lobe appear to have better prognostic accuracy for conversion from an at-risk state of mild cognitive impairment (MCI) to Alzheimer’s dementia (Zeifman et al., 2015) when compared to clinical ratings scores used in the Alzheimer’s Disease Neuroimaging Initiative (ADNI: Aksu, Miller, Kesidis, Bigler and Yang, 2011). These results are consistent with the cortical signature of Alzheimer’s dementia put forth by Dickerson and colleagues (Dickerson et al., 2009) who reported alterations in the medial and inferior temporal lobes, posterior cingulate-precuneus, superior parietal, and superior and inferior frontal regions forming a structural phenotype of participants with Alzheimer’s dementia. This structural phenotype not only correlates with disease severity ante-mortem (Dickerson et al., 2009), but also mirrors the topography of neuropathology found post-mortem. Despite the anatomic similarities, relatively less work has been done comparing the neuroimaging phenotype of Alzheimer’s dementia with the neuroimaging phenotype of CVD risk factors in older adults.
Commonalities across CVD Risk Factors and Alzheimer’s Dementia
As a result of this review, several grey matter and subcortical structures appear to be consistently associated with CVD risk factor burden, hypertension, or diabetes mellitus, as well as Alzheimer’s dementia (Table 1). More specifically, 23 areas appeared to be commonly, congruently associated with our select indices of CVD risk and Alzheimer’s dementia. These areas include the superior frontal gyrus, inferior frontal gyrus (pars opercularis, pars triangularis, pars orbitalis), rostral and caudal middle frontal gyrus, caudal and rostral anterior, posterior, and isthmus cingulate cortex, entorhinal cortex, supramarginal gyrus, middle and inferior temporal gyrus, hippocampus, amygdala, superior and inferior parietal cortex, the basal ganglia (caudate, putamen, pallidum, and accumbens), and precuneus. Although other regions showed overlap, the congruence of these areas was not as consistent across all studies reviewed as the 23 regions listed above and outlined in Table 1. A recent empirical investigation of over 8000 participants in the UK Biobank to determine common, overlapping grey matter regions between modifiable risk factors for dementia and Alzheimer’s dementia further supported our decision making (Suzuki et al., 2019) as do reports that cardiovascular disease risk factors (Silbert et al., 2018), especially diabetes mellitus (Schneider et al., 2017; Zeifman et al., 2015; Y. Zhang et al., 2014), are associated with the cortical signature of Alzheimer’s dementia.
Neuroimaging of White Matter
Cardiovascular Disease Risk
CVD risk factor burden is also associated with white matter alterations (see Wassenaar, Yaffe, van der Werf and Sexton, 2019 for a recent review). In a large population-based lifespan sample, a cardiovascular disease risk score revealed a causal relationship between overall burden and white matter hyperintensities (Habes et al., 2016) and more nuanced diffusion-tensor imaging (DTI) derived white matter integrity (Habes et al., 2018). Furthermore, in large-scale studies of older adults, mid-life vascular risk exposure including hypertension, current smoking, and diabetes mellitus were associated with greater white matter hyperintensity volume (Debette et al., 2011) and reduced white matter tract integrity within both association and commissural fibers in late-life (de Groot et al., 2015). Lastly, a recent study reported that mid- as well as late-life cardiovascular disease risk factors commonly included in quantifications of total burden were associated with changes in white matter over time (Scharf et al., 2019).
Individually, hypertension and diabetes mellitus are associated with increased white matter hyperintensities (Debette et al., 2011; Firbank et al., 2007; Iadecola et al., 2016; Marseglia et al., 2019; Meusel et al., 2014) predominantly within parietal and frontal (for hypertension; Fennema-Notestine et al., 2016; Salvado et al., 2019) or temporal and frontal (for diabetes; Moran et al., 2013) white matter regions. Furthermore, DTI-derived fractional anisotropy also reveals a loss of white matter integrity associated with these same CVD risk factors (Gonzales et al., 2017; Haight et al., 2018; Hoogenboom et al., 2014; Jacobs et al., 2013). Research done in a cross-sectional study of late-middle-aged men found that individuals reporting a longer duration of hypertension showed lower DTI-derived measures of white matter integrity within several association fibers connecting anterior to posterior regions of brain including the inferior and superior longitudinal fasciculi (McEvoy et al., 2015) with more recent studies suggesting these associations may exist independent of age (Sabisz et al., 2019). Similar findings have been noted in more diverse samples both cross-sectionally (Gonzales et al., 2017; Kennedy and Raz, 2009) and longitudinally (Wang et al., 2015a).
There is increasing evidence suggesting that these white matter alterations may manifest earlier than originally thought. For example, investigators have shown tissue damage when investigating white matter integrity in 30–40 year old adults with elevated blood pressure (Munoz Maniega et al., 2017; Weinstein et al., 2015) and blood glucose (Maillard et al., 2012). These findings suggest that alterations to white matter integrity may manifest earlier putting, mid-life to young-old adults at increased risk for earlier pathological aging, lending credence to an emerging hypothesis that early effects on white matter integrity may confer a vulnerability across the lifespan (Jefferson, 2020). When coupled with findings relating CVD risk factors to alterations in regional white matter integrity that are also associated with risk for and development of Alzheimer’s dementia (see below), the assumption that CVD risk factors influence vascular forms of dementia exclusively is changing (Nelson et al., 2016; Raz et al., 2016), further supporting the role of CVD risk factors in dementia regardless of etiology (Hachinski, 2019; Nelson et al., 2016; Raz et al., 2016).
Alzheimer’s Dementia Risk and Development
Over the past two decades, a literature has emerged showing the importance of white matter alterations to risk for (Bangen et al., 2018; Bryan et al., 2014; Carmichael et al., 2010; Lee et al., 2016) and development of Alzheimer’s dementia (Delano-Wood et al., 2009; Libon et al., 2008; Price et al., 2012; Tosto et al., 2015). For example, periventricular white matter hyperintensities, more prominent in Alzheimer’s dementia than normal aging (Damulina et al., 2019; Sundar, Manwatkar, Joshi and Bhandarkar, 2019), appear early in the course of dementia with white matter damage moving more distally to include deep white matter and finally white matter closer to the cortex over time with increasing disease severity (Spilt et al., 2006; Zimmerman, Fleming, Lee, Saint-Louis and Deck, 1986). Although a recent study suggested that maternal family history of Alzheimer’s disease was associated with higher white matter hyperintensity volumes within temporal and occipital regions (Salvado et al., 2019), frontal (Kao, Chou, Chen and Yang, 2019) and parietal white matter have emerged in non-familial late-onset studies as key regions of vulnerability associated with Alzheimer’s dementia (Brickman, 2013; Kao et al., 2019). For example, white matter hyperintensity burden within frontal and parietal regions has been shown to associate with amyloid-PET in these same regions (Graff-Radford et al., 2019). Furthermore, higher parietal white matter hyperintensity volumes have been reported to predict increasing levels of CSF-derived t-tau (Tosto et al., 2015), and when combined with low baseline levels of t-tau led to faster rates of entorhinal cortex atrophy and faster conversion to Alzheimer’s dementia (Tosto et al., 2015). Superior and inferior parietal, as well as rostral and caudal middle frontal, supramarginal, and precuneus white matter hyperintensity burden appear to distinguish MCI and Alzheimer’s dementia (Lindemer et al., 2017a) with parietal white matter hyperintensity volume predicting Alzheimer’s dementia (Brickman et al., 2012; Brickman et al., 2015) and frontal, as well as temporal white matter hyperintensities pointing to a decreasing time-to-Alzheimer’s conversion (Lindemer, Greve, Fischl, Augustinack and Salat, 2017b).
Commonalities across CVD Risk Factors and Alzheimer’s Dementia
When taken together, the alterations of white matter, for example, regionally distributed white matter hyperintensities within the parietal lobe, appear to be associated with both CVD risk factor burden including hypertension and diabetes mellitus, as well as Alzheimer’s dementia (Table 2). While few studies noted a strong role for temporal lobe white matter alterations across disease states (Lindemer et al., 2017a), others have advocated for a shared vulnerability to white matter alterations within frontal as well as parieto-occipital white matter regions (Kao et al., 2019). Additionally, infarcts within select subcortical structures including the basal ganglia and caudate, reported for both CVD risk factor burden and Alzheimer’s disease (Olazaran et al., 2014), may disconnect temporal from frontal regions allowing for disruptions within either region to exert their effect (Catani and Mesulam, 2008; Geschwind, 1965a, 1965b).
Directions for Future Research and Larger Cerebrovascular Implications
The congruent alterations in grey matter, subcortical structures, as well as white matter discussed above suggests the need for a more integrated approach to structural neuroimaging that includes multi-modal capture and analytic integration of these distinct findings, both to understand the brain at a more holistic level, but also to decipher how CVD risk factors and Alzheimer’s dementia may be associated with similar brain regions and the role this may play on behavior. Thus, we will turn our attention away from a review of the literature to place findings of this review within a larger context, discuss future directions for research, and implications for the field.
Previous studies investigating cerebral hypo-perfusion, that is, decreased blood flow through the brain, as it relates to grey matter atrophy in risk for as well as development of Alzheimer’s dementia confirm results of this review as it relates to common regional involvement across vascular and Alzheimer’s disease processes (de la Torre, 2018) and suggest potential rationale for our noted regional congruence, a topic we will return to toward the end of this review. Using arterial spin-labeling investigators reported decreased regional cerebral blood flow within the posterior cingulate and precuneus across MCI and Alzheimer’s dementia compared to controls, as well as reductions in inferior parietal, superior temporal and frontal regions for Alzheimer’s dementia compared to MCI and controls (Dai et al., 2009). Interestingly, increases in rCBF in this same study were seen within multiple subcortical and basal ganglia structures including the hippocampus, amygdala, caudate, putamen, and global pallidus for MCI, suggesting an attempt at compensation for vulnerability in the at-risk stage (Dai et al., 2009). These results, and the results of similar such perfusion studies (see Montagne et al., 2016 for review), involve nearly all 23 regions highlighted by the current review. Thus, a link between the vascular components of Alzheimer’s dementia, established via rCBF and patterns of atrophy in Alzheimer’s dementia in past literature, is confirmed and extended to include congruent regions of involvement across CVD risk factors and Alzheimer’s dementia in the current manuscript.
In contrast to the multi-modal imaging across neurovascular dysfunction in Alzheimer’s dementia noted above, much of the work to date focused exclusively on structural brain aging, CVD risk factor burden, and Alzheimer’s dementia has focused on a single neuroimaging modality approach. This is despite the fact that the landscape of brain aging research is rapidly changing (e.g., Montagne et al., 2016) to incorporate a more nuanced approach to gray and white matter structures. Advances in image analytics, through the application of graph theory have made possible the ability to examine the structural connectivity of grey matter, subcortical structures or white matter as it relates to indices of interest (Rubinov and Sporns, 2010). These advanced neuroimaging methods allow analysis of brain structure in a more integrated form, including but not limited to system properties of how the brain exchanges information (efficiency), how strong connections are between brain regions (strength), how important regions are to effective network communication (hubness), and how groups of brain regions preferentially interact to form communities (modularity). Information on these metrics of brain network integrity may fill gaps in the literature related to the interplay of cortical grey matter, subcortical structures, and white matter brain structures common to CVD risk factor burden and risk for and development of Alzheimer’s dementia in older adults.
We believe one such approach to understand the interplay of grey matter, subcortical structures, and the white matter that connects them is via tract-based structural connectomics, that is, using the cortical grey matter and subcortical volumes common to CVD risk factor burden and risk for and development of Alzheimer’s dementia to determine the integrity of white matter tract-based streamlines connecting these brain regions. Within the normal aging literature, tract-based structural connectomics have been used to predict brain age (Lin et al., 2016), investigate regional importance for brain network efficiency, and particularly relevant to the results of the present review, better understand reductions in network strength between frontal and temporal regions (e.g., Zhao et al., 2015). Likewise, studies have used this analytic approach to outline regions critically important for efficient network communication (e.g., temporal and prefrontal, precentral and precuneus, superior and inferior parietal grey matter regions as well as limbic and basal ganglia structures) and the changes in such communication associated with normal aging (Betzel et al., 2014; Perry et al., 2015; Sun et al., 2015), MCI, and Alzheimer’s dementia (Daianu et al., 2015; Daianu et al., 2013; Jacquemont et al., 2017; Mallio et al., 2015; Nir et al., 2015; Yan et al., 2018). Many of these reported regional associations are those that show congruent alterations across CVD risk factors and risk for, as well as development of Alzheimer’s dementia as reported in the current review.
We recently took a more directed approach to tract-based structural connectomics as it relates to the 23 ROIs common to both CVD risk factors and Alzheimer’s dementia. In a community-based cohort of non-demented older adults (n = 94; ~68 years of age, ~29 on the MMSE). Our investigation (Boots et al., 2019) revealed that CVD risk factors differentially impact the efficiency and nodal strength of the tract-based structural connectome within these 23 ROIs in fully adjusted models that included a term for white matter hyperintensity burden (i.e., total volume). More specifically, higher CVD risk factor burden was associated with lower efficiency within the left hippocampus and right pars opercularis, and higher efficiency in the right supramarginal gyrus as well as lower nodal strength in bilateral rostral middle frontal gyri, bilateral hippocampi, the thalamus bilaterally, right pars triangularis, and left amygdala (Boots et al., 2019). Furthermore, the tract-based structural connectome metric of nodal strength for left and right hippocampi mediated the association between CVD risk factor burden and cognition, specifically attention and information processing, while this same metric for the left middle frontal gyrus mediated the association between CVD risk factor burden and attention and information processing, as well as executive function (Boots et al., 2019). While this work highlights a means by which tract-based structural connectomics may provide insight into the structural vulnerabilities and the brain-behavior relationships common to both CVD risk factors and Alzheimer’s dementia, it is not the only method of multi-modal integration available (Liu et al., 2015; Sui, Adali, Yu, Chen and Calhoun, 2012; Valdes-Sosa, Kotter and Friston, 2005), and readers are encouraged to consider what works best for their research interests as well as the MRI modalities used to support their work.
Conclusion
While a discussion of the possible underlying pathophysiology linking common cerebral structures associated with CVD risk factors and Alzheimer’s dementia is beyond the scope of this review, as is an outline of the potential temporal nature of theses alterations over time, multiple empirical (e.g., Thompson et al., 2003) and conceptual (e.g., Zlokovic, 2011) studies as well as Special Issue collections exist (Murphy, Corriveau and Wilcock, 2016), relating to one or both of these disease states. The focus of this review, however, was to present evidence of the overlap between grey, white, and subcortical structural alterations associated with CVD risk factors as well as risk for and development of Alzheimer’s dementia. Given the two-hit vascular hypothesis for Alzheimer’s disease (Zlokovic, 2011) includes CVD risk factors as part of ‘hit one’, and the results of previous studies investigating hypoperfusion in Alzheimer’s dementia (see Montagne et al., 2016 for review), we advocate that the congruent structural imaging findings reported in this study as related to both CVD risk factors and Alzheimer’s dementia further support the consideration of the role CVD risk factors play across dementia subtypes including Alzheimer’s disease.
Only with a continued more integrated approach to neurodegeneration will we be able to move beyond increasingly isolated and unsuccessful clinical trials to slow risk for and ultimately stop development of Alzheimer’s dementia. This position is further supported by the fact that several large-scale intervention trials of modifiable CVD risk factors including targeted foci, for example, the SPRINT MIND trial (Systolic Blood Pressure Intervention Trial – Memory and cognition in Decreased Hypertension: Sprint Mind Investigators for the SPRINT Research Group et al., 2019), as well as multidomain interventions including diet, exercise, and vascular risk monitoring, for example, the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER: Kivipelto et al., 2013), have reported success in reducing age-related neurodegeneration. More specifically, targeting lower levels of systolic blood pressure led to smaller increases in white matter hyperintensity burden over approximately 4 years (SPRINT Research Group et al., 2019), and a multidomain 2-year intervention that included vascular risk monitoring led to improved cognitive functioning (Ngandu et al., 2015), regardless of participant characteristics including global mental status (Rosenberg et al., 2018). Thus, by considering a more complete picture of neuropathological alterations present in individuals with Alzheimer’s dementia including those associated with CVD risk factors, more relevant, more inclusive, and more successful clinical trials may follow.
References
Aksu, Y., Miller, D. J., Kesidis, G., Bigler, D. C., & Yang, Q. X. (2011). An MRI-derived definition of MCI-to-AD conversion for long-term, automatic prognosis of MCI patients. PLoS One, 6(10), e25074. https://doi.org/10.1371/journal.pone.0025074
Apostolova, L. G., Mosconi, L., Thompson, P. M., Green, A. E., Hwang, K. S., Ramirez, A., … de Leon, M. J. (2010). Subregional hippocampal atrophy predicts Alzheimer's dementia in the cognitively normal. Neurobiology of Aging, 31(7), 1077–1088. https://doi.org/10.1016/j.neurobiolaging.2008.08.008
Bangen, K. J., Preis, S. R., Delano-Wood, L., Wolf, P. A., Libon, D. J., Bondi, M. W., … Brickman, A. M. (2018). Baseline white matter Hyperintensities and hippocampal volume are associated with conversion from Normal cognition to mild cognitive impairment in the Framingham offspring Study. Alzheimer Disease and Associated Disorders, 32(1), 50–56. https://doi.org/10.1097/WAD.0000000000000215
Beauchet, O., Celle, S., Roche, F., Bartha, R., Montero-Odasso, M., Allali, G., & Annweiler, C. (2013). Blood pressure levels and brain volume reduction: A systematic review and meta-analysis. Journal of Hypertension, 31(8), 1502–1516. https://doi.org/10.1097/HJH.0b013e32836184b5
Bendlin, B. B., Carlsson, C. M., Gleason, C. E., Johnson, S. C., Sodhi, A., Gallagher, C. L., … Asthana, S. (2010). Midlife predictors of Alzheimer's disease. Maturitas, 65(2), 131–137. https://doi.org/10.1016/j.maturitas.2009.12.014
Betzel, R. F., Byrge, L., He, Y., Goni, J., Zuo, X. N., & Sporns, O. (2014). Changes in structural and functional connectivity among resting-state networks across the human lifespan. Neuroimage, 102(Pt 2), 345–357. https://doi.org/10.1016/j.neuroimage.2014.07.067
Boots, E. A., Zhan, L., Dion, C., Karstens, A. J., Peven, J. C., Ajilore, O., & Lamar, M. (2019). Cardiovascular disease risk factors, tract-based structural connectomics, and cognition in older adults. Neuroimage, 196, 152–160. https://doi.org/10.1016/j.neuroimage.2019.04.024
Boyle, P. A., Yu, L., Wilson, R. S., Leurgans, S. E., Schneider, J. A., & Bennett, D. A. (2018). Person-specific contribution of neuropathologies to cognitive loss in old age. Annals of Neurology, 83(1), 74–83. https://doi.org/10.1002/ana.25123
Brickman, A. M. (2013). Contemplating Alzheimer's disease and the contribution of white matter hyperintensities. Current Neurology and Neuroscience Reports, 13(12), 415. https://doi.org/10.1007/s11910-013-0415-7
Brickman, A. M., Provenzano, F. A., Muraskin, J., Manly, J. J., Blum, S., Apa, Z., … Mayeux, R. (2012). Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Archives of Neurology, 69(12), 1621–1627. https://doi.org/10.1001/archneurol.2012.1527
Brickman, A. M., Schupf, N., Manly, J. J., Stern, Y., Luchsinger, J. A., Provenzano, F. A., … Portet, F. (2014). APOE epsilon4 and risk for Alzheimer's disease: Do regionally distributed white matter hyperintensities play a role? Alzheimers Dement, 10(6), 619–629. https://doi.org/10.1016/j.jalz.2014.07.155
Brickman, A. M., Tosto, G., Gutierrez, J., Andrews, H., Gu, Y., Narkhede, A., … Mayeux, R. (2018). An MRI measure of degenerative and cerebrovascular pathology in Alzheimer disease. Neurology, 91(15), e1402–e1412. https://doi.org/10.1212/WNL.0000000000006310
Brickman, A. M., Zahodne, L. B., Guzman, V. A., Narkhede, A., Meier, I. B., Griffith, E. Y., … Mayeux, R. (2015). Reconsidering harbingers of dementia: Progression of parietal lobe white matter hyperintensities predicts Alzheimer's disease incidence. Neurobiology of Aging, 36(1), 27–32. https://doi.org/10.1016/j.neurobiolaging.2014.07.019
Bruehl, H., Wolf, O. T., Sweat, V., Tirsi, A., Richardson, S., & Convit, A. (2009). Modifiers of cognitive function and brain structure in middle-aged and elderly individuals with type 2 diabetes mellitus. Brain Research, 1280, 186–194. https://doi.org/10.1016/j.brainres.2009.05.032
