Abstract
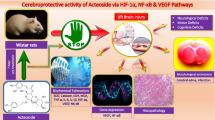
Intracerebral hemorrhage (ICH) is a devastating cerebrovascular disease with a high mortality rate affecting individuals worldwide. After ICH, persistent inflammation results in the death of brain cells, as well as the promotion of secondary brain injury. Verbascoside (VB), an active component in herbal medicine, possesses antioxidant, anti-inflammatory and neuroprotective properties. Furthermore, previous studies have shown that VB improves recovery of neuronal function after spinal cord injury in rats. In this study, we investigated whether VB limited inflammation induced by ICH through the targeting of NLRP3, which is associated with acute inflammation and apoptosis. Administration of VB reduced neurological impairment and pathological abnormalities associated with ICH, while increasing cell viability of neurons. This was achieved through NLRP3 inhibition and microglial activation. VB treatment decreased neuronal damage when co-cultured with microglia. Furthermore, knockout of NLRP3 eliminated the ability of VB to inhibit inflammation, cell death or protect neurons. Taken together, VB suppressed the inflammatory response following ICH by inhibiting NLRP3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous or mechanical damage to the brain can cause intracerebral hemorrhage (ICH) that account for 10–15% of all strokes [1]. An ICH can be devastating, resulting in hemiparesis or hemiplegia. Moreover, it is associated with high morbidity and mortality if not properly treated [2]. The complicated pathophysiological processes involved in ICH are associated with primary and secondary brain injuries [3,4,5]. A primary injury is characterized by physical compression, hematoma volume and disruption of brain tissues [6]. A secondary injury is triggered by hematoma toxicity, acute inflammation and oxidative stress. This leads to microglial activation, mitochondrial dysfunction and neuroinflammation [7,8,9,10]. The potential outcomes of these injuries are loss of brain cells through apoptosis or autophagy as well as death. It has been indicated that neuroprotective agents may be promising therapeutics to alleviate the damage caused by secondary brain injuries and improve brain function recovery [11,12,13].
The nucleotide-binding oligomerization domain (NOD)-like receptor (NLR) pyrin domain-containing protein 3 (NLRP3) is a member of the NLR family and is involved in activating the inflammasome [14]. It has been reported that NLRP3 is an essential mediator of the inflammatory response following ICH [15]. Upon activation of the inflammasome, NLRP3 recruits the adaptor protein apoptosis-associated speck-like (ASC) and pro-caspase-1. Active caspase-1 then promotes the maturation of interleukin pro-inflammatory cytokines (e.g. interleukin IL-1β), induced neuroinflammation and apoptosis [16]. The glycosylated phenylpropanoid verbascoside (VB) isolated from the medicinal plant Syringa vulgaris (Oleaceae), exhibits a wide range of biological activities. In neuroprotection studies, VB showed anti-inflammatory and neuroprotective effects in a rodent model of ICH and cerebral ischemia. Previous studies have also demonstrated that VB reduces brain edema, blood–brain barrier disruption, inflammatory injury to the brain and neuronal apoptosis [17]. However, the mechanisms underlying the anti-inflammatory effects of VB are unclear. In this study, we aimed to investigate whether VB can suppress neuroinflammation and neuronal apoptosis after ICH through the inhibition of NLRP3 in a mouse model.
Materials and Methods
Chemicals, Reagents and Antibodies
VB (Shilan biology, Tianjin, China) was resuspended in PBS and stored in a 4 °C refrigerator. Dulbecco’s modified Eagle medium (DMEM), fetal bovine serum (FBS), B27 and glutamine were purchased from Gibco (Grand Island, USA). Antibodies recognizing NLRP3, NF-κB, TNFα, IL-1β and GAPDH were purchased from Cell Signaling Technology (Beverly, MA).
ICH Mouse Model
Male C57BL/6 and C57BL/6-NLRP3−/− mice (Nanjing Model Organism; between 8 and 10 weeks of age and weighing 22–25 g) were housed at 23–25 °C with a 12/12 h light–dark cycle along with food and water ad libitum. Studies performed on mice were authorized by the Animal Ethics Committee of the Southwest Medical University.
