Abstract
Neuropathic pain is one of the most common conditions requiring treatment worldwide. Salidroside (SAL), a phenylpropanoid glucoside extracted from Rhodiola, has been suggested to produce an analgesic effect in chronic pain. However, whether SAL could alleviate pain hypersensitivity after peripheral nerve injury and its mode of action remains unclear. Several studies suggest that activation of the spinal NOD-like receptor protein 3 (NLRP3) inflammasome and its related proteins contribute to neuropathic pain’s pathogenesis. This study investigates the time course of activation of spinal NLRP3 inflammasome axis in the development of neuropathic pain and also whether SAL could be an effective treatment for this type of pain by modulating NLRP3 inflammasome. In the chronic constriction injury (CCI) mice model, spinal NLRP3 inflammasome-related proteins and TXNIP, the mediator of NLRP3, were upregulated from the 14th to the 28th day after injury. The TXNIP and NLRP3 inflammasome-related proteins were mainly present in neurons and microglial cells in the spinal dorsal horn after CCI. Intraperitoneal injection of SAL at 200 mg/kg for 14 consecutive days starting from the 7th day of CCI injury could ameliorate mechanical and thermal hypersensitivity in the CCI model. Moreover, SAL inhibited the activation of the TXNIP/NLRP3 inflammasome axis and mitigated the neuronal loss of spinal dorsal horn induced by nerve injury. These results indicate that SAL could produce analgesic and neuroprotective effects in the CCI model of neuropathic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain is highly prevalent, affecting 6–8% of the general adult population worldwide. The limitations and challenges of the clinical treatment for neuropathic pain result in considerable life and economic burden for patients, leading to high healthcare costs and productivity loss. Patients suffering from neuropathic pain exhibit varying degrees of mechanical and thermal hypersensitivity. These manifestations are also observed in animal models with peripheral nerve injuries, such as chronic constriction injury (CCI) and spared nerve injury [1]. A lesion in the peripheral nervous system leads to neuroinflammation, a localized inflammation occurring in the peripheral and central nervous system, including activation and infiltration of leukocytes, activation of glial cells, and increased production of inflammatory mediators. Persistent neuroinflammation contributes significantly to the persistence of neuropathic pain [2].
Inflammasomes are a group of pattern recognition receptors that can detect pathogen- or damage-associated molecular patterns and subsequently activate inflammatory responses. To date, there are six known inflammasome multiprotein complexes: NACHT, LRR, and PYD/CARD domains containing proteins NLRP1, NLRP3, NLRP6, NLRP12, and NLRC4, and AIM2 [3]. Of all the NLR inflammasomes, NLRP3 is an essential molecular platform [4], which on activation, cleaves pro-caspase-1 and pro-IL-1β into their active forms [5]. Thioredoxin-interacting protein (TXNIP), also known as thioredoxin-binding protein-2 or vitamin D3 upregulated binding protein-2, binds NLRP3 and leads to its activation in conditions of oxidative stress, which is an essential step in the signaling pathway activated by NLRP3 inflammasome [6, 7]. As IL-1β is a well-known pain-inducing molecule, the NLRP3 inflammasome has been implicated in the pathology of many painful diseases and conditions such as bladder pain [8], metastatic cancer-induced bone pain [9], chemotherapy-induced peripheral neuropathy [10], pain caused by burns [11], post-operative pain [12], migraine [13], etc. Yet, varied outcomes have also been reported by studies assessing the contribution of NLRP3 to neuropathic pain [14,15,16], which may be accompanied by significant neuroinflammation. Increased expression and activation of NLRP3 and increased production of IL-1β have been reported in several rodent models of nerve injury and chemotherapy-induced neuropathic pain. Additionally, active caspase-1 cleaves the pore former pro-gasdermin D into its active form, inducing pyroptosis, a form of inflammatory cell death [17]. Nonetheless, there is lack of direct evidence on the specific contribution of spinal TXNIP/NLRP3 pathway to the development or the maintenance phase of neuropathic pain.
