Abstract
Injury severity is correlated with poor prognosis after traumatic brain injury (TBI). It is not known whether triglycerides (TGs) or total cholesterol (TC) is good biomarker of increased injury of neuroinflammation and apoptosis in a high fat diet (HFD)-treated rat after TBI episodes. Five-week-old male Sprague–Dawley (SD) rats were fed a HFD for 8 weeks. The anesthetized male SD rats were divided into three sub-groups: sham-operated and TBI with 1.6 atm or with 2.4 atm fluid percussion injury (FPI). Cell infarction volume (triphenyltetrazolium chloride stain), tumor necrosis factor-alpha (TNF-α) expression in the microglia (OX42 marker) and astrocytes (Glial fibrillary acidic protein marker), TNF-α receptor expression in the neurons (TNFR1 and TNFR2 markers), and the extent of neuronal apoptosis (TUNEL marker) were evaluated by immunofluorescence, and the functional outcome was assessed by an inclined plane test. These tests were performed 72 h after TBI. Serum triglyceride and cholesterol levels were measured at 24, 48 and 72 h after TBI. The FPI with 2.4 atm significantly increased body weight loss, infarction volume, neuronal apoptosis and TNF-α expression in the microglia and astrocytes, and it decreased the maximum grasp degree and TNFR1 and TNFR2 expression in neurons at the 3rd day following TBI. The serum TG level was positively correlated with FPI force, infarction volume, Neu-N-TUNEL, GFAP-TNFα, and OX42-TNFα Simultaneously; the serum TG level was negatively correlated with Neu-N-TNFR1 and Neu-N-TNFR2. TG is a good biomarker of increased injury for neuroinflammation and apoptosis at the 3rd day after TBI in HFD rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) remains a great public health challenge, with worldwide incidence rates estimated from 811 per 100,000/year in New Zealand to 7.3 per 100,000/year in Western Europe [1]. A high fat diet (HFD), which induces hyperlipidemia by increasing serum total cholesterol (TC) and triglyceride (TG) levels, is associated with metabolic syndrome [2], which affects approximately 25% of the world’s population and increases in incidence and prevalence with age [3]. Therefore, neurosurgeons can expect to see more TBI patients with pre-existing hyperlipidemia in daily practice. Since the brain tissue has the highest lipid content and the lipid expression in the blood is reflective of its expression in brain tissues, the serum TG level is positively correlated with that of the brain [4,5,6]. In this research, we determine whether TC or TG can be used as a potential biomarker of increased injury severity in HFD to represent the major aspects of therapeutic management and be clinically useful after TBI.
Neuroinflammation is a key secondary injury after a TBI event. The extent of neuroinflammation depends on the severity of cell damage. Following TBI, activated astrocytes and microglia led to the prolonged release of the neuroinflammatory factor tumor necrosis factor-alpha (TNF-α), resulting in neuronal apoptosis [7, 8] through the TNF-α-mediated death/survival cognate receptorsTNFR1/TNFR2 [9, 10]. However, it has been reported that the consumption of a HFD can induce neuroinflammationin a non-TBI animal model [11,12,13,14], such as in a kainic acid-induced seizure mouse model [14]. However, the effects of injury severity of TBI on neuroinflammation and apoptosis of HFD rats have not been investigated.
The effect of HFD on TBI animal models show that a HFD can impair cognitive function [15], impair somatosensory and working memory performance [16] shorten telomere length [17] and induce epigenetic change [18]. In our recent study, we have demonstrated rats fed a HFD for 8 weeks had higher neuronal apoptosis or neuroinflammation after 2.2 atm fluid percussion injuries (FPI) model when compared to sham rats [19]. However, it is not known whether TG or TC is a biomarker of neuroinflammation and apoptosis in a HFD-fed rat after different injury force of TBI episodes.
The current study hypothesized that the severity of injury would affect the development of increased TC and TGs, followed by neuroinflammation and neuronal apoptosis, and would eventually exacerbate the functional outcomes in HFD-fed rats after TBI events; TG and TC are biomarkers of neuroinflammation and neuronal apoptosis. To test this hypothesis, we investigated regional microglia and astrocyte activation, TNF-α expression, TNFR1 and TNFR2 expression in neurons, and neuronal apoptosis in the brain. We also measured the peripheral TC and TG concentrations at 24 h, 48 h, and 72 h. After TBI and the functional outcome on the 3rd day after TBI using 1.6 atm or 2.4 atm FPI model. Our results will help elucidate the effects of different injury force on TBI in HFD rats. Monitoring the severity of TBI progression by indicators and analyzing the results may provide laboratory evidence for subsequent anti-injury research. These findings will improve our understanding of the adverse effects of increased injury force on HFD and help establish treatment and prevention protocols.
Materials and Methods
Experimental Design
Figure 1 shows the overall experimental protocol. A total of 54 rats were used in current study. The rats were numbered in random order and assigned to different study groups. All of the experimental procedures followed the Animal Protection Act, Council of Agriculture, Executive Yuan, R.O.C. (Taiwan) and were approved by the Chi-Mei Medical Center Animal Care and Use Committee (ICCUC), which conformed to National Institutes of Health guidelines. Animals were separated into three major groups: sham, TBI with 1.6 atm FPI, and TBI with 2.4 atm FPI. To avoid potential interrater variability for all objects and lab experimenters, all rats were measured by the same lab experimenter.
Induced High Cholesterol and Triglyceride Rat Model Methods
Five-week-old male Sprague–Dawley rats were fed a high fat diet containing 60.9 kcal% fat, 18.3 kcal% protein, and 20.1 kcal carbohydrates (58Y1; TestDiet, Richmond, IN, USA) ad libitum for 8 weeks. Serum total cholesterol, triglycerides and body weights were measured at the end of 8 weeks. Blood samples (1 mL) were drawn from the tail vein and analyzed using an auto-analyzer (Quik-Lab, Elkhart I, NJ, USA).
Traumatic Brain Injury
Animals were anesthetized and intramuscularly injected with a mixture of ketamine (44 mg/kg), atropine (0.02633 mg/kg), and Rompun (6.77 mg/kg). Using a stereotaxic frame, a right craniectomy (with a radius of 2 mm) was performed 4 mm from the bregma and 3 mm from sagittal sutures. A fluid percussion device (VCU Biomedical Engineering, Richmond, VA, USA) was connected, and the brain was injured with a 1.6 atm (moderate TBI) or 2.4 atm (high TBI) with 25 ms percussion, which produced brain trauma [20]. The detailed procedures are as described by Chuang et al. [21].
TC and TG Measurement
Blood samples (1 mL) were drawn from the tail vein and centrifuged at 3500 rpm for 15 min at 4 °C to separate the serum and blood cells. The TC and TG concentrations were measured at 24, 48 and 72 h after TBI using an enzymatic method in an ARCHITECTC8000 machine (Abbott, Illinois, US).
Motor Function Test
Animals were placed facing right and then left perpendicular to the 20 × 20-cm buffer ribbed surface of an inclined plane, which was initially positioned at a slope of 55°. The maximal angle at which an animal could remain on the inclined plan was recorded. Motor deficit measurements were conducted with left- and right-side maximal angles at 72 h following TBI.
Cerebral Infarction Volume Assay
Infarction volume was measured using triphenyltetrazolium chloride (TTC) staining at 72 h following TBI [22]. Briefly, The brain tissue was immersed in cold saline for 5 min and sliced into 2.0-mm sections, and then the slices were incubated in 2% TTC dissolved in phosphate-buffered saline for 30 min at 37 °C and then transferred to a 5% formaldehyde solution for fixation. The infarction volume, as revealed by negative TTC stains indicating dehydrogenase-deficient tissue, was measured in each slice and summed using computerized planimetry (PC-based Image Tools software, Image-Pro Plus Media Cybernetics, Inc., Rockville, MD, USA). The infarction volume was calculated as 2 mm (thickness of the slice) × [sum of the infarction areas in all brain slices (mm2)].
Immunofluorescence Staining
Adjacent 6 μm sections corresponding to coronal coordinates 0.20 mm to 0.70 mm anterior to the bregma were incubated in 2 mol/L HCl for 30 min, rinsed in 0.1 mol/L boric acid (pH 8.5) for 3 min at room temperature and incubated with primary antibodies in PBS containing 0.5% normal bovine serum at 4 °C overnight. Sections were washed in PBS and incubated with secondary antibodies for 1 h at room temperature. The number of positive immunofluorescent cells was calculated in five coronal sections near the Bregman − 4.8 mm corresponding to the peri-lesioned cortex (×400 magnification) and are expressed as the mean number of positive cells from each rat using computerized planimetry (Image-Pro Plus Media Cybernetics, Inc., Rockville, MD, USA).