Bryan, R. N., Bilello, M., Davatzikos, C., Lazar, R. M., Murray, A., Horowitz, K., … Launer, L. J. (2014). Effect of diabetes on brain structure: The action to control cardiovascular risk in diabetes MR imaging baseline data. Radiology, 272(1), 210–216. https://doi.org/10.1148/radiol.14131494
Cardenas, V. A., Reed, B., Chao, L. L., Chui, H., Sanossian, N., DeCarli, C. C., … Weiner, M. W. (2012). Associations among vascular risk factors, carotid atherosclerosis, and cortical volume and thickness in older adults. Stroke, 43(11), 2865–2870. https://doi.org/10.1161/STROKEAHA.112.659722
Carmichael, O., Schwarz, C., Drucker, D., Fletcher, E., Harvey, D., Beckett, L., … Alzheimer's Disease Neuroimaging, I. (2010). Longitudinal changes in white matter disease and cognition in the first year of the Alzheimer disease neuroimaging initiative. Archives of Neurology, 67(11), 1370–1378. https://doi.org/10.1001/archneurol.2010.284
Catani, M., & Mesulam, M. (2008). What is a disconnection syndrome? Cortex, 44(8), 911–913. https://doi.org/10.1016/j.cortex.2008.05.001
Chen, J., Zhang, J., Liu, X., Wang, X., Xu, X., Li, H., … Chen, Z. (2017). Abnormal subcortical nuclei shapes in patients with type 2 diabetes mellitus. European Radiology, 27(10), 4247–4256. https://doi.org/10.1007/s00330-017-4790-3
Cox, S. R., Lyall, D. M., Ritchie, S. J., Bastin, M. E., Harris, M. A., Buchanan, C. R., … Deary, I. J. (2019). Associations between vascular risk factors and brain MRI indices in UK biobank. European Heart Journal, 40(28), 2290–2300. https://doi.org/10.1093/eurheartj/ehz100
Cui, D., Liu, X., Liu, M., Cao, W., Xue, Y., Guo, Y., … Jiao, Q. (2019). Subcortical gray matter structural alterations in prediabetes and type 2 diabetes. Neuroreport, 30(6), 441–445. https://doi.org/10.1097/WNR.0000000000001224
Cui, X., Abduljalil, A., Manor, B. D., Peng, C. K., & Novak, V. (2014). Multi-scale glycemic variability: A link to gray matter atrophy and cognitive decline in type 2 diabetes. PLoS One, 9(1), e86284. https://doi.org/10.1371/journal.pone.0086284
Dai, W., Lopez, O. L., Carmichael, O. T., Becker, J. T., Kuller, L. H., & Gach, H. M. (2009). Mild cognitive impairment and alzheimer disease: Patterns of altered cerebral blood flow at MR imaging. Radiology, 250(3), 856–866. https://doi.org/10.1148/radiol.2503080751
Daianu, M., Jahanshad, N., Nir, T. M., Jack Jr., C. R., Weiner, M. W., Bernstein, M. A., … Alzheimer's Disease Neuroimaging, I. (2015). Rich club analysis in the Alzheimer's disease connectome reveals a relatively undisturbed structural core network. Human Brain Mapping, 36(8), 3087–3103. https://doi.org/10.1002/hbm.22830
Daianu, M., Jahanshad, N., Nir, T. M., Toga, A. W., Jack Jr., C. R., Weiner, M. W., … Alzheimer's Disease Neuroimaging, I. (2013). Breakdown of brain connectivity between normal aging and Alzheimer's disease: A structural k-core network analysis. Brain Connectivity, 3(4), 407–422. https://doi.org/10.1089/brain.2012.0137
Damulina, A., Pirpamer, L., Seiler, S., Benke, T., Dal-Bianco, P., Ransmayr, G., … Schmidt, R. (2019). White matter Hyperintensities in Alzheimer's Disease: A lesion probability mapping Study. Journal of Alzheimer's Disease, 68(2), 789–796. https://doi.org/10.3233/JAD-180982
de Groot, M., Ikram, M. A., Akoudad, S., Krestin, G. P., Hofman, A., van der Lugt, A., … Vernooij, M. W. (2015). Tract-specific white matter degeneration in aging: The Rotterdam Study. Alzheimers Dement, 11(3), 321–330. https://doi.org/10.1016/j.jalz.2014.06.011
de la Torre, J. C. (2010). The vascular hypothesis of Alzheimer's disease: Bench to bedside and beyond. Neurodegenerative Diseases, 7(1–3), 116–121. https://doi.org/10.1159/000285520
de la Torre, J. C. (2018). The vascular hypothesis of Alzheimer's Disease: A key to preclinical prediction of dementia using Neuroimaging. Journal of Alzheimer's Disease, 63(1), 35–52. https://doi.org/10.3233/JAD-180004
Debette, S., Seshadri, S., Beiser, A., Au, R., Himali, J. J., Palumbo, C., … DeCarli, C. (2011). Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology, 77(5), 461–468. https://doi.org/10.1212/WNL.0b013e318227b227
Delano-Wood, L., Bondi, M. W., Sacco, J., Abeles, N., Jak, A. J., Libon, D. J., & Bozoki, A. (2009). Heterogeneity in mild cognitive impairment: Differences in neuropsychological profile and associated white matter lesion pathology. Journal of the International Neuropsychological Society, 15(6), 906–914. https://doi.org/10.1017/S1355617709990257
den Heijer, T., van der Lijn, F., Koudstaal, P. J., Hofman, A., van der Lugt, A., Krestin, G. P., … Breteler, M. M. (2010). A 10-year follow-up of hippocampal volume on magnetic resonance imaging in early dementia and cognitive decline. Brain, 133(Pt 4), 1163–1172. https://doi.org/10.1093/brain/awq048
Dickerson, B. C., Bakkour, A., Salat, D. H., Feczko, E., Pacheco, J., Greve, D. N., … Buckner, R. L. (2009). The cortical signature of Alzheimer's disease: Regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cerebral Cortex, 19(3), 497–510. https://doi.org/10.1093/cercor/bhn113
Erus, G., Battapady, H., Zhang, T., Lovato, J., Miller, M. E., Williamson, J. D., … Davatzikos, C. (2015). Spatial patterns of structural brain changes in type 2 diabetic patients and their longitudinal progression with intensive control of blood glucose. Diabetes Care, 38(1), 97–104. https://doi.org/10.2337/dc14-1196
Eskildsen, S. F., Coupe, P., Garcia-Lorenzo, D., Fonov, V., Pruessner, J. C., Collins, D. L., & Alzheimer's Disease Neuroimaging, I. (2013). Prediction of Alzheimer's disease in subjects with mild cognitive impairment from the ADNI cohort using patterns of cortical thinning. Neuroimage, 65, 511–521. https://doi.org/10.1016/j.neuroimage.2012.09.058
Fennema-Notestine, C., McEvoy, L. K., Notestine, R., Panizzon, M. S., Yau, W. W., Franz, C. E., … Kremen, W. S. (2016). White matter disease in midlife is heritable, related to hypertension, and shares some genetic influence with systolic blood pressure. Neuroimage Clin, 12, 737–745. https://doi.org/10.1016/j.nicl.2016.10.001
Firbank, M. J., Wiseman, R. M., Burton, E. J., Saxby, B. K., O'Brien, J. T., & Ford, G. A. (2007). Brain atrophy and white matter hyperintensity change in older adults and relationship to blood pressure. Brain atrophy. WMH change and blood pressure. J Neurol, 254(6), 713–721. https://doi.org/10.1007/s00415-006-0238-4
Fox, N. C., Warrington, E. K., Freeborough, P. A., Hartikainen, P., Kennedy, A. M., Stevens, J. M., & Rossor, M. N. (1996). Presymptomatic hippocampal atrophy in Alzheimer's disease. A longitudinal MRI study. Brain, 119(Pt 6), 2001–2007.
Friedman, J. I., Tang, C. Y., de Haas, H. J., Changchien, L., Goliasch, G., Dabas, P., … Narula, J. (2014). Brain imaging changes associated with risk factors for cardiovascular and cerebrovascular disease in asymptomatic patients. JACC: Cardiovascular Imaging, 7(10), 1039–1053. https://doi.org/10.1016/j.jcmg.2014.06.014
Geschwind, N. (1965a). Disconnexion syndromes in animals and man. I. Brain, 88(2), 237–294. https://doi.org/10.1093/brain/88.2.237
Geschwind, N. (1965b). Disconnexion syndromes in animals and man. II. Brain, 88(3), 585–644. https://doi.org/10.1093/brain/88.3.585
Gianaros, P. J., Greer, P. J., Ryan, C. M., & Jennings, J. R. (2006). Higher blood pressure predicts lower regional grey matter volume: Consequences on short-term information processing. Neuroimage, 31(2), 754–765. https://doi.org/10.1016/j.neuroimage.2006.01.003
Glodzik, L., Mosconi, L., Tsui, W., de Santi, S., Zinkowski, R., Pirraglia, E., … de Leon, M. J. (2012). Alzheimer's disease markers, hypertension, and gray matter damage in normal elderly. Neurobiology of Aging, 33(7), 1215–1227. https://doi.org/10.1016/j.neurobiolaging.2011.02.012
Gonzales, M. M., Ajilore, O., Charlton, R. C., Cohen, J., Yang, S., Sieg, E., … Lamar, M. (2017). Divergent influences of cardiovascular Disease risk factor domains on cognition and gray and white matter morphology. Psychosomatic Medicine, 79(5), 541–548. https://doi.org/10.1097/PSY.0000000000000448
Graff-Radford, J., Arenaza-Urquijo, E. M., Knopman, D. S., Schwarz, C. G., Brown, R. D., Rabinstein, A. A., … Vemuri, P. (2019). White matter hyperintensities: Relationship to amyloid and tau burden. Brain, 142(8), 2483–2491. https://doi.org/10.1093/brain/awz162
Habes, M., Erus, G., Toledo, J. B., Bryan, N., Janowitz, D., Doshi, J., … Davatzikos, C. (2018). Regional tract-specific white matter hyperintensities are associated with patterns to aging-related brain atrophy via vascular risk factors, but also independently. Alzheimers Dement (Amst), 10(1), 278–284. https://doi.org/10.1016/j.dadm.2018.02.002
Habes, M., Erus, G., Toledo, J. B., Zhang, T., Bryan, N., Launer, L. J., … Davatzikos, C. (2016). White matter hyperintensities and imaging patterns of brain ageing in the general population. Brain, 139(Pt 4), 1164–1179. https://doi.org/10.1093/brain/aww008
Hachinski, V. C. (2019). Dementia: Paradigm shifting into high gear. Alzheimer's & Dementia, 15(7), 985–994. https://doi.org/10.1016/j.jalz.2019.01.006
Haight, T., Nick Bryan, R., Erus, G., Hsieh, M. K., Davatzikos, C., Nasrallah, I., … Launer, L. J. (2018). White matter microstructure, white matter lesions, and hypertension: An examination of early surrogate markers of vascular-related brain change in midlife. Neuroimage Clin, 18, 753–761. https://doi.org/10.1016/j.nicl.2018.02.032
Hoogenboom, W. S., Marder, T. J., Flores, V. L., Huisman, S., Eaton, H. P., Schneiderman, J. S., … Musen, G. (2014). Cerebral white matter integrity and resting-state functional connectivity in middle-aged patients with type 2 diabetes. Diabetes, 63(2), 728–738. https://doi.org/10.2337/db13-1219
Iadecola, C., Yaffe, K., Biller, J., Bratzke, L. C., Faraci, F. M., Gorelick, P. B., … Stroke, C. (2016). Impact of hypertension on cognitive function: A scientific statement from the American Heart Association. Hypertension, 68(6), e67–e94. https://doi.org/10.1161/HYP.0000000000000053
Jack Jr., C. R., Bennett, D. A., Blennow, K., Carrillo, M. C., Dunn, B., Haeberlein, S. B., … Contributors. (2018). NIA-AA research framework: Toward a biological definition of Alzheimer's disease. Alzheimers Dement, 14(4), 535–562. https://doi.org/10.1016/j.jalz.2018.02.018
Jacobs, H. I., Leritz, E. C., Williams, V. J., Van Boxtel, M. P., van der Elst, W., Jolles, J., … Salat, D. H. (2013). Association between white matter microstructure, executive functions, and processing speed in older adults: The impact of vascular health. Human Brain Mapping, 34(1), 77–95. https://doi.org/10.1002/hbm.21412
Jacquemont, T., De Vico Fallani, F., Bertrand, A., Epelbaum, S., Routier, A., Dubois, B., … Alzheimer's Disease Neuroimaging, I. (2017). Amyloidosis and neurodegeneration result in distinct structural connectivity patterns in mild cognitive impairment. Neurobiology of Aging, 55, 177–189. https://doi.org/10.1016/j.neurobiolaging.2017.03.023
Jefferson, A. L. (2020). Midlife consequences of cumulative blood pressure exposure: Importance of a lifespan approach. Circulation, 141(9), 725–727. https://doi.org/10.1161/CIRCULATIONAHA.120.044447
Jellinger, K. A. (2010). Prevalence and impact of cerebrovascular lesions in Alzheimer and lewy body diseases. Neurodegenerative Diseases, 7(1–3), 112–115. https://doi.org/10.1159/000285518
Jenkins, L. M., Garner, C. R., Kurian, S., Higgins, J. P., Parrish, T. B., Sedaghat, S., … Sorond, F. A. (2020). Cumulative blood pressure exposure, basal ganglia, and thalamic morphology in midlife. Hypertension, 75(5), 1289–1295. https://doi.org/10.1161/HYPERTENSIONAHA.120.14678
Kalaria, R. N. (2010). Vascular basis for brain degeneration: Faltering controls and risk factors for dementia. Nutrition Reviews, 68(Suppl 2), S74–S87. https://doi.org/10.1111/j.1753-4887.2010.00352.x
Kao, Y. H., Chou, M. C., Chen, C. H., & Yang, Y. H. (2019). White matter changes in patients with Alzheimer's Disease and associated factors. Journal of Clinical Medicine, 8(2). https://doi.org/10.3390/jcm8020167
Kapasi, A., DeCarli, C., & Schneider, J. A. (2017). Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathologica, 134(2), 171–186. https://doi.org/10.1007/s00401-017-1717-7
Kennedy, K. M., & Raz, N. (2009). Pattern of normal age-related regional differences in white matter microstructure is modified by vascular risk. Brain Research, 1297, 41–56. https://doi.org/10.1016/j.brainres.2009.08.058
Kiuchi, K., Kitamura, S., Taoka, T., Yasuno, F., Tanimura, M., Matsuoka, K., … Kishimoto, T. (2014). Gray and white matter changes in subjective cognitive impairment, amnestic mild cognitive impairment and Alzheimer's disease: A voxel-based analysis study. PLoS One, 9(8), e104007. https://doi.org/10.1371/journal.pone.0104007
Kivipelto, M., Solomon, A., Ahtiluoto, S., Ngandu, T., Lehtisalo, J., Antikainen, R., … Soininen, H. (2013). The Finnish geriatric intervention Study to prevent cognitive impairment and disability (FINGER): Study design and progress. Alzheimers Dement, 9(6), 657–665. https://doi.org/10.1016/j.jalz.2012.09.012
Kumar, A., Haroon, E., Darwin, C., Pham, D., Ajilore, O., Rodriguez, G., & Mintz, J. (2008). Gray matter prefrontal changes in type 2 diabetes detected using MRI. Journal of Magnetic Resonance Imaging, 27(1), 14–19. https://doi.org/10.1002/jmri.21224
Lamar, M., Rubin, L. H., Ajilore, O., Charlton, R., Zhang, A., Yang, S., … Kumar, A. (2015). What metabolic syndrome contributes to brain outcomes in African American & Caucasian Cohorts. Current Alzheimer Research, 12(7), 640–647.
