Abstract
Chemotherapy has always been one of the most effective ways in combating human glioma. However, the high metastatic potential and resistance toward standard chemotherapy severely hindered the chemotherapy outcomes. Hence, searching effective chemotherapy drugs and clarifying its mechanism are of great significance. Salinomycin an antibiotic shows novel anticancer potential against several human tumors, including human glioma, but its mechanism against human glioma cells has not been fully elucidated. In the present study, we demonstrated that salinomycin treatment time- and dose-dependently inhibited U251 and U87 cells growth. Mechanically, salinomycin-induced cell growth inhibition against human glioma was mainly achieved by induction of G1-phase arrest via triggering reactive oxide species (ROS)-mediated DNA damage, as convinced by the activation of histone, p53, p21 and p27. Furthermore, inhibition of ROS accumulation effectively attenuated salinomycin-induced DNA damage and G1 cell cycle arrest, and eventually reversed salinomycin-induced cytotoxicity. Importantly, salinomycin treatment also significantly inhibited the U251 tumor xenograft growth in vivo through triggering DNA damage-mediated cell cycle arrest with involvement of inhibiting cell proliferation and angiogenesis. The results above validated the potential of salinomycin-based chemotherapy against human glioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioma is the most frequent brain tumor which accounts for about half of all intracranial primary tumors. The average survival time of malignant glioma sufferers is approximately 16 months due to its high malignant degree. Patients with glioma carry poor prognosis, and only 20–30% patients could survive 5 years [1–3]. Although the surgical treatment and postoperative radiotherapy have achieved exciting success, chemotherapy still represents one of the most effective strategies in treating human glioma [4–7]. Hence, search of novel chemotherapy drugs against glioma is still urgent and significant.
Salinomycin has always been used as a veterinary antibiotic originally to prevent coccidiosis in poultry and to improve nutrient absorption in ruminants [8–10]. Gupta et al. firstly found that salinomycin could selectively kill breast cancer stem cells [11]. Recently, increasing studies revealed that salinomycin had the potential to inhibit the growth of various cancer cells, such as pancreatic cancer [12], ovarian cancer [13], gastric cancer [14], breast cancer [15], fibrosarcoma [16] and glioma [17–19]. Several mechanisms were involved in salinomycin mediated-anticancer effects, such as inhibition of Wnt signaling [20], anti-angiogenesis [21], apoptosis [22], autophagy [23] and induction of oxidative stress [24]. However, the underlying mechanism of salinomycin against human tumors remains unclear. Particularly, as yet, salinomycin-mediated cell cycle arrest has not been reported. Hence, the anticancer effect of salinomycