Abstract
This article presents a review of studies that have investigated the neuropsychological effects of antiretroviral treatment (ART) for HIV-1 infection. It provides a brief overview of the era of monotherapy, dual-therapy, and an extended overview of the current era of combination antiretroviral therapy (CART). This review highlights that while CART has had a dramatic effect on the incidence and the severity of HIV-associated neurocognitive disorders (HAND), HAND, in its mild form, still remains prevalent. New causes of this sustained prevalence are poor CNS penetration of some antiretroviral agents, drug resistance, poor adherence, potential neurotoxicity, co-morbidities such as the long-term CART side effects in relation to cardio-vascular disease, and chronic HIV brain infection that may facilitate the expression of new forms of neurodegenerative processes. The review emphasizes the need to address methodological limitations of published studies and the need for large and representative cross-disciplinary longitudinal investigations across the HIV illness span.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neuropsychological (NP) deficits associated with Human Immunodeficiency Virus type-1 (HIV-1) infection were identified early in the course of the HIV epidemic. For example Ayers et al. (1987) demonstrated a 33% prevalence of NP-impairment in symptomatic HIV-positive individuals. From 1987 to 1995, a large number of studies investigated whether asymptomatic HIV-positive persons (Center for Diseases Control [CDC], 1993 stage A1 and A2) demonstrated a clinically meaningful level of NP dysfunctions. Impairment was observed in a subset of studies providing rigorous definition of NP deficits and comprehensive assessment (White et al. 1995).
During this period, antiretroviral treatment (ART) was seldom considered in NP investigations. Many studies did not clearly report how many of their participants were taking ART, and several studies excluded such participants (Cysique et al. 2006a). One early randomised clinical trial (Schmitt et al. 1988) and two conducted some years later documented the positive effect of AZT monotherapy (also known as zidovudine, ZDV) and dual therapy—a combination of two antiretroviral drugs—(Sidtis et al. 1993; Brouwers et al. 1997) on overall NP performance derived from comprehensive assessments. These studies included HIV-positive persons at various HIV stages and various NP-impairment levels except for Sidtis et al. who included only persons with HIV-associated dementia (HAD), but the latter study had small sample sizes. Lastly, a randomized, double-blind placebo controlled trial (Llorente et al. 2001) of high doses of ZDV (1500 mg/day; N = 46) demonstrated no improvement in any of the NP functions investigated (i.e., four tests evaluating memory, attention and psychomotor speed) at six and 12 month intervals. The authors acknowledged that the inclusion of only mildly symptomatic patients, but no patients with Acquired Immune Deficiency Syndrome (AIDS) conditions may have weakened their ability to detect a treatment effect.
In addition to these clinical trials, some prospective studies demonstrated the positive effect of monotherapy on NP functions. Two of these studies were based on small samples: Reinvang et al. (1991; N = 11); and Tozzi et al. (1993; N = 13). Both found NP improvement in psychomotor speed at five and six months after AZT monotherapy, but deterioration was observed in retested subsets at 12 months. The authors suggested that a possible reason for only transient benefit was the development of drug resistance. A larger study Baldeweg et al. (1995; N = 143) conducted longitudinal comparisons of treated and untreated HIV-infected persons. They observed a positive impact of AZT up to 12 months, more so in AIDS patients, on memory, psychomotor speed, and executive functions. The last study (N = 401) which investigated the effect of AZT or didanosine (ddI) monotherapy vs. dual-therapy AZT in combination with either zalcitabine (ddC), lamivudine (3TC), or stavudine (D4T) was conducted by Arendt et al. (2001). They used a brief electrophysiological evaluation of fine motor functions. Improvement in this area was observed in HIV-positive persons treated with monotherapy but no additive effect of dual-therapy was found.
Several methodological issues can be delineated in the studies described above which will be relevant to the entire review. A substantial number of studies were conducted with small samples or comparisons involving small sub-samples. Treatment effect was tested at various intervals. Variations in NP battery sizes render cross-study comparisons difficult. Some studies also used questionable statistical methodology—a point which will be further developed. Lastly only two studies (Sidtis et al. 1993; Tozzi et al. 1993) determined that all their participants had NP-impairment at baseline using validated NP methodology.
Perhaps most importantly this brief review highlights two methodological principles in studying ART effects in HIV-positive persons, also relevant to the entire review: selection of appropriate samples to study (i.e., HIV-positive persons who have documented NP-impairment in comparison to relevant reference groups) and disease vulnerability (i.e., patients who are most vulnerable to incident NP impairment are those with lower CD4 counts—current or nadir).
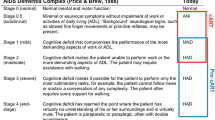
During these first 10 years of the HIV epidemic, HIV-associated Neurocognitive Disorder (HAND) diagnostic criteria were operationalised (American Academy of Neurology 1996). They were updated in 2007 (Antinori et al. 2007). Briefly, these latter criteria recognised three categories of HAND: Asymptomatic Neurocognitive Impairment (ANI, documented mild to moderate NP impairment in at least two cognitive domains without everyday life difficulties); Mild Neurocognitive Impairment (MNI, documented mild to moderate NP impairment in at least two cognitive domains with mild everyday life difficulties), and HIV-associated Dementia (HAD, documented moderate to severe NP impairment in at least two cognitive domains with moderate to severe everyday life difficulties). These guidelines also make recommendations about NP battery size and other relevant neurological investigations. However, they do not provide guidelines for long-term follow-up.
In 1995, the first therapeutic trials of combination therapy started and by 1996-1997 most individuals living in more affluent countries had access to a combination of usually three antiretroviral drugs (sometimes four or five). These combinations often called “Highly Active Antiretroviral Treatment” (HAART) and now more commonly Combination Antiretroviral Treatment (CART) had a dramatic effect on the natural history of HIV as a systemic disease and its more severe neurological manifestations (including HAD). Despite this success, HAND has not been eradicated and remains prevalent as we will detail later.
The review will be structured in two sections: the CART findings, and the new challenges. First, we will review CART findings on NP functions that have been published according to four study designs, and provide methodological examination as well as clinical interpretation. As part of the first section, we will review the issue of drugs’ Central Nervous System (CNS) penetration effectiveness (CPE) and its impact on NP functions. In the second section, we will discuss issues of treatment toxicities, resistance, adherence and their effects on NP functioning as well as issues of chronic infection, cardiovascular diseases and aging. Lastly, Table 1 provides a summary of the review findings and Table 2 provides a summary of the new issues and new challenges to consider for treatment effect studies in long-term NeuroAIDS. Figure 1 illustrates putative profiles of cognitive improvement after successful CART as well as partial cognitive improvement after unsuccessful CART.
a: Estimate of successful CART was defined as a significant reversal of cognitive impairment in HIV-positive individuals diagnosed with HAND and then initiated on CART (see Cysique et al., in press—up to 40%). This is different from the medical definition that is an undetectable viral load in the plasma which was reached up to 60% in the same study. b: Estimate of unsuccessful CART was derived from HAND prevalence in observational cohort studies for HIV-positive individuals who have been on CART for several years (up to 50%)
Neuropsychological Findings in the Cart ERA
Studies Documenting the Beneficial Effect of CART
Currently, there are seven classes of antiretroviral drugs: Nucleoside Reverse Transcriptase Inhibitors (NRTIs); Nucleotide Reverse Transcriptase Inhibitors (NtRTIs); Nonnucleoside Reverse Transcriptase Inhibitors (NNRTIs); Protease Inhibitors (PIs); Fusion Inhibitors; Entry Inhibitors—CCR5 co-receptor antagonist; and HIV integrase strand transfer inhibitors (see online resource: United States Drug & Food Administration [FDA] (2008). While there are new antiretroviral drugs developed each year, the current review includes CART regimens in use between 1996 and January 2009 (date of the current review): NRTIs, NtRTIs NNRTIs, PIs and Fusion inhibitors. The CART era has been characterised by four types of findings (Table 1) relating to four types of study design: 1. Historical cross-sectional cohort studies; 2. Prospective observational cohort studies; 3. Prospective treatment effect studies, and 4. Randomised trials of ART and neuroprotective agents.
