Abstract
Aim of the present review paper was to evaluate the hypothesis (included in the proposal of new research criteria for Alzheimer’s disease; Dubois et al., Lancet Neurology, 6, 734–746, 2007) that a neuropsychological tool which provides support for the semantic encoding of memorandum at the time of study and supplies category cues at the time of retrieval (i.e. the Grober-Buschke paradigm) is more effective than traditional measures of free recall in 1) differentiating patients affected by the amnestic form of Mild Cognitive Impairment (MCI) or by mild to moderate forms of Alzheimer’s disease (AD) from healthy matches, 2) predicting the conversion of individuals with MCI to AD, and 3) differentiating AD patients from individuals affected by other forms of dementia. Results of the review are controversial regarding the superiority of the Grober-Buschke procedure in differentiating individuals affected by AD or MCI from healthy individuals. The only study that evaluated this issue directly found that the Grober-Buschke procedure was more sensitive and specific than more traditional memory tests in predicting the conversion of MCI patients to AD. Finally, two studies reported that patients affected by AD or other forms of dementia showed different performance patterns in the free and cued recall tasks of the Grober-Buschke procedure. In conclusion, although encouraging results are reported in the few studies that investigated the ability of this procedure to predict the evolution of individuals with amnestic MCI and to differentiate AD patients from patients with other forms of cortical and subcortical dementia, more experimental work is needed to confirm these positive findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The feasibility of using a neuropsychological approach in the early diagnosis of Alzheimer’s disease (AD) and the differential diagnosis between AD and other forms of dementia rests on the assumption of “selective regional vulnerability” of degenerative diseases affecting the central nervous system. According to Cummings (2003, p. 148), “...the molecular biology of neurodegenerative diseases is linked to the behavioral phenotype through selective regional vulnerability of cell populations. Cells exhibit differential vulnerability to abnormalities of protein metabolism resulting in protein-specific regional dysfunction, and the topography of the cellular dysfunction, in turn, determines the clinical phenotype....”. In other words, each etiological form of degenerative dementia is characterized by the deposition of a specific altered protein in a particular region (or regions) of the brain (e.g., Kovacs et al. 2010; Rademakers and Rovelet-Lecrux 2009; Ludolph et al. 2009) and the clinical, behavioral, and neuropsychological manifestations of a particular form of dementia depend strictly on the specific cortical and/or subcortical area in which the protein deposition occurs or is at least prevalent (e.g., Rascovsky et al. 2002; Grossman et al. 2007; Davies et al. 2005; Kraybill et al. 2005). When applied to the issue of differential diagnosis of degenerative dementias, one corollary of the “selective regional vulnerability” principle is that the selectivity of the regional involvement is particularly stringent in the very early phases of the degenerative process. In more advanced phases, the neuropathological changes tend to spread and overlap the localization of degenerative changes which is typical of other diseases and thus undermine the possibility of differentiating the various forms of dementia based on the phenotype (e.g., Garrard et al. 2001; Sonnen et al. 2007;).
The Declarative Memory Impairment in Alzheimer’s Disease
According to Braak and Braak (1995), a typical progression in the localization of neuropathological changes, particularly the neurofibrillary tangles, occurs in the brains of patients who are developing AD. In the very early phases, corresponding to Braak’s stages 1 and 2, lesions are confined to a restricted neuronal population, in the so called transentorhinal region, located at the boundary between the perirhinal and entorhinal cortices. At this stage, there is no clinical and/or neuropsychological evidence of cognitive dysfunction. In the second phase, corresponding to Braak’s stages 3 and 4, the neuropathological changes spread to the entorhinal cortex in the parahippocampal region and to the hippocampus proper. According to Van Hoesen and Damasio (1987), Alzheimer’s pathology in the mesial temporal lobe is localized in such a way that it selectively affects the neural projections between the hippocampal formation and the entorhinal region; this results in functional disconnection of the hippocampus from associative neocortical afferents and efferents. In view of the critical role played by the hippocampal formation in declarative memory functioning (e.g., Squire et al. 2004), in this phase patients present the clinical features of an amnesic syndrome without concomitant cognitive deficits. Finally, in the advanced phases (corresponding to Braak’s stages 5 and 6) the neuropathology also involves the isocortex in the associative areas of the temporal, parietal, and frontal lobes and, thus, gives rise to the full range of linguistic, gnosic, praxic, and executive deficits that characterize the full-blown manifestation of the dementia syndrome.
A neuropsychological approach to the diagnosis of AD should take into account the above-mentioned pattern of progression of neuropathological changes in this disease as compared to the patterns of progression of other diseases also characterized by a dementia syndrome. Several recent studies on autopsy-confirmed cases of dementia support the high sensitivity and specificity of batteries of neuropsychological tests in differentiating patients affected by different etiological forms of degenerative dementias. Indeed, it is generally acknowledged that a neuropsychological profile characterized by an early and predominant amnesic disturbance (later associated with linguistic, praxic, visual-spatial, and executive disorders) is pathognomonic of AD (e.g., Salmon et al. 2002); furthermore it differentiates AD patients from patients affected, for example, by fronto-temporal dementia (Grossman et al. 2007; Libon et al. 2007; Rascovsky et al. 2008) or dementia underlain by Lewy body pathology (Galasko et al. 1996; Connor et al. 1998; Kraybill et al. 2005). Some limitations to generalize this claim is represented by cases in which an early amnesic disorder was actually underlain by Lewy body (e.g., Hamilton et al. 2004) or fronto-temporal dementia (Graham et al. 2005) and, on the other side, by cases in which atypical localization of AD pathology resulted in a primary progressive posterior lobar syndrome (e.g., progressive agnosia or Balint’s syndrome; von Gunten et al. 2006) or a primary progressive language disorder (Davies et al. 2005; Forman et al. 2006).
Category Cued Recall in the Diagnosis of Alzheimer’s Disease
All diagnostic criteria proposed thus far for AD acknowledge that declarative memory dysfunction is the earliest and most peculiar characteristic of the cognitive impairment in this disease. In particular, in the criteria established by the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association (McKhann et al. 1984), a deficit of memory and of at least one other cognitive domain has to be present before a diagnosis of probable AD can be made; likewise, in the criteria proposed in the Diagnostic and Statistical Manual of mental disorders (American Psychiatric Association 2000), a deficit of declarative memory (in the anterograde and/or retrograde domain) is required in association with a deficit in at least one other cognitive domain.
