Abstract
Alzheimer's disease (AD) is the most common form of dementia that progressively disrupts neurocognitive function, which has neither cure nor effective treatment. Hypercholesterolemia might be involved in brain alterations that could evolve into AD. The present study aims to evaluate the potential of omega-3, Co-enzyme Q10 (Co-Q10), as well as their combination in ameliorating hypercholesterolemia-initiated AD-like disease. We adapted a hypercholesterolemic (HC) rat model, a model of oxidative stress-mediated neurodegeneration, to study AD-like pathology. Hypercholesterolemia resulted in increased lipid peroxidation coupled with declined nitric oxide production, reduced glutathione levels, and decreased antioxidant activities of glutathione-s-transferase (GST) and glutathione peroxidase (GSH-Px) in the brain. Moreover, hypercholesterolemia resulted in decreased acetylcholine (ACh) levels and increased acetylcholine-esterase (AChE) activity, along with an increment of tumor necrosis factor and amyloid-β 42. Behaviorally, HC-rats demonstrated depressive-like behavior and declined memory. Treatment of HC-rats with omega-3 and Co-Q10 (alone or in combination) alleviated the brain oxidative stress and inflammation, regulated cholinergic functioning, and enhanced the functional outcome. These findings were verified by the histopathological investigation of brain tissues. This neuroprotective potential of omega-3 and Co-Q10 was achieved through anti-oxidative, anti-inflammatory, anti-amyloidogenic, pro-cholinergic, and memory-enhancing activities against HC-induced AD-like disease; suggesting that they may be useful as prophylactic and therapeutic agents against the neurotoxic effects of hypercholesterolemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer's disease (AD) is the most common form of senile dementia, accounting for between 60 and 80% of all dementias; the number of cases of AD worldwide is estimated to rise to approximately 40 million by 2020 and to 100 million by 2050 [1]. AD is a multifactorial disorder with complex etiology; besides genetic factors, environmental factors have been identified including obesity, diabetes mellitus, hypertension, and physical inactivity [2]. Interestingly, most of the AD risk factors may also be correlated with obesity and resulting comorbidities [3]. Obesity is associated with elevated risk for the development of neurodegenerative disorders, such as Alzheimer disease (AD) [4].
Accordingly, hypercholesterolemia could be regarded as one of the underlying molecular mechanisms leading to neurocognitive impairment [3] in several neurodegenerative disorders such as Alzheimer’s disease (AD) [5] and Parkinson’s disease [6]. Hypercholesterolemia is capable of inducing neuroinflammation [7], oxidative stress [8], mitochondrial dysfunction [9], and disturbing the balance of neurotransmitters [10]. Besides, hypercholesterolemia disrupts blood–brain barrier (BBB) permeability [11] that might be an early event in the pathogenesis of AD [12]. In addition, cardiovascular disease is a known risk factor for developing neurocognitive decline and dementia [13]; it has been estimated that 35% of coronary artery disease (CAD) patients may suffer from neurocognitive decline [14].
Unfortunately, there are not effective available drugs for completely cure AD, they can partially limit the symptoms but do not mitigate the progression of AD. Besides, cholesterol-lowering drugs such as statins could cause undesirable side effects [15]. Therefore, there is a pressing need for "new complementary therapeutic approaches", thus, the modulation of dietary habits and nutritional interventions could be an effective approach [16]. Neuroinflammation is involved in the development of neurodegenerative diseases [17]; therefore, anti-inflammatory therapeutic interventions could be used to manage hypercholesterolemia-related changes [18]. Thus, there is a great interest to explore the neuroprotective potential of natural antioxidants such as omega 3 polyunsaturated fatty acids (PUFAs) and coenzyme Q10 (Co-Q10) against hypercholesterolemia-induced AD-like pathology. Furthermore, anti-oxidant based therapy is considered a promising low-risk therapeutic strategy for AD.
The omega 3 precursor α-linolenic acid is metabolized into eicosapentaenoic acid (EPA; 20:5n-3) and docosahexaenoic acid (DHA; 22:6n- 3), which are the two major omega 3 fatty acids [19]. Omega 3 mediates different neural functions, such as signal transduction, neurotransmission, membrane fluidity, and myelination [20]. DHA is one of the most abundant lipids in the brain [21], it constitutes about 30% of the phosphoglycerides in the gray matter of the brain [22], suggesting that its action is essential for neural functioning [23]. Dietary intake of omega-3 is vital for normal neurodevelopment and brain health [24], as brain DHA levels tend to decrease with ageing and in AD-patients [25].
Coenzyme Q10 (Co-Q10) or ubiquinone, is a precursor of endogenous cholesterol and other metabolites [26], and acts as an electron carrier in the mitochondrial electron transport chain [27]. Ubiquinol, the reduced form of Co-Q10, is a potent lipophilic antioxidant, in the mitochondria, that participates in tocopherol and ascorbate resurrecting as antioxidants [28]. Disruption in levels of Co-Q10 might contribute to the development of neurodegenerative diseases [29]; this demonstrates the potential therapeutic use of Co-Q10 in AD-like pathology.
This study explores the possibility of using omega 3 and Co-Q10 for treatment of hypercholesterolemia-induced neurotoxicity in rats since most studies have concentrated on the peripheral tissues. Therefore, this study aimed to investigate the effect of hypercholesterolemia on brain alterations at behavioral, biochemical and morphological levels and to evaluate the neuroprotective potential of supplementation of omega 3 and/or Co-Q10 to HC-rats. It is important to investigate whether these brain alterations are reversible and thus whether the pathological mechanisms might be targeted by “nutritional or pharmacological interventions”.
Materials and Methods
Drugs
Omega-3 oil was purchased from (SEDICO Pharmaceutical Co., Egypt), in the form of soft gelatin capsules containing 1000 mg omega-3 fish oil (eicosapentaenoic acid (EPA) minimum 13% and docosahexaenoic acid minimum 9% (DHA)). Coenzyme Q10 (Co-Q10) powder was obtained from (MEPACO Pharmaceutical Co., Egypt).
Chemicals
The following ELISA kits were used: Amyloid-β peptide-42 (Aβ-42) ELISA kit was purchased from CUSABIO (USA), acetylcholinesterase (AChE) and acetylcholine (ACh) ELISA kit were purchased from MyBioSource (USA), tumor necrosis factor-α (TNF-α) was purchased from Biovision (USA), and Other chemicals were purchased from Sigma‐Aldrich Chem. (St. Louis, MO, USA). Determination of brain tissue levels of malondialdehyde (MDA), glutathione reduced (GSH), nitric oxide (NO), glutathione-s-transferase (GST) and glutathione peroxidase (GSH-Px) was performed using assay kits from Biodiagnostic Company (Egypt).