Neuroinflammation and Neuronal Apoptotic Assay in the Peri-Lesioned Cortex Using Immunofluorescence Staining on the 3rd Day After TBI
Activated microglia and astrocytes were evaluated by detecting OX42- (microglia marker) and GFAP (astrocyte marker)-positive cells using an immunofluorescence assay [23] TNF-α expression in activated microglia or astrocytes was evaluated by detecting OX42- or GFAP- plus TNFα-positive cells using a double-stained immunofluorescence assay.
TNFR1 and TNFR2 expression in neuronal cells was evaluated by detecting co-stained neu-N and TNFR1 or TNFR2 positive cells using a double-stained immunofluorescent assay.
Neuronal apoptotic cells were identified by staining with terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick-end labeling (TUNEL) [24].The numbers of Neu-N-positive cells in 4′,6-diamidino-2-phenylindole(DAPI)-positive cells and TUNEL-positive or caspase-3-positive cells in Neu-N-positive cells were calculated. The detailed information of antibodies used was summarized on Table 1.
Statistical Analysis
A descriptive statistical analysis was used in this study. The average of the TC and TGs (means ± standard deviation) between the three groups (sham, TBI 1.6 atm, and TBI 2.4 atm) from Day0 to Day3 presented with a trend towards change. In addition, the distribution of the variables of interest between these three groups was plotted using a box plot with a Kruskal–Wallis test to compare the difference. To estimate the association between the TG/TC and variables of interest, a scatter plot was used to display the set of two variables of interest, and the strength of the linear relationship was measured using Pearson’s correlation coefficient. All of the statistical analyses were performed with STATA (version 12; Stata Corp., College Station, TX, USA), and a p value < 0.05 was considered to be statistically significant.
Results
Daily Change in Serum TG and TC Levels After TBI
Serum TC was not Different in HFD-Fed Rats 3 Days After Different Injury Force of TBI
Figure 2 shows the peak TC level occurs at day 2 after TBI. The daily TC level shows no significant difference among the sham and the TBI of 1.6 atm or of 2.4 atm groups.
Serum TG Increased Significantly in Rats at Day 1 and Days 3 After Different Injury Force of TBI
Figure 3 shows that the peak serum TG level occurs at day 1.Compared with the sham group, the daily TG level is significantly higher at day 1 and day3 after TBI of 1.6 atm or of 2.4 atm.
High FPI Force Significantly Increased TNF-α Expression in Activated Astrocytes and Microglia in the Peri-Lesioned Cortex on the 3rd Day After TBI
The number of OX42 plus TNF-α double stained cells was significantly higher in the TBI of 1.6 atm group (12.5 (median) group vs. 0, ***p < 0.001, n = 6 per group) and the TBI of 2.4 atm group (19.5 (median) vs. 0, ***p < 0.001, n = 6 per group, Fig. 4) than the sham-operated rats in the peri-lesioned cortex region 3 days after TBI. The number of GFAP plus TNF-α double stained cells was significantly higher in the TBI of 1.6 atm group (16 (median) vs. 0, ***p < 0.001, n = 6 per group) and the TBI of 2.4 atm group (17 (median) vs. 0, ***p < 0.001, n = 6 per group, Fig. 5) than the sham-operated rats in the peri-lesioned cortex region 3 days after TBI.
High FPI Force Significantly Decreased the TBI-Induced TNFR1 and TNFR2 Expression in Neuronal Cells in the Peri-Lesioned Cortex on the 3rd Day After TBI
In the TNFR1 plus Neu-N double stained assay, the number of positive neuronal TNFR1 cells in the peri-lesioned cortex of the TBI 1.6 atm rats (24 (median) vs. 76.5 (median), ***p < 0.001, n = 6 per group) and TBI of 2.4 atm rats (34.5vs.76.5 (median), ***p < 0.001, n = 6 per group, Fig. 6)were significantly decreased compared with those in the sham controls. Simultaneously, the number of positive neuronal TNFR2 cells in the peri-lesioned cortex of the TBI of 1.6 atm rats (25 (median) vs. 76.5 (median), ***p < 0.001, n = 6 per group) and TBI of 2.4 atm rats (16 (median) vs. 59 (median), ***p < 0.001, n = 6 per group, Fig. 7) were significantly decreased compared with those in the sham controls.
High FPI Force Significantly Increased Neuronal Apoptosis in the Peri-Lesioned Cortex on the 3rd Day After TBI
The TUNEL assay revealed that the number of apoptotic neuronal cells (Neu-N plus TUNEL) in the peri-lesioned cortex was increased in the TBI of 1.6 atm rats (29.5 (median) vs. 0 ± 0, ***p < 0.01) and the TBI 2.4 atm rats (57.5 (median) vs. 0, ***p < 0.001; n = 6 per group) compared to the sham rats 3 days after TBI (Fig. 8).Among these three groups, the TBI of 2.4 atm rats had the greatest degree of neuronal apoptosis (Fig. 8).