Historical Cross-Sectional Cohort Studies
Several investigations explored NP performance on a single testing between HIV-positive individuals initiating CART and clinically comparable individuals who were on dual-therapy or monotherapy. One of these studies showed better cognitive abilities in HIV-positive CART-treated persons in comparison with a demographically comparable pre-CART treated group, especially in the domains of psychomotor speed, attention, verbal learning and verbal memory (Ferrando et al. 1998). However, these results are difficult to interpret as some of the difference may have been due to uncontrolled cohort effects, such as the changing HIV risk factors between treatment eras especially in the U.S. (Sacktor et al. 2002). In this respect, Cysique et al. (2004b) took advantage of the stable HIV risk factors (men who have sex with men) of the Australian HIV epidemic between treatment eras and compared a pre-CART cohort and a post-CART cohort of advanced HIV-positive individuals on a comprehensive NP battery. NP-impairment was determined in each cohort, using NP data from demographically comparable HIV-negative controls that had been tested at the same time as the HIV + cohort. The prevalence of NP impairment did not differ between the pre-and post-CART cohorts. However in NP-impaired subjects, verbal learning and complex attention disturbances were more frequent in the CART-treated group as compared to the pre-CART treated group.
Prospective Observational Cohort Studies
Contrary to the previous historical cross-sectional studies, the following assessed NP functioning over several time points. Some of these longitudinal studies were drawn from observational HIV + cohorts to determine the NP effects of switching from pre-CART to CART in the same individuals. Others compared over-time groups who were on pre-CART versus CART regimens. These studies were observational because, due to Ethics reasons, HIV + individuals could not be randomised into a pre-CART regimen for comparison. Despite this shortcoming, they demonstrated significant NP-improvements when switching to CART, most reliably on psychomotor speed, attention, verbal learning and verbal memory as well as fine motor coordination (Tozzi et al. 1999; Ferrando et al. 2003). Another study compared groups of HIV-positive individuals with psychomotor slowing who were either ART-naïve, or on monotherapy, or on CART over a two-year period on three psychomotor speed tests (Symbol Digit Modalities test; Trail Making Test part B) and one fine motor coordination test (Grooved Pegboard). The CART-treated individuals improved significantly more on these tests as compared to both ART-naïve and monotherapy treated individuals (Sacktor et al. 1999). Another study demonstrated that HIV-positive women,—less represented in other studies—also benefited from CART over an 18-month period compared to clinically comparable HIV-positive women who were not on CART, especially in the domains of psychomotor speed, verbal fluency and executive functions (Cohen et al. 2001).
Other studies have involved long-term follow-up of CART-treated patients over several years (Suarez et al. 2001; Cysique et al. 2006b; McCutchan et al. 2007; Cole et al. 2007; Tozzi et al. 2007; Robertson et al. 2007a). Their findings can be summarised as follows: 1. CART is associated with stable NP functions over the long-term in a majority of individuals. This in turn is more likely if plasma viral load is undetectable and the patient is clinically stable over a long-period of time. 2. Overall severity of NP disturbances has been attenuated by CART in that mild forms of HAND are now more common. 3. Nevertheless, when studies investigated NP decline in individual cases a non-negligible proportion of individuals have demonstrated NP decline (up to 21% incident impairment in addition to 22% of sustained cognitive deficits over the study period in Robertson et al. 2007a, the largest observational prospective study to date N = 991). One study found stable NP performance in all clinically stable, CART-treated HIV-positive individuals (Cole et al. 2007) when focusing on four psychomotor speed measures (Trail Making Test parts A & B; Symbol Digit Modalities Test correct responses and recall), and compared to age comparable controls. Although this study used mixed effect regression allowing control for attrition, number of NP testing and baseline level of NP performance across their groups, it is unclear how many HIV infected individuals were NP-impaired at baseline (see Table 1). Variability in the detection and quantification of cognitive change between studies is likely due to methodological factors such as lack of control for attrition of drop out cases that may have done less well; presence or absence of adequate comparison groups to derive or control for practice effect; as well as ascertainment bias (sub-selection of cohorts with more or less severe HIV disease acuity—acuity being the combination between disease duration and disease severity—Brew et al. 2008).
For example one study that adjusted for attrition, using mixed effects regression modelling (Ferrando et al. 2003) in an advanced HIV infected cohort with moderate HIV disease acuity found that “one-third of this sample continued to be NP-impaired at the end of the study, and nine percent of the patients who were unimpaired at baseline became NP-impaired after 6-12 months of follow-up. Moreover, about two-thirds of them had NP-impairment despite being on HAART and one-third despite having plasma viral loads below detectable limits”. This suggests that CART is not effective for all HIV-positive persons and that the analysis strategy needs to focus on individual change. Cysique et al. (2006b) used a modified Reliable Change Index (Mollica et al. 2004) to determine long-term NP decline in individuals, and these authors reached similar conclusions; that decline occurs despite effective CART in a subset of HIV-positive individuals (in this case, 13% at 12 months). Robertson et al. (2007a) used a multivariate Cox regression proportional hazard model, correcting for age, education, gender and ethnicity as well as multiple assessments, and also reached similar conclusions in a large sample with moderate HIV disease acuity.
Other methodological issues in these studies are that they did not assess the effect of CART by assessing NP performance strictly before and after initiation, and that they included participants with varying lengths of treatment and varying HIV disease advancement. Moreover, some of the largest studies used a limited number of tests covering just a few of the relevant ability domains usually affected in HAND (Sacktor et al. 1999; Cole et al. 2007; Robertson et al. 2007a). Some included patients at varying levels of baseline NP impairment which was not appropriately controlled when NP change was estimated (see Table 1). All but one study (Ferrando et al. 2003) did not explore the causes underlying missing data, as is now recommended by statisticians for analysing longitudinal data (Hedeker and Gibbons 2006).
Prospective Treatment Effect Studies
Contrary to the previous longitudinal studies, the following investigations carefully characterised their participants at baseline, then when CART was initiated, and the participants were re-tested at several targeted time points after CART initiation to quantify NP improvement. However, they also have limitations. The first of these studies was conducted by Sacktor et al. (2003), and used a subsample (n = 49) of the Multicenter AIDS Cohort Study (MACS). These participants were identified as having psychomotor slowing on two NP tests, and were tested before and after CART initiation. Results showed that participants who achieved complete suppression of plasma HIV viral load on CART were more likely to significantly improve on both tests. The second study (Marra et al. 2003) tested 25 HIV-positive individuals on four NP tests - summarized as a total z-score—at baseline (prior CART initiation), and at four and eight weeks after CART initiation. NP improvement was associated with decreased HIV levels in the CSF of the individuals who were ART naïve. The third study included 48 HIV-positive individuals tested prior to CART initiation and six months after, on a comprehensive battery of 17 NP tests (Roberston et al. 2004). This study found significant overall NP improvement as well as significant decrease in plasma and CSF viral load. Letendre et al. (2004) observed overall NP improvement from pre-treatment to 15 weeks after CART initiation, also on a summary score derived from a comprehensive NP battery. Overall NP improvement was associated with CSF viral suppression, highly CNS-penetrating CART regimens and being naïve to ART. Another study has documented the beneficial effect of CART in a resource limited setting (Kampala, Uganda) in 23 advanced HIV-positive persons using a medium size battery (Sacktor et al. 2006). Results showed overall NP improvement from pre-treatment at baseline, at three and six months after CART initiation especially in the domains of psychomotor speed, verbal memory and executive functions.