Salidroside (SAL), a phenylpropanoid glycoside compound [2-(4-hydroxyphenyl)-ethyl-β-d-glucopyranoside], is the main active ingredient in Rhodiola rosea. R. rosea is a precious plant growing at high altitudes, and has been used as a traditional medicine for treating high altitude sickness for hundreds of years. The literature reports that salidroside exhibits neuroprotective activities in the central nervous system, including protective effects against Alzheimer’s disease [18, 19], Parkinson’s disease [20, 21], stroke [22, 23], Huntington’s disease [24], and depression [25]. In a painful diabetic neuropathy model, SAL treatment also has an analgesic effect by inhibiting the P2X7 receptor pathway [26]. However, it is still unclear whether SAL alleviates the pain and hypersensitivity induced by peripheral nerve injury.
Materials and Methods
Animals
Adult male C57/BL 6 N mice (8–10 weeks old, 23 g–25 g, Charles River Experimental Animal Technical Co., Ltd., Beijing, China) were housed in SPF level lab with a 12 h light-12 h dark cycle at a constantly maintained temperature (23 ± 2 ℃), and allowed free access to food and water. The animal study was reviewed and approved by the Capital Medical University Animal Care and Use Committee.
Chronic Constriction Nerve Injury (CCI) Model
Mice were anesthetized with isoflurane (1.0–1.5% in 100% O2, 0.5 L/min), and the body temperature was maintained at 36 °C with a heating pad. The biceps femoris and gluteus muscles were separated through blunt dissection and the sciatic nerve was exposed. The sciatic nerve was ligated with 6–0 silk thread (Cheng-He, China) at three knots with an interval of approximately 1 mm. The ligation strength of each knot is based on the slight indentation of the sciatic nerve observed under the microscope, and the slight twitching of the muscles around the exposed site. The sciatic nerve of sham group mice was exposed in the same method, but not ligated [27, 28].
Nociceptive Assays
von Frey test: Mice were allowed to acclimate to the acrylic chambers with a metal mesh platform for 3 days (15 min/day) before the baseline testing. When the mice were motionless and sober, the von Frey hairs (NC12775, Northcoast-Medical, USA) were used to apply pressure, which began at 0.16 g and progressed according to an up-down method. As described previously [29], the von Frey hairs were bent into a S shape and held for five seconds underneath the hind paw. The withdrawal or licking the hind paw were considered as positive responses.
Hargreaves test: Mice were placed into the acrylic cases with a transparent glass platform for 3 days (30 min/day) to acclimate before the baseline testing. When the mice were motionless and sober, the thermal emitter of hargreaves apparatus (37,370, ugo-basile, Italy) was set on 16–19 intensity. Withdrawal or lick of the hind paw was considered a positive response when mice hind paw was stimulated with a radiant heat. The withdrawal latency was recorded 3 times for each hind paw, with an interval of 5 min. The cutoff time for stimulation was set to 25 s to avoid tissue damage [30].
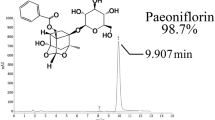
Salidroside (Sal) Treatment
After the CCI surgery for 7 days, the sham and CCI mice were treated with vehicle (normal saline) or different doses of SAL (100 or 200 mg/kg, i.p.) (110,818, National Institutes for Food and Drug Control, China) for 14 consecutive days.