Mice were anesthetized with 1% pentobarbital sodium (50 mg/kg) using an intraperitoneal injection [18]. After fixing the mice to a stereotaxic frame, bacterial collagenase VII (0.1 U in 0.4 μL; Sigma) was injected into the right striatum (stereotaxic coordinates: 0.2 mm posterior, 2.8 mm ventral, and 2.2 mm lateral to the bregma) at a rate of 400 nL/min for 1 min using an infusion pump. The needle was held in place for 10 min after injection [19]. The craniotomy was sealed with bone wax and the scalp was closed using sutures. Body temperature was maintained at 37 °C throughout the procedure and mice were given free access to food and water after the operation. Animals were randomized to sham, ICH + Vehicle, ICH + VB (30 mg/kg) and ICH + VB (60 mg/kg) groups. After ICH induction for 1 h, 30 or 60 mg/kg of VB or regular saline were administrated to mice intraperitoneally.
Neurological Scoring
To test neurological function in ICH mice, the Modified Garcia Score was used [20] for three consecutive days. Modified Garcia is composed of the following: (1) spontaneous activity, (2) symmetry in the movement of four limbs, (3) forepaw outstretching, (4) climbing, (5) body proprioception or (6) response to vibrissae touch. The score assigned to each mouse after evaluation includes the sum of all six individual test scores. The minimum neurological score was 3 and the maximum was 18.
Assessment of Lesion Volume
Lesion volume was calculated using Image Pro-Plus software (Media Cybernetics). Brains were collected 72 h after ICH. Following perfusion of PBS containing 4% paraformaldehyde, serial 1 mm thick slices of mouse brains were prepared. Digital photography of the serial slices was performed and lesion volume was measured using an image analysis program (Image Pro-Plus; Media Cybernetics). Total lesion volume (mm3) was calculated by summing the blood clot area in each section by the distance between sections.
Assessment of Brain Edema
Brain edema was examined using the wet/dry method performed 3 days after ICH. Mouse brains from each group were quickly removed from the skull and weighed to obtain the wet weight. Subsequently, brains were dried in an oven at 160 °C for 24 h to obtain the dry weight. Water content was calculated as follows: (wet weight − dry weight)/(wet weight) × 100% [11].
Reverse Transcription-Quantitative PCR (RT-qPCR)
Cellular RNA was isolated using Trizol (Invitrogen; Thermo Fisher Scientific, Inc.) [21]. Next, mRNAs were converted into cDNAs using a PrimeScript RT Reagent kit. The StepOne Plus device (Applied Biosystems) was used to perform RT-PCR using the following conditions: denaturation at 95 °C for 10 s followed by 40 cycles of 95 °C for 5 s and 60 °C for 20 s using specific primers: PCR was performed using Taq DNA polymerase (Takara, China) and the following primers:
-
TLR4: 5′-CCATCGGTTGATCTTGGGAGAA-3′ (forward) and 5′-TGCCAGAGACATTGCAGA AACA-3′ (reverse)
-
NF-κB: 5′-CCTTGAAGGGATTTCCCTCC′ (forward) and 5′-GGAACTTCCCTAAAGGGAGG-3′ (reverse)
-
TNFα: 5′-CAGGCGGTGCCTATGTCTC-3′ (forward) and 5′-CGATCACCCCGAAGTTCAGTAG-3′ (reverse)
-
IL-1β: 5′-ATG GCA ACT GTT CCT GAA CTC AAC T-3′ (forward) and 5′-CAGGACAGGTATAGA TTCTTTCCTTT-3′ (reverse)
-
GAPDH: 5′-AGGTCGGTGTGAACGGATTTG-3′ (forward) and 5′-GGGGTCGTTGATGGCAACA-3′ (reverse)
Immunoblotting
Cells lysates or tissues extracted from the ICH lesion (including the area 1 mm surrounding the ICH lesion) were lysed in 1× RIPA lysis buffer (CWBIO, China). All protein samples were separated by electrophoresis on 10% gradient SDS–PAGE gels and were transferred to PVDF membranes. Membranes were then blocked in 1× TBST containing 5% BSA for 1 h at RT, then incubated overnight at 4 °C with primary antibodies diluted in 5% BSA (1× TBST). After, membranes were incubated with peroxidase-conjugated secondary antibody diluted in 1× TBST solution. The ECL chemiluminescence was used to detect protein bands on membranes (Merck Millipore, German ECL kit).