While these studies demonstrated that CART-related improvement on overall NP performance occurs within a few months, several questions remain. First, because these studies included no comparison group of untreated participants or patients who were on stable treatment, it is not possible to determine how much of the observed NP-impairment is due to practice effect on repeated testing (Rabbitt et al. 2004). Second the studies only used group statistics, and they did not provide an empirical basis for determining NP improvement in individual cases. Therefore it is unclear what proportion of individuals truly benefited, and with what magnitude each benefited. In addition, a non-conservative estimate of NP improvement could bias the magnitude of association between biomarkers and putative NP improvement. Other limitations in some cases included testing change in some participants who were not NP-impaired at baseline, no statistical adjustment for attrition / missing data (or sub-selection of participants with complete data over a certain period of time), testing of a very limited range of NP functions, and the absence of concomitant assessment of the time association (i.e., time Covariance) of HIV RNA suppression, immune recovery and NP change.
A recent study has addressed some of these limitations by using a stricter definition of NP improvement in a group of 37 HIV + persons with HAND at baseline and about to initiate CART (Cysique et al., in press). NP performance change was standardised against a demographically comparable comparison group and corrected for practice effect, regression towards the mean and baseline performance using the regression based change score approach (Heaton et al. 2001). Mixed effect regression modelling was used on the standardised change scores allowing attrition adjustment. The authors found that in some persons with HAND initiating CART, cognitive improvement happens soon after initiation (13% at week 12), but more often 24, 36 and 48 weeks after initiation (up to 41%). In addition, whether the initial NP improvement happens sooner or later, the magnitude of improvement was greater in individuals who had lowest baseline performance, although improvement of lesser magnitude was observable in less impaired participants at baseline. Moreover, greater CART CPE (CPE > 2) was found to be a unique predictor of NP improvement in multivariate analyses, while greater viral load decrease was associated with NP improvement, only in univariate analyses. CSF viral load was not associated with NP improvement which was probably due the lack of variability in this predictor (i.e., 80% of subjects had undetectable viral load just 12 weeks after CART initiation). Limitations in this study were that that the NP battery used covered only a relatively limited range of NP functions (i.e., fine motor-coordination, psychomotor speed, attention/working memory and verbal fluency) as well as having a medium size sample, calling for larger studies.
More work needs to be done to determine which and, to what extent NP functions are likely to improve, and in association with which biological treatment response variables (e.g., magnitude, long-term course and long-term covariations of NP changes). Studies have most reliably demonstrated continued benefit on psychomotor speed functions, an umbrella term which often includes different NP tests and for which long-term construct validity remains to be explored in HIV-positive persons. The rationale for targeting this cognitive ability is that it is a central feature of HAND, correlates with other cognitive abilities and predicts overall NP-impairment at a group level (Sacktor et al. 1996). It also allows NP screening in large samples. Nevertheless, this screening strategy obscures certain complexities or more importantly may sub-select certain type of patients (i.e., if only psychomotor tests are used to establish baseline NP-impairment and change over time). Indeed some studies have found that learning and memory reached a plateau (Suarez et al. 2001) suggesting irreversible deficits in this domain. Future studies also require designs that control for practice effect and other statistical artefacts that may confound the interpretation (e.g., baseline level of impairment) ideally across multiple NP functions, and that use norms for change that allow classification of change in individual participants.
Randomised Trials of ART and Non-ART Agents
In the CART era, only one Phase III randomized, double-blind placebo-controlled trial of an antiretroviral agent (Abacavir, ABC) has been published (Brew et al. 2007). This is in contrast with the monotherapy era, again highlighting the complexity of testing for CART effect on NP functions within ethical standards. This trial aimed at determining the efficacy of adding ABC to optimal stable background CART in HIV + individuals that had been characterised as having mild to moderate HAND. The authors found no difference in cognitive change between the placebo (N = 41) and treatment groups (N = 42) at 12 weeks. They argued that the addition of ABC to CART for persons with HAND was not efficacious, possibly because of the inefficacy of ABC per se, but also potentially because of masked baseline ABC drug resistance, prolonged benefit from existing CART, statistical power issues due to various levels of baseline NP impairment, and lack of disease activity. This trial also highlights the complexities of conducting trials in the context of ongoing CART. The authors make several propositions to improve future trials: 1. Assess drug resistance prior to study entry 2. Enroll CART-treated participants at least 5 months after CART initiation 3. Characterize baseline level of NP-impairment to determine subgroups and sample sizes, and 4. Test whether virally “active” and “inactive” HAND translate into different degree of NP improvement. Concepts of active HAND with no CART, and inactive HAND on successful CART were initially proposed by Brew in 2001, and extended by Brew in 2004).
Illustrative of these issues are the clinical trials that have investigated neuroprotective effects of non-ART agents (see also critical review in Brew 2007) such as memantine (Schifitto et al. 2007a), selegeline (Evans et al. 2007; Schifitto et al. 2007b) and CPI-1189 (Clifford et al. 2002). All failed to demonstrate a positive treatment effect on NP performance in HIV-positive persons with mild to moderate HAND. Most of these studies used brief NP assessment; none took into account the question of virally active and inactive HAND, some were not adequately powered, most argued that the assessment period was too short (less than 6 months) and all assessed NP change only at the group level.
Another complication of the study of NP change in the CART era in persons who are chronically infected with HIV is the heterogeneity of the patient’s past and current CART regimens. A single person across 10 years of HIV infection can have his/her treatment modified many times to manage therapeutic efficacy, side effects and adherence. One related aspect we will discuss here is the issue of CPE of CART regimens.
The Question of CART Regimens’ CNS-penetration Effectiveness in HAND
ART agent entry into the CNS is hampered by the blood brain barrier (BBB) especially for drugs with very high protein binding (i.e., most PIs), low lipid solubility (some NRTIs), high molecular weight (some PIs) (Enting et al. 1998), and for drugs that are substrates for active efflux of transporter systems such as the P-glycoprotein complex (most PIs—Gimenez et al. 2004).
There have been several reports demonstrating that CART composed of agents able to cross the BBB is more effective at improving NP deficits in HIV-positive individuals with HAND. In a longitudinal study of 15 months on average, Cysique et al. (2006b) reproduced their cross-sectional findings (Cysique et al. 2004a) of better NP performance in NP-impaired HIV-positive persons receiving at least three antiretroviral drugs with good CNS penetrance. In addition, Letendre et al. (2004) showed better overall NP improvement 15 weeks after CART initiation in persons with HAND who received a CART with high CPE (CPE > 2) as compared to persons who did not (See Letendre et al. 2008 for details on the CPE score). An analysis of the same study (described above in details—Cysique et al. in press), but this time using a stricter yet more sensitive definition of NP change as well as including all study time points also confirmed that a CPE >2 was associated with NP improvement.
Overall, future studies will need to better anticipate issues of samples’ selection and issues of disease vulnerability as outlined in introduction while determining longitudinal construct validity of NP measures used. These will require the operationalisation of HIV-associated NP decline and improvement in individual cases (Heaton et al. 2001; Cysique and Brew 2009) and use statistical modelling that adjust for attrition to infer NP change from all available data and/or modelling of missing data (Hedeker and Gibbons 2006). HIV infection in the context of CART, however, potentially requires complex modelling of NP change due to the multifactorial effects of HIV disease and CART as well as historical change in the epidemic (e.g., change in demographics and survival bias). One rigorous solution may be studies across the life span (here across HIV illness, therefore starting at the time of primary infection) such as those which have emerged in the field of psychology of aging (e.g., Schaie and Hofer 2001) as well as more randomised trials with innovative designs (e.g., adaptive clinical trials), some of which are underway (May et al. 2007). Indeed, one aspect that will gain importance for chronic HIV infection is the total duration of HIV illness, as well as the duration and severity of symptomatic neurological complications. These factors in combination with others, described next, may help determine to which extent some deficits are irreversible.