High FPI Force Significantly Increased TBI-Induced Cerebral Infarction Volume on the 3rd Day After TBI
At 72 h following TBI, the TTC-stained infarction volume was significantly higher in the TBI of 1.6 atm rats than in the infarcted area of sham controls (73.3 mm3 (median) vs. 0, p < 0.001; n = 6 per group). Among these three groups, the TBI of 2.4 atm rats (127.0 mm3 (median); n = 6 per group) had the greatest cerebral infarction volume (Fig. 9).
High FPI Force Significant Increase in TBI-Induced Body Weight loss On the 3rd Day After TBI
On the 3rd day after TBI, body weight losses were significantly increased in the TBI of 1.6 atm (20 (median) vs. 13.5 (median), *p < 0.05, n = 6 per group) and the TBI of 2.4 atm (43 (median) vs. 13.5 (median), ***p < 0.001, n = 6 per group) rats compared to the sham controls. Among these three groups, the TBI of 2.4 atm rats had the greatest weight loss (Fig. 10).
High FPI force Significantly Decreased Motor Function on the 3rd Day After TBI
The maximal grip angle of rats on the inclined plane on the 3rd day after TBI was significantly lower in the TBI 2.4 atm rats rats 46.05 (median) Vs TBI 1.6 atm rats 52.3 (median #p < 0.001, n = 6 per group)), and vs. sham rats 57 (median**p < 0.001, n = 6 per group. Among these three groups, the TBI 2.4 atm rats had the smallest maximal grip angle (Fig. 11).
Serum TC is Significantly Positively Correlated with Infarction Volume but not Neuroinflammation or Apoptosis Markers at the 3rd Day After TBI
Figure 12 shows that the serum TC is significantly positively correlated with infarction volume in the cortex (r = 0.657, p = 0.0031).Serum TC showed a non-significant positive correlation with NeuN-TUNEL (r = 0.3218, p = 0.1929), OX42-TNF-α (r = 0.2528, p = 0.3115), and GFAP-TNF-α (r = 0.2862, p = 0.2496); non-significant negative correlations to Neu-N-TNFR1 (r = − 0.2944, p = 0.2357), Neu-N-TNFR2 ( r = − 0.136, p = 0.5904) and body weight loss (r = − 0.3218 p = 0.1929) were also observed.
Serum TG is Significantly Correlated with Infarction Volume, Neuroinflammation and Apoptosis, and Body Weight Loss at the 3rd Day After TBI
As shown in Fig. 13, on the third day after TBI, serum TG is significantly positively correlated with body weight loss (r = 0.5259 p = 0.0250) and infarction volume in the cortex (r = 0.7201, p = 0.0008). Serum TG was also significantly positively correlated with NeuN-TUNEL (r = 0.4999, p = 0.0347), OX42-TNF-α (r = 0.6064, p = 0.0076), and GFAP-TNF-α (r = 0.6123, p = 0.0069). Serum TG was significant negatively correlated with Neu-N-TNFR1 (r = − 0.7144, = 0.0009) and Neu-N-TNFR2 (r = − 0.5567, p = 0.0164). However, TG is non-significantly negatively correlated with motor function (r = − 0.4241, p = 0.0794).
Discussion
Summary of Current Study
To our knowledge, this is the first study to test whether TG or TC is a biomarker of neuroinflammation and apoptosis in a HFD-fed rat after different injury force of TBI episodes. We found dose–response correlation between sham, low, and high intensity brain FPI and serum triglycerides (and to a much lesser extent serum total cholesterol) in HFD rats. We consider since the serum TG is easy to measure; we have the opportunity to treat high TG in clinical applications by drugs or dietary management in TBI patients.
Daily Change in Serum TG and TC Levels After TBI
In the present study, the peak serum TG occurred at day 1 after TBI, while peak serum TC occurred at day 2 after TBI. Under normal conditions, TG can rapidly cross the blood–brain barrier (BBB) while cholesterol cannot. One explanation for the presence of TG in the blood at earlier time points than TC may be that TG crosses the BBB more easily, especially following TBI, TG and TC were excreted from the injured brain and the BBB breakthrough increased permeability at day 1 after brain insult [25,26,27]. Following TBI, activated astrocytes in the brain cortex released pancreatic TG lipase, which hydrolyzes the esteratic linkage of TG to free fatty acids [28]. Therefore, the increase in TG lipase following TBI may be one mechanism to explain the decrease in serum TG. These may also explain why are serum triglycerides higher in TBI 1.6 atm than in TBI 2.4 atm on day 1.