Also, in the new diagnostic criteria proposed by Bruno Dubois’ work group (Dubois et al. 2007), a declarative memory impairment is at the core of the diagnostic decision of AD (corroborated by the presence of at least one or more abnormal biomarkers in structural neuroimaging with MRI, molecular neuroimaging with PET, and cerebrospinal fluid analysis of amyloid β or tau proteins). In a neuropsychological perspective, at least two crucial novelties characterize these criteria. The first is that the presence of a progressive memory deficit is considered sufficient to make a diagnosis of AD even if it is the patient’s only cognitive deficit. In other words, according to the new criteria the simultaneous presence of a deficit in two or more cognitive domains is not necessary to make a diagnosis of AD. Interestingly, the criterion of an isolated memory deficit as diagnostic of AD (corroborated by at least one of the supportive neuroradiological, neurometabolic, and neurochemical criteria) captures cases of amnestic Mild Cognitive Impairment (MCI); the latter is a clinical entity, of relatively recent appearance in the neurological literature on dementia (Petersen et al. 1999, 2001), which is characterized by an isolated deficit of declarative memory in an otherwise healthy elderly person. Amnestic MCI is currently considered a preclinical phase of AD. In fact, the declared aim of the new criteria is to provide a diagnostic tool able to capture the earliest stages of the disease, that is, before the development of full-blown dementia. At this early stage, clinical/drug treatment might have the greatest impact, as indicated by the many drugs being developed that are directed at changing the pathogenesis, particularly the production and clearance of amyloid β and the hyperphosphorylation state of tau (e.g., Kurz and Perneczky 2010).
The second novelty of the new criteria concerns the neuropsychological approach to AD. Indeed, to provide a qualitative characterization of the declarative memory deficit in AD patients, the second point of the “core diagnostic criteria” section clarifies that for a deficit in recall on a test of declarative memory to be considered diagnostic of AD, two procedural requests in the memory paradigm have to be satisfied: 1) a testing procedure has to be used that facilitates the retrieval of studied information, such as a cued recall or a recognition paradigm, and 2) the effective encoding of the memorandum during the study phase has to be controlled. To explain the rationale for this procedural request, the authors refer to a very general model of the role played by distinct cerebral areas implicated in normal declarative memory functioning. Indeed, when a sensory stimulus enters the perceptual field it is first categorized according to its physical and semantic properties at the level of sensory-associative areas in the parietal, temporal, and occipital lobes. Then, the categorized information is transferred to the mesio-temporal areas. From the interplay between the hippocampal formation and the sensory associative areas of the posterior half of the brain, consolidation of the memory trace containing the core information and the associative and contextual data takes place. Apposite retrieval cues are then able to reactivate the memory trace and make possible the subjective experience of remembering. The frontal lobes interact actively with this mechanism at two levels: 1) by providing the attentional and executive resources necessary for the deep, elaborative encoding of the incoming information at the time of learning, and 2) by implementing the most effective retrieval strategies for recollecting that particular encoded experience.
Based on the differential role played by the mesio-temporal areas and the frontal lobes in declarative memory functioning, the existence of two qualitatively different amnesic syndromes following damage in these two portions of the central nervous system has been postulated. In mesio-temporal amnesia, encoded information is unavailable because of a deficit in the consolidation processes of the memory trace. Therefore, it cannot be recollected regardless of the facilitatory conditions (e.g., category cues) available at the time of retrieval. Conversely, although consolidation of the memory trace takes place normally in frontal lobe amnesia, the elaborative encoding of incoming information at the time of study and the ability to implement effective retrieval strategies at the time of memory testing are defective. Thus, these patients are generally poor in free recall procedures that follow unassisted encoding conditions. Nevertheless, if the experimental conditions ensure support for elaborative encoding at the time of study and provide valuable cues at the time of retrieval, then these patients may have normal or quasi-normal retrieval accuracy. Support for the existence of qualitatively different patterns of memory impairment following mesio-temporal vs. frontal lobe damage comes from studies in patients with focal parenchymal lesions in these two regions (e.g., Godefroy et al. 2009; Janowsky et al. 1989; Shimamura et al. 1990).
The paper by Dubois and coworkers lists a series of physiological and pathological conditions of the elderly. Inasmuch as these conditions are characterized by subjective complaints and objective demonstrations of a declarative memory deficit, they have to be differentiated from those conditions that characterize the memory impairment of patients with AD. Among the latter, the authors include the physiological memory decline that accompanies normal aging, the memory deficit suffered by depressed patients, and the memory impairment present in other non-AD dementias, such as fronto-temporal dementia, dementia with Lewy bodies, or vascular dementia. Indeed, the main neuropsychological assumption of these “new criteria” is that although the memory deficit in AD is mainly (or even fully) explained by mesio-temporal damage, the memory deficit in non-AD (dementing and non dementing) conditions is mainly explained by malfunctioning of the frontal circuits because of direct involvement of the frontal cortex by the neuropathological changes (e.g., as in the frontal variant of fronto-temporal dementia) or deafferentation of the frontal areas from subcortical inputs (e.g., in vascular dementia). In any case, and irrespective of the exact mechanism of the frontal lobe dysfunction, the critical prediction is that the memory deficit in AD can be differentiated from deficits in these other conditions because of the presence of the qualitative features of mesio-temporal amnesia in the patients with AD and, conversely, the presence of a memory deficit with qualitative features similar to those of frontal lobe amnesia in the other patients.
Review of the Evidence
In the remaining part of this manuscript, we will selectively review studies in the literature aimed at demonstrating this general assumption. In particular, we will review papers that directly contrasted (in the same AD and non-AD samples) the diagnostic accuracy of a memory test that controls for encoding at the time of study and provides retrieval cues at the time of memory testing with more traditional free-recall procedures in which encoding is typically not controlled and cues are not provided at retrieval (for an overview of neuropsychological tools for analyzing memory disorders, see Lezak 2004). The hypothesis to be proved is that the former type of declarative memory test is more effective than the latter in differentiating AD patients (in the preclinical or clinical phase) from healthy controls or from patients with memory deficits underlain by other pathological conditions. We will review the literature pertaining to the discrimination between: 1) patients with AD vs. healthy elderly individuals, 2) individuals with amnestic forms of MCI vs. healthy elderly individuals, 3) individuals with amnestic MCI who will convert to AD vs. those who will not convert and 4) patients with AD vs. patients with other forms of dementia.
Before reviewing the single studies, we will describe the neuropsychological procedure which has been most frequently utilized in these kind of studies and which is considered paradigmatic of a declarative memory test which, at the same time, controls for a deep encoding of the study material and provides effective cues at retrieval. In the original version of the Grober-Buschke paradigm (GB), also called Free and Cued Selective Reminding Test, (Grober and Buschke 1987), at the time of study patients are presented with 16 line drawings (4 at a time) representing concrete objects, each from a different semantic category. The semantic encoding of each word is controlled by providing the name of each category and requesting the subject to point to and name the specific exemplar. Moreover, immediately following each 4-item display replacement, the encoding of the four items is tested by means of a category cued recall. If the participants fail to remember one or more of the just presented items, the study phase of the 4-item display is repeated until their recall is perfect. Episodic memory for the 16-word list is tested immediately after the study phase is completed by using a free recall procedure; words that are not recalled are tested using a category cued recall procedure. When participants fail to retrieve the item with the cue, the examiner reminds them of the missed word. The memory test (free recall followed by cued recall) is repeated three times in a row and in some cases it is repeated again after a 15-min delay. The test provides measures of free recall and total recall (including items recalled in the free plus cued recall tests). To avoid risking a ceiling effect in the healthy individuals’performance of the cued recall test, Buschke et al. (1997) proposed a modified version of the original GB procedure. In the Double Memory test (DMT), the number of items to be remembered is increased to 64 (4 items for each of 16 categories), written words instead of drawings are presented during the study phase, the immediate cued recall of each 4-item display is not tested, and episodic memory is assessed in a single trial of immediate cued recall. In some cases, an additional delayed recall test is administered 10 to 30 min after immediate recall is completed. The Rappel Indicè (RI48) (Ivanoiu et al. 2005) is similar to the DMT; the only difference is that a list of 48 items (4 for each of 12 categories) is used and that the cued recall for each 4-item display is tested during the study phase.
To confirm the reliability of the GB paradigm (original and modified versions) in diagnosing AD, we should find 1) that AD patients do not improve or, at the very least, improve significantly less than patients with other dementing and non dementing conditions passing from the free to the category cued recall and 2) that the GB paradigm is more sensitive and more specific for identifying people affected by AD than more traditional declarative memory tests, which provide no support for encoding or cue for retrieval (free recall procedures).
Papers Selection
The main constraints in selecting papers for this review were: 1) that at least one group of the reported patients had a diagnosis of AD or MCI according to widely accepted diagnostic criteria (e.g., for AD: McKhann et al. 1984 or American Psychiatric Association 2000; for MCI: Petersen et al. 2001; Petersen 2004), 2) that the study had used the original or some modified version of the GB procedure for the declarative memory assessment, 3) that the paper reported a comparison of performance on the cued recall test of the GB procedure with performance on a free recall test from the same GB procedure (in its original version) or from other memory tests (in the case a modified GB procedure was used).
Sources for paper collection included the following: 1) PubMed, using [Alzheimer] or [dementia] or [mild cognitive impairment] and [Grober] or [Buschke] or [selective reminding] as key words for the search, which was limited to papers written in English and reporting new experimental data; 2) the reference lists of the articles produced by the PubMed search, which were perused for other relevant articles.
Overall, 11 articles (published between 1987 and 2007) were considered eligible for the present review: eight compared performances of AD patients with those of healthy controls; two of the former also reported a comparison between individuals with MCI and healthy elderly subjects; one assessed the utility of the GB procedure for predicting conversion of MCI to AD; and, finally, two compared the performances of different etiological groups of demented patients.
Discrimination of Patients with AD from Healthy Elderly Individuals
Seven studies reported sensitivity and specificity indexes of the cued recall vs. free recall paradigm for differentiating patients affected by mild to moderate forms of AD from matched healthy individuals (Table 1). Three of these studies (Grober and Buschke 1987; Grober et al. 1988; Saka et al. 2006) used the original GB paradigm; therefore, they directly contrasted the diagnostic accuracy of immediate total and free recall following assisted encoding. Sensitivity in identifying individuals with AD was consistently higher in the total with respect to the free recall procedure. Total recall was also more specific than free recall in identifying healthy matches in two of the three studies (Grober and Buschke, 1987; Grober et al. 1988), but was less specific in the third study (Saka et al. 2006). The other four studies used the revised version of the GB procedure with 64 or 48 items. Therefore, they contrasted diagnostic accuracy of cued recall for items whose elaborative encoding had been controlled with free recall procedures that did not follow assisted encoding. Three of these studies tested cued recall immediately after the study phase (Buschke et al. 1997; Brown and Storandt 2000; Ivanoiu et al. 2005); one study tested recall immediately and after a 30 min. delay. Here, results were less consistent. Indeed, sensitivity in diagnosing AD was better in cued than in free recall in two studies (Buschke et al. 1997; Brown and Storandt 2000) and was less accurate in two other studies (Ivanoiu et al. 2005; Vogel et al. 2007). Specificity in recognizing nondemented individuals was better in cued than in free recall in three studies (Buschke et al. 1997; Ivanoiu et al. 2005; Vogel et al. 2007), but was comparable in the remaining study (Brown and Storandt 2000).
The sensitivity of the cued recall test in the GB procedure (both original and modified) seemed to improve as dementia severity increased. Indeed, out of three studies that reported the average MMSE score of the individuals in the AD group, sensitivity on the cued recall test was highest (and actually better than in the free recall test) in the study with the most severely impaired patients (Saka et al. 2006) and was poorer (and actually lower than that displayed by the free recall procedures) in the two studies with less severely impaired patients (Ivanoiu et al. 2005; Vogel et al. 2007). Moreover, Brown and Storandt (2000) reported considerable improvement in the sensitivity of cued recall passing from individuals with very mild to mild AD. Finally, in a study by Tounsi et al. (1999), which did not report diagnostic indexes for sensitivity and specificity, four groups of AD patients (n = 31, 43, 34 and 23, respectively) of increasing dementia severity (MMSE score: >25, 22–25, 18–21 and <18, respectively) performed analogously in the free recall condition of the original GB procedure. Nevertheless, the total recall score decreased progressively passing from the milder subgroup to the more severe subgroup, which suggests higher diagnostic sensitivity of total recall in the latter subgroup.
The relative inconsistency of the results reported in various studies could be related to uncertain AD diagnosis, heterogeneity in sampling criteria, and discrepancies in the GB procedures used. In fact, although all studies reviewed above used standard clinical criteria to diagnose AD, none of them verified the diagnosis of AD using a postmortem histologic examination. Therefore, due to the less than perfect congruency between clinical and pathological diagnosis of AD (Varma et al. 1999; Kazee et al. 1993), there is an obvious risk of circularity in the neuropsychological confirmation of a diagnosis made according to clinical criteria. In these studies, sample sizes were small, that is, they ranged from 22 to 45 participants (Brown and Storandt reported 58 patients but split in two subgroups of mildly and moderately demented). Finally, four out of the seven studies that reported diagnostic sensitivity and specificity indexes did not report MMSE scores of the recruited patients (Grober and Buschke 1987; Grober et al. 1988; Buschke et al. 1997; Brown and Storandt 2000); therefore, it was difficult to compare these results with those of the other studies. There are potential advantages and disadvantages in using the original or a modified version of the GB procedure. Indeed, the risk of score saturation in the original version, due to the limited number of items, did not prevent studies relying on this procedure from obtaining the highest indexes of diagnostic specificity and sensitivity (Grober and Buschke 1987; Grober et al. 1988; Saka et al. 2006). Even though it is difficult to make a direct comparison with other studies (because of the interaction of these indexes with dementia severity of patients included in the different studies), the shorter time required to administer the original version of the GB procedure and the chance to compare free and cued recall for words subject to the same elaborative encoding makes this version preferable for clinical use. Finally, it should be noted that delayed recall tests were not more accurate than immediate tests in discriminating AD from healthy individuals. This suggests that a deficit in learning, not in long-term retention, is at the origin of the memory impairment in these patients. Indeed, in the latter case accelerated decay of the memory trace would make the delayed recall tests particularly sensitive in capturing the memory deficit of the AD patients. Further studies that directly contrast immediate and delayed recall in the same group of patients are needed to confirm this hypothesis.
Discrimination of Individuals with Amnestic MCI From Healthy Elderly Individuals
As reported in Table 2, two studies used the GB paradigm to differentiate individuals affected by MCI from healthy elderly subjects. In Saka et al.’s study (2006), which used the original 16-item version of the GB paradigm, the total immediate recall score was both more sensitive and more specific than the immediate free recall score in differentiating between the two groups. No other test was used for comparison. In the second study (Ivanoiu et al. 2005), which used an expanded, 48-item (RI 48) version of the GB paradigm, the specificity of the immediate category cued recall in identifying healthy controls was higher than that obtained by other tests of free recall for verbal and visuospatial material not preceded by controlled encoding. But, although sensitivity in recognizing MCI individuals was higher than that identified with free recall tests for visual stimuli, it was somewhat lower than that identified with word list free recall.
In keeping with most of the literature on MCI (see for a review, Mitchell and Shiri-Feshki 2008) uncertainty in the interpretation of the results of Saka et al.’s (2006) and Ivanoiu et al.’s (2005) studies derives from the diagnostic criteria adopted to recruit participants. Indeed, in both studies the description of the criteria used to select patients for the MCI group is vague. In fact, in face of the obligatory requirements of subjective memory complaint confirmed by objective testing and non fulfillment of diagnostic criteria for dementia, it is not clear whether these patients suffered from an isolated memory deficit or whether they also performed poorly on other cognitive tests. Moreover, no neuroimaging data, which could have helped discriminate degenerative from vascular forms of MCI (Erkinjuntti et al. 2000), is given. Finally, severity of the memory impairment and rate of conversion to dementia in the follow-up are not quantified. As considered in some detail in the Discussion section, MCI is a heterogeneous clinical condition and its preclinical AD status (demonstrated by rate of conversion) depends greatly on the diagnostic criteria adopted for inclusion by the different studies (Petersen et al. 2001). With this in mind, the higher specificity of total recall over free recall is suggestive of primary hippocampal dysfunction in the patients included in the two studies. The relatively lower sensitivity of Ivanoiu et al.’s (2005) than Saka et al.’s (2006) study may be cautiously interpreted as further confirmation that the original version of the GB procedure is, at the very least, not inferior to the modified (and more time consuming) versions for diagnostic use. Also in this case, the delayed recall test (in Ivanoiu et al. 2005) was not more accurate than the immediate recall test (in Saka et al. 2006) in discriminating MCI from healthy individuals. This supports the view that also in the preclinical phase of AD the memory deficit has a more severe effect on learning than on long-term retention processes.
Discrimination of Converter Vs. Non Converter Amnestic MCI Individuals
Thus far, only one study has investigated the reliability of the GB procedure in discriminating between individuals with the amnestic form of MCI who will eventually convert to AD and those who will not convert. In that study, Sarazin et al. (2007) longitudinally followed up a cohort of 223 individuals who, at the time they entered the study, fulfilled the criteria for amnestic MCI. During the 3 years of observation, 59 of these individuals developed full-blown AD and 6 other patients developed non AD dementias. The immediate total recall score on the original version of the GB procedure (administered at the time of study entry) was more sensitive than the immediate free recall score (79.7 vs. 71.2) in identifying individuals who converted to AD. But, it was somewhat less specific than immediate free recall (89.9 vs. 91.8) in recognizing participants who did not convert to AD. Scores on delayed recall were less sensitive and less specific than scores on immediate recall. This finding provides further confirmation of the hypothesis that the memory deficit in these patients is more likely due to failure of initial learning than to an accelerated decay of the memory trace due to defective storage mechanisms. On another memory test, that is, Benton’s Visual Retention test, the memory scores provided by the GB procedure (both free and cued recall) were more sensitive and more specific.
Discrimination of Patients with AD From Patients with Other Forms of Dementia
Two studies tried to confirm the hypothesis that in a paradigm controlling for semantic encoding of material to be remembered cued recall is better than free recall in differentiating patients with AD from patients with other etiological forms of dementia.
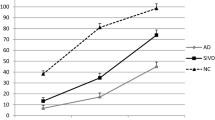
In the first study (Pillon et al. 1994), performance of a group of 15 AD patients on the original GB paradigm were compared with performances of three groups of patients with subcortical forms of dementia, namely Progressive Supranuclear Palsy (n = 15), Huntington’s disease (n = 15) and Parkinson’s disease with dementia (n = 15). The four groups of patients were matched for overall severity of dementia, as documented by similar average scores on the Mattis Dementia Rating scale (ranging from 107 to 112). In agreement with the claim that in the subcortical dementias the memory deficit is due to hypofunctioning of frontal circuits impairing strategic retrieval, the three groups of subcortical dementia patients improved their recall accuracy passing from free to cued recall much more than the group of AD participants. In fact, although in the free recall test a significant difference emerged between the AD patients and the other three groups of demented patients only in the third immediate and the delayed recall trial, in the cued recall paradigm the AD patients performed significantly worse than the patients in the other three groups from the very first immediate recall trial.
In the second study, Pasquier et al. (2001) compared the performances of 30 patients with AD and 15 patients with the frontal variant of fronto-temporal dementia on the original GB paradigm. The two groups were matched for overall level of cognitive deterioration (average MMSE scores: 22.6 and 23.9, respectively). Interestingly, although the two groups of demented patients performed similarly on the free recall test, the participants with fronto-temporal dementia significantly outperformed the participants with AD on the cued recall test. These results are clearly in keeping with the hypothesis that basic mechanisms of the memory deficit differ at least partly in the two groups of patients because in the individuals with Fronto-temporal dementia there is a larger component of deficient retrieval than in those with AD. Nevertheless, the fact that the availability of a category cue did not completely normalize the performances of the fronto-temporal dementia patients (in fact, they still performed worse than matched healthy individuals) suggests that a retrieval deficit might not have been the only determinant of their memory impairment and that storage mechanisms might also have been partly damaged in these patients.
Unfortunately, neither study reported the sensitivity and specificity of the free and cued recall scores in discriminating between patients suffering from different forms of dementia. Therefore, even though the reported results fit well with the expected differential pattern of memory deficits in AD vs. non AD demented patients, the actual contribution of the GB procedure to the differential diagnosis of degenerative dementias still has to be documented.
Discussion
The diagnostic criteria proposed by Dubois et al. (2007) provide, first among the various diagnostic criteria so far proposed, a theoretically driven approach to the neuropsychological diagnosis of AD. In view of the early localization of neuropathological changes in the hippocampal formation in AD, these criteria differentiate AD patients from healthy elderly and individuals with other dementing and nondementing conditions of the elderly based on a qualitative pattern of declarative memory impairment characterized by a deficit in memory trace consolidation as opposed to a memory pattern characterized by a deficit in elaboratively encoding and/or strategically retrieving the information to be remembered. For this purpose, these authors proposed using a neuropsychological tool – the GB paradigm – which, controlling for elaborative encoding at study and providing a strong category cue at retrieval, should be able to compensate for the encoding/retrieval deficit and permit highlighting the “true” memory deficits, that is, those underlain by reduced efficiency in consolidating the memory trace.
A detailed review of the extant literature revealed 11 articles reporting data on the use of the GB paradigm in individuals with AD or the amnestic form of MCI. Eight of these studies reported data on the diagnostic utility of this neuropsychological tool for differentiating patients affected by mild to moderate forms of AD from healthy elderly individuals. The three studies that used the original version of the GB paradigm quite consistently confirmed the diagnostic superiority of the category cued recall test with respect to the free recall test. The only exception was the lower specificity of the cued with respect to the free recall test in Saka et al. (2006). But, when the modified versions of the GB paradigm (which do not include a free recall test) were used, the comparison with more traditional free recall procedures (such as the CERAD word list recall in Ivanoiu et al. 2005) was less favorable for the GB paradigm. Indeed, the GB paradigm was both more sensitive and more specific than verbal free recall tests in only one of the four studies (Buschke et al. 1997). In the other three studies, the GB paradigm was comparable or less sensitive and specific than the other memory tests. As noted above, quite unsurprisingly the diagnostic accuracy of the GB procedure tended to increase in more severe forms of AD.
Overall, these results do not clearly support the superiority of the GB procedure over more traditional neuropsychological tests of declarative memory in differentiating individuals affected by mild to moderate forms of AD from healthy controls. As noted, methodological issues concerning sample recruitment and specific GB procedures used could be responsible for the discrepant results obtained by different studies. More generally, when the dementia syndrome in AD is full blown, the underlying neuropathological changes (corresponding to Braak’s stages 5 and 6) are no longer circumscribed to the MTL region but also involve neocortical regions in the temporal, parietal, and frontal lobes (Braak and Braak 1995). In fact, in this phase, AD patients typically exhibit a declarative memory impairment as well as linguistic, praxic, and behavioral/executive deficits. Due to the spread of neuropathological changes to these neocortical regions, the memory deficit at this stage can no longer be considered as purely “hippocampal”, but likely also entails features of a “frontal amnesic syndrome”. This may be why a neuropsychological tool devised to highlight a purely “hippocampal” memory deficit fails to consistently discriminate individuals with AD from healthy individuals better than more traditional, less theoretically driven memory tasks.
Results of experimental studies investigating the efficacy of the GB paradigm in differentiating individuals with amnestic MCI from healthy elderly individuals are also controversial. Indeed, one out of two studies documented that the total recall (free + cued) score was both more sensitive and more specific than the free recall score alone (Saka et al. 2006). The other study (Ivanoiu et al. 2005), which used an expanded version of the GB paradigm that included 48 items to be remembered, revealed equal specificity and lower sensitivity than the delayed recall score on the CERAD word list memory test. The failure of the GB paradigm to differentiate MCI from healthy matches better than more traditional memory measures was likely due to the lack of homogeneity of the patients classified as amnestic MCI. Indeed, the assumption that patients with an amnestic MCI syndrome are affected by preclinical AD is, at best, conjectural and currently under debate (see, Jicha et al. 2006). In fact, it is now widely accepted that MCI is a heterogeneous condition with a variable qualitative pattern of cognitive impairment that a variety of underlying neuropathological conditions presumably correspond to (Jicha et al. 2006). In an attempt to take into account this variety of conditions, Petersen (2004) proposed classifying MCI patients according to neuropsychological criteria, distinguishing the amnestic form (in which the unique/prevalent deficit is that of declarative memory) from non amnestic forms (in which deficits uniquely or mainly affect executive, visuo-perceptual, or linguistic abilities). In the context of each of the main MCI groups, a further distinction was made between patients with a unique memory or extra-memory deficit (single domain MCI) and those with additional cognitive deficits (multiple domain MCI). Data from the literature document that evolution toward AD most likely occurs among patients with amnestic rather than non-amnestic forms of MCI (Mitchell et al. 2009; Tabert et al. 2006; Ravaglia et al. 2006). But, even among MCI patients with isolated or prevalent memory deficits evolution toward AD is not the rule. In fact, in the clinical studies that included cohorts of individuals with the amnestic form of MCI and that reported 2- to 5-year follow-ups, a relevant proportion of the recruited samples (ranging, in the various studies, between 61 and 78%) did not convert to full-blown AD (De Jager et al. 2005; Wahlund et al. 2003; Visser et al. 2000). In other words, in many individuals who fulfill the diagnostic criteria for MCI (or even of amnestic MCI) the memory deficit is not an expression of AD pathology but is likely the result of a variety of conditions (e.g., depression, cerebro-vascular damage, and other degenerative dementias). In this view, the poor ability of the GB paradigm to discriminate these individuals from healthy matched controls simply reflects the heterogeneity of the pathological conditions underlying the memory deficit, most of which likely affect frontal rather than MTL memory circuits.