Immunohistochemistry
Twenty one days after surgery, mice were anesthetized with 1% pentobarbital sodium (10 ml/kg) and transcardially perfused with 0.01 M PBS and 4% paraformaldehyde. L3–L5 spinal cord was taken and post fixed in 4% paraformaldehyde at 4 °C for overnight. Tissue was placed in 20% sucrose in 0.01 M PBS at 4 °C for 24 h and then in 30% sucrose in 0.01 M PBS at 4 °C for 48 h. Subsequently, tissue was embedd in OCT, and performed frozen section (16 μm) using a cryotome (CM3050 S, Leica Microsystems, Germany). The sections were treated with sodium citrate antigen retrieval solution for 10 min in 95 °C and then 1% Triton-X-100 for 15 min, followed by 3 washes for 5 min each with 0.01 M PBS, incubation with 0.3% H2O2 for 10 min, and 3 washes for 5 min each with 0.01 M PBS. After blocking for 30 min with 5% goat serum containing 0.3% Triton-X-100, sections were respectively incubated with following antibodies dissolved in 1% goat serum in 0.3% Triton-X-100 overnight at 4 °C: TXNIP (1:200; A9342, ABclonal, China), NLRP3 (1:200; A12694, ABclonal, China), caspase-1 (1:200; A0964, ABclonal, China), IL-1β (1:200; A17361, ABclonal, China), NeuN (1:500; MAB377, Merck, USA), GFAP(1:500; G3893, Sigma-Aldrich, USA), and Iba1(1:50; ab48004, abcam, USA). After washing 3 times with 0.01 M PBS for 5 min each, sections were incubated with secondary antibody (1:500; Invitrogen, USA) for 1 h at room temperature. After washing, sections were mounted with DAPI (ab104139, abcam, USA) in dark, and then coverslipped. Immunohistochemical images were taken using a microscope (DS-iR2, Nikon) for each section, and the positive cells in ipsilateral spinal cord were counted using ImageJ software.
Western Blot
Mice were anesthetized with 1% pentobarbital sodium (10 ml/kg), and then the whole spinal cord of L3–L5 segments was taken. Tissues were lysed in RIPA lysis buffer (C1053, Applygen, China), and then performed protein quantification using BCA protein assay kit (23,227, Thermo Scientific, USA). All protein samples were separated by 10% or 12% SDS-PAGE gels (ZD304, ZOMANBIO, China), transferred to PVDF membranes (1,620,177, Bio-rad, USA) that were blocked in 5% nonfat dry milk for 60 min, and incubated with the following antibodies (in TBST containing 5% nonfat dry milk) at 4 °C for overnight: TXNIP (1:1000; sc-271237, Santa Cruz, U.S.A), NLRP3 (1:1000; A14223, ABclonal, China), caspase-1 (1:1000; A0964, ABclonal, China), IL-1β (1:1000; A17361, ABclonal, China), and α-tubulin (1:10,000; B1052, Biodragon, China). Next, after washing with TBST, they were incubated with secondary antibody (1:1000, Cell Signaling Technology, U.S.A) for 1 h at room temperature. Finally, Proteins were detected by ECL reagents (WBKLS0500, Millipore, USA). The relative intensity of proteins were quantified by ImageJ software.
Cresyl Violet (CV) Staining
CV staining is used to observe neurons with no damage or minimal damage, which are stained blue [31]. Sections were washed with 0.01 M PBS for 5 min, dried in oven at 56 °C for 30 min, immersed into 70% ethyl alcohol for overnight at room temperature, and then stained with 0.2% cresyl violet solution for 5 min. After washing with ddH2O for 1 min, sections were dehydrated in graded ethanol, cleared with xylene and mounted with coverslips. Images were taken using a microscope (DS-iR2, Nikon) for each section, and the cells positively stained by CV in ipsilateral spinal cord were counted using ImageJ software.
Fluoro-Jade C (FJC) Staining
FJC is mainly used to visualize already damaged neurons, which are stained green [32]. After washing 5 min with 0.01 M PBS, sections dried in oven at 56 °C for 30 min. Subsequently, they were successively immersed into ethyl alcohol containing 1% sodium hydroxide for 2 min, into 70% ethyl alcohol for 2 min, and into ddH2O for 2 min, and incubated with 0.06% potassium permanganate solution for 10 min on a shaker. After washing with ddH2O, these sections were stained with 0.0004% FJC solution for 20 min in the dark, cleared with xylene and then mounted with coverslips. Images were taken using a microscope (DS-iR2, Nikon) for each section, and the cells positively stained by FJC in ipsilateral spinal cord were counted using ImageJ software.
Statistical Analysis
All data were represented as the mean ± SEM, and analyzed using GraphPad Prism 7.00 (GraphPad Software, USA). Two-tailed unpaired t-test was used to compare means for two groups. A one-way ANOVA test or two-way ANOVA test was used to compare the means of more than two groups. Once differences were determined to exist among the means, Dunnett's test or Tukey's test was used for pairwise multiple comparisons between any two groups, which depends on homogeneity of variance. P values less than 0.05 were considered statistically significant.
Results
The Spinal Protein Level of the TXNIP/NLRP3 Axis was Found to be Upregulated in the CCI Model
Compared to sham animals, paw withdrawal threshold (PWT) to mechanical stimuli and paw withdrawal latency (PWL) to heat stimuli of nerve-injured (ipsilateral) hind paw were found to be significantly decreased in CCI mice from the 7th to the 28th-day post-injury (dpi). The PWT and PWL of the contralateral hind paw did not significantly differ between CCI and sham animals (Fig. 1a, b). To determine whether the spinal NLRP3 inflammasome-related proteins were involved in the development of neuropathic pain, the protein level of spinal, NLRP3, caspase-1, IL-1β and TXNIP (a mediator of NLRP3 inflammasome activation) at different dpi’s were measured (Fig. 1c). The expression of TXNIP and NLRP3 in the lumbar spinal cord was significantly increased at the 14th and 21st dpi. The level of cleaved caspase-1 and IL-1β were observed to be upregulated at 14th, 21st and 28th dpi. The results suggested that TXNIP and NLRP3 inflammasome related-proteins may contribute to the maintenance of CCI-induced pain behaviors.
Expression of TXNIP/NLRP3 axis in ipsilateral spinal cord dorsal horn of CCI model mice. a, b Chronic constriction injury induced mechanical allodynia and thermal hyperalgesia in mice. von Frey (a) and Hargreaves (b) tests showed mechanical withdrawal threshold and thermal withdrawal latency for sham and CCI groups. Data are presented as mean ± SEM (n = 8 mice in each group). ***p < 0.001, compared with the sham group (two-way ANOVA, followed by Tukey's multiple comparisons test). c The representative images of western blot for the expression of TXNIP/NLRP3 axis in ipsilateral spinal cord of CCI model mice in different time points. Data are expressed as means ± SEM (n = 3–5 mice in each group). *p < 0.05, **p < 0.01, and ***p < 0.001, compared with day 0 (one-way ANOVA, followed by Tukey's multiple comparisons test)
The Cellular Localization of TXNIP and NLRP3 Inflammasome Related-Proteins in the Spinal Dorsal Horn
The co-localization of TXNIP, NLRP3, caspase-1, and IL-1β were examined with a marker of the neuron (NeuN) (Fig. 2), astrocyte (GFAP) (Fig. 3), and microglia (Iba1) (Fig. 4) in the ipsilateral spinal cord of the CCI model at 21 days. This was done to investigate the TXNIP/NLRP3 axis expression level in different cell types in the spinal dorsal horn after CCI-injury. Consistent with the previous reports, in the spinal dorsal horn of sham animals, a small number of neurons and microglia expressed TXNIP and NLRP3 inflammation-related proteins, while few astrocytes expressed TXNIP and NLRP3 inflammation-related proteins. At 21 days post nerve injury, the co-localization of TXNIP, NLRP3, caspase-1, and IL-1β with NeuN and Iba1 but not GFAP increased. These results suggested that the neurons and microglia in the spinal dorsal horn were the primary cellular source of IL-1β induced by NLRP3 inflammasome activation.