Animals and Grouping
Thirty Male Wistar rats (6–8 weeks) weighing 120 ± 10 g were obtained from the Animal House of the National Research Center (NRC), Egypt. Rats were allowed to acclimate for 1 week prior to experimental use. Rats were group-housed (6 rats/cage) and maintained at a constant temperature (22 ± 1.0 °C) and humidity (55 ± 5%), on an artificial 12 h light/dark cycle with lights on at 06:00 a.m. Rodent Chow and tap water were available ad libitum.
Induction of Hypercholesterolemia
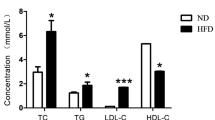
Hypercholesterolemia was induced in rats according to the method of Adaramoye [30], cholesterol was orally administrated at a dose of (30 mg/0.3 ml olive oil /1 kg animal) five times a week, and feeding rats a high fat "lard-based" diet for three consecutive months.
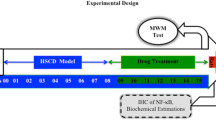
Experimental Design
After a 7-day acclimatization period, the 30 rats were randomly assigned to five groups (6 rats/group): Group (1): Negative control group. Group (2): Hypercholesterolemic (HC) rats served as positive control group and administrated high-fat diet and cholesterol (30 mg/0.3 ml olive oil /1 kg animal) for three months. Group (3): (HC-omega 3): HC-rats, after the 3-month-lasting diet, received an oral dose of omega-3 for 30 consecutive days at a dose 500 mg/kg body weight, according to Lakhwani et al. [31]. Group (4): (HC-CoQ 10): HC-rats, after the 3-month-lasting diet, received an oral dose of CoQ10 for 30 consecutive days at a dose 10 mg/kg body weight, according to Coldiron et al. [32]. Group (5): (HC-omega 3-CoQ 10): HC-rats, after the 3-month-lasting diet, treated orally with a combined treatment of both omega-3 (500 mg/kg body weight) and CoQ10 (10 mg/kg body) for 30 consecutive days.
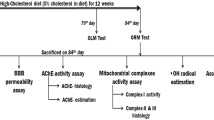
Behavioral Assessments
The behavioral tests were performed 24 h after a 30-day treatment period to assess depression and memory performance. The order of behavioral tests in each animal was the same: (a) forced swimming test (FST): on the 31st (pre-test day) and 32nd day (test day), (b) rewarded T-maze test: The order consisted of three successive days of training (33rd–35th) followed by a test on day 4 (on 36th day).
Porsolt Test (Forced Swimming Test (FST))
Porsolt test was used to evaluate depression-like behaviors [33]. Animals were forced to swim individually in the water tank (22 cm in diameter × 40 cm in height) containing water of 20 cm in depth at 25 °C from which there was no escape. In FST, a 10-min pre-test was done 24 h before the test day. Three actions were recorded using a digital timer: (1) Immobility: lack of motion of the whole body, the animal remained floating motionless in the water, making only those movements necessary to keep the head above water. (2) Swimming: represented as horizontal movements of the forepaws. (3) Climbing (struggling): represented as vigorous vertical movements of the forepaws, directed against the wall of the tank. These actions were recorded (in seconds) in the first 2 min of the test for each rat.
Rewarded T-Maze Test
The neurocognitive function and learning ability of rats were estimated by T-maze test (constructed in the NRC, Egypt) according to Deacon and Rawlins [34]. Before performing this experiment, the animals were left without food for 24 h, only with access to water. Behavioral observations were recorded (in seconds) at the end of the experiment.
Collection of Blood Sample
On 37th day, rats were fasted overnight, with free access to water; blood samples were collected from all groups just before sacrificing the rats (by cervical decapitation, to avoid the possible biochemical changes because of ischemia), under light anesthesia with diethyl ether. The blood was collected, before decapitation, from the sublingual vein of random rats in each group, the blood samples were left to clot in clean, dry test tubes for 30 min at room temperature and then centrifuged at 4000 RPM for 10 min. The clear supernatant serum was then frozen at − 20 °C for biochemical analysis of acetylcholine (ACh), acetylcholine esterase (AChE), amyloid-β 42 (Aβ-42), and tumor necrosis factor-α (TNF-α).
Brain Tissue Homogenate Sampling and Preparation
Rats were anesthetized and decapitated, with the head moved onto the dry ice, the whole brain was rapidly dissected on an ice-cooled glass plate, thoroughly washed with isotonic saline, dried on a filter paper, and sagittally divided into two portions. The first portion was homogenized using an electrical homogenizer (Remi 8000 RPM), to give 10% (w/v) homogenate in ice-cold medium in 9 volumes (1:9 w/v) of a 50 mM phosphate-buffered saline (PBS) pH 7.4 containing 0.1 mmol/L ethylene-diamine-tetra-acetic acid (EDTA). The unbroken cells and cell debris were removed by centrifugation at 4000 RPM for 30 min at 4 °C to prepare clear supernatants (10%). The obtained supernatant was used for biochemical analyses. The second portion of the brain (either right or left) was used for histopathological investigation.
Biochemical Analyses
Determination of Serum Acetylcholine (ACh)
Serum Acetylcholine (ACh) level was measured by ELISA according to the manufacturer’s instructions.
Determination of Serum Acetylcholinesterase (AChE)
Serum Acetylcholinesterase (AChE) level was estimated by ELISA according to the manufacturer’s instructions.
Determination of Brain Oxidative Stress Biomarkers
Lipid peroxidation was expressed as MDA that was determined by measuring thiobarbituric acid reactive species (TBARS) according to Ohkawa et al. [35]. Brain glutathione reduced (GSH) content was determined using the method of Beutler et al. [36]. Brain nitric oxide (NO) level was determined according to Montgomery and Dymock [37].
Determination of Brain Antioxidant Enzymes Activities
The enzymatic activities of GST and GSH-Px were measured spectrophotometrically in the brain homogenates according to Habig et al. [38] and Paglia and Valentine [39], respectively. The enzymatic activities were expressed as U/g tissue.
Determination of Serum Tumor Necrosis Factor-α (TNF-α)
Serum tumor necrosis factor-α (TNF-α) level was measured by ELISA according to the manufacturer’s instructions.
Determination of Serum Amyloid-β (Aβ-42)
Serum amyloid-β (Aβ-42) was determined using a commercially available ELISA kit, according to Selkoe [40].
Histopathological Investigations of the Brain
Sections of brain tissues were fixed in 4% buffered-saline formalin, dehydrated in graded ethanol and embedded in paraffin using standard procedures. Sections of 4-μm thickness were stained with hematoxylin and eosin (H&E) for histopathological examination, using a light microscope [41].
Statistical Analysis
Data were presented as Mean ± SEM (Standard Error of the mean), for n = 6 rats of each group. Data were subjected to Simple one-way analysis of variance (ANOVA) using SPSS (2016). Duncan’s multiple range test were used to differentiate between significant means at p < 0.05.