In the present study, the serum TG and TC may possibly originate from peripheral tissues [29]; therefore, we speculated that the brain-gut axis may play a role in the regulation of intestinal lipid profile metabolism after TBI [30]. Further studies are needed to confirm the exact role of the brain-gut axis after brain injury.
High FPI Force Significantly Worsens Neuroinflammation, Apoptosis And Functional Outcome In HFD Rats
Several studies have shown that TBI results in poor outcomes in rats on a normal diet [31, 32]. In reviewing the previous studies about the effects of TBI on HFD-fed rats, all of the focus is on the effects after a single impact force in different models [15,16,17,18]. As expected, we provide the scientific results that a high impact force with FPI 2.4 atm significantly worsens neuroinflammation, apoptosis and functional outcome in HFD rats.
Serum TG, but not TC, is Significantly Correlated with Infarction Volume, Neuroinflammation and Apoptosis Markers on the 3rd Day After FPI
Our study showed that serum TG, which was correlated with body weight loss, was significantly correlated with the expression of cerebral OX42-TNF-α, GFAP-TNF-α, Neu-N-TNFR1, Neu-N-TNFR2, NeuN-TUNEL, and TTC staining. Because BBB breakthrough increased permeability after brain insult has been reported [25,26,27], we therefore propose that serum TG could pass the BBB and promote the secretion of the inflammatory cytokine TNF-α from activated microglia and astrocytes, in addition to affecting the expression of Neu-N-TNFR1 Neu-N-TNFR2, inducing neuronal apoptosis, and finally increasing infarction volume. These results support our hypothesis that serum TG could be a biomarker of neuroinflammation and neuronal apoptosis in this HFD condition.
The TNF-α receptors in the central nervous system include TNFR1 and TNFR2. TNFR1 promotes inflammatory degeneration and cell death, while TNFR2 regulates cell regeneration and survival [9, 10]. In the current study, compared with the TBI 1.6 atm group, we found that the numbers of apoptosis neurons were increased, while Neu-N-TNFR1 expression was significantly increased andNeu-N-TNFR2 expression was significantly decreased simultaneously in the TBI2.4 atm group. This result supports the concept that TNFR2 plays an important role in neural repair and survival, but failed to function in this critical condition. However, compared with the sham group, Neu-N-TNFR1 and Neu-N-TNFR2 were decreased both in the TBI 1.6 atm and 2.4 atm groups. One possible explanation for the decreased expression in these groups might be that fewer neurons are associated with lower Neu-N-TNFR1and Neu-N-TNFR2 expression after TBI.
Abnormal TTC staining represents cell infarction or death. Following TBI, the mechanism of cell death included necrosis, apoptosis and autophagy [33, 34]. In the current study, we found that the serum TG level is positively correlated with both TCC staining and neuronal apoptosis in HFD-fed rats. However, we found that the TC level is positively correlated with TCC staining but is not correlated with neuronal apoptosis in HFD-fed rats. This finding implies that the pathophysiology of TG and TC on neuronal death maybe not be on the same pathway. Funakoshi et al. reported that the accumulation of cellular cholesterol may cause necroptosis-like neuronal cell death, which is a form of cell death that has the morphological features of necrosis [35]. This issue is worth investigating in the future.
Consistent with previous studies, TBI increased body weight loss in rats on a normal diet [31, 32]. In the present study, we provide the new information that a high impact force with an FPI of 2.4 atm significantly worsens body weight loss at the 3rd day after TBI. However, when considering body weight control, leptin should be mentioned. Leptin, which is secreted from adipose tissue, crosses the blood brain barrier to the hypothalamus and regulates the body weight via decreasing appetite and increasing energy consumption [36]. Leptin also has an inverse correlation with proinflammatory cytokines after TBI [37]. Therefore, the role of leptin in our neuroinflammation/HFD/TBI model is worth investigating in the future.
The TG level was not significantly negatively correlated with motor function (r = − 0.4241, p = 0.0794).Since the pathophysiology of TBI is so complicated and complex, the functional outcome maybe determinate by multiple factors and difficult to predict [38]. Our result supports the hypothesis that high serum TG plays part of a negative role on motor function.