Lee, S., Viqar, F., Zimmerman, M. E., Narkhede, A., Tosto, G., Benzinger, T. L., … Dominantly Inherited Alzheimer, N. (2016). White matter hyperintensities are a core feature of Alzheimer's disease: Evidence from the dominantly inherited Alzheimer network. Annals of Neurology, 79(6), 929–939. https://doi.org/10.1002/ana.24647
Leritz, E. C., Salat, D. H., Williams, V. J., Schnyer, D. M., Rudolph, J. L., Lipsitz, L., … Milberg, W. P. (2011). Thickness of the human cerebral cortex is associated with metrics of cerebrovascular health in a normative sample of community dwelling older adults. Neuroimage, 54(4), 2659–2671. https://doi.org/10.1016/j.neuroimage.2010.10.050
Li, J. Q., Tan, L., Wang, H. F., Tan, M. S., Tan, L., Xu, W., … Yu, J. T. (2016). Risk factors for predicting progression from mild cognitive impairment to Alzheimer's disease: A systematic review and meta-analysis of cohort studies. Journal of Neurology, Neurosurgery, and Psychiatry, 87(5), 476–484. https://doi.org/10.1136/jnnp-2014-310095
Libon, D. J., Price, C. C., Giovannetti, T., Swenson, R., Bettcher, B. M., Heilman, K. M., & Pennisi, A. (2008). Linking MRI hyperintensities with patterns of neuropsychological impairment: Evidence for a threshold effect. Stroke, 39(3), 806–813. https://doi.org/10.1161/STROKEAHA.107.489997
Lin, L., Jin, C., Fu, Z., Zhang, B., Bin, G., & Wu, S. (2016). Predicting healthy older adult's brain age based on structural connectivity networks using artificial neural networks. Computer Methods and Programs in Biomedicine, 125, 8–17. https://doi.org/10.1016/j.cmpb.2015.11.012
Lindemer, E. R., Greve, D. N., Fischl, B., Augustinack, J. C., Salat, D. H., & Alzheimer's Disease Neuroimaging, I. (2017a). Differential regional distribution of Juxtacortical white matter signal abnormalities in aging and Alzheimer's Disease. Journal of Alzheimer's Disease, 57(1), 293–303. https://doi.org/10.3233/JAD-161057
Lindemer, E. R., Greve, D. N., Fischl, B. R., Augustinack, J. C., & Salat, D. H. (2017b). Regional staging of white matter signal abnormalities in aging and Alzheimer's disease. Neuroimage Clin, 14, 156–165. https://doi.org/10.1016/j.nicl.2017.01.022
Liu, S., Liu, S., Cai, W., Che, H., Pujol, S., Kikinis, R., … Adni. (2015). Multimodal neuroimaging feature learning for multiclass diagnosis of Alzheimer's disease. IEEE Transactions on Biomedical Engineering, 62(4), 1132–1140. https://doi.org/10.1109/TBME.2014.2372011
Maillard, P., Seshadri, S., Beiser, A., Himali, J. J., Au, R., Fletcher, E., … DeCarli, C. (2012). Effects of systolic blood pressure on white-matter integrity in young adults in the Framingham heart Study: A cross-sectional study. Lancet Neurology, 11(12), 1039–1047. https://doi.org/10.1016/S1474-4422(12)70241-7
Mallio, C. A., Schmidt, R., de Reus, M. A., Vernieri, F., Quintiliani, L., Curcio, G., … van den Heuvel, M. P. (2015). Epicentral disruption of structural connectivity in Alzheimer's disease. CNS Neuroscience & Therapeutics, 21(10), 837–845. https://doi.org/10.1111/cns.12397
Marseglia, A., Fratiglioni, L., Kalpouzos, G., Wang, R., Backman, L., & Xu, W. (2019). Prediabetes and diabetes accelerate cognitive decline and predict microvascular lesions: A population-based cohort study. Alzheimers Dement, 15(1), 25–33. https://doi.org/10.1016/j.jalz.2018.06.3060
McEvoy, L. K., Fennema-Notestine, C., Eyler, L. T., Franz, C. E., Hagler Jr., D. J., Lyons, M. J., … Kremen, W. S. (2015). Hypertension-related alterations in white matter microstructure detectable in middle age. Hypertension, 66(2), 317–323. https://doi.org/10.1161/HYPERTENSIONAHA.115.05336
Meusel, L. A., Kansal, N., Tchistiakova, E., Yuen, W., MacIntosh, B. J., Greenwood, C. E., & Anderson, N. D. (2014). A systematic review of type 2 diabetes mellitus and hypertension in imaging studies of cognitive aging: Time to establish new norms. Frontiers in Aging Neuroscience, 6, 148. https://doi.org/10.3389/fnagi.2014.00148
Moller, C., Vrenken, H., Jiskoot, L., Versteeg, A., Barkhof, F., Scheltens, P., & van der Flier, W. M. (2013). Different patterns of gray matter atrophy in early- and late-onset Alzheimer's disease. Neurobiology of Aging, 34(8), 2014–2022. https://doi.org/10.1016/j.neurobiolaging.2013.02.013
Montagne, A., Nation, D. A., Pa, J., Sweeney, M. D., Toga, A. W., & Zlokovic, B. V. (2016). Brain imaging of neurovascular dysfunction in Alzheimer's disease. Acta Neuropathologica, 131(5), 687–707. https://doi.org/10.1007/s00401-016-1570-0
Moran, C., Phan, T. G., Chen, J., Blizzard, L., Beare, R., Venn, A., … Srikanth, V. (2013). Brain atrophy in type 2 diabetes: Regional distribution and influence on cognition. Diabetes Care, 36(12), 4036–4042. https://doi.org/10.2337/dc13-0143
Moulton, C. D., Costafreda, S. G., Horton, P., Ismail, K., & Fu, C. H. (2015). Meta-analyses of structural regional cerebral effects in type 1 and type 2 diabetes. Brain Imaging and Behavior, 9(4), 651–662. https://doi.org/10.1007/s11682-014-9348-2
Munoz Maniega, S., Chappell, F. M., Valdes Hernandez, M. C., Armitage, P. A., Makin, S. D., Heye, A. K., … Wardlaw, J. M. (2017). Integrity of normal-appearing white matter: Influence of age, visible lesion burden and hypertension in patients with small-vessel disease. Journal of Cerebral Blood Flow and Metabolism, 37(2), 644–656. https://doi.org/10.1177/0271678X16635657
Murphy, M. P., Corriveau, R. A., & Wilcock, D. M. (2016). Vascular contributions to cognitive impairment and dementia (VCID). Biochimica et Biophysica Acta, 1862(5), 857–859.
Nelson, A. R., Sweeney, M. D., Sagare, A. P., & Zlokovic, B. V. (2016). Neurovascular dysfunction and neurodegeneration in dementia and Alzheimer's disease. Biochimica et Biophysica Acta, 1862(5), 887–900. https://doi.org/10.1016/j.bbadis.2015.12.016
Ngandu, T., Lehtisalo, J., Solomon, A., Levalahti, E., Ahtiluoto, S., Antikainen, R., … Kivipelto, M. (2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet, 385(9984), 2255–2263. https://doi.org/10.1016/S0140-6736(15)60461-5
Nir, T. M., Jahanshad, N., Toga, A. W., Bernstein, M. A., Jack Jr., C. R., Weiner, M. W., … Alzheimer's Disease Neuroimaging, I. (2015). Connectivity network measures predict volumetric atrophy in mild cognitive impairment. Neurobiology of Aging, 36(Suppl 1), S113–S120. https://doi.org/10.1016/j.neurobiolaging.2014.04.038
Olazaran, J., Ramos, A., Boyano, I., Alfayate, E., Valenti, M., Rabano, A., & Alvarez-Linera, J. (2014). Pattern of and risk factors for brain microbleeds in neurodegenerative dementia. American Journal of Alzheimer's Disease and Other Dementias, 29(3), 263–269. https://doi.org/10.1177/1533317513517043
Perry, A., Wen, W., Lord, A., Thalamuthu, A., Roberts, G., Mitchell, P. B., … Breakspear, M. (2015). The organisation of the elderly connectome. Neuroimage, 114, 414–426. https://doi.org/10.1016/j.neuroimage.2015.04.009
Pini, L., Pievani, M., Bocchetta, M., Altomare, D., Bosco, P., Cavedo, E., … Frisoni, G. B. (2016). Brain atrophy in Alzheimer's Disease and aging. Ageing Research Reviews, 30, 25–48. https://doi.org/10.1016/j.arr.2016.01.002
Price, C. C., Mitchell, S. M., Brumback, B., Tanner, J. J., Schmalfuss, I., Lamar, M., … Libon, D. J. (2012). MRI-leukoaraiosis thresholds and the phenotypic expression of dementia. Neurology, 79(8), 734–740. https://doi.org/10.1212/WNL.0b013e3182661ef6
Raz, L., Knoefel, J., & Bhaskar, K. (2016). The neuropathology and cerebrovascular mechanisms of dementia. Journal of Cerebral Blood Flow and Metabolism, 36(1), 172–186. https://doi.org/10.1038/jcbfm.2015.164
Raji, C. A., Ho, A. J., Parikshak, N. N., Becker, J. T., Lopez, O. L., Kuller, L. H., … Thompson, P. M. (2010). Brain structure and obesity. Human Brain Mapping, 31(3), 353–364. https://doi.org/10.1002/hbm.20870
Reitz, C., Guzman, V. A., Narkhede, A., DeCarli, C., Brickman, A. M., & Luchsinger, J. A. (2017). Relation of Dysglycemia to structural brain changes in a multiethnic elderly cohort. Journal of the American Geriatrics Society, 65(2), 277–285. https://doi.org/10.1111/jgs.14551
Roberts, R. O., Knopman, D. S., Przybelski, S. A., Mielke, M. M., Kantarci, K., Preboske, G. M., … Jack Jr., C. R. (2014). Association of type 2 diabetes with brain atrophy and cognitive impairment. Neurology, 82(13), 1132–1141. https://doi.org/10.1212/WNL.0000000000000269
Rosenberg, A., Ngandu, T., Rusanen, M., Antikainen, R., Backman, L., Havulinna, S., … Kivipelto, M. (2018). Multidomain lifestyle intervention benefits a large elderly population at risk for cognitive decline and dementia regardless of baseline characteristics: The FINGER trial. Alzheimers Dement, 14(3), 263–270. https://doi.org/10.1016/j.jalz.2017.09.006
Rubinov, M., & Sporns, O. (2010). Complex network measures of brain connectivity: Uses and interpretations. Neuroimage, 52(3), 1059–1069. https://doi.org/10.1016/j.neuroimage.2009.10.003
Sabisz, A., Naumczyk, P., Marcinkowska, A., Graff, B., Gasecki, D., Glinska, A., … Narkiewicz, K. (2019). Aging and hypertension - independent or intertwined white matter impairing factors? Insights from the quantitative diffusion tensor imaging. Frontiers in Aging Neuroscience, 11, 35. https://doi.org/10.3389/fnagi.2019.00035
Salvado, G., Brugulat-Serrat, A., Sudre, C. H., Grau-Rivera, O., Suarez-Calvet, M., Falcon, C., … Study, A. (2019). Spatial patterns of white matter hyperintensities associated with Alzheimer's disease risk factors in a cognitively healthy middle-aged cohort. Alzheimer's Research & Therapy, 11(1), 12. https://doi.org/10.1186/s13195-018-0460-1
Scharf, E. L., Graff-Radford, J., Przybelski, S. A., Lesnick, T. G., Mielke, M. M., Knopman, D. S., … Vemuri, P. (2019). Cardiometabolic health and longitudinal progression of white matter Hyperintensity: The Mayo Clinic Study of aging. Stroke, 50(11), 3037–3044. https://doi.org/10.1161/STROKEAHA.119.025822
Schneider, A. L. C., Selvin, E., Sharrett, A. R., Griswold, M., Coresh, J., Jack Jr., C. R., … Gottesman, R. F. (2017). Diabetes, Prediabetes, and brain volumes and subclinical cerebrovascular Disease on MRI: The atherosclerosis risk in communities neurocognitive Study (ARIC-NCS). Diabetes Care, 40(11), 1514–1521. https://doi.org/10.2337/dc17-1185
Silbert, L. C., Lahna, D., Promjunyakul, N. O., Boespflug, E., Ohya, Y., Higashiuesato, Y., … Dodge, H. H. (2018). Risk factors associated with cortical thickness and white matter Hyperintensities in dementia free Okinawan elderly. Journal of Alzheimer's Disease, 63(1), 365–372. https://doi.org/10.3233/JAD-171153
Spilt, A., Goekoop, R., Westendorp, R. G., Blauw, G. J., de Craen, A. J., & van Buchem, M. A. (2006). Not all age-related white matter hyperintensities are the same: A magnetization transfer imaging study. AJNR. American Journal of Neuroradiology, 27(9), 1964–1968.
Sprint Mind Investigators for the SPRINT Research Group, Nasrallah, I. M., Pajewski, N. M., Auchus, A. P., Chelune, G., Cheung, A. K., . . . Bryan, R. N. (2019). Association of Intensive vs standard blood pressure control with cerebral white matter lesions. JAMA, 322(6), 524–534. doi:https://doi.org/10.1001/jama.2019.10551
Sui, J., Adali, T., Yu, Q., Chen, J., & Calhoun, V. D. (2012). A review of multivariate methods for multimodal fusion of brain imaging data. Journal of Neuroscience Methods, 204(1), 68–81. https://doi.org/10.1016/j.jneumeth.2011.10.031
Sun, Y., Lee, R., Chen, Y., Collinson, S., Thakor, N., Bezerianos, A., & Sim, K. (2015). Progressive gender differences of structural brain networks in healthy adults: A longitudinal, diffusion tensor imaging study. PLoS One, 10(3), e0118857. https://doi.org/10.1371/journal.pone.0118857
Sundar, U., Manwatkar, A. A., Joshi, A. R., & Bhandarkar, P. (2019). The effect of hypertension and diabetes mellitus on white matter changes in MRI brain: A comparative Study between patients with Alzheimer's Disease and an age-matched control group. The Journal of the Association of Physicians of India, 67(4), 14–17.
Suzuki, H., Venkataraman, A. V., Bai, W., Guitton, F., Guo, Y., Dehghan, A., … Alzheimer's Disease Neuroimaging, I. (2019). Associations of regional brain structural differences with aging, modifiable risk factors for dementia, and cognitive performance. JAMA Network Open, 2(12), e1917257. https://doi.org/10.1001/jamanetworkopen.2019.17257
Thompson, P. M., Hayashi, K. M., de Zubicaray, G., Janke, A. L., Rose, S. E., Semple, J., … Toga, A. W. (2003). Dynamics of gray matter loss in Alzheimer's disease. The Journal of Neuroscience, 23(3), 994–1005.
Tolppanen, A. M., Solomon, A., Soininen, H., & Kivipelto, M. (2012). Midlife vascular risk factors and Alzheimer's disease: Evidence from epidemiological studies. Journal of Alzheimer's Disease, 32(3), 531–540. https://doi.org/10.3233/JAD-2012-120802
Tosto, G., Zimmerman, M. E., Hamilton, J. L., Carmichael, O. T., Brickman, A. M., & Alzheimer's Disease Neuroimaging, I. (2015). The effect of white matter hyperintensities on neurodegeneration in mild cognitive impairment. Alzheimers Dement, 11(12), 1510–1519. https://doi.org/10.1016/j.jalz.2015.05.014
Valdes-Sosa, P. A., Kotter, R., & Friston, K. J. (2005). Introduction: Multimodal neuroimaging of brain connectivity. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 360(1457), 865–867. https://doi.org/10.1098/rstb.2005.1655
Wang, R., Fratiglioni, L., Laukka, E. J., Lovden, M., Kalpouzos, G., Keller, L., … Qiu, C. (2015a). Effects of vascular risk factors and APOE epsilon4 on white matter integrity and cognitive decline. Neurology, 84(11), 1128–1135. https://doi.org/10.1212/WNL.0000000000001379
Wang, W. Y., Yu, J. T., Liu, Y., Yin, R. H., Wang, H. F., Wang, J., … Tan, L. (2015b). Voxel-based meta-analysis of grey matter changes in Alzheimer's disease. Transl Neurodegener, 4(1), 6. https://doi.org/10.1186/s40035-015-0027-z
Wassenaar, T. M., Yaffe, K., van der Werf, Y. D., & Sexton, C. E. (2019). Associations between modifiable risk factors and white matter of the aging brain: Insights from diffusion tensor imaging studies. Neurobiology of Aging, 80, 56–70. https://doi.org/10.1016/j.neurobiolaging.2019.04.006
Weinstein, G., Maillard, P., Himali, J. J., Beiser, A. S., Au, R., Wolf, P. A., … DeCarli, C. (2015). Glucose indices are associated with cognitive and structural brain measures in young adults. Neurology, 84(23), 2329–2337. https://doi.org/10.1212/WNL.0000000000001655
Whitwell, J. L., Tosakulwong, N., Weigand, S. D., Senjem, M. L., Lowe, V. J., Gunter, J. L., … Jack Jr., C. R. (2013). Does amyloid deposition produce a specific atrophic signature in cognitively normal subjects? Neuroimage Clin, 2, 249–257. https://doi.org/10.1016/j.nicl.2013.01.006
Wiseman, R. M., Saxby, B. K., Burton, E. J., Barber, R., Ford, G. A., & O'Brien, J. T. (2004). Hippocampal atrophy, whole brain volume, and white matter lesions in older hypertensive subjects. Neurology, 63(10), 1892–1897.
Wu, G., Lin, L., Zhang, Q., & Wu, J. (2017). Brain gray matter changes in type 2 diabetes mellitus: A meta-analysis of whole-brain voxel-based morphometry study. Journal of Diabetes and its Complications, 31(12), 1698–1703. https://doi.org/10.1016/j.jdiacomp.2017.09.001
Yan, T., Wang, W., Yang, L., Chen, K., Chen, R., & Han, Y. (2018). Rich club disturbances of the human connectome from subjective cognitive decline to Alzheimer's disease. Theranostics, 8(12), 3237–3255. https://doi.org/10.7150/thno.23772
Yarchoan, M., Xie, S. X., Kling, M. A., Toledo, J. B., Wolk, D. A., Lee, E. B., … Arnold, S. E. (2012). Cerebrovascular atherosclerosis correlates with Alzheimer pathology in neurodegenerative dementias. Brain, 135(Pt 12), 3749–3756. https://doi.org/10.1093/brain/aws271
Zeifman, L. E., Eddy, W. F., Lopez, O. L., Kuller, L. H., Raji, C., Thompson, P. M., & Becker, J. T. (2015). Voxel level survival analysis of Grey matter volume and incident mild cognitive impairment or Alzheimer's Disease. Journal of Alzheimer's Disease, 46(1), 167–178. https://doi.org/10.3233/JAD-150047
Zhang, Y., Zhang, X., Zhang, J., Liu, C., Yuan, Q., Yin, X., … Wang, J. (2014). Gray matter volume abnormalities in type 2 diabetes mellitus with and without mild cognitive impairment. Neuroscience Letters, 562, 1–6. https://doi.org/10.1016/j.neulet.2014.01.006
Zhang, Y. W., Zhang, J. Q., Liu, C., Wei, P., Zhang, X., Yuan, Q. Y., … Wang, J. (2015). Memory dysfunction in type 2 diabetes mellitus correlates with reduced hippocampal CA1 and subiculum volumes. Chinese Medical Journal, 128(4), 465–471. https://doi.org/10.4103/0366-6999.151082
Zhao, T., Cao, M., Niu, H., Zuo, X. N., Evans, A., He, Y., … Shu, N. (2015). Age-related changes in the topological organization of the white matter structural connectome across the human lifespan. Human Brain Mapping, 36(10), 3777–3792. https://doi.org/10.1002/hbm.22877
Zimmerman, R. D., Fleming, C. A., Lee, B. C., Saint-Louis, L. A., & Deck, M. D. (1986). Periventricular hyperintensity as seen by magnetic resonance: Prevalence and significance. AJR. American Journal of Roentgenology, 146(3), 443–450. https://doi.org/10.2214/ajr.146.3.443
Zlokovic, B. V. (2011). Neurovascular pathways to neurodegeneration in Alzheimer's disease and other disorders. Nature Reviews. Neuroscience, 12(12), 723–738. https://doi.org/10.1038/nrn3114
Funding
RADC research presented in this chapter was supported by the National Institute on Aging (P30 AG010161; R01 AG056405; R01 AG052200; R01 AG062711) and the National Institute of Neurological Disorders and Stroke (UH3 NS100599).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lamar, M., Boots, E.A., Arfanakis, K. et al. Common Brain Structural Alterations Associated with Cardiovascular Disease Risk Factors and Alzheimer’s Dementia: Future Directions and Implications. Neuropsychol Rev 30, 546–557 (2020). https://doi.org/10.1007/s11065-020-09460-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-020-09460-6