Results
The Effect of Omega 3 or/and CoQ-10 on Depressive-Like Behavior in HC-Rats During Forced Swimming Test (FST)
Immobility (Floating)
As shown in Fig. 1, HC-rats demonstrated a significant increase in time spent motionless (136.9%), as compared to control rats. Whereas, the mono-treatment with omega 3 or Co-Q10 reduced significantly the duration of immobility by 47.5% and 66.3%, respectively, as compared to HC-rats. In addition, the co-treatment with omega 3 and Co-Q10 resulted in a significant reduction in the duration of immobility by 73.7%, as compared to HC-rats.
The neuroprotective effect of omega 3, Co-Q10, and omega 3 + Co-Q10 on the time spent in the Porsolt test: immobility, swimming and climbing by HC-rats and different therapeutic groups. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c, d, e) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
Mobility (Swimming and Climbing/Struggling)
As shown in Fig. 1, HC-rats demonstrated a significant reduction for time spent during swimming (41.2%) or climbing (23.6%), as compared to control rats. On the other hand, mono-treatment with omega 3 increased significantly the durations of swimming and climbing by 96.2% and 8.2%, respectively. The same was for mono-treatment with Co-Q10; the durations of swimming and climbing were increased to 86.4% and 29.9%, respectively. The co-treatment showed a significant increase by 110.4% for the duration of swimming and 25.8% for the duration of climbing, as compared to HC-rats.
The Effect of Omega 3 or/and Co-Q10 on Memory Function in HC-Rats in Behavior Stress Maze: T-Maze Test
Our results in Fig. 2 showed a significant increase in time (90.5%) for HC-rats to reach the food in the T-maze, indicating neurocognitive impairment and memory decline. Whereas treated HC-groups with either omega 3 or/and Co-Q10 demonstrated a significant decrease in transit time to attain food, in comparison to HC-induced group; denoting improved cognitive function and learning ability.
The neuroprotective effect of omega 3, Co-Q 10, and omega 3 + Co-Q 10 on the transit time spent in the T-maze by HC-rats and different rat groups. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on Serum Acetylcholine (ACh) Levels and Acetylcholinesterase (AChE) Activities in HC-Rats
In HC-rats, the serum ACh levels were significantly lower by 22.7%, as compared to negative controls (Fig. 3). A slight increase in serum ACh was demonstrated after mono-treatment with omega 3 (8.8%) or Co-Q10 (5.6%), and (10.6%) for the combination treatment, as compared to HC-rats. On the other hand, by comparison to the control group, serum AChE activities in HC-rats were found to be higher than those of the control group, by 38.7%. However, treatment of HC-rats with omega 3, CoQ-10, or their combination resulted in a significant inhibition in serum AChE activities (11.3, 12.3 and 18.9%, respectively), as compared to HC-rats.
The neuroprotective effect of omega 3, Co-Q10, and omega 3 + Co-Q 10 on serum levels of acetylcholine (ACh) and acetylcholine esterase (AChE) in HC-rats. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c, d, e) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on Oxidative Stress Status in HC Rats
Induction of hypercholesterolemia in rats resulted in a statistically significant increase in lipid peroxidation marker (MDA) in the brain by 192.3%, whereas glutathione reduced (GSH) and nitric oxide (NO) were significantly declined by 49.1% and 70.9% respectively, as compared to control rats (Fig. 4a–c). In treated HC-rats, brain levels of MDA recorded a significant decrease (43.7%) for omega-3, (16.2%) for CoQ10 and (66.6%) for the co-treatment, as compared to HC-group. On the other hand, brain GSH and NO levels were significantly elevated by (27.9, 205.3%) for omega 3, (61.9, 225.6%) for Co-Q10 and (59.9, 355.1%) for the co-treatment, as compared with HC-rats. The results demonstrated a more significant anti-oxidative effect by the co-treatment than that of mono-treatment by omega 3 or Co-Q10.
The neuroprotective effect of omega 3, Co-Q10, and omega 3 + Co-Q10 on brain levels of malondialdehyde (MDA), glutathione reduced (GSH), and nitric oxide (NO) in HC-rats. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c, d) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on Enzymatic Antioxidants in HC Rats
HC-rats demonstrated significant inhibition in the enzymatic activities of GST and GSH-Px in the brain by 35.4, 61.3%, respectively, as compared to the control group (Fig. 5a, b). On the other side, treatment of HC-rats significantly increased the activities of these enzymes, as compared to the HC-rats, by (34.2, 88.6%) for omega-3, (51.4, 111.4%) for Co-Q10 and (57.5, 121.5%) for the co-treatment. It is worthy to mention that the co-treatment showed the highest enzymatic activities of GST and GSH-Px.
The neuroprotective effect of omega 3, Co-Q 10, and omega 3 + Co-Q 10 on activities of GST and GSH-Px in the brain of HC-rats. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on TNF-α Level in HC Rats
In HC-rats, hypercholesterolemia resulted in a significant increase in serum TNF-α level by 47.6%, as compared to negative controls. Treatment of HC-rats reversed the increase in serum TNF-α, by (7.3%) for omega 3, (7.0%) for Co-Q 10, and (13.1%) for the co-treatment, as compared to HC-rats (Fig. 6).
The neuroprotective effect of omega 3, Co-Q 10, and omega 3 + Co-Q 10 on serum levels of tumor necrosis factor-α (TNF-α) in HC-rats. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c, d) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on Aβ(1–42) Levels in HC-Rats
HC-induced rats demonstrated a significant elevation of serum amyloid-β protein that reached to 102.5%, as compared to control rats. On the other hand, mono-treatment of HC-rats with omega 3 and Co-Q10 resulted in a significant decrease in Aβ(1–42) production by 19.3 and 17.3%, as compared to the HC group. The co-treatment showed the most potent effect in this regard through reducing pathogenic amyloid-β protein production by 27.9%, as compared to HC-rats (Fig. 7).
The neuroprotective effect of omega 3, Co-Q 10, and omega 3 + Co-Q 10 on serum levels of amyloid-beta (Aβ) in HC-rats. Data are presented as mean ± SEM, (n = 6). Mean with different superscripts (a, b, c, d) are significant at p ≤ 0.05. Groups having the same letter are not significantly different from each other, while those having different letters are significantly different from each other
The Effect of Omega 3 or/and Co-Q10 on Brain Histopathology in Different Experimental Groups
Histopathological examination of the brain in different experimental groups is shown in Fig. 8. The brain tissues of negative control group revealed normal well-preserved cellular histoarchitecture with intact cell membrane, without histopathological alteration, and normal morphological structure of the cerebral cortex (Fig. 8a).