Cellular localization of TXNIP (a), NLRP3 (b), caspase-1 (c) and IL-1β (d) with NeuN (a neuronal marker) in ipsilateral spinal cord dorsal horn of the sham and CCI model mice of day 21 (scale bar = 50 μm). e Schematic diagram of the captured image area. f Data are presented as mean ± SEM (n = 3 mice in each group). *p < 0.05, **p < 0.01, compared with the sham group (t-test)
Cellular localization of TXNIP (a), NLRP3 (b), caspase-1 (c) and IL-1β (d) with Iba1 (a microglial marker) in ipsilateral spinal cord dorsal horn of the sham and CCI model mice of day 21 (scale bar = 50 μm). e Data are presented as mean ± SEM (n = 3 mice in each group). *p < 0.05, **p < 0.01, compared with the sham group (t-test)
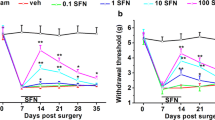
SAL Alleviated Mechanical Allodynia and Thermal Hyperalgesia in the CCI Model
CCI mice were daily intraperitoneal injected with SAL from the 7th to the 21st day after injure. During this period, behavioral tests were performed every other day 1 h after treatment to determine the analgesic effect of SAL (Fig. 5). Compared to the vehicle and SAL at 100 mg/kg groups, SAL at 200 mg/kg group significantly relieved the mechanical allodynia on the 8th day of treatment, and thermal hyperalgesia on the 4th day of treatment. Compared with the sham group, SAL (200 mg/kg) treatment has no effect on the mechanical allodynia and thermal hyperalgesia of the sham + SAL (200 mg/kg) group mice.
SAL attenuated thermal and mechanical allodynia of CCI model mice. Mice were injected with SAL or vehicle for 14 consecutive days, and mechanical withdrawal threshold (a) and thermal withdrawal latency (b) were measured 1 h after injection. Data are presented as mean ± SEM (n = 8 mice in each group). *p < 0.05, **p < 0.01, and ***p < 0.001, compared with the CCI + vehicle group (two-way ANOVA, followed by Tukey's multiple comparisons test)
SAL Suppressed the Activation of Spinal TXNIP and NLRP3 Inflammasome
SAL’s inhibitory effect was examined on the activation of spinal TXNIP and NLRP3 inflammasome-related proteins to confirm further the mechanism underlying SAL’s analgesic effect. Consistent with the results presented above, the protein level of TXNIP, NLRP3, caspase-1, and IL-1β were significantly upregulated in the ipsilateral spinal cord on the 21st day in the CCI plus vehicle group, compared to the expression in sham and sham plus 200 mg/kg SAL group (Fig. 6a). Although 100 mg/kg SAL treatment did not reverse the upregulation, repeated treatment for 14 days with 200 mg/kg SAL significantly inhibited the activation of TXNIP and NLRP3 inflammasome-related proteins. Since neuronal loss in spinal dorsal horn contributes to the maintenance of neuropathic pain, we examined whether SAL alleviated neuronal death in the CCI model (Fig. 6b). As per the CV staining results, the number of neurons in the ipsilateral spinal dorsal horn was decreased on the 21st day in the CCI model. The Fluoro-Jade C (FJC) staining also indicated that the number of degenerative neurons increased on the 21st day in the CCI model. SAL’s 2-week treatment reversed the loss of neurons in the spinal dorsal horn and produced a neuroprotective effect in the CCI model.
SAL protected ipsilateral spinal cord neuron via inhibiting the TXNIP/NLRP3 axis in CCI model mice. a The representative images of western blot showed the expression of TXNIP/NLRP3 axis in ipsilateral spinal cord of mice in each group. Data are expressed as means ± SEM (n = 3–7 mice in each group). *p < 0.05, **p < 0.01, and ***p < 0.001, compared with the CCI + vehicle group (one-way ANOVA, followed by Dunnett's multiple comparisons test). b Effects of SAL on the ipsilateral spinal cord neurons after administration for 14 days. CV and FJC staining in the ipsilateral spinal cord for each group. Data are presented as mean ± SEM (n = 5 mice in each group). *p < 0.05, **p < 0.01, and ***p < 0.001, compared with the CCI + vehicle group (two-way ANOVA, followed by Tukey's multiple comparisons test). Scale bars = 50 µm
Discussion
This article illustrates the time course of upregulated TXNIP and NLRP3 inflammasome-related proteins in the spinal cord of CCI model. The upregulation of TXNIP, NLRP3, caspase-1, and IL-1β were mainly expressed in neurons and microglial of the spinal dorsal horn. Moreover, the study demonstrated that SAL ameliorated neuropathic pain by blocking TXNIP and NLRP3 inflammasome activation. SAL also exhibited a neuroprotective effect in the CCI model.