Immunofluorescence
Immunofluorescence was detected using the primary antibodies Iba-1 and NeuN (Cell Signaling Technology, Beverly, MA) as previously described [13]. Mice were perfused with saline, followed by 4% paraformaldehyde under deep anesthesia (100 mg/kg sodium pentobarbital) and brains were sectioned at 20 μm thickness using a cryostat. Sections were blocked in 5% normal donkey serum diluted in PBS for 1 h at room temperature and then incubated overnight at 4 °C with mouse anti-Iba1 primary antibodies, followed by being washed three times with PBS. Neurons were fixed with 4% paraformaldehyde and blocked in 5% normal donkey serum diluted in PBS for 1 h at room temperature. Neurons were then incubated overnight at 4 °C with mouse anti-NeuN primary antibodies before being washed three times with PBS. Donkey anti-mouse Alexa-Fluor 555 was used as a secondary antibody. Nuclei were counterstained using DAPI for 10 min before imaging. Images were obtained by confocal microscopy.
TUNEL Staining
To visualize DNA fragmentation as an apoptosis marker, TUNEL staining was performed using an In Situ Cell Death Detection kit (Roche, Mannheim, Germany). Sections were incubated in permeabilization solution containing 0.1% sodium citrate and 0.1% Triton X-100 at 4 °C for 2 min, followed by an incubation with TdT enzyme in reaction buffer containing TMRred labeled dUTP at 37 °C for 1 h. Finally, sections were rinsed and visualized using a converter-POD with 0.03% 3,3′-diaminobenzidine (DAB).
Primary Neuron Cultures
Primary mouse brain cells were isolated from embryonic C57BL/6 mice aged 12–16 days. Briefly, cortical-striatal tissue was minced in cold HBSS with 20% FBS before resuspending in trypsin containing 100 U/mL DNAse I (Gibco, USA). Neuronal cells were seeded into poly-d-lysine-coated flasks supplemented with 2% B27 and 1% glutamine. Neurons were cultured at 37 °C under 5% CO2 for 3 days and harvested 14 days after seeding.
Transwell Co-cultures
Primary neurons and microglial cells were co-cultured using transwell inserts. Briefly, 2 × 104 BV2 microglial cells were seeded into the upper chamber and 1 × 104 neurons were seeded in the lower chamber. Both were cultured in Neurobasal Medium (Gibco, USA) supplemented with 2% B27 and 1% glutamine.
Statistical Analyses
Data are presented as mean ± SD. One-way ANOVA was used to compare multiple groups followed by LSD or Dunnett’s post hoc test. SPSS 20.0 was used for statistical analyses and a p < 0.05 was considered as statistically significant.
Results
VB Decreases the Neurological and Pathological Deficits Causes by ICH
Before exploring whether VB inhibited inflammation associated with ICH, we first investigated changes in neurobehavioral function following ICH. ICH mice were treated with different doses of VB and their neurological deficits were assessed. No significant differences were observed when comparing the ICH + vehicle group to ICH mice treated with a VB dose less than 30 mg/kg. However, when the VB dose was greater than 60 mg/kg (for example, 120 mg/kg), there was no additional benefit compared to ICH mice administered 60 mg/kg. In summary, 30 and 60 mg/kg VB doses were chosen to perform subsequent experiments. A VB does of 60 mg/kg was found to be the optimal dose achieving maximum protective effects. Moreover, nerve function deficits in injured mice were significantly reduced when treated with VB in a dose- and time-dependent manner; which was evaluated using the Garcia scoring method (Fig. 1a).