When compared serum TG at day 1 with infarction volume, neuroinflammation and apoptosis, and body weight loss on the 3rd day after TBI, serum TG was significantly correlated with neuroinflammation and apoptosis markers (data not showed). Whether serum TG on day 1 could be an early biomarker for neuroinflammation and apoptosis was difficult to conclude because of the lack of corresponding information on neuroinflammation and apoptosis on day 1. This issue needs evaluated in the future.
Limitations of the Current Study
Several limitations in our study should be considered. First, in the current study, we focus on the effects of different injury force on TBI in the experimental HFD rat. Whether these neurobehavioral and neuroinflammatory parameters were significantly different between rats fed with a HFD and normal diet rats, and injured control mice after different injury force of TBI are worth investigating.
Second, the potential sex differences in lipid metabolism following TBI should be evaluated [39]. In the future, a study design included both HFD male and female rats to clarify the differences in sex effects after different injury force of TBI will solve this consideration.
Third, the duration of HFD exposure would affect cerebral lipid and neurons in rat [40]. According to a report by Hoane et al., rats in the current study received 8 weeks of HFD exposure [16]. Whether long-term exposure to a HFD leads to a greater risk to the brain should be investigated in the future.
Fourth, since the lipid expression in blood is reflective of expression in brain tissue [4] and cerebral TG was positively correlated with serum TG [40], we did not investigate the TG concentrations in brain tissue or cerebrospinal fluid, which may truly reflect the time course of lipid metabolism in HFD-fed rats after a TBI event. In the future, in addition to detecting the lipid profile in brain tissue and cerebrospinal fluid, we also emphasize that sphingolipids are highly specific to the brain, are significantly up-regulated in post-injury serum, and can be used as quantifiable TBI biomarkers [41].
Fifth, in current study, these data strongly suggested that that serum TG was significantly correlated with the expression of cerebral OX42-TNF-α, GFAP-TNF-α, Neu-N-TNFR1, Neu-N-TNFR2 and neuronal apoptosis. However, the exactly mechanisms of triglyceride concentration associated with cellular activities remained unknown. Furthermore, it is very important to clarify the mechanism of changes in triglyceride concentration, such as were they due to catecholamine release as a consequence of stress? [42, 43].
Sixth, cholesterol in the blood plasma compartment exists in two forms, free cholesterol and cholesteryl esters. Both of which are constituents of circulating lipoproteins including chylomicrons, very low density lipoproteins, intermediate density lipoproteins, low density lipoproteins, and gigh ensity lipoproteins [44]. In current study, we only check the total cholesterol concentration, it needs to clarify how much of the total cholesterol increase was due to elevated cholesterol esters in the future.
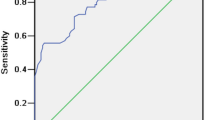
Finally, the current study showed that serum TG at a TBI of 1.6 atm and TBI of 2.4 atm could be a good biomarker of increased injury in HFD-fed rats at the 3rd after TBI. However, the optimal threshold to predict the severity and outcome needs to be clarified in the future. A combined receiver operating characteristic curve and specific severity score and functional score may solve this question.
Conclusion
We concluded that in the HFD-fed rats, the FPI force is correlated with neuroinflammation, apoptosis, functional outcome and serum TG level; serum TG is significantly correlated with the severity of injury in TNF-α production in activated microglia and astrocytes, TNFR1 and TNFR2 expression in neurons, neuronal apoptosis and infarction volume after FPI. Therefore, we have determined that serum TG is a good biomarker for neuroinflammation and apoptosis after different force of FPI at the 3rd day after TBI in a HFD rat model.