Rhodiola rosea L. belongs to the Crassulaceae family and has been used as a botanical medicine for a long time. It possesses a wide range of pharmacological effects, including cardioprotective, vasculoprotective, and hepatoprotective effects. Recently, an increasing number of studies have been conducted to illuminate the neuroprotective effects of SAL on multiple diseases, such as degenerative diseases, brain injury, and dysfunction of the central nervous system [33]. Although some evidence indicates that SAL may act as a pain killer, no study on SAL’s direct analgesic mechanism has been reported in neuropathic pain induced by peripheral nerve injury. One research suggests that SAL alleviates mechanical and heat hypersensitivity in diabetic neuropathic pain by inhibiting the neuroinflammation. The present study observed that SAL treatment at a 200 mg/kg dose for 14 consecutive days ameliorated the mechanical allodynia and thermal hyperalgesia in the CCI model. The analgesic effect was evident on the 4th day of the treatment and increased gradually till the 14th day. To the author’s best knowledge, this finding provided direct evidence for the first time that SAL ameliorated pain hypersensitivity induced by peripheral nerve injury. Compared with the lower dosage (25 and 50 mg/kg) of SAL and a more prolonged treatment period (at least five consecutive weeks treatment) required to exhibit analgesia in diabetic neuropathic pain, it was found that a higher dose of SAL (200 mg/kg) could suppress pain behaviors with a much shorter latency (1–2 weeks).
The NLRP3 inflammasome has been widely implicated as a regulator of caspase-1 and IL-1β activation. Excessive caspase-1 and IL-1β activity, which leads to prolonged or chronic inflammation, may also promote neurological disorders, including neurodegenerative diseases. A previous study found that 7 days after spared nerve injury, Caspase-1 and IL-1β were released in the prelimbic and infralimbic (PL-IL) cortex of mice [34]. Mechanical allodynia was reduced in mice after the PL-IL cortex was injected with pan-caspase inhibitor [34]. Several pieces of evidence indicates that NLRP3 inflammasome and its mediator TXNIP are activated during peripheral nerve injury. The inhibition of the NLRP3 inflammasome is a potential treatment strategy for neuropathic pain [3]. Little is known about the temporal profiles of spinal TXNIP and NLRP3 inflammasome activation after peripheral nerve injury. Here the authors showed that spinal TXNIP and NLRP3 were significantly activated on the 14th and 21st day but returned to baseline on the 28th day post-CCI surgery. The activation of caspase-1 and IL-1β was evident from the 14th and 21st to the 28th day. The PWT to mechanical and PWL to thermal stimuli decreased significantly from the 7th day to the 28th day post-CCI surgery. The results suggested that spinal TXNIP and NLRP3 inflammasome contributed to the maintenance phase of pain hypersensitivity in the CCI model.
The existing literature on the cellular distribution of NLRP3 in the spinal cord is conflicting. In one study [35], double immunofluorescence staining showed that NLRP3 was expressed only in microglia and not in the neurons or astrocytes of the spinal cord of a rat model of neuropathic pain. Another study reported that NLRP3 was primarily expressed in neurons and microglia in a rat’s spinal cord, and only a few astrocytes were found to express NLRP3 [36]. Thus, whether the NLRP3 inflammasome is localized in spinal neurons and the mechanism of change of the expression level in neuropathic pain need to be addressed. In sham animals, the results of double immunofluorescence staining indicated that NLRP3 was predominantly expressed in neurons and microglial cells within the spinal dorsal horn, and few astrocytes were found to express NLRP3.
Moreover, TXNIP, caspase-1, and IL-1β are also mainly localized in the spinal neurons and microglial cells but not in astrocytes. On the 21st day, the upregulation of TXNIP/NLRP3 inflammasome axis-related proteins was also seen in spinal neurons and microglial cells in the CCI model. These results suggested that peripheral nerve injury led to the activation of TXNIP, which consequently activated the NLRP3 inflammasome-related proteins in neurons and microglial cells in the spinal dorsal horn.