VB reduced neurological and pathological deficits induced by ICH. (a) Garcia test scores of different groups at the indicated time points after ICH or sham-operation. (b) Representative images of brain sections showing lesion areas and quantification of lesion volumes 72 h post ICH. (c) Brain water content of ipsilateral hemorrhagic hemispheres in the different groups. (d) Percentage of apoptotic cells after 72 h (bar = 50 μm). *p < 0.05, ***p < 0.001, compared to sham group; #p < 0.05, compared to ICH + vehicle group
Similarly, VB significantly decreased intracerebral lesion volume post-ICH in a dose dependent manner compared to the ICH group (Fig. 1b). Compared to mice in the sham group, the brain water content was dramatically elevated post-ICH, which was reversed by VB in a dose-dependent manner (Fig. 1c). As expected, VB limited the degree of apoptosis within hemorrhagic lesions and in the periphery after ICH (Fig. 1d). These results revealed that VB exhibited neuroprotective effects following ICH induced-pathological and neurological impairment.
VB Inhibited the Expression Levels of NLRP3 and Inflammatory Mediators While Inhibiting Microglial Activation
Expression levels of NLRP3, NF-κB, TNF-α and IL-1β were analyzed in hemorrhagic lesions. All these markers are involved in inflammatory damage of the brain and are upregulated after ICH. VB was shown to reverse the increased mRNA and protein levels of NLRP3, NF-κB, TNF-α and IL-1β in a dose-dependent manner in ICH mice (Fig. 2a, b). We hypothesized that microglia, as the primary immune effector cells in the brain, may be activated to induce inflammatory damage following ICH [22]. As expected, VB inhibited the activation of microglial cells following ICH in a dose-dependent manner (Fig. 2c). These findings suggested that VB may suppress ICH-induced inflammation by targeting the NLRP3 pathway. To validate this hypothesis, microglial cells were activated using murine red blood cell (RBC) lysates to induce acute inflammation. Expression levels of NLRP3, NF-κB, TNF-α, and IL-1β were reduced by VB treatment in a dose-dependent manner (Fig. 3a, b). In Transwell co-culture experiments, VB significantly inhibited cell death following stimulation with RBC lysates (Fig. 3c). Altogether, we concluded that VB protected neurons from inflammatory damage, potentially by inhibiting both NLRP3-mediated inflammatory effects and microglial activation.
VB attenuated NLRP3 signaling and microglial activation in peri-hemorrhagic areas. (a) RT-PCR and (b) immunoblots showing mRNA and protein levels of NLRP3 and downstream effectors 72 h after ICH induction. (c) Representative images showing Iba-1+ active microglial cells in the lesions and quantifications after 72 h (scale bar = 50 μm). *p < 0.05, compared to sham group; #p < 0.05, compared to ICH + vehicle group
VB reduced microglial activation and neuronal damage induced by RBC lysis in vitro. (a) RT-PCR and (b) immunoblots showing mRNA and protein levels of NLRP3 and downstream effectors in primary microglial cells co-cultured with primary neurons in the presence of RBC lysates and VB. (c) Representative images of NeuN+ (red) primary neurons co-cultured and treated as described (scale bar = 50 μm) and viability levels. *p < 0.05, compared to sham group; #p < 0.05, compared to ICH + vehicle group
NLRP3-Deficiency Abolishes the Neuroprotective Function of VB
To confirm that VB targets NLRP3, the ICH model was used in NLRP3−/− mice. Few differences were observed in NLRP3−/− mice compared to wild type mice following ICH, as indicated by nerve function deficits, brain water content and number of apoptotic neurons (Fig. 4a–c). Moreover, VB exhibited anti-inflammatory effects in neurons isolated from NLRP3−/− mice (Fig. 4d). Altogether, VB did not enforce anti-inflammatory effects in the absence of NLRP3 and thus may impact the NLRP3 pathway to limit inflammation.