More informative about the accuracy of the GB procedure in recognizing individuals in the preclinical stages of AD would be studies which provide a confirm (or disconfirm) of the diagnosis by means of reasonably long follow-up periods. In fact, encouraging results come from the only study that tested the ability of the GB procedure (original version) to predict the conversion to AD of individuals with an amnestic form of MCI. Compared to the Benton Visual Retention test, the GB procedure was much more effective in differentiating MCI individuals who converted from those who did not convert. Note, however, that among the memory indexes provided by the GB paradigm, the diagnostic specificity achieved by using the total recall scores was not substantially different from that achieved by using free recall alone. Moreover, Benton’s Visual Retention test is not one of the most commonly used memory tests for the diagnosis of dementia (possibly because of the confounding effect caused by constructional disorders); therefore, a direct comparison with more frequently used memory measures (such as word list or prose passage free recall) would have been more informative.
The results obtained using the GB paradigm to compare individuals affected by AD or by other forms of degenerative dementia are particularly interesting. Indeed, the total recall score was more effective than the free recall score in differentiating AD patient from demented patients with frontal lobe dysfunction due to either subcortical localization of the neuropathological changes (Progressive Supranuclear, Huntington’s disease and Parkinson’s disease; Pillon et al. 1994) or direct involvement of the frontal lobes (frontal variant of fronto-temporal dementia; Pasquier et al. 2001). Unfortunately, neither of these two studies reported sensitivity and specificity indexes, thus failing to provide information about the clinical usefulness of the neuropsychological tool for differentiating patients affected by different forms of dementia.
In summary, this review of the available evidence does not fully confirm the superiority of the GB paradigm over more traditional neuropsychological tools for analyzing memory disorders in patients with AD. In fact, controversial results emerged from studies that compared the sensitivity/specificity of the cued recall task in the GB paradigm compared to the free recall task in the same or a different experimental paradigm in differentiating patients with full-blown AD or amnestic MCI from healthy individuals. More encouraging results were reported in studies that evaluated the predictive role of performance on the GB paradigm regarding the possible conversion of individuals with amnestic MCI to AD or the qualitative differentiation of the memory deficit in individuals with AD as compared to individuals with other non-AD degenerative dementias. Note, however, that these positive results must be confirmed in independent laboratories (currently, most of them come from the same group of researchers). Furthermore, to determine their true diagnostic usefulness, the values of sensitivity and specificity in differentiating AD from demented non-AD individuals must be reported.
More generally, the results of studies that used the GB paradigm to discriminate individuals affected by preclinical or full-blown AD from matched healthy individuals or individuals with other etiological forms of dementia are important because they help clarify the nature of the memory impairment that characterizes pathological as opposed to physiological aging. Indeed, as noted above, due to the early localization of neuropathological changes at the level of the mesio-temporal structures, the declarative memory deficit in AD patients has been considered a consequence of hippocampal damage. In fact, the proposal of the GB procedure in this context rests on the assumption that the memory deficit in these patients results from a storage deficit (for hippocampal dysfunction) as opposed to the elaborative encoding/strategic retrieval deficit (for primary frontal dysfunction) that characterizes other forms of age-related memory deficits (e.g., depression in the elderly and other dementia syndromes). Nevertheless, the uncertainty of the results reported above suggests the need for caution in accepting this assumption. Indeed, when the clinical presentation of AD is full blown, the neuropathological changes are diffused at the level of the associative neocortex in the temporal, parietal, and frontal lobes (Braak and Braak 1995). This clearly challenges the notion of AD related memory deficit as purely hippocampal and, at least partially, accounts for mixed results of studies assessing the hypothesis of higher accuracy of cued than free recall in discriminating AD patients from matched healthy controls. On the other side, the claim that MCI could provide a more reliable model of hippocampal amnesia is questioned by the heterogeneous nature of this condition, which, as noted, actually includes disparate patterns of age-related cognitive deficits (Petersen 2004). Even when only the amnestic form of MCI is considered, it likely includes patients with memory impairment of various origins (Jicha et al. 2006). Therefore, it seems that the usefulness of the GB procedure as a theoretically driven instrument for differentiating between memory deficits of frontal and hippocampal origin, actually pertains to two cases: 1) discriminating whether an isolated memory deficit in an elderly person is due to incipient AD or to other causes and 2) helping in the differential diagnosis between AD and other etiological forms of dementia. Indeed, according to Braak and Braak’s classical neuropathological model (1995), the memory deficit in preclinical AD closely depends on hippocampal dysfunction and could be differentiated (in the GB procedure) from other forms of aging related memory impairment. On the other side, even though neuropathology spreads to extra-hippocampal regions in clinically manifest AD, the relative burden of hippocampal vs. frontal involvement remains clearly unequal in AD as opposed to non AD dementia patients, thus supporting the feasibility of a differential diagnosis based on the qualitative characteristics of the memory deficit.
In conclusion, further experimental work is needed to support the claim that a memory paradigm which controls for the semantic encoding of incoming stimuli and facilitates retrieval by providing category cues is more effective than other memory procedures in capturing the qualitative features of the memory deficit that characterizes incipient AD and in differentiating AD from other degenerative or vascular dementing and non dementing conditions of the elderly. Future studies in this field could take advantage of independent diagnostic procedures (e.g., structural and functional neuroimaging) to isolate patients with memory disorders that are homogeneous in makeup (i.e., suspected AD pathology vs., for example, vascular dementia) and are at the earliest stages of the disease process, because it is in this phase that clinical/treatment implications might have the greatest impact.
References
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (IV-TR), 4th ed. American Psychiatric Association (ed.) Washington, DC.
Blessed, G., Tomlinson, B. E., & Roth, M. (1968). The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. The British Journal of Psychiatry, 114, 1797–1811.
Braak, H., & Braak, E. (1995). Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiology of Aging, 16, 271–278.
Brown, L. B., & Storandt, M. (2000). Sensitivity of category cued recall to very mild dementia of the Alzheimer type. Archives of Clinical Neuropsychology, 15, 529–534.
Buschke, H., Sliwinski, M. J., Kuslansky, G., & Lipton, R. B. (1997). Diagnosis of early dementia by the Double Memory Test: encoding specificity improves diagnostic sensitivity and specificity. Neurology, 48, 989–997.
Connor, D. J., Salmon, D. P., Sandy, T. J., Galasko, D., Hansen, L. A., & Thal, L. J. (1998). Cognitive profiles of autopsy-confirmed Lewy body variant vs pure Alzheimer disease. Archives of Neurology, 55, 994–1000.
Cummings, J. L. (2003). Toward a molecular neuropsychiatry of neurodegenerative diseases. Annals of Neurology, 54, 147–154.
Davies, R. R., Hodges, J. R., Kril, J. J., Patterson, K., Halliday, G. M., & Xuereb, J. H. (2005). The pathological basis of semantic dementia. Brain, 128, 1984–1995.
De Jager, C., Blackwell, A. D., Budge, M. M., & Sahakian, B. J. (2005). Predicting cognitive decline in healthy older adults. The American Journal of Geriatric Psychiatry, 13, 735–740.
Dubois, B., Feldman, H. H., Jacova, C., Dekosky, S. T., Barberger-Gateau, P., Cummings, J., et al. (2007). Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurology, 6, 734–746.
Erkinjuntti, T., Inzitari, D., Pantoni, L., Wallin, A., Scheltens, P., Rockwood, K., et al. (2000). Research criteria for subcortical vascular dementia in clinical trials. Journal of Neural Transmission. Supplementum, 59, 23–30.
Folstein, M. F., Folstein, S. E., & McHigh, P. R. (1975). The “mini-mental state”: a practical method for grading the cognitive state of patients for the clinicians. Journal of Psychiatric Research, 12, 189–198.
Forman, M. S., Farmer, J., Johnson, J. K., Clark, C. M., Arnold, S. E., Coslett, H. B., et al. (2006). Frontotemporal dementia: clinicopathological correlations. Annals of Neurology, 59, 952–962.
Galasko, D., Katzman, R., Salmon, D. P., & Hansen, L. (1996). Clinical and neuropathological findings in Lewy body dementias. Brain and Cognition, 31, 166–175.
Garrard, P., Lambon-Ralph, M. A., Watson, P. C., Powis, J., Patterson, K., & Hodges, J. R. (2001). Longitudinal profiles of semantic impairment for living and nonliving concepts in dementia of Alzheimer’s type. Journal of Cognitive Neuroscience, 13, 892–909.
Godefroy, O., Roussel, M., Leclerc, X., & Leys, D. (2009). Deficit of episodic memory: anatomy and related patterns in stroke patients. European Neurology, 61, 223–229.
Graham, A., Davies, R., Xuereb, J., Halliday, G., Kril, J., Creasey, H., et al. (2005). Pathologically proven frontotemporal dementia presenting with severe amnesia. Brain, 128, 597–605.
Grober, E., & Buschke, H. (1987). Genuine memory deficit in dementia. Developmental Neuropsychology, 3, 13–36.
Grober, E., Buschke, H., Crystal, H., Bang, S., & Dresner, R. (1988). Screening for dementia by memory testing. Neurology, 38, 900–903.
Grossman, M., Libon, D. J., Forman, M. S., Massimo, L., Wood, E., Moore, P., et al. (2007). Distinct antemortem profiles in patients with pathologically defined frontotemporal dementia. Archives of Neurology, 64, 1601–1609.
Hamilton, J. M., Salmon, D. P., Galasko, D., Delis, D. C., Hansen, L. A., Masliah, E., et al. (2004). A comparison of episodic memory deficits in neuropathologically-confirmed Dementia with Lewy bodies and Alzheimer’s disease. Journal of the International Neuropsychological Society, 10, 689–697.
Ivanoiu, A., Adam, S., Van der Linden, M., Salmon, E., Juillerat, A. C., Mulligan, R., et al. (2005). Memory evaluation with a new cued recall test in patients with mild cognitive impairment and Alzheimer’s disease. Journal of Neurology, 252, 47–55.
Janowsky, J. S., Shimamura, A. P., Kritchevsky, M., & Squire, L. R. (1989). Cognitive impairment following frontal lobe damage and its relevance to human amnesia. Behavioral Neuroscience, 103, 548–560.
Jicha, G. A., Parisi, J. E., Dickson, D. W., Johnson, K., Cha, R., Ivnik, R. J., et al. (2006). Neuropathologic outcome of mild cognitive impairment following progression to clinical dementia. Archives of Neurology, 63, 674–681.
Kazee, A. M., Eskin, T. A., Lapham, L. W., Gabriel, K. R., McDaniel, K. D., & Hamill, R. W. (1993). Clinico-pathological correlates in Alzheimer’s disease: assessment of clinical and pathologic diagnostic criteria. Alzheimer Disease and Associated Disorders, 7, 152–164.
Kovacs, G. G., Botond, G., & Budka, H. (2010). Protein coding of neurodegenerative dementias: the neuropathological basis of biomarker diagnostics. Acta Neuropathologica, 119, 389–408.
Kraybill, M. L., Larson, E. B., Tsuang, D. W., Teri, L., McCormick, W. C., Bowen, J. D., et al. (2005). Cognitive differences in dementia patients with autopsy-verified AD, Lewy body pathology, or both. Neurology, 64, 2069–2073.
Kurz, A., & Perneczky, R. (2010). Novel insights for the treatment of Alzheimer’s disease. Progresses in Neuropsychopharmacology and Biological Psychiatry, doi:10.1016/j.pnpbp.2010.07.018
Lezak, M. D. (2004). Neuropsychological assessment. Oxford University Press United Kingdom.
Libon, D. J., Xie, S. X., Moore, P., Farmer, J., Antani, S., McCawley, G., et al. (2007). Patterns of neuropsychological impairment in frontotemporal dementia. Neurology, 68, 369–375.
Ludolph, A. C., Kassubek, J., Landwehrmeyer, B. G., Mandelkow, E., Mandelkow, E. M., Burn, D. J., et al. (2009). Tauopathies with parkinsonism: clinical spectrum, neuropathologic basis, biological markers, and treatment options. European Journal of Neurology, 16, 297–309.
Mattis, S. (1976). Mental status examination for organic mental syndrome in the elderly patients. In Bellak, L., Karasu, T., B. (eds). Geriatric Psychiatry. (pp 77–101) Grun & Stratton.
McKhann, G., Drachman, D., Folstein, M., Katzman, R., Price, D., & Stadlan, E. M. (1984). Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology, 34, 939–944.
Mitchell, A. J., & Shiri-Feshki, M. (2008). Temporal trends in the long term risk of progression of mild cognitive impairment: a pooled analysis. Journal of Neurology, Neurosurgery and Psychiatry, 79, 1386–1391.
Mitchell, J., Arnold, R., Dawson, K., Nestor, P. J., & Hodges, J. R. (2009). Outcome in subgroups of mild cognitive impairment (MCI) is highly predictable using a simple algorithm. Journal of Neurology, 256, 1500–1509.
Morris, J., C. (1993). The clinical dementia rating (CDR): current version and scoring rules. Neurology, 43, 2412-2414.
Pasquier, F., Grymonprez, L., Lebert, F., & Van der Linden, M. (2001). Memory impairment differs in frontotemporal dementia and Alzheimer’s disease. Neurocase, 7, 161–171.
Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256, 183–194.
Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Tangalos, E. G., & Kokmen, E. (1999). Mild cognitive impairment: clinical characterization and outcome. Archives of Neurology, 56, 303–308.
Petersen, R. C., Doody, R., Kurz, A., Mohs, R. C., Morris, J. C., Rabins, P. V., et al. (2001). Current concepts in mild cognitive impairment. Archives of Neurology, 58, 1985–1992.
Pillon, B., Deweer, B., Michon, A., Malapani, C., Agid, Y., & Dubois, B. (1994). Are explicit memory disorders of progressive supranuclear palsy related to damage to striatofrontal circuits? Comparison with Alzheimer’s, Parkinson’s, and Huntington’s diseases. Neurology, 44, 1264–1270.
Rademakers, R., & Rovelet-Lecrux, A. (2009). Recent insights into the molecular genetics of dementia. Trends in Neurosciences, 32, 451–461.
Rascovsky, K., Salmon, D. P., Ho, G. J., Galasko, D., Peavy, G. M., Hansen, L. A., et al. (2002). Cognitive profiles differ in autopsy-confirmed frontotemporal dementia and AD. Neurology, 58, 1801–1808.
Rascovsky, K., Salmon, D. P., Hansen, L. A., & Galasko, D. (2008). Distinct cognitive profiles and rates of decline on the Mattis Dementia Rating Scale in autopsy-confirmed frontotemporal dementia and Alzheimer’s disease. Journal of the International Neuropsychological Society, 14, 373–383.
Ravaglia, G., Forti, P., Maioli, F., Martelli, M., Servadei, L., Brunetti, N., et al. (2006). Conversion of mild cognitive impairment to dementia: predictive role of mild cognitive impairment subtypes and vascular risk factors. Dementia and Geriatric Cognitive Disorders, 21, 51–58.
Saka, E., Mihci, E., Topcuoglu, M. A., & Balkan, S. (2006). Enhanced cued recall has a high utility as a screening test in the diagnosis of Alzheimer’s disease and mild cognitive impairment in Turkish people. Archives of Clinical Neuropsychology, 21, 745–751.
Salmon, D. P., Thomas, R. G., Pay, M. M., Booth, A., Hofstetter, C. R., Thal, L. J., et al. (2002). Alzheimer’s disease can be accurately diagnosed in very mildly impaired individuals. Neurology, 59, 1022–1028.
Sarazin, M., Berr, C., De Rotrou, J., Fabrigoule, C., Pasquier, F., Legrain, S., et al. (2007). Amnestic syndrome of the medial temporal type identifies prodromal AD: a longitudinal study. Neurology, 69, 1859–1867.
Shimamura, A. P., Janowsky, J. S., & Squire, L. R. (1990). Memory for the temporal order of events in patients with frontal lobe lesions and amnesic patients. Neuropsychologia, 28, 803–813.
Sonnen, J. A., Larson, E. B., Crane, P. K., Haneuse, S., Li, G., Schellenberg, G. D., et al. (2007). Pathological correlates of dementia in a longitudinal, population-based sample of aging. Annals of Neurology, 62, 406–413.
Squire, L. R., Stark, C. E., & Clark, R. E. (2004). The medial temporal lobe. Annual Review of Neuroscience, 27, 279–306.
Tabert, M. H., Manly, J. J., Liu, X., Pelton, G. H., Rosenblum, S., Jacobs, M., et al. (2006). Neuropsychological prediction of conversion to Alzheimer disease in patients with mild cognitive impairment. Archives of General Psychiatry, 63, 916–924.
Tounsi, H., Deweer, B., Ergis, A. M., Van der Linden, M., Pillon, B., Michon, A., et al. (1999). Sensitivity to semantic cuing: an index of episodic memory dysfunction in early Alzheimer disease. Alzheimer Disease and Associated Disorders, 13, 38–46.
Van Hoesen, G. W., & Damasio, A. R. (1987). Neural correlates of cognitive impairment in Alzheimer’s disease. In F. Plum (Ed.), The handbook of physiology, the nervous system, V (pp. 871–898). Baltimore: Williams and Wilkins.
Varma, A. R., Snowden, J. S., Lloyd, J. J., Tablot, P. R., Mann, D. N., & Neary, D. (1999). Evaluation of the NINCDS-ADRDA criteria in the differentiation of Alzheimer’s disease and frontotemporal dementia. Journal of Neurology, Neurosurgery and Psychiatry, 66, 184–188.
Visser, P. J., Verhey, F. R., Ponds, R. W., Cruts, M., Van Broeckhoven, C. L., & Jolles, J. (2000). Course of objective memory impairment in non-demented subjects attending a memory clinic and predictors of outcome. International Journal of Geriatric Psychiatry, 15, 363–372.
Vogel, A., Mortensen, E. L., Gade, A., & Waldemar, G. (2007). The category cued recall test in very mild Alzheimer’s disease: discriminative validity and correlation with semantic memory functions. European Journal of Neurology, 14, 102–108.
von Gunten, A., Bouras, C., Kövari, E., Giannakopoulos, P., & Hof, P. R. (2006). Neural substrates of cognitive and behavioral deficits in atypical Alzheimer’s disease. Brain Research Reviews, 51(2), 176–211.
Wahlund, L. O., Pihlstrand, E., & Jonhagen, M. E. (2003). Mild cognitive impairment: experience from a memory clinic. Acta Neurologica Scandinavica. Supplementum, 179, 21–24.
Disclosures
All authors report no conflicts of interest. They have full control of all primary data and they agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carlesimo, G.A., Perri, R. & Caltagirone, C. Category Cued Recall Following Controlled Encoding as a Neuropsychological Tool in the Diagnosis of Alzheimer’s Disease: A Review of the Evidence. Neuropsychol Rev 21, 54–65 (2011). https://doi.org/10.1007/s11065-010-9153-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-010-9153-7