The effect of Omega 3 or/and Co-Q10 on brain histopathology in different experimental groups (Color figure online). a Brain section of normal control group the cerebellum showed normal histological features, a well-defined molecular (thin arrow), granular (presence of numerous closely packed small cells in the granular layer) (thick arrow) and Purkinje layers or Pyramid layer (large pyramid cells with vesicular nuclei) (dashed arrow) with normal structure of neuronal cells of the frontal cortex (white arrow), (H&E stain, ×200, ×400, ×400). b Brain section of HC-induced group showed the cerebellum with congestion and hemorrhage in meninges with congestion in cerebral cortical blood vessels (dashed arrow) with reduction in cellular size of the molecular layer (thin arrow), focal gliosis in cerebral cortex (white arrow) also showed granular cell layer (rounded head). Scattered sparse cell distribution of Purkinje layers or pyramid cells with vesicular nuclei (thick arrow), perineuronal oedema with neuronal shrinkage, amyloid plaque surrounded by astrocytes and microglia cells (rounded head) (H&E stain, ×100, ×200, ×400, ×400). c Brain section of HC-rats treated with omega 3 the cerebellum showed a well-defined molecular (thick arrow), granular (presence of numerous closely packed small cells in the granular layer) (white arrow) and Scattered sparse cell distribution of Purkinje layers or pyramid cells with vesicular nuclei (black arrow) with neuronal degeneration associated with neuronophagia in which the degenerated neurons appeared shrunken and surrounded by microglia cells (dashed arrow), Alzheimer type II astrocyte with enlarged nuclei of these astrocytes (rounded head). (H&E stain, ×200, ×400, ×400). d Brain section of HC-rats treated with Co-Q10 the cerebellum showed a well-defined molecular (dashed arrow), granular (presence of numerous closely packed small cells in the granular layer) (white arrow) and Scattered sparse cell distribution of Purkinje layers or pyramid cells with vesicular nuclei (black arrow) with neuronal degeneration associated with neuronophagia in which the degenerated neurons appeared shrunken and surrounded by microglia cells (thick arrow), focal gliosis with eosinophilic plaques (rounded head). (H&E stain, ×200, ×400, ×400). e Brain section of HC-rats treated with the combined treatment of both omega 3 and Co-Q10 the cerebellum showed almost normal histological features, a well-defined molecular (thick arrow), granular (presence of numerous closely packed small cells in the granular layer) (white arrow) and Purkinje layers or Pyramidal layer (large pyramid cells with vesicular nuclei) (thin arrow) with normal structure of neuronal cells of the frontal cortex (dashed arrow) (H&E stain, ×200, ×400, ×400)
On the other hand, the brain sections of HC-induced group (HC-brains), demonstrated congestion and hemorrhage in meninges with congestion in cortical blood vessels, spongy appearance, deposition of Aβ-plaques surrounded by astrocytes and microglia, fatty changes, loss of normal structure with vacuolations, and disruption of the cell membrane. The cerebral cortices showed focal gliosis and disorganization in the pyramidal cellular arrangement (Fig. 8b).
On the contrary, the examination of the brain tissues of HC-rats received mono-treatment with either omega 3 or Co-Q10 appeared more or less like normal sections but with some changes (Fig. 8c, d); the cerebella showed a well-defined histoarchitecture, associated with "neuronophagia" in which the degenerated neurons appeared shrunken and surrounded by phagocytic cells. In addition, the brain sections of HC-rats treated with the co-treatment (Fig. 8e) revealed almost normal histological features.
Discussion
Hypercholesterolemia is strongly correlated with the elevated risk of dementia [42]. This study sheds light on the neuroprotective potential of omega 3 and/or Co-Q10 against hypercholesterolemia-induced AD-like disease. In the current study, a hypercholesterolemic (HC) rat model was adapted. This is the first study that demonstrates the relation between hypercholesterolemia (as a depressant) and the effect of omega 3 and/or Co-Q10 (as anti-depressant) on the duration of immobility and active behavior (either swimming or climbing) in HC-rats. In the current study, HC-rats demonstrated a significant increase in duration of immobility while concomitantly showing a significant decrease in time spent during swimming or climbing (struggling), and increased transit time in T-maze (90.6%) as compared to controls, indicating depression-like behavior and displaying cognitive decline. This runs in agreement with several studies [43,44,45]. In contrast, Lavin et al. [46] and Nguyen et al. [47] observed that hypercholesterolemia has insignificant behavioral changes. This contradiction might be attributed to several factors including age and species of the animal, quality, quantity, and type of administrated fat [43], for example, lard-based fats were reported to induce a cognitive decline in HC-animals [45]. In this study, the "lard-based fat" was employed to induce hypercholesterolemia (HC) in rats.
The cholinergic function seems to be vulnerable to HC-induced neurotoxicity. HC-rats demonstrated cholinergic dysfunction represented by a significant decrease in serum ACh levels along with a significant elevation in serum AChE activity, as compared to the control group. This increased AChE activity accelerates the hydrolysis of ACh and resulted in its scarcity at the synaptic connections [48]. Besides, the deterioration of cholinergic activity might be related to the reduction of choline acetyltransferase activity and the disruption of acetyl Co-A synthesis that depends on pyruvate formation through energy-dependent glycolysis [48, 49]. This proves the assumption that hypercholesterolemia can disrupt the balance of neurotransmitters and induces changes in neurotransmission [50]
On the other hand, supplementation of omega 3 and/or Co-Q10 to HC-rats demonstrated anti-depressive behavior by significantly decreasing the duration of immobility. Omega 3 reduced depression-like behaviors, this runs in accord with several studies [51, 52]. In contrast, Jackson et al. [53] showed an insignificant effect of omega 3 on depression-related behavior or learning. Similarly, Co-Q10 demonstrated antidepressant-like behavior, this runs in agreement with Aboul-Fotouh [54] and Ashkani-Esfahani et al. [55]. Therefore, the omega 3 and Co-Q 10 demonstrated their the pro-cholinergic and anti-cholinesterase potentials via promoting cholinergic transmission, either through increasing ACh synthesis/release or inhibition of AChE activity, that finally results in preventing behavioral despair and neurocognitive decline. Both Omega 3 and Co-Q10 are capable of modulating cholinergic function, up-regulating mitochondrial function, and protecting neurons against neurotoxicity [56,57,58]. The neuroprotective activity of Co-Q10 is strongly co-related with its ability to cross BBB [59]. This explains the possible use of omega 3 and/or Co-Q10 as a therapeutic intervention in HC-induced neurotoxicity.
Besides, hypercholesterolemia induced oxidative stress in the HC-brains, manifested by elevated lipid peroxidation, depleted GSH content, decreased NO levels, and declined activities of GST and GSH-Px. This runs in parallel with several studies [60,61,62,63]. The declined activities of the antioxidant enzymes might be ascribed to high demand for these enzymes to de-activate HC-induced ROS generation [63]. The brain, due to its high metabolic rate, is highly sensitive to oxidative stress [64]. Lipid peroxidation is an early event in the AD progression [65]. Moreover, the reduced GSH content, the main antioxidant in the brain, increased the vulnerability of neurons to oxidative damage [66]; changes in glutathione redox status have been regarded as a very sensitive marker of oxidative stress [67], GSH antioxidant system is the main defense system against oxidative stress [68]. On the other side, the "NO depletion" is coupled with vascular dysfunction in HC-animals [69], and could represent a major player in the "early brain injury" through aggravating endothelial dysfunction, decreasing CBF and intensifying the brain injury [70].