VB failed to protect against ICH in NLRP3-deficient mice. Effects of VB treatment on the (a) neurological deficit score, (b) brain water content and (c) percentage of apoptotic cells in WT and NLRP3−/− mice treated as described 72 h after ICH (scale bar = 100 μm). (d) Representative images of NeuN+ (red) primary neurons from WT and NLRP3−/− mice co-cultured and treated as described (scale bar = 50 μm) and viability levels. ***p < 0.001, compared to ICH + WT group
Discussion
ICH is a destructive stroke subtype linked to high disability and recurrence rates due to damage induced by primary and secondary brain injuries [23]. Inflammation plays a critical role in secondary brain damage following ICH, however, the mechanisms underlying inflammatory injury following ICH are still unclear. Therefore, there is increasing interest in investigating secondary brain injuries and exploring the potential therapeutic benefits of limiting inflammation [24]. In this study, we explored the effects of VB on the NLRP3 signaling pathway in ICH-induced secondary inflammatory damage.
Inflammation causes damage to the cerebral tissue following ICH. It induces and amplifies mitochondrial damage, cytokine release and neuronal dysfunction; leading to neuronal apoptosis and abnormal sensorimotor function [25,26,27]. It has been reported that VB is involved in multiple biological activities and contains anti-inflammatory, antioxidant, anti-microbial and neuroprotective properties [17, 28, 29]. In this study, neurological deficit scores were reduced to minimum levels, indicating that we generated an ideal ICH model for subsequent experiments. Mice displayed characteristics of ICH including increased ICH volume, increased brain water content and enhanced neuronal apoptosis. As expected, VB significantly prevented brain injuries induced by ICH in a dose-dependent manner.
Previous studies have shown that NLRP3 inflammasome activation is involved in the secretion of cytokines and in microglial activation, both of which are crucial contributors to inflammatory damage related to ICH [30, 31]. Indeed, the mRNA and protein expression levels of NLRP3 were noticeably increased in this ICH model. This was accompanied by increased NF-κB, TNF-α and IL-1β expression levels. Expression of these mediators was significantly reduced when treated with VB. Moreover, microglial activation following ICH was markedly inhibited with VB treatment, which we hypothesized may be mediated by NLRP3. We further explored the involvement of NLRP3 in the anti-inflammatory functions of VB following ICH. We found that VB inhibited expression of NLRP3 and prevented pro-inflammatory cytokine release promoted by RBC lysates. Moreover, VB decreased neuronal death caused by the infiltration of microglia following induction of RBC lysate-mediated inflammation. These results indicated that the anti-inflammatory effects of VB in the ICH model may be mediated by the NLRP3 signaling pathway. Consistent with our observations, VB was no longer able to exert its protective effects in mice lacking NLRP3, which suggested that VB promoted neuroprotective effects against ICH through NLRP3 inhibition.
Despite these findings, several limitations were faced in this study. For example, RBC lysates contained multiple elements inducing an inflammatory response, such as heme, hemoglobin, iron and ions. Therefore, we will explore detailed effects of each RBC lysate element in the inflammatory response. In addition, activation and regulation of the NLRP3 inflammasome pathway is complex and the effects of VB on inflammasome activity should be further investigated.
In summary, administration of VB may have therapeutic potential to protect brain tissue from secondary damage caused by acute ICH. Moreover, we highlighted that the protective effects of VB were partially due to the inhibition of NLRP3-mediated inflammation and microglial activation. In the future, clinical studies should be conducted to explore the potential of VB as a novel therapeutic to limit inflammation and secondary damage in ICH patients.