New Challenges
Potential Antiretroviral Neurotoxicity
Definite evidence for brain neurotoxicity related to ART is sparse. As for exploring the course of HAND, there are many pitfalls that render these studies hard to undertake. Nevertheless, there are several reasons why drug neurotoxicity is a plausible side effect of CART.
The fact that NRTIs (especially didanosine, stavudine, zalcitabine, and to a lesser extent zidovudine, abacavir and lamivudine) may be responsible for CNS toxicity is based on their documented toxicity on peripheral tissues (e.g., liver, heart, muscles). This toxicity has been shown to involve dysfunction of mitochondria resembling those in genetic mitochondrial diseases (Lewis 2005). The NRTIs’ pharmacologic effectiveness depends on their relative selective interference with viral DNA as opposed to host DNA, especially with long-term treatment (Lewis 2005). Clinically, NRTIs can cause hematologic toxicity, myopathy, cardiomyopathy, lactic acidosis, exocrine pancreas failure, liver failure, bone marrow failure and peripheral neuropathy. Toxicity sometimes reverses when the treatment is stopped but not always. In addition, HIV itself has been shown to cause mitochondrial toxicity (Cherry et al. 2005) and it has been suggested that long-term NRTI treatment may lead to additive mitochondrial toxicity. Some have argued that as in mitochondrial genetic diseases, a threshold of toxicity may have to be reached before obvious clinical signs appear and this is especially true in tissues with high metabolic turnover (e.g., liver and brain; Cherry et al. 2005). While some NRTIs have poor CNS penetration, potentially leading to less mitochondrial toxicity in brain tissues, it has been shown that with advanced HIV infection, the BBB is often impaired (Berger and Avison 2004), therefore increasing the likelihood of NRTIs toxicity in the brain.
To date only one study has directly addressed this issue, and it observed tentative evidence for NRTIs neurotoxicity on brain metabolic functions, as measured by Magnetic Resonance Spectroscopy (MRS) in 18 HIV-positive persons on didanosine and/or stavudine, compared to 14 HIV-positive persons on zidovudine and lamivudine, 16 HIV-positive on no ART, and 17 HIV-negative controls (Schweinsburg et al. 2005). The investigators found that “those taking didanosine and/or stavudine had a significant 11.4% decrease in concentrations of frontal white matter N-Acetayl Aspartate” (NAA—a marker of neuronal integrity; Sullivan et al. 2001) compared with HIV-negative controls, whereas NAA levels of the other HIV-positive groups were intermediate. In addition these authors found that lower levels of frontal white matter NAA were associated with longer periods of didanosine and/or stavudine treatment. The authors argue that NAA depletion may reflect mitochondrial dysfunction and/or depletion of cellular respiration. Clearly, additional studies are needed which would ideally include information such as the CART CPE, CART duration as well as the level of initial cognitive impairment (at the time of CART initiation) and advancement of the disease to infer the fitness of the BBB (Deeks et al. 2001). Also, ideally, a combination of MRS and NP testing both before and after CART initiation would be required to better explore what may be due to CART benefit vs. CART neurotoxicity.
Another tentative finding comes from the ACTG 5170 multicenter prospective study (Robertson et al. 2007b). This 96-week study enrolled 167 advanced HIV-positive persons with planned Structured Treatment Interruption (STI) at entry. In 46 HIV-positive persons who restarted ART before the 96 weeks period, NP testing showed improved cognitive functions that could not be fully explained by practice effect and any selections bias of the sample reinitiating ART. The authors argue that neurotoxicity of long-term CART is a plausible explanation of their findings, which demands specific investigation in the near future.
Another potential cause of neurotoxicity to consider comes from recent in vitro research (Piccinini et al. 2005) which showed that protease inhibitors (nelfinavir and saquinavir) adversely affect human proteasome function. Proteasomes constitute the central process of the ubiquitin ATP-dependent pathway—a central metabolic function involved in cellular defence against a variety of toxins. At therapeutic dosages, nelfinavir and saquinavir inhibited proteasome peptidase activity and caused intracellular accumulation of toxic proteins, a mechanism implicated in cell death. While still speculative, this in vitro result requires further investigation.
CART can also lead to an indirect form of neurotoxicity. Indeed, following treatment initiation some HIV-positive persons can develop a paradoxical neurological deterioration, despite improvements in HIV viral load and CD4 T-cell counts (Riedel et al. 2006). This immune reconstitution inflammatory syndrome (IRIS) has been reported in several case studies which observed the occurrence of a dementing illness (Gray et al. 2005; Venkataramana et al. 2006). While these studies suggest that IRIS may be responsible for HAND worsening in some cases, a recent longitudinal study demonstrated that, long-term, immune reconstituted HIV-positive individuals had improved NP functioning over a 96 weeks period (McCutchan et al. 2007). However, this study did not include an adequate control group so that it remains possible that a minority of participants actually worsen. More longitudinal studies will be necessary to thoroughly address these questions, but it appears from currently available evidence that IRIS would be an uncommon cause of HAND expression or deterioration.
Resistance
Resistance to ART drugs is well documented (Miller and Larder 2001) and clinically translates into treatment failure, and viral load rebound. The emergence of drug-resistant HIV variants is facilitated by the high adaptation capacity of the virus. In addition, HIV mutates in key specific regions under the effect of one ART agent (i.e., providing resistance to this agent), which itself can lead to poorer efficacy for ART agents of the same class or even on occasion multi-drug resistance. Resistance primarily occurs within the context of long-term ART treatment, but it may also be the result of transmission of HIV drug resistant strains in ART-naïve individuals (Verbiest et al. 2001).
There is evidence that HAND may progress despite CART being virologically efficacious systemically (Pialoux et al. 1997) leading to the notion that the CNS may become a reservoir for HIV mutants. It has been shown that resistance is compartmentalised and different between the CNS and systemic tissues (Venturi et al. 2000) and that HAND may be more prevalent in individuals with discordant resistance profile between the CNS and the blood (Cunningham et al. 2000). This process is likely to be compounded by poor ART CNS penetration and/or suboptimal CNS drug concentration, as well as by HIV evolution (mainly mutation leading to resistance). Of even greater concern is the fact that mutations conferring resistance to multiple ART drugs may predominate in brain regions where drug levels are suboptimal (Cunningham et al.; Smit et al. 2004).
NP studies specifically investigating the effect of ART resistance are underway. Preliminary results from the HIV Neurobehavioral Research Center (HNRC) group appear to show that paradoxically, viral resistance to some drugs may render HIV less fit and therefore less neuropathogenic than other viral strains (Hightower et al. 2008). Specifically, it was found that in 94 HIV-positive persons on CART, of whom 20% had detectable resistance specific to some NRTIs. This resistance was associated with lower CSF viral load - but not in the plasma—and better NP performance. This finding, while in keeping with the current understanding of viral resistance dynamics, presently awaits confirmation from other studies, as this was based on a retrospective analysis.
It should be remembered that this finding is almost certainly not a general principle—resistance to only some but not all drugs may be associated with a less fit virus. Indeed, Brew et al. (2007) found that among the causes for abacavir’s lack of efficacy in reversing cognitive disturbance in a large group of patients with HAND, was the high frequency of baseline resistance to the drug (to which the patients were naïve) and which had been acquired most likely through cross resistant drug mutations within the same class of ART agents. In fact, another study from the HNRC group (Strain et al. 2005) with 18 individuals having advanced HIV infection, showed that nine of 13 participants with drug resistance had discordant resistance patterns between the CSF and plasma compartments, supporting other findings (Cunningham et al. 2000). In addition they found that the compartmental differences were associated with the presence of discordant resistance, which they interpreted as reflecting autonomous replication of HIV and independent evolution of drug resistance in the CNS. Furthermore, the discordance of resistance was associated with severity of NP deficits.