SAL has been suggested to attenuate high-fat diet-induced nonalcoholic fatty liver disease via AMPK-dependent TXNIP/NLRP3 pathway in previous reports [37]. The oral administration of SAL at 100 mg/kg for 8 weeks could reverse the increase in cleaved caspase-1 and IL-1β in HFD and db/db mice, and the expression level of pro-IL-1β also was reduced in db/db mice after treatment. However, it is still unknown whether SAL can regulate the activation of the NLRP3 pathway in the nervous system. The present study found that i.p. injection of SAL at 200 mg/kg for 2 weeks inhibited the activation of spinal TXNIP and NLRP3 inflammasome and their related proteins, caspase-1 and IL-1β. FJC staining showed that the increase in degenerative spinal neurons was reversed by SAL treatment. To the best knowledge of the authors, this is the first study to demonstrate the inhibitory effect of SAL on the TXNIP/NLRP3 pathway in the central nervous system, which suggests the potential neuroprotective application of SAL in the central nervous system diseases induced by the NLRP3 inflammasome.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
References
Campbell JN, Meyer RA (2006) Mechanisms of neuropathic pain. Neuron 52(1):77–92
Ji RR, Chamessian A, Zhang YQ (2016) Pain regulation by non-neuronal cells and inflammation. Science 354(6312):572–577
Starobova H, Nadar EI, Vetter I (2020) The NLRP3 inflammasome: role and therapeutic potential in pain treatment. Front Physiol 11:1016
Lamkanfi M, Dixit VM (2014) Mechanisms and functions of inflammasomes. Cell 157(5):1013–1022
Nakahira K et al (2011) Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol 12(3):222–230
Zhou R et al (2010) Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat Immunol 11(2):136–140
Choe JY, Kim SK (2017) Quercetin and ascorbic acid suppress fructose-induced NLRP3 inflammasome activation by blocking intracellular shuttling of TXNIP in human macrophage cell lines. Inflammation 40(3):980–994
Butler DSC et al (2018) Neuroepithelial control of mucosal inflammation in acute cystitis. Sci Rep 8(1):11015
Chen SP et al (2019) Pharmacological inhibition of the NLRP3 in flammasome as a potential target for cancer-induced bone pain. Pharmacol Res 147:104339
Son S et al (2019) Chemotherapeutic agent paclitaxel mediates priming of NLRP3 inflammasome activation. Front Immunol 10:1108
Deuis JR et al (2017) Role of the NLRP3 inflammasome in a model of acute burn-induced pain. Burns 43(2):304–309
Cowie AM et al (2019) NOD-like receptor protein 3 inflammasome drives postoperative mechanical pain in a sex-dependent manner. Pain 160(8):1794–1816
He W et al (2019) Microglial NLRP3 inflammasome activation mediates IL-1beta release and contributes to central sensitization in a recurrent nitroglycerin-induced migraine model. J Neuroinflammation 16(1):78
Khan N et al (2018) Pharmacological inhibition of the NLRP3 inflammasome as a potential target for multiple sclerosis induced central neuropathic pain. Inflammopharmacology 26(1):77–86
Pan Z et al (2018) miRNA-23a/CXCR4 regulates neuropathic pain via directly targeting TXNIP/NLRP3 inflammasome axis. J Neuroinflammation 15(1):29
Tonkin RS et al (2018) Attenuation of mechanical pain hypersensitivity by treatment with Peptide5, a connexin-43 mimetic peptide, involves inhibition of NLRP3 inflammasome in nerve-injured mice. Exp Neurol 300:1–12
Sagulenko V et al (2013) AIM2 and NLRP3 inflammasomes activate both apoptotic and pyroptotic death pathways via ASC. Cell Death Differ 20(9):1149–1160
Liao ZL et al (2019) Salidroside protects PC-12 cells against amyloid beta-induced apoptosis by activation of the ERK1/2 and AKT signaling pathways. Int J Mol Med 43(4):1769–1777
Wang H et al (2020) Neuroprotective effects of salidroside in a mouse model of Alzheimer’s disease. Cell Mol Neurobiol 40(7):1133–1142
Zhang X et al (2020) Salidroside ameliorates Parkinson’s disease by inhibiting NLRP3-dependent pyroptosis. Aging (Albany NY) 12(10):9405–9426