References
Wang M, Cheng L, Chen ZL, Mungur R, Xu SH, Wu J, Liu XL, Wan S (2019) Hyperbaric oxygen preconditioning attenuates brain injury after intracerebral hemorrhage by regulating microglia polarization in rats. CNS Neurosci Ther 25:1126–1133
An SJ, Kim TJ, Yoon BW (2017) Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke 19:3–10
Xi G, Keep RF, Hoff JT (2006) Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 5:53–63
Wang J (2010) Preclinical and clinical research on inflammation after intracerebral hemorrhage. Prog Neurogibol 92:463–477
Wang J, Dore S (2007) Inflammation after intracerebral hemorrhage. J Cereb Blood Flow Metab 27:894–908
Haque ME, Gabr RE, George SD, Zhao X, Boren SB, Zhang X, Ting SM, Sun G, Hasan KM, Savitz S, Aronowski J (2019) Serial metabolic evaluation of perihematomal tissues in the intracerebral hemorrhage pig model. Front Neurosci 13:888–889
Bobinger T, Burkardt P, Huttner HB, Manaenko A (2018) Programmed cell death after intracerebral hemorrhage. Curr Neuropharmacol 16:1267–1281
Rodríguez C, Sobrino T, Agulla J, Bobo-Jiménez V, Ramos-Araque ME, Duarte JJ, Gómez-Sánchez JC, Bolaños JP, Castillo J, Almeida Á (2017) Neovascularization and functional recovery after intracerebral hemorrhage is conditioned by the Tp53 Arg72Pro single-nucleotide polymorphism. Cell Death Differ 24:144–154
Salman RAS, Law ZK, Bath PM, Steiner T, Sprigg N (2018) Haemostatic therapies for acute spontaneous intracerebral haemorrhage. Cochrane Database Syst Rev 4:D5951
Wen J, Yang CY, Lu J, Wang XY (2018) Ptprj-as1 mediates inflammatory injury after intracerebral hemorrhage by activating NF-κB pathway. Eur Rev Med Pharmacol 22:2817–2823
Zhang Y, Yi B, Ma J, Zhang L, Zhang H, Yang Y, Dai Y (2015) Quercetin promotes neuronal and behavioral recovery by suppressing inflammatory response and apoptosis in a rat model of intracerebral hemorrhage. Neurochem Res 40:195–203
Xu J, Wang H, Ding K, Zhang L, Wang C, Li T, Wei W, Lu X (2014) Luteolin provides neuroprotection in models of traumatic brain injury via the Nrf2–ARE pathway. Free Radic Biol Med 71:186–195
Zhu HT, Bian C, Yuan JC, Chu WH, Xiang X, Chen F, Wang CS, Feng H, Lin JK (2014) Curcumin attenuates acute inflammatory injury by inhibiting the tlr4/myd88/nf-κb signaling pathway in experimental traumatic brain injury. J Neuroinflammation 59:1–17
Fann DY, Lee SY, Manzanero S, Chunduri P, Sobey CG, Arumugam TV (2013) Pathogenesis of acute stroke and the role of inflammasomes. Ageing Res Rev 12:941–966
Xu F, Shen G, Su Z, He Z, Yuan L (2019) Glibenclamide ameliorates the disrupted blood–brain barrier in experimental intracerebral hemorrhage by inhibiting the activation of NLRP3 inflammasome. Brain Behav 9:e01254
Ismael S, Zhao L, Nasoohi S, Ishrat T (2018) Inhibition of the NLRP3-inflammasome as a potential approach for neuroprotection after stroke. Sci Rep 8:5971
Lai X, Xiong Y, Zhou J, Yang F, Peng J, Chen L, Zhong W (2019) Verbascoside attenuates acute inflammatory injury in experimental cerebral hemorrhage by suppressing TLR4. Biochem Biophys Res Commun 519:721–726
Wang YC, Wang PF, Fang H, Chen J, Xiong XY, Yang QW (2013) Toll-like receptor 4 antagonist attenuates intracerebral hemorrhage-induced brain injury. Stroke 44:2545–2552
Xiong L, Mao S, Lu B, Yang J, Zhou F, Hu Y, Jiang Y, Shen C, Zhao Y (2016) Osmanthus fragrans flower extract and acteoside protect against d-galactose-induced aging in an icr mouse model. J Med Food 19:54–61