Again, on this complex aspect of long-term CART, larger and longer-term prospective studies are needed. Ideally, studies would include a variety of individuals representing a large range of possible mutations, type of CART, disease stage, and HAND stage. If some HIV-mutant variants are less neuropathogenic (Deeks et al. 2001), it is conceivable that others are more neurovirulent due to the high virus adaptability and the presence of a CNS reservoir with low accessibility.
Structured Treatment Interruption
The large Strategies for Management of Anti-Retroviral Therapy (SMART) study has demonstrated that structured treatment interruption (STI) is less beneficial than continuous CART and rapidly leads to viral rebound and worsening of immune functions which are risk factors for HAND (El-Sadr et al. 2006). As a result of these findings, STI is not recommended. However, Childers et al. (2008) argue that STI still occurs frequently for a variety of reasons in clinical practice (e.g., poor adherence, treatment modification, treatment access). These investigators explored NP performance, plasma HIV RNA and CD4 count as well as mood state in 11 HIV-positive individuals at three time points: while on CART prior to STI, after STI (6 months in average), and after reinitiating CART. They found that during STI, plasma HIV RNA increased and CD4 counts declined significantly, and that NP performance did not change. With CART re-initiation, they found that viral loads fell below pre-STI levels, and CD4 counts rose. In addition, improved viral suppression and immune restoration with CART re-initiation were associated with significant improvement in NP performance. Childers et al. therefore concluded that STI of up to 6 months appears to be neurocognitively safe for most patients.
The above mentioned study of Robertson et al. (2007b) yielded different results in that their sample had improved NP performance after STI. These discrepant findings require further investigation, and again ideally using a robust estimate of cognitive change in larger samples. Lastly, the possibility cannot be excluded that the effect of a period of viral rebound and immunosuppression could affect NP functions at a much later time point. Indeed, it is now accepted that low nadir CD4 is a risk factor for cognitive impairment (Valcour et al. 2006a) and incident cognitive impairment (Cysique et al. 2006b) in HIV-positive persons; therefore caution should be exerted when interpreting the above findings.
Adherence
One aspect of chronic diseases with long-term treatment is the question of medication adherence. There is an extensive literature advocating routine assessment of medication adherence of HIV medication (reviewed by Simoni et al. 2006) and targeted and strategic intervention to boost adherence (Bangsberg 2008), as even less than 95% of adherence leads to significant virological rebound and immune function impairment (Chesney 2003), themselves factors for HAND. Incomplete adherence has been associated with the development of drug resistance, disease progression, and death (Bangsberg et al. 2007). Also, poor adherence has been shown to be associated severity of cognitive impairment especially in older adults (Hinkin et al. 2004) and with complex regimens (Hinkin et al. 2002). Some have found that prospective memory deficits in HIV infected people uniquely predict poor adherence (Woods et al. 2008). Also, adherence is often higher in clinical trials than in clinical practice, and this should be taken into consideration in treatment effect studies.
Chronicity of the Disease and Co-morbidities
CART is widely used to treat HIV infection and substantially lowers CNS brain opportunistic infections and neoplasms as well as effectively lengthens patients’ life expectancy (Dore et al. 2003). For patients stable on their medications, HIV infection is now a chronic disease. Despite this success, HAND has not been eradicated and remains as prevalent as before CART (i.e., up to 50% in advanced HIV-positive individuals). Several prevalence studies have provided cumulative evidence of these pictures in different parts of the world (Sacktor et al. 2002; Cysique et al. 2004b; Robertson et al. 2007a; Tozzi et al. 2007; Heaton et al. 2008; Wright et al. 2008). To some extent this high prevalence might be attributed to HAND cases who initially improved on HAART, and then relapsed despite long-term treatment (up to 69% of cases; Tozzi et al. 2007). In addition, for a significant minority of cases (reported to be about 20%), this represents new cognitive deficits despite effective CART (Robertson et al. 2007b).
Increased survival in chronically HIV-positive persons may unfortunately be the fertile ground for co-morbidities that are the indirect consequences of the widespread use of CART such as CART side effects like cardio-vascular disease as well as age-related phenomena. Regarding aging, the concern is that both chronic HIV infection and aging may be the basis for the development of new forms of neurodegenerative processes involving Alzheimer’s Disease (AD) pathology and/or Parkinson Disease (PD) pathology combined with the subcortical deficits initially described as being due to HIV (Brew 2004; Valcour and Paul 2006; Brew et al. 2008). Indeed, if chronic HIV infection lowers the threshold for the clinical presentation of neurodegenerative diseases, then these could likely impact middle-aged patients. In addition, some HIV-positive individuals are reaching an age where these conditions are more prevalent in the general population. A recent international epidemiological study of HAND has found that HIV infection duration, age and age at seroconversion were new risk factors for the development of neurocognitive complications (Bhaskaran et al. 2008). This was despite the use of a poor definition of HAND, potentially missing the majority of the cases (i.e., mild forms of HAND). In the future, not only age may be considered, but also how age interacts in relation to HIV duration and HIV disease acuity (Brew et al. 2008).
Regarding cardio-vascular disease, which also is more common in older persons and a known risk factor for dementia, the number of patients with raised cholesterol and triglycerides is increasing as a result of advancing age, HIV disease itself, and also CART per se, especially the protease inhibitor drugs (Lekakis et al. 2008). Hyperlipidemia as a side effect of long-term CART in HIV-positive persons is often difficult if not impossible to control. Lastly, a study has shown that the increasing degree of insulin resistance, also a side effect of long-term CART, was associated with lower NP performance (Valcour et al. 2006b). Altogether, it could be expected that the nature of HAND may now be based partly on vascular-related cognitive impairment in long-term CART-treated HIV + individuals.
At the moment the NeuroAIDS research community is unsure which and when these factors may happen and become predominant (see Table 2), and how they may operate in various combinations to influence neurobehavioral outcomes in HIV-positive individuals. Our current position is to emphasise that the nature of HAND will increasingly become multifactorial in long-term treated HIV + individuals, potentially leading to several “hybrid” forms of the disease. This concept may in fact be applicable to other chronic form of neurological conditions.
Future Directions
Our review has highlighted the complexity of treatment effect studies in HIV infection and HAND across ART eras. We have emphasized that the understanding of efficacious treatment is multi-factorial and requires sophisticated study designs which would be ideally longitudinal and (at best across the HIV illness span), with large and representative samples (emphasizing collaborate work). Importantly, we have demonstrated that issues of samples’ selection (i.e., HAND severity, HIV disease stage, comparison groups) and issues of disease vulnerability (i.e., risk factors for NP decline or HAND progression) need to be anticipated for improving the interpretability of treatment effect studies. Innovative clinical trial design may open new avenues, such as adaptive clinical trials (Gao et al. 2008). These designs allow more flexible recruitment strategies to increase sample sizes, but they do not replace sound experimental timing and relevant outcome measures, or appropriate longitudinal statistical modelling. Another effort in the current NeuroAIDS research community is to include multiple outcomes (e.g., neuropsychology and neuroimaging). Still, this will demand a reliable estimate of change for all these outcomes, and an understanding of how they co-vary over-time (Cysique and Brew 2009). The relevance of this research is global, and should impact regions/countries where the HIV epidemic is most prevalent and where treatment disparities may lead to greater complexities in understanding HAND evolution.
References
American Academy of Neurology, & Dana Consortium. (1996). Clinical confirmation of the American academy of neurology algorithm for HIV-1-associated cognitive/motor disorder (Dana Consortium on therapy for HIV dementia and related cognitive disorders). Neurology, 47, 1247–1253.
Antinori, A., Arendt, G., Becker, J. T., Brew, B. J., Byrd, D. A., Cherner, M., et al. (2007). Updated research nosology for HIV-associated neurocognitive disorders. Neurology, 69(18), 1789–1799.