Treatment of HC-rats with omega 3 and/or Co-Q10 almost completely reversed the oxidative damage by restoring the enzymatic activities, decreasing MDA levels, and increasing GSH and NO levels (Fig. 4.). The co-treatment demonstrated the best antioxidative potential. Omega 3 is able to inhibit lipid peroxidation in the brain [71] and to improve the complexes "I and IV" of the mitochondrial respiratory chain [72]. More interestingly, omega 3 reduced lipid peroxidation by increasing NO production that subsequently increasing CBF and supply of nourishment and facilitating the removal of toxic metabolites from the brain [73].
Our findings revealed a significant increase in brain GSH content in HC-omega 3 treated rats, this run in accordance with de Mello et al. [74]. On the other side, the anti-oxidative potential of Co-Q10 is accredited to its ability to revive antioxidants [75], to inhibit lipid peroxidation [76], and to increase endogenous brain Co-Q10 content [77]. Therefore, this anti-oxidative action of Co-Q10 and omega 3 could be a partial contributor to the enhancement of cholinergic activity and the subsequent anti-depressive and memory-enhancing activities. In a good connection with previous data, enhancing antioxidative activities could be employed as a therapeutic strategy to prevent cognitive decline or even to reduce secondary brain injury.
Oxidative stress activates the inflammatory cascade with enhanced production of inflammatory mediators; the oxidative stress and inflammation are enclosed in a vicious circle [78]. Hyperlipidemia-induced inflammation can damage the brain tissue and disrupts several neuronal functions [79]. That is why dyslipidemia and inflammation are currently regarded as risk factors for AD [80]. In this study, HC-induced oxidative stress enhanced the production of TNF-α by 47.6%, in comparison to controls, indicating the presence of neuroinflammation in the HC-brains. This runs in agreement with Puig et al. [81]. More interestingly, TNF-α was found to be responsive to the reversal of high-fat intake, indicating markers that may be responsive to therapeutic intervention [82].
The treatment of HC-rats with omega 3 and/or Co-Q10 antagonized the increment in TNF-α and mitigating the inflammatory state. Omega 3 showed its anti-inflammatory character through the direct interaction of DHA and EPA with inflammatory signaling pathways, inhibiting pro-inflammatory cytokines production, and subsequent inhibition of NF-κB phosphorylation [83,84,85]. Whereas, Co-Q10 was able to alleviate the inflammatory cascade through inhibiting the transcription of TNF-α genes, suppressing the activation of inflammatory signaling pathways and downregulating transcription factor NF-κB (nuclear factor kappa B), that up-regulates the pro-inflammatory TNF-α [86, 87]. Therefore, these potentials might play an essential role in the management of hypercholesterolemia and its involvement in the neuroinflammation. This study reinforces the beneficial effects of omega 3 and Co-Q10 even when eating too much-saturated fat and without any diet changes, which is quite common for obese patients.
Hypercholesterolemia provoked the elevation of serum Aβ level in HC-rats by 102.5%, as compared to control rats. This runs in agreement with de Lima Oliveira et al. [82] and Park et al. [88]. Hypercholesterolemia boosts the severity of Aβ-induced pathologies by stimulating the amyloidogenic pathway, through enhancing β- and γ-secretase activities, facilitating abnormal Aβ-production and deposition [89], reducing clearance, or a combination of these factors [80]. Besides, astrocytic and glial activation plays a key role in amyloid degradation and enhanced microglial activation [90].
Mono-treatment of HC-rats with omega 3 or Co-Q10 resulted in a significant reduction in serum Aβ levels by (19.3 and 17.3%), while the co-treatment showed the highest anti-amyloidogenic activity (27.9%), as compared to control rats. Treatment with omega 3 and Co-Q10 limits the overproduction and accumulation of neurotoxic Aβ through enabling the interaction of α-secretase with APP, to produce non-amyloidogenic and non-pathogenic products, attenuates Aβ-induced neurotoxicity, and suppresses neuroinflammation. This runs in agreement with several studies [91,92,93,94].
Meanwhile, the histopathological study supports the behavioral and biochemical findings. Neuroprotection has been found in the brain tissues following treatment with omega 3 and/or CoQ-10, signifying the structural and functional roles of omega-3 through influencing the membrane fluidity and enzyme activity in the brain [95]. Similarly, Co-Q10 resulted in the improved histopathological structure of the brain and reduced Aβ formation [96].
Future Directions
Further studies, on the molecular level, in different brain regions are recommended to elucidate the underlying neuroprotective mechanisms against hypercholesterolemia-induced neurotoxicity and to endorse the combination of omega 3 and Co-Q10 as a routine clinical treatment for AD-like patients. Furthermore, this study aimed to provide a set of blood-based biomarkers that could predict cognitive decline in obese patients.
Conclusion
This present study offered more evidence regarding the role of hypercholesterolemia as a risk factor for AD, and showed the potentials of omega 3 and/or Co-Q10 against hypercholesterolemia-induced neurotoxicity. Treatment of HC-rats with omega 3 or Co-Q10 improved the selected parameters with variable degrees; however, the co-treatment showed the most promising outputs; through exerting synergistic "amplified" pro-cholinergic, anti-cholinesterase, anti-amyloidogenic, anti-oxidative anti-inflammatory potentials that resulted ultimately in the improvement of cognitive function. Omega 3 and Co-Q10 seems to be "attention-grabbing antioxidants" that merits supplementation in obese patients at high risk of developing AD.