Garcia JH, Wagner S, Liu KF, Hu XJ (1995) Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats: statistical validation. Stroke 26:627–635
Yang Y, Zhang Y, Wang Z, Wang S, Gao M, Xu R, Liang C, Zhang H (2016) Attenuation of acute phase injury in rat intracranial hemorrhage by cerebrolysin that inhibits brain edema and inflammatory response. Neurochem Res 41:748–757
Chang CF, Wan J, Li Q, Renfroe SC, Heller NM, Wang J (2017) Alternative activation-skewed microglia/macrophages promote hematoma resolution in experimental intracerebral hemorrhage. Neurobiol Dis 103:54–69
Song HL, Zhang SB (2019) Therapeutic effect of dexmedetomidine on intracerebral hemorrhage via regulating NLRP3. Eur Rev Med Pharmacol Sci 23:2612–2619
Yuan R, Fan H, Cheng S, Gao W, Xu X, Lv S, Ye M, Wu M, Zhu X, Zhang Y (2017) Silymarin prevents NLRP3 inflammasome activation and protects against intracerebral hemorrhage. Biomed Pharmacother 93:308–315
Zhao H, Pan P, Yang Y, Ge H, Chen W, Qu J, Shi J, Cui G, Liu X, Feng H, Chen Y (2017) Endogenous hydrogen sulphide attenuates NLRP3 inflammasome-mediated neuroinflammation by suppressing the P2X7 receptor after intracerebral haemorrhage in rats. J Neuroinflammation 14:163
Yin D, Zhou S, Xu X, Gao W, Li F, Ma Y, Sun D, Wu Y, Guo Q, Liu H, Han L, Wang Z, Wang Y, Zhang J (1698) Dexmedetomidine attenuated early brain injury in rats with subarachnoid haemorrhage by suppressing the inflammatory response: The TLR4/NF-κB pathway and the NLRP3 inflammasome may be involved in the mechanism. Brain Res 2018:1–10
Zheng B, Zhang S, Ying Y, Guo X, Li H, Xu L, Ruan X (2018) Administration of Dexmedetomidine inhibited NLRP3 inflammasome and microglial cell activities in hippocampus of traumatic brain injury rats. Biosci Rep 38:BSR20180892
Alipieva K, Korkina L, Orhan IE, Georgiev MI (2014) Verbascoside-a review of its occurrence, (bio) synthesis and pharmacological significance. Biotechnol Adv 32:1065–1076
Pérez-Barrón G, Avila-Acevedo JG, García-Bores AM, Montes S, García-Jiménez S, León-Rivera I, Rubio-Osornio M, Monroy-Noyola A (2015) Neuroprotective effect of buddleja cordata methanolic extract in the 1-methyl-4-phenylpyridinium parkinson’s disease rat model. J Nat Med 69:86–93
Wang S, Yao Q, Wan Y, Wang J, Huang C, Li D, Yang B (2019) Adiponectin reduces brain injury after intracerebral hemorrhage by reducing NLRP3 inflammasome expression. Int J Neurosci 22:1–8
Li X, Wang T, Zhang D, Li H, Shen H, Ding X, Chen G (2018) Andrographolide ameliorates intracerebral hemorrhage induced secondary brain injury by inhibiting neuroinflammation induction. Neuropharmacology 141:305–315
Acknowledgments
I would like to express my gratitude to all who contributed to this study. I would like to thank my supervisor, Changren Huang, who has offered valuable suggestions and helped design the experiments. Secondly, I would like to express my heartfelt gratitude to Huiyong Huang who provided strong advice when revising this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, H., Zhang, C. & Huang, C. Verbascoside Attenuates Acute Inflammatory Injury Caused by an Intracerebral Hemorrhage Through the Suppression of NLRP3. Neurochem Res 46, 770–777 (2021). https://doi.org/10.1007/s11064-020-03206-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-03206-9