Li R, Chen J (2019) Salidroside protects dopaminergic neurons by enhancing PINK1/Parkin-mediated mitophagy. Oxid Med Cell Longev 2019:9341018
Zhong ZF et al (2019) Neuroprotective effects of salidroside on cerebral ischemia/reperfusion-induced behavioral impairment involves the dopaminergic system. Front Pharmacol 10:1433
Li S et al (2020) Fibroblast growth factor 2 contributes to the effect of salidroside on dendritic and synaptic plasticity after cerebral ischemia/reperfusion injury. Aging (Albany NY) 12(11):10951–10968
Kallscheuer N et al (2019) Identification and microbial production of the raspberry phenol salidroside that is active against Huntington’s disease. Plant Physiol 179(3):969–985
Vasileva LV et al (2018) Antidepressant-like effect of salidroside and curcumin on the immunoreactivity of rats subjected to a chronic mild stress model. Food Chem Toxicol 121:604–611
Ni GL et al (2017) Salidroside ameliorates diabetic neuropathic pain in rats by inhibiting neuroinflammation. J Mol Neurosci 63(1):9–16
Bennett GJ, Xie YK (1988) A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 33(1):87–107
Fischer R et al (2019) TNFR2 promotes Treg-mediated recovery from neuropathic pain across sexes. Proc Natl Acad Sci USA 116(34):17045–17050
Chaplan SR et al (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53(1):55–63
Hargreaves K et al (1988) A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 32(1):77–88
Türeyen K et al (2004) Infarct volume quantification in mouse focal cerebral ischemia: a comparison of triphenyltetrazolium chloride and cresyl violet staining techniques. J Neurosci Methods 139(2):203–207
Ikenari T et al (2020) Evaluation of fluoro-jade C staining: specificity and application to damaged immature neuronal cells in the normal and injured mouse brain. Neuroscience 425:146–156
Zhong Z et al (2018) Pharmacological activities, mechanisms of action, and safety of salidroside in the central nervous system. Drug Des Dev Ther 12:1479–1489
Giordano C et al (2012) TRPV1-dependent and -independent alterations in the limbic cortex of neuropathic mice: impact on glial caspases and pain perception. Cereb Cortex 22(11):2495–2518
Grace PM et al (2016) Morphine paradoxically prolongs neuropathic pain in rats by amplifying spinal NLRP3 inflammasome activation. Proc Natl Acad Sci USA 113(24):E3441–E3450
Zendedel A et al (2016) Activation and regulation of NLRP3 inflammasome by intrathecal application of SDF-1a in a spinal cord injury model. Mol Neurobiol 53(5):3063–3075
Zheng T et al (2018) Salidroside attenuates high-fat diet-induced nonalcoholic fatty liver disease via AMPK-dependent TXNIP/NLRP3 pathway. Oxid Med Cell Longev 2018:8597897
Funding
This work was supported by National Natural Science Foundation of China (Grant No. 81971037 to F. Yang) the Beijing Natural Science Foundation Program and Scientific Research Key Program of Beijing Municipal Commission of Education (KZ201910025026 to F. Yang) and Support Project of High-level Teachers in Beijing Municipal Universities in the Period of 13th Five–year Plan CIT&TCD201904092 (QL).
Author information
Authors and Affiliations
Contributions
FY and TH designed the overall approach, coordinated the study, and drafted the manuscript. TH, QL, and FY prepared the manuscript. TH did most of the behavioral, Western blot and immunostaining studies and statistical analysis of the data. QS, YG, YZ, YD, YM, JL, WC and TL contributed to the design of the different experiments and executed a number of them. PW provided critical analysis of the experiments and the results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Approval
The animal study was reviewed and approved by the Capital Medical University Animal Care and Use Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, T., Sun, Q., Gou, Y. et al. Salidroside Alleviates Chronic Constriction Injury-Induced Neuropathic Pain and Inhibits of TXNIP/NLRP3 Pathway. Neurochem Res 47, 493–502 (2022). https://doi.org/10.1007/s11064-021-03459-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-021-03459-y