Abbreviations
- AD:
-
Alzheimer's disease
- AChE:
-
Acetylcholine-esterase
- TNF-α:
-
Tumor necrosis factor-α
- Aβ-42:
-
Amyloid-β 42
- ACh:
-
Acetylcholine
- EPA:
-
Eicosapentaenoic acid
- DHA:
-
Docosahexaenoic acid
- GST:
-
Glutathione-s-transferase
- GSH-Px:
-
Glutathione peroxidase
References
Alzheimer Association (2016) Alzheimer’s disease facts and figures. Alzheimer’s Dement 12:1–80. https://doi.org/10.1016/j.jalz.2016.03.001
Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C (2014) Potential for primaryprevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol 13:819–828
Petrov D, Pedros I, Artiach G, Sureda FX, Barroso E, Pallas M et al (2015) High-fat diet-induced deregulation of hippocampal insulin signaling and mitochondrial homeostasis deficiencies contribute to Alzheimer disease pathology in rodents. Biochim Biophys Acta 1852(9):1687–1699
Shefer G, Marcus Y, Stern N (2013) Is obesity a brain disease? Neurosci Biobehav Rev 37(10 Pt 2):2489–2503
Bane TJ, Cole C (2015) Prevention of Alzheimer disease: the roles of nutrition and primary care. Nurse Pract 40(5):30–36
Miyake Y, Tanaka K, Fukushima W, Sasaki S, Kiyohara C, Tsuboi Y et al (2010) Case-control study of risk of Parkinson’s disease in relation to hypertension, hypercholesterolemia, and diabetes in Japan. J Neurol Sci 293(1–2):82–86
Parrott MD, Greenwood CE (2007) Dietary influences on cognitive function with aging: from high-fat diets to healthful eating. Ann N Y Acad Sci 1114:389–397
Matsuda M, Shimomura I (2013) Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes Res Clin Pract 7(5):e330–e341
Heinonen S, Buzkova J, Muniandy M, Kaksonen R, Ollikainen M, Ismail K, Hakkarainen A, Lundbom J et al (2015) Impaired mitochondrial biogenesis in adipose tissue in acquired obesity. Diabetes 64(9):3135–3145
Sandoval-Salazar C, Ramirez-Emiliano J, Trejo-Bahena A, Oviedo-Solis CI, Solis-Ortiz MS (2016) A high-fat diet decreases GABA concentration in the frontal cortex and hippocampus of rats. Biol Res 49:15–20
Loffler T, Flunkert S, Temmel M, Hutter-Paier B (2016) Decreased plasma abeta in hyperlipidemic APPSL transgenic mice is associated with BBB dysfunction. Front Neurosci 10:232
van de Haar HJ, Jansen JF, van Osch MJ, van Buchem MA, Muller M, Wong SM, Hofman PA, Burgmans S, Verhey FR, Backes WH (2016) Neurovascular unit impairment in early Alzheimer's disease measured with magnetic resonance imaging. Neurobiol Aging 45:190–196
Bleckwenn M, Kleineidam L, Wagner M, Jessen F, Weyerer S, Werle J, Scherer M (2017) Impact of coronary heart disease on cognitive decline in Alzheimer's disease: a prospective longitudinal cohort study in primary care. Br J Gen Pract 67(655):e111–e117. https://doi.org/10.3399/bjgp16X688813
Silbert BS, Scott DA, Evered LA, Lewis MS, Maruff PT (2007) Preexisting cognitive impairment in patients scheduled for elective coronary artery bypass graft surgery. Anesth Analg 104(5):1023–1028. tables of contents. https://doi.org/10.1213/01.ane.0000263285.03361.3a
Qiang F, Lee BJ, Lee W, Han HK (2009) Pharmacokinetic drug interaction between fexofenadine and fluvastatin mediated by organic anion-transporting polypeptides in rats. Eur J Pharm Sci 37(3–4):413–417
Cremonini AL, Caffa I, Cea M, Nencioni A, Odetti P, Monacelli F. (2019) Nutrients in the prevention of Alzheimer’s disease. Oxid Med Cell Longev 2019
Villalba JM, Parrado C, Santos-Gonzalez M, Alcain FJ (2010) Therapeutic use of coenzyme Q 10 and coenzyme Q 10 -related compounds and formulations. Expert Opin Investig Drugs 19(4):535–554
Johnson AR, Milner JJ, Makowski L (2012) The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev 249(1):218–238
Gow RV, Hibbeln JR (2014) Omega-3 fatty acid and nutrient deficits in adverse neurodevelopment and childhood behaviors. Child Adol Psych Clin 23(3):555–590. https://doi.org/10.1016/j.chc.2014.02.002
Innis SM (2008) Dietary omega 3 fatty acids and the developing brain. Brain Res 1237:35–43
Simopoulos AP (2008) The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood) 233(6):674–688
Brenna JT, Diau GY (2007) The influence of dietary docosahexaenoic acid and arachidonic acid on central nervous system polyunsaturated fatty acid composition, prostaglandins. Leukot Essent Fatty Acids 77:247–250
Agrawal R, Gomez-Pinilla F (2012) ‘Metabolic syndrome’ in the brain: deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signaling and cognition. J Physiol 590(Pt 10):2485–2499
Moreira JD, Knorr L, Ganzella M et al (2010) Omega-3 fatty acids deprivation affects ontogeny of glutamatergic synapses in rats: relevance for behavior alterations. Neurochem Int 56(6–7):753–759
Akbar M, Calderon F, Wen Z, Kim HY (2005) Docosahexaenoic acid: a positive modulator of Akt signaling in neuronal survival. Proc Natl Acad Sci USA 102(31):10858–10863
Bookstaver D, Nancy P, Pharm B, Hatzigeorgiou C (2012) Effect of Coenzyme Q10 supplementation on statin-Induced myalgias. Am J Cardiol 110:526–529
Bentinger M, Brismar K, Dallner G (2007) The antioxidant role of coenzyme Q. Mitochondrion S7:S41–S50
Wyman M, Leonard M, Morledge T (2010) Coenzyme Q10: a therapy for hypertension and statin-induced myalgia? Cleve Clin J Med 77:435–442
Ernster L, Dallner G (1995) Biochemical, physiological and medical aspects of ubiquinone function. Biochim Biophys Acta 1271(1):195–204
Adaramoye O, Akinatyo O, Achen J, Michel A (2008) Lipid lowering effects of methanolic extracts of Vernonia anygdalina leaves in rats fed on high cholesterol diet. Vasc Health Risk Manag 4(1):235–241
Lakhwani LALIT, Tongia SK, Pal VS, Agrawal RP, Nyati PREM, Phadnis PRADEEP (2007) Omega-3 fatty acids have antidepressant activity in forced swimming test in Wistar rats. Acta Pol Pharm 64(3):271–276
Coldiron AD, Sanders RA, Watkins JB (2002) Effects of combined quercetin and coenzyme Q(10) treatment on oxidative stress in normal and diabetic rats. J Biochem Mol Toxicol 16:197–202
Porsolt RD, Bertin A, Jalfre M (1978) Behavioural despair in rats and mice: strain differences and the effects of imipramine. Eur J Pharmacol 51:291–294
Deacon RMJ, Rawlins JNP (2006) T-maze alternation in the rodent. Nat Protoc 1:7–12. https://doi.org/10.1038/nprot
Ohkawa H et al (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358
Beutler E, Duron O, Kelly BM (1963) An improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Montgomery HAC, Dymock JF (1961) The determination of nitrate in water. Analyst 86:414–416
Habig WH, Pabst MJ, Jakoby WB (1974) Glutathione S-transferases the first enzymatic step in mercapturic acid formation. J Bio Chem 249(22):7130–7139
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clinic Med 70(1):158–169
Selkoe DJ (1994) Normal and abnormal biology of the beta-amyloid precursor protein. Ann Rev Neurosc 17(1):489–517
Banchroft TDJD, Stevens A (1996) Theory and practice of histological techniques, 4th edn. Churchil Livingstone, New York
Loera-Valencia R, Goikolea J, Parrado-Fernandez C, Merino-Serrais P, Maioli S (2019) Alterations in cholesterol metabolism as a risk factor for developing Alzheimer's disease: potential novel targets for treatment. J Steroid Biochem.