Arendt, G., von Giesen, H.-J., Hefter, H., & Theisen, A. (2001). Therapeutic effects of nucleoside analogues on psychomotor slowing in HIV infection. AIDS, 15, 493–500.
Ayers, M., Abrams, D., Newell, T., & Frieddrich, F. (1987). Performance of individuals with AIDS on the Luria-Nebraska Neuropsychological Battery. The International Journal of Clinical Neuropsychology, 9(3), 101–104.
Baldeweg, T., Catalan, J., Lovett, E., Gruzelier, J., Riccio, M., & Hawkins, D. (1995). Long-term Zidovudine reduces neurocognitive deficits in HIV-1 infection. AIDS, 9, 589–596.
Bangsberg, D. R. (2008). Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. Journal of Infectious Diseases, 197(Suppl 3), S272–278.
Bangsberg, D. R., Kroetz, D. L., & Deeks, S. G. (2007). Adherence-resistance relationships to combination HIV antiretroviral therapy. Current HIV/AIDS Reports, 4(2), 65–72.
Berger, J. R., & Avison, M. (2004). The blood brain barrier in HIV infection. Frontiers Biosciences, 9, 2680–2685.
Bhaskaran, K., Mussini, C., Antinori, A., Walker, A. S., Dorrucci, M., Sabin, C., et al. (2008). Changes in the incidence and predictors of Human Immunodeficiency Virus-associated Dementia in the era of highly active antiretroviral therapy. Annals of Neurology, 63(2), 213–221.
Brew, B. J. (2001). Markers of AIDS Dementia Complex: The role of cerebrospinal fluid assays. AIDS, 15(14), 1883–1884.
Brew, B. J. (2004). Evidence for a change in AIDS dementia complex in the era of highly active antiretroviral therapy and the possibility of new forms of AIDS Dementia Complex. AIDS, 18(suppl 1), S75–S78.
Brew, B. J. (2007). Lost in translation: again, another failed neuroprotection trial. Neurology, 69(13), 1308–1309.
Brew, B. J., Halman, M., Catalan, J., Sacktor, N., Price, R. W., Brown, S., et al. (2007). Factors in AIDS dementia complex trial design: Results and lessons from the abacavir trial. PLoS Clinical Trials, 2(3), e13.
Brew, B., Crowe, S. M., Landay, A., Cysique, L., & Guillemin, G. (2008). Neurodegeneration and Ageing in the HAART Era. Journal of Neuroimmune Pharmacology, 6, 6.
Brouwers, P., Hendricks, M., Lietzau, J. A., Pluda, J. M., Mitsuya, H., Broder, S., et al. (1997). Effect of combination therapy with zidovudine and didanosine on neuropsychological functionning in patients with symptomatic HIV disease: A comparison of simultaneous and alternating regimens. AIDS, 11, 59–66.
Center for Diseases Control [CDC]. (1993). 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. Mortality and Morbidity Weekly Report, 41, No. RR-17.
Cherry, C. L., Lala, L., & Wesselingh, S. L. (2005). Mitochondrial toxicity of nucleoside analogues: mechanism, monitoring and management. Sexual Health, 2(1), 1–11.
Chesney, M. (2003). Adherence to HAART regimens. AIDS Patient Care and STDs, 17(4), 169–177.
Childers, M. E., Woods, S. P., Letendre, S., McCutchan, J. A., Rosario, D., Grant, I., et al. (2008). Cognitive functioning during highly active antiretroviral therapy interruption in Human Immunodeficiency Virus type-1 infection. Journal of Neurovirology, 18, 1–8.
Clifford, D. B., McArthur, J. C., Schifitto, G., Kieburtz, K., McDermott, M. P., Letendre, S., et al. (2002). A randomized clinical trial of CPI-1189 for HIV-associated cognitive-motor impairment. Neurology, 59(10), 1568–1573.
Cohen, R., Boland, R., Paul, R., Tashima, K. T., Schoenbaum, E. E., Celentano, D. D., et al. (2001). Neurocognitive performance enhanced by highly active antiretroviral therapy in HIV-infected women. AIDS, 15, 341–345.
Cole, M. A., Margolick, J. B., Cox, C., Li, X., Selnes, O. A., Martin, E. M., et al. (2007). Longitudinally preserved psychomotor performance in long-term asymptomatic HIV-infected individuals. Neurology, 69(24), 2213–2220.
Cunningham, P., Smith, D., Satchell, C., Cooper, D. A., & Brew, B. (2000). Evidence for independent development of resistance to HIV-1 reverse transcriptase inhibitors in the cerebrospinal fluid. AIDS, 14, 1949–1954.
Cysique, L., & Brew, B. (2009). The assessment of HIV-associated neurocognitive disorders: New challenges in the HAART era. In R. Paul, N. Sacktor, V. Valcour & K. Tashima (Eds.), HIV and the Brain: New Challenges in the Modern Era. Totowa, NJ: Humana Press Inc.
Cysique, L., Maruff, P., & Brew, B. (2004a). Antiretroviral therapy in HIV infection: are neurologically active drugs important? Archives of Neurology, 61(11), 1699–1704.
Cysique, L., Maruff, P., & Brew, B. (2004b). Prevalence and pattern of neuropsychological impairment in HIV/AIDS-infection across pre and post- Highly Active Antiretroviral Therapy eras: a combined study of 2 cohorts. Journal of Neurovirology, 10, 350–357.
Cysique, L., Maruff, P., & Brew, B. (2006a). The neuropsychological profile of symptomatic, AIDS and ADC patients in the pre-HAART era: a meta-analysis. Journal of the International Neuropsychological Society, 12, 1–15.
Cysique, L. A., Maruff, P., & Brew, B. J. (2006b). Variable benefit in neuropsychological function in HIV-infected HAART-treated patients. Neurology, 66(9), 1447–1450.
Cysique, L., Vaida, F., Letendre, S., Gibson, S., Woods, S., Cherner, M., et al. (in press). Dynamics of cognitive change in impaired HIV + individuals initiating antiretroviral therapy. Neurology.
Deeks, S. G., Wrin, T., Liegler, T., Hoh, R., Hayden, M., Barbour, J. D., et al. (2001). Virologic and immunologic consequences of discontinuing combination antiretroviral-drug therapy in HIV-infected patients with detectable viremia. New England Journal of Medicine, 344(7), 472–480.
Dore, G. J., McDonald, A., Li, Y., Kaldo, J. M., & Brew, B. J. (2003). Marked improvement in survival following AIDS Dementia Complex in the era of highly active antiretroviral therapy. AIDS, 17, 1539–1545.
El-Sadr, W. M., Lundgren, J. D., Neaton, J. D., Gordin, F., Abrams, D., Arduino, R. C., et al. (2006). CD4 + count-guided interruption of antiretroviral treatment. New England Journal of Medicine, 355(22), 2283–2296.
Enting, R., Hoetelmans, R., Lange, J., Burger, D. M., Beijnen, J. H., & Portegies, P. (1998). Antiretroviral drugs and the central nervous system. AIDS, 12, 1941–1953.
Evans, S. R., Yeh, T. M., Sacktor, N., Clifford, D. B., Simpson, D., Miller, E. N., et al. (2007). Selegiline transdermal system (STS) for HIV-associated cognitive impairment: open-label report of ACTG 5090. HIV Clinical Trials, 8(6), 437–446.
Ferrando, S., Van Gorp, W., McElhiney, M., Goggin, K., Sewell, M., & Rabkin, J. (1998). Highly active antiretroviral treatment in HIV infection: benefits for neuropsychological function. AIDS, 12(8), F65–F70.
Ferrando, S. J., Rabkin, J. G., van Gorp, W. G., Lin, S.-H., & McElhiney, M. (2003). Longitudinal improvement in psychomotor processing is associated with potent antiretroviral therapy in HIV-1 infection. Journal of Neuropsychiatry and Clinical Neurosciences, 15(2), 208–214.