References
Li M, Zhao Z, Yu G, Zhang J (2016) Epidemiology of traumatic brain injury over the world: a systematic review. Austin Neurol Neurosci 1:1007
Laaksonen DE, Niskanen L, Lakka HM, Lakka TA, Uusitupa M (2004) Epidemiology and treatment of the metabolic syndrome. Ann Med 36:332–346
O'Neill S, O'Driscoll L (2015) Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev 16:1–12
Hogan SR, Phan JH, Alvarado-Velez M, Wang MD, Bellamkonda RV, Fernandez FM, LaPlaca MC (2018) Discovery of lipidome alterations following traumatic brain injury via high-resolution metabolomics. J Proteome Res 17(6):2131–2143
Sparvero LJ, Amoscato AA, Kochanek PM, Pitt BR, Kagan VE, Bayär H (2010) Massspectrometry based oxidative lipidomics and lipid imaging: applications in traumatic brain injury. J Neurochem 115:1322–1336
Yang W, Shi H, Zhang J, Shen Z, Zhou G, Hu M (2017) Effects of the duration of hyperlipidemia on cerebral lipids, vessels and neurons in rats. Lipids Health Dis 16(1):26
Zhang D, Hu X, Qian L, O’Callaghan JP, Hong JS (2010) Astrogliosis in CNS pathologies: is there a role for microglia? Mol Neurobiol 41:232
Lim SW, Wang CC, Wang YH, Chio CC, Niu KC, Kuo JR (2013) Microglial activation induced by traumatic brain injury is suppressed by postinjury treatment with hyperbaric oxygen therapy. J Surg Res 184:1076–1084
Dong Y, Fischer R, Naudé PJ, Maier O, Nyakas C, Duffey M, Van der Zee EA, Dekens D, Douwenga W, Herrmann A, Guenzi E, Kontermann RE, Pfizenmaier K, Eisel UL (2016) Essential protective role of tumor necrosis factor receptor 2 in neurodegeneration. Proc Natl Acad Sci USA 113:12304–12309
Probert L (2015) TNF and its receptors in the CNS: the essential, the desirable and the deleterious effects. Neuroscience 32:2–22
Thirumangalakudi L, Prakasam A, Zhang R, Bimonte-Nelson H, Sambamurti K, Kindy MS, Bhat NR (2008) High cholesterol-induced neuroinflammation and amyloid precursor protein processing correlate with loss of working memory in mice. J Neurochem 106:475–485
Pistell P, Morrison CD, Gupta S, Knight A, Keller JN, Ingram D (2010) Cognitive impairment following high fat diet consumption is associated with brain inflammation. J Neuroimmunol 219:25–32
Spagnuolo MS, Mollica MP, Maresca B, Cavaliere G, Cefaliello C, Trinchese G et al (2015) High fat diet and inflammation—modulation of haptoglobin level in rat brain. Front Cell Neurosci 9:479
Kang DH, Heo RW, Yi CO, Kim H, Choin CH, Roh GS (2015) High fat diet—induced obesity exacerbates kainic acid-induced hippocampal cell death. BMC Neurosci 16:72
Wu A, Molteni R, Ying Z, Gomez-Pinilla F (2003) A saturated-diet aggravates the Outcome of traumatic brain injury on hippocampal plasticity and cognitive function By reducing brain-derived neurotrophic factor. Neuroscience 119:365–375
Hoane MR, Swan AA, Herk SE (2011) The effects of a high-fat sucrose diet on functional outcome following cortical contusion injury in rat. Behav Brain Res 223:119–124
Mychasiuk R, Hehar H, Ma I, Esser MJ (2015) Dietary intake alters behavioral recovery and gene expression profiles in the brain of juvenile rats that have experienced a concussion. Front Behav Neurosci 9:17
Mychasiuk R, Hehar H, van Waes L, Esser MJ (2015) Diet, age, and prior injury status differentially alter behavioral outcomes following concussion in rats. Neurobiol Dis 73:1–11
Chong AJ, Wee HY, Chang CH, Chio CC, Kuo JR, Lim SW (2019) Effects of a high fat diet on neuroinflammation and apoptosis in acute stage after moderate traumatic brain injury in rats. Neurocrit Care. https://doi.org/10.1007/s12028-019-00891-5
McIntosh TK, Vink R, Noble L et al (1989) Traumatic brain injury in the rat: characterization of a lateral fluid-percussion model. Neuroscience 28:233
Chuang TJ, Lin KC, Chio CC, Wang CC, Chang CP, Kuo JR (2012) Effects of secretome obtained from normoxia-preconditioned human mesenchymal stem cells in traumatic brain injury rats. J Trauma Acute Care Surg 73:1161–1167
Wang Y, Lin SZ, Chiou AL, Williams LR, Hoffer BJ (1997) Glial cell line-derived neurotrophic factor protects against ischemia-induced injury in the cerebral cortex. J Neurosci 17:4341–4348
Koshinaga M, Katayama Y, Fukushima M (2000) Rapid and widespread microglial activation induced by traumatic brain injury in rat brain slices. J Neurotrauma 17:185–192