Freeman LR, Zhang L, Nair A, Dasuri K, Francis J, Fernandez-Kim SO, Bruce-Keller AJ, Keller JN (2013) Obesity increases cerebrocortical reactive oxygen species and impairs brain function. Free Radic Biol Med 56:226–233
Greenwood CE, Winocur G (1996) Cognitive impairment in rats fed high-fat diets: a specific effect of saturated fatty-acid intake. Behav Neurosci 110(3):451–459
Abbasnejad Z, Nasseri B, Zardooz H, Ghasemi R (2019) Time-course study of high fat diet induced alterations in spatial memory, hippocampal JNK, P38, ERK and Akt activity. Metab brain dis 34(2):659–673
Lavin DN, Joesting JJ, Chiu GS, Moon ML, Meng J, Dilger RN, Freund GG (2011) Fasting induces an anti-inflammatory effect on the neuroimmune system which a high-fat diet prevents. Obesity (Silver Spring) 19(8):1586–1594
Nguyen JC, Ali SF, Kosari S, Woodman OL, Spencer SJ, Killcross AS et al (2017) Western diet chow consumption in rats induces striatal neuronal activation while reducing dopamine levels without affecting spatial memory in the radial arm maze. Front Behav Neurosci 11:22
Singh M, Kaur M, Kukreja H, Chugh R, Silakari O, Singh D (2013) Acetylcholinesterase inhibitors as Alzheimer therapy: from nerve toxins to neuroprotection. Eur J Med Chem 70:165–188. https://doi.org/10.1016/j.ejmech.2013.09.050
Singla N, Dhawan DK (2012) Regulatory role of zinc during aluminium-induced altered carbohydrate metabolism in rat brain. J Neurosci Res 90:698–705. https://doi.org/10.1002/jnr.22790
Valladolid-Acebes I, Merino B, Principato A, Fole A, Barbas C, Lorenzo MP et al (2012) High-fat diets induce changes in hippocampal glutamate metabolism and neurotransmission. Am J Physiol Endocrinol Metab 302(4):E396–402
Ferraz AC, Delattre AM, Almendra RG, Sonagli M, Borges C, Araujo P, Andersen ML, Tufik S, Lima MM (2011) Chronic omega-3 fatty acids supplementation promotes beneficial effects on anxiety, cognitive and depressive-like behaviors in rats subjected to a restraint stress protocol. Behav Brain Res 219:116–122
Park Y, Moon HJ, Kim SH (2012) N-3 polyunsaturated fatty acid consumption produces neurobiological effects associated with prevention of depression in rats after the forced swimming test. J Nutr Biochem 23:924–928
Jackson C, Barrett DW, Shumake J, Gonzales E, Gonzalez-Lima F, Lane MA (2018) Maternal omega-3 fatty acid intake during neurodevelopment does not affect pup behavior related to depression, novelty, or learning. BMC Res Notes 11(1):812
Aboul-Fotouh S (2013) Coenzyme Q10 displays antidepressant-like activity with reduction of hippocampal oxidative/nitrosative DNA damage in chronically stressed rats. Pharmacol Biochem Behav 104:105–112
Ashkani-Esfahani S, Bagheri F, Emami Y, Esmaeilzadeh E, Azarpira N, Hassanabadi N, Noorafshan A (2016) Protective effects of co-enzyme Q10 on thioacetamide-induced acute liver damage and its correlation with behavioral, biochemical, and pathological factors. Iran Red Crescent Med J 18(8)
Minami M, Kimura S, Endo T, Hamaue N, Hirafuji M, Togashi H et al (1997) Dietary docosahexaenoic acid increases cerebral acetylcholine levels and improves passive avoidance performance in stroke-prone spontaneously hypertensive rats. Pharmacol Biochem Behav 58(4):1123–1129
Choi H, Park HH, Koh SH, Choi NY, Yu HJ, Park J et al (2012) Coenzyme Q10 protects against amyloid β-induced neuronal cell death by inhibiting oxidative stress and activating the P13K pathway. Neurotox 33:85–90. https://doi.org/10.1016/j.neuro.2011.12.005
Young AJ, Johnson S, Steffens DC, Doraiswamy PM (2007) Coenzyme Q10: a review of its promise as a neuroprotectant. CNS Spectr 12:62–68
Abdin A, Hamouda H (2008) Mechanism of the neuroprotective role of coenzyme Q10 with or without L-dopa in rotenone-induced parkinsonism. Neuropharmacol 55:1340–1346
de Mello AH, Gassenferth A, de Bona Schraiber R, da Rosa Souza L, Florentino D, Danielski LG, et al (2014) Effects of omega-3 on behavioral and biochemical parameters in rats submitted to chronic mild stress. Metab Brain Dis 29(3):691–699
Freeman LR, Haley-Zitlin V, Rosenberger DS, Granholm AC (2014) Damaging effects of a high-fat diet to the brain and cognition: a review of proposed mechanisms. Nutr Neurosci 17(6):241–251
Ma W, Yuan L, Yu H, Xi Y, Xiao R (2014) Mitochondrial dysfunction and oxidative damage in the brain of diet-induced obese rats but not in diet-resistant rats. Life Sci 110(2):53–60
Otunola GA, Oloyede OB, Oladiji AT, Afolayan J (2014) Selected spices and their combination modulate hypercholesterolemia-induced oxidative stress in experimental rats. Bio Res 47(1):5
Federico A, Cardaioli E, Da Pozzo P, Formichi P, Gallus GN, Radi E (2012) Mitochondria, oxidative stress and neurodegeneration. J Neurol Sci 322(1–2):254–262
Williams TI, Lynn BC, Markesbery WR, Lovell MA (2006) Increased levels of 4-hydroxynonenal and acrolein, neurotoxic markers of lipid peroxidation, in the brain in Mild Cognitive Impairment and early Alzheimer's disease. Neurobiol Aging 27(8):1094–1099
Gawryluk JW, Wang JF, Andreazza AC, Shao L, Young LT (2011) Decreased levels of glutathione, the major brain antioxidant, in post-mortem prefrontal cortex from patients with psychiatric disorders. Int J Neuropsychopharmacol 14(1):123–130
Dominguez C, Ruiz E, Gussinye M, Carrascosa A (1998) Oxidative stress at onset and in early stages of type 1 diabetes in children and adolescents. Diabetes Care 21(10):1736–1742
Shrag M, Mueller C, Zabel M, Crofton A, Kirsch WM, Ghribi O (2013) Oxidative stress in blood in Alzheimer's disease and mild cognitive impairment: a meta-analysis. Neurobiol Aging 59:100–110
Kawashima S, Yokoyama M (2004) Dysfunction of endothelial nitric oxide synthase and atherosclerosis. Arteriosc Thromb Vasc Bio 24(6):998–1005
Garry PS, Ezra M, Rowland MJ, Westbrook J, Pattinson KTS (2015) The role of the nitric oxide pathway in brain injury and its treatment—from bench to bedside. Exp neuro 263:235–243