Gao, P., Ware, J. H., & Mehta, C. (2008). Sample size re-estimation for adaptive sequential design in clinical trials. Journal of Biopharmaceutical Statistics, 18(6), 1184–1196.
Gimenez, F., Fernandez, C., & Mabondzo, A. (2004). Transport of HIV protease inhibitors through the blood-brain barrier and interactions with the efflux proteins, P-glycoprotein and multidrug resistance proteins. Journal of Acquired Immune Deficiency Syndrome, 36(2), 649–658.
Gray, F., Bazille, C., Adle-Biassette, H., Mikol, J., Moulignier, A., & Scaravilli, F. (2005). Central nervous system immune reconstitution disease in Acquired Immunodeficiency Syndrome patients receiving highly active antiretroviral treatment. Journal of Neurovirology, 11(Suppl 3), 16–22.
Heaton, R., Temkin, N., Dikmen, S., Avitable, N., Taylor, M., Marcotte, T., et al. (2001). Detecting change: A comparison of three neuropsychological methods, using normal and clinical samples. Archives of Clinical Neuropsychology, 16(1), 75–91.
Heaton, R. K., Cysique, L. A., Jin, H., Shi, C., Yu, X., Letendre, S., et al. (2008). Neurobehavioral effects of human immunodeficiency virus infection among former plasma donors in rural China. Journal of Neurovirology, 7, 1–14.
Hedeker, D., & Gibbons, R. D. (2006). Longitudinal Data Analysis. Hoboken, NJ: Wiley.
Hightower, G., Letendre, S., Cherner, M., Gibson, S., Ellis, R., Ignacio, C., et al. (2008). ART Resistance Influences CSF HIV RNA Levels and Neuropsychological Performance in HIV-infected Individuals Poster presented at the 15th Conference on Retroviruses and Opportunistic Infections, February 3-6.
Hinkin, C. H., Castellon, S. A., Durvasula, R. S., Hardy, D. J., Lam, M. N., Mason, K. I., et al. (2002). Medication adherence among HIV + adults: Effects of cognitive dysfunction and regimen complexity. Neurology, 59(12), 1944–1950.
Hinkin, C. H., Hardy, D. J., Mason, K. I., Castellon, S. A., Durvasula, R. S., Lam, M. N., et al. (2004). Medication adherence in HIV-infected adults: effect of patient age, cognitive status and substance. AIDS, 18(suppl 1), S19–S25.
Lekakis, J., Tsiodras, S., Ikonomidis, I., Palios, J., Poulakou, G., Rallidis, L., et al. (2008). HIV positive patients treated with protease inhibitors have vascular changes resembling those observed in atherosclerotic cardiovascular disease. Clinical Science (London, England), 5, 5.
Letendre, S., Marquie-Beck, J., Capparelli, E., Best, B., Clifford, D., Collier, A. C., et al. (2008). Validation of the CNS penetration-effectiveness rank for qualifying antiretroviral penetration into the central nervous system. Archives of Neurology, 65(1), 65–70.
Letendre, S., McCutchan, J., Childers, M., Woods, S., Lazzaretto, D., Heaton, R., et al. (2004). Enhancing antiretroviral therapy for Human Immunodeficiency Virus cognitive disorders. Annals of Neurology, 56(3), 416–423.
Lewis, W. (2005). Nucleoside reverse transcriptase inhibitors, mitochondrial DNA and AIDS therapy. Antiviral Therapy, 10(Suppl 2), M13–27.
Llorente, A. M., van Gorp, W. G., Stern, M. J., George, L., Satz, P., Marcotte, T. D., et al. (2001). Long-term effects of high-dose zidovudine treatment on neuropsychological performance in mildly symptomatic HIV-positive patients: results of a randomized, double-blind, placebo-controlled investigation. Journal of the International Neuropsychological Society, 7, 27–32.
Marra, C. M., Lockhart, D., Zunt, J. R., Perrin, M., Coombs, R. W., & Collier, A. C. (2003). Changes in CSF and plasma HIV-1 RNA and cognition after starting potent antiretroviral therapy. Neurology, 60, 1388–1390.
May, S., Letendre, S., Haubrich, R., McCutchan, J. A., Heaton, R., Capparelli, E., et al. (2007). Meeting practical challenges of a trial involving a multitude of treatment regimens: an example of a multi-center randomized controlled clinical trial in neuroAIDS. Journal of Neuroimmune Pharmacology, 2(1), 97–104.
McCutchan, J. A., Wu, J. W., Robertson, K., Koletar, S. L., Ellis, R. J., Cohn, S., et al. (2007). HIV suppression by HAART preserves cognitive function in advanced, immune-reconstituted AIDS patients. AIDS, 21(9), 1109–1117.
Miller, V., & Larder, B. A. (2001). Mutational patterns in the HIV genome and cross-resistance following nucleoside and nucleotide analogue drug exposure. Antiviral Therapy, 6(Suppl 3), 25–44.
Mollica, C., Maruff, P., & Vance, A. (2004). Development of a statistical approach to classifying treatment response in individual children with ADHD. Human Psychopharmacology, 19(7), 445–456.
Pialoux, G., Fournier, S., Moulignier, A., Poveda, J., Clavel, F., & Dupont, B. (1997). Central nervous system as a sanctuary for HIV-1 infection despite treatment with zidovudine, lamivudine and indinavir. AIDS, 11(10), 1302–1303.
Piccinini, M., Rinaudo, M. T., Anselmino, A., Buccinna, B., Ramondetti, C., Dematteis, A., et al. (2005). The HIV protease inhibitors nelfinavir and saquinavir, but not a variety of HIV reverse transcriptase inhibitors, adversely affect human proteasome function. Antiviral Therapy, 10(2), 215–223.
Rabbitt, P., Diggle, P., Holland, F., & McInnes, L. (2004). Practice and drop-out effects during a 17-year longitudinal study of cognitive aging. Journal of Gerontology Psychological Sciences, 59B(2), 84–97.
Reinvang, I., Froland, S., Karlsen, N., & Lundervold, A. (1991). Only temporary improvement in impaired neuropsychological function in AIDS patients treated with zidovudine. AIDS, 5(2), 228–229.
Riedel, D. J., Pardo, C. A., McArthur, J., & Nath, A. (2006). Therapy Insight: CNS manifestations of HIV-associated immune reconstitution inflammatory syndrome. Nature Clinical Practice Neurology, 2(10), 557–565.
Roberston, K., Roberston, T. W., Ford, S., Watson, D., Fiscus, S., Harp, A. G., et al. (2004). Highly Active Antiretroviral Therapy improves neurocognitive functioning. Journal of Acquired Immune Deficiency Syndrome, 36(1), 562–566.
Robertson, K. R., Smurzynski, M., Parsons, T. D., Wu, K., Bosch, R. J., Wu, J., et al. (2007a). The prevalence and incidence of neurocognitive impairment in the HAART era. AIDS, 21(14), 1915–1921.
Roberston, K., Su, Z., Krambrink, A., Evans, S. R., Havlir, D., Margolis, D., et al. (2007b). This Is Your Brain off Drugs: Neurocognitive Function before and after ART Discontinuation in Patients with High CD4 Nadir (ACTG A5170). Paper presented at the 14th Conference on Retroviruses and Opportunistic Infections February 25 -February 28.
Sacktor, N. C., Bacellar, H., Hoover, D. R., Nance-Sproson, T. E., Selnes, O. A., Miller, E. N., et al. (1996). Psychomotor slowing in HIV infection: a predictor of dementia, AIDS and death. Journal of Neurovirology, 2, 404–410.