Mullen RJ, Buck CR, Smith AM (1992) Neu-N, a neuronal specific nuclear protein in vertebrates. Development 116:201–211
Bowman GL, Kaye JA, Quinn JF (2012) Dyslipidemia and blood-brain barrier integrity in Alzheimer's disease. Curr Gerontol Geriatr Res 2012:184042
Sekaran H, Gan CY, Latiff AA, Harvey TM, Nazri LM, Hanapi NA, Azizi J, Yusof SR (2019) Changes in blood-brain barrier permeability and ultrastructure, and protein expression in a rat model of cerebral hypoperfusion. Brain Res Bull 152:63–73
Backs WA, Farr SA, Salameh TS, Niehoff ML, Rhea EM, Morley JE, Hanson AJ, Hansen KM, Craft S (2017) Triglyceride cross the blood-brain-barrier and induce central leptin and insulin receprot resistance. Int J Obes 231:381–397
Jia J, Yan M, Lu Z, Sun M, He J, Xia C (2010) Regulated expression of pancreatic triglyceride lipase after rat traumatic brain injury. Mol Cell Biochem 335:127–136
Zhang J, Liu Q (2015) Cholesterol metabolism and homeostasis in the brain. Protein Cell 6:254–264
Farr S, Taher J, Adeli K (2016) Central nervous system regulation of intestinal lipid and lipoprotein metabolism. Curr Opin Lipidol 27:1–7
Wang CC, Wee HY, Hu CY, Chio CC, Kuo JR (2018) The effects of memantine on glutamic receptor-associated nitrosative stress in a traumatic brain injury rat model. World Neurosurg 112:e719–e731
Lim SW, Sung KC, Shiue YL, Wang CC, Chio CC, Kuo JR (2017) Hyperbaric oxygen effects on depression-like behavior and neuroinflammation in traumatic brain injury rats. World Neurosurg 100:128–137
Conti AC, Raghupathi R, Trojanowski JQ, McIntosh TK (1998) Experimental brain injury induces regionally distinct apoptosis during the acute and delayed post-traumatic period. J Neurosci 18:5663–5672
Zhang L, Wang H (2018) Autophagy in traumatic brain injury: a new target for therapeutic intervention. Front Mol Neurosci 11:190
Funakoshi T, Aki T, Tajiri M, Unuma K, Uemura K (2016) Necroptosis-like neuronal cell death caused by cellular cholesterol accumulation. J Biol Chem 291:25050–25065
Banks WA (2012) Role of the blood–brain barrier in the evolution of feeding and cognition. Ann NY Acad Sci 1264:13–19
Karaoğlan A, Akdemir O, Cınar N, Cal MA, Kelten B, Uzun H, Colak A (2011) Correlation between leptin and pro-inflammatory cytokines in cortical contusion injury model. Ulus Travma Acil Cerrahi Derg 17:298–302
Martinez BI, Stabenfeldt SE (2019) Current trends in biomarker discovery and analysis tools for traumatic brain injury. J Biol Eng 13:16
Palmisano BT, Zhu L, Ecke RH, Stafford JM (2018) Sex differences in lipid and lipoprotein metabolism. Mol Metab 15:45–55
Yang W, Shi H, Zhang J, Shen Z, Zhou G, Hu M (2017) Effects of the duration of hyperlipidemia on cerebral lipids, vessels and neurons in rats. Lipids Health Dis 16:26
Sheth SA, Iavarone AT, Liebeskind DS, Won SJ, Swanson RA (2015) Targeted lipid profiling discovers plasma biomarkers of acute brain injury. PLoS ONE 10:e0129735
McIntosh TK, Yu T, Gennarelli TA (1994) Alterations in regional brain catecholamine concentrations after experimental brain Iijury in the Rat. J Neurochem 63:1426–1433
Kunihara M, Oshima T (1983) Effects of epinephrine on plasma cholesterol levels in rats. J Lipid Res 24:639–644
Mahley RW (2016) Central nervous system lipoproteins: ApoE and regulation of cholesterol metabolism. Arterioscler Thromb Vasc Biol 36:1305–1315
Acknowledgements
The authors thank all of the researchers, especially Chiao-Ya Hu, who participated in this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
S-WL, H-XZ, H-YH, J-RK conceived and designed the experiments. H-XZ and J-RK performed the experiments. H-YH, C-HH and J-RK analyzed the data, C-HC and C-CC contributed reagents/materials/analysis tools, H-YH, J-RK wrote the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no biomedical financial interests or potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuo, JR., Lim, SW., Zheng, HX. et al. Triglyceride is a Good Biomarker of Increased Injury Severity on a High Fat Diet Rat After Traumatic Brain Injury. Neurochem Res 45, 1536–1550 (2020). https://doi.org/10.1007/s11064-020-03018-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-03018-x