Hossain MS, Hashimoto M, Gamoh S, Masumura S (1999) Antioxidative effects of docosahexaenoic acid in the cerebrum versus cerebellum and brainstem of aged hypercholesterolemic rats. J Neurochem 72(3):1133–1138
Stanley WC, Khairallah RJ, Dabkowski ER (2012) Update on lipids and mitochondrial function: impact of dietary n-3 polyunsaturated fatty acids. Curr Opin Clin Nutr Metab Care 15:122–126
Green P, Glozman S, Yavin E (2001) Ethyl docosahexaenoate-associated decrease in fetal brain lipid peroxide production is mediated by activation of prostanoid and nitric oxide pathways. Biochim Biophys Acta 1531(1–2):156–164
de Mello AH, de Bona SR, de Souza Goldim MP, Garcez ML, Gomes ML, de Bem SG et al (2019) Omega-3 fatty acids attenuate brain alterations in high-fat diet-induced obesity model. Molecular neurobiology 56(1):513–524
Crane FL (2001) Biochemical functions of coenzyme Q10. J Am Coll Nutr 20:591–598
Wadsworth TL, Bishop JA, Pappu AS, Woltjer RL, Quinn JF (2010) Evaluation of coenzyme Q as an antioxidant strategy for Alzheimer’s disease. J Alzheimers Dis 14:225–234
Hargreaves I (2014) Coenzyme Q 10 as a therapy for mitochondrial disease. Int J Biochem Cell Biol 49:105–111. https://doi.org/10.1016/j.biocel.2014.01.020
Oguntibeju OO (2019) Type 2 diabetes mellitus, oxidative stress and inflammation: examining the links. IJPPP 11(3):45
Cao XL, Du J, Zhang Y, Yan JT, Hu XM (2015) Hyperlipidemia exacerbates cerebral injury through oxidative stress, inflammation and neuronal apoptosis in MCAO/reperfusion rats. Exp Brain Res 233(10):2753–2765
Walker JM, Dixit S, Saulsberry AC, May JM, Harrison FE (2017) Reversal of high fat diet-induced obesity improves glucose tolerance, inflammatory response, β-amyloid accumulation, and cognitive decline in the APP/PSEN1 mouse model of Alzheimer's disease. Neurobiol Dis 100:87–98
Puig KL, Floden AM, Adhikari R, Golovko MY, Combs CK (2012) Amyloid precursor protein and proinflammatory changes are regulated in brain and adipose tissue in a murine model of high fat diet-induced obesity. PLoS ONE 7(1):e30378
de Lima Oliveira BC, Bellozi PMQ, Reis HJ, de Oliveira ACP (2018) Inflammation as a possible link between dyslipidemia and Alzheimer’s Disease. Neuroscience 376:127–141
Lorente-Cebrián S, Costa AG, Navas-Carretero S, Zabala M, Laiglesia LM, Martínez JA et al (2015) An update on the role of omega-3 fatty acids on inflammatory and degenerative diseases. J Physiol Biochem 71(2):341–349
Yates CM, Calder PC, Rainger G (2014) Pharmacology and therapeutics of omega-3 polyunsaturated fatty acids in chronic inflammatory disease. Pharmacol Ther 141(3):272–282
Yan L, Xie Y, Satyanarayanan SK, Zeng H, Liu Q, Huang M, et al (2019) Omega-3 polyunsaturated fatty acids promote brain-to-blood clearance of β-Amyloid in a mouse model with Alzheimer’s disease. Brain Behav Immun
Sanoobar M, Eghtesadi S, Azimi A, Mohammad K (2013) Coenzyme Q10 supplementtion reduces oxidative stress and increases antioxidant enzyme activity in patients with relapsing–remitting multiple sclerosis. Int J Neurosci 123:776–782
de Oliveira FE, Fernandes MYSD, de Lima NMR, Neves KRT, do Carmo MRS, Lima FAV et al (2016) Neuroinflammatory response to experimental stroke is inhibited by eriodictyol. Behav Brain Res 312:321–332
Park SH, Kim JH, Choi KH, Jang YJ, Bae SS, Choi BT, Shin HK (2013) Hypercholesterolemia accelerates amyloid beta-induced cognitive deficits. Int J Mol Med 31:577–582
Maesako M, Uemura M, Tashiro Y, Sasaki K, Watanabe K, Noda Y, Ueda K, Asada-Utsugi M (2015) High fat diet enhances beta-site cleavage of amyloid precursor protein (APP) via promoting beta-site APP cleaving enzyme 1/adaptor protein 2/clathrin complex formation. PLoS ONE 10(9):e0131199
Graham LC, Harder JM, Soto I, de Vries WN, John SW, Howell GR et al (2016) Chronic consumption of a western diet induces robust glial activation in aging mice and in a mouse model of Alzheimer's disease. Sci Report 6:21568
Green KN, Martinez-Coria H, Khashwji H, Hall EB, Yurko-Mauro KA, Ellis L et al (2007) Dietary docosahexaenoic acid and docosapentaenoic acid ameliorate amyloid-beta and tau pathology via a mechanism involving presenilin 1 levels. J Neurosci 27(16):4385–4395
Eckert GP, Chang S, Eckmann J, Copanaki E, Hagl S, Hener U et al (2011) Liposome-incorporated DHA increases neuronal survival by enhancing non-amyloidogenic APP processing. Biochim Biophys Acta 1808(1):236–243
Dumont M, Kipiani K, Yu F, Wille E, Katz M, Calingasan NY et al (2011) Coenzyme Q10 decreases amyloid pathology and improves behavior in a transgenic mouse model of Alzheimer's disease. J Alzheimers Dis 27(1):211–223
Yang X, Yang Y, Li G, Wang J, Yang ES (2008) Coenzyme Q10 attenuates beta-amyloid pathology in the aged transgenic mice with Alzheimer presenilin 1 mutation. J Mol Neurosci 34(2):165–171
Segarra AB, Ruiz-Sanz JI, Ruiz-Larrea MB et al (2011) The profile of fatty acids in frontal cortex of rats depends on the type of fat used in the diet and correlates with neuropeptidase activities. Horm Metab Res 43(2):86–91
Monsef A, Shahidi S, Komaki A (2019) Influence of chronic coenzyme Q10 supplementation on cognitive function, learning, and memory in healthy and diabetic middle-aged rats. Neuropsychobiology 77(2):92–100
Acknowledgements
The author would like to thank reviewers for their in-depth comments that improved the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there are no competing interests.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the Ethical Committee of the NRC under approval number: 19–105.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ibrahim Fouad, G. Combination of Omega 3 and Coenzyme Q10 Exerts Neuroprotective Potential Against Hypercholesterolemia-Induced Alzheimer's-Like Disease in Rats. Neurochem Res 45, 1142–1155 (2020). https://doi.org/10.1007/s11064-020-02996-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-02996-2