Sacktor, N. C., Lyles, R. H., Skolasky, R. L., Anderson, D. E., McArthur, J. C., McFarlane, G., et al. (1999). Combination antiretroviral therapy improves psychomotor speed performance in HIV-seropositive homosexual men. Neurology, 52, 1640–1647.
Sacktor, N., McDermott, M., Marder, K., Schifitto, G., Selnes, O. A., McArthur, J. C., et al. (2002). HIV-associated cognitive impairment before and after the advent of combination therapy. Journal of Neurovirology, 8, 136–142.
Sacktor, N., Skolasky, R. L., Tarwater, P. M., McArthur, J. C., Selnes, O. A., Becker, J., et al. (2003). Response to systemic HIV viral load suppression correlates with psychomotor speed performance. Neurology, 61, 567–569.
Sacktor, N., Nakasujja, N., Skolasky, R., Robertson, K., Wong, M., Musisi, S., et al. (2006). Antiretroviral therapy improves cognitive impairment in HIV + individuals in sub-Saharan Africa. Neurology, 67(2), 311–314.
Schaie, K. W., & Hofer, S. M. (2001). Handbook of the Psychology of Aging. In K. W. Schaie & J. E. Birren (Eds.), Longitudinal studies in aging research (5th ed.). San Diego: Academic Press.
Schifitto, G., Navia, B. A., Yiannoutsos, C. T., Marra, C. M., Chang, L., Ernst, T., et al. (2007a). Memantine and HIV-associated cognitive impairment: a neuropsychological and proton magnetic resonance spectroscopy study. AIDS, 21(14), 1877–1886.
Schifitto, G., Zhang, J., Evans, S. R., Sacktor, N., Simpson, D., Millar, L. L., et al. (2007b). A multicenter trial of selegiline transdermal system for HIV-associated cognitive impairment. Neurology, 69(13), 1314–1321.
Schmitt, F. A., Bigley, J. W., McKinnis, R., Logue, P. E., Evans, R. W., Drucker, J. L., et al. (1988). Neuropsychological outcome of Zidovudine (AZT) treatment fo patients with AIDS and AIDS related-complex. New England Journal of Medicine, 319, 1573–1578.
Schweinsburg, B. C., Taylor, M. J., Alhassoon, O. M., Gonzalez, R., Brown, G. G., Ellis, R. J., et al. (2005). Brain mitochondrial injury in Human Immunodeficiency Virus-seropositive (HIV+) individuals taking nucleoside reverse transcriptase inhibitors. J Neurovirol, 11(4), 356–364.
Sidtis, J. J., Gatsonis, C., Price, R. W., Singer, E. J., Collier, A. C., Richman, D. D., et al. (1993). Zidovudine treatment of the AIDS Dementia Complex: results of a placebo-controlled trial. Annals of Neurology, 33, 343–349.
Simoni, J. M., Kurth, A. E., Pearson, C. R., Pantalone, D. W., Merrill, J. O., & Frick, P. A. (2006). Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior, 10(3), 227–245.
Smit, T. K., Brew, B. J., Tourtellotte, W., Morgello, S., Gelman, B. B., & Saksena, N. K. (2004). Independent evolution of human immunodeficiency virus (HIV) drug resistance mutations in diverse areas of the brain in HIV-infected patients, with and without dementia, on antiretroviral treatment. Journal of Virology, 78(18), 10133–10148.
Strain, M. C., Letendre, S., Pillai, S. K., Russell, T., Ignacio, C. C., Gunthard, H. F., et al. (2005). Genetic composition of Human Immunodeficiency Virus type-1 in cerebrospinal fluid and blood without treatment and during failing antiretroviral therapy. Journal of Virology, 79(3), 1772–1788.
Suarez, S., Baril, L., Stankoff, B., Khellaf, M., Dubois, B., Lubetski, C., et al. (2001). Outcome of patients with HIV-1 related cognitive impairment on highly active antiretroviral therapy. AIDS, 15, 192–200.
Sullivan, E. V., Adalsteinsson, E., Spielman, D. M., Hurd, R. E., & Pfefferbaum, A. (2001). N-acetylaspartate–a marker of neuronal integrity. Annals of Neurology, 50(6), 823.
Tozzi, V., Narciso, P., & Calgani, S. (1993). Effects of Zidovudine in 30 patients with mild to end-stage AIDS Dementia Complex. AIDS, 7, 638–692.
Tozzi, V., Balestra, P., Galgani, S., Narciso, P., Ferri, F., Sebastiani, G., et al. (1999). Positive and sustained effects of highly active antiretroviral therapy on HIV-1 associated neurocognitive impairment. AIDS, 13, 1889–1897.
Tozzi, V., Balestra, P., Bellagamba, R., Corpolongo, A., Salvatori, M. F., Visco-Comandini, U., et al. (2007). Persistence of neuropsychological deficits despite long-term highly active antiretroviral therapy in patients with HIV-related neurocognitive impairment: prevalence and risk factors. Journal of Acquired Immune Deficiency Syndrome, 45(2), 174–182.
U.S. Food and Drug Administration [FDA]. (2008). Drugs Used in the Treatment of HIV Infection. Retrieved November 2008 <http://www.fda.gov/oashi/aids/virals.html >
Valcour, V., & Paul, R. (2006). HIV infection and dementia in older adults. Clinical Infectious Diseases, 42(10), 1449–1454.
Valcour, V., Yee, P., Williams, A. E., Shiramizu, B., Watters, M., Selnes, O., et al. (2006a). Lowest ever CD4 lymphocyte count (CD4 nadir) as a predictor of current cognitive and neurological status in human immunodeficiency virus type 1 infection–The Hawaii Aging with HIV Cohort. Journal of Neurovirology, 12(5), 387–391.
Valcour, V. G., Sacktor, N. C., Paul, R. H., Watters, M. R., Selnes, O. A., Shiramizu, B. T., et al. (2006b). Insulin resistance is associated with cognition among HIV-1-infected patients: the Hawaii Aging with HIV cohort. Journal of Acquired Immune Deficiency Syndrome, 43(4), 405–410.
Venkataramana, A., Pardo, C. A., McArthur, J. C., Kerr, D. A., Irani, D. N., Griffin, J. W., et al. (2006). Immune reconstitution inflammatory syndrome in the CNS of HIV-infected patients. Neurology, 67(3), 383–388.
Venturi, G., Catucci, M., Romano, L., Corsi, P., Leoncini, F., Valensin, P. E., et al. (2000). Antiretroviral resistance mutations in human immunodeficiency virus type 1 reverse transcriptase and protease from paired cerebrospinal fluid and plasma samples. The Journal of Infectious Diseases, 181, 740–745.
Verbiest, W., Brown, S., Cohen, C., Conant, M., Henry, K., Hunt, S., et al. (2001). Prevalence of HIV-1 drug resistance in antiretroviral-naive patients: a prospective study. AIDS, 15(5), 647–650.
White, D. A., Heaton, R., & Monsch, A. U. (1995). Neuropsychological studies of asymptomatic Human Immunodeficiency Virus-type-1 infected individuals. Journal of the International Neuropsychological Society, 1, 304–315.
Woods, S. P., Moran, L. M., Carey, C. L., Dawson, M. S., Iudicello, J. E., Gibson, S., et al. (2008). Prospective memory in HIV infection: is "remembering to remember" a unique predictor of self-reported medication management? Archives of Clinical Neuropsychology, 23(3), 257–270.
Wright, E., Brew, B., Arayawichanont, A., Robertson, K., Samintharapanya, K., Kongsaengdao, S., et al. (2008). Neurologic disorders are prevalent in HIV-positive outpatients in the Asia-Pacific region. Neurology, 71(1), 50–56.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cysique, L.A., Brew, B.J. Neuropsychological Functioning and Antiretroviral Treatment in HIV/AIDS: A Review. Neuropsychol Rev 19, 169–185 (2009). https://doi.org/10.1007/s11065-009-9092-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-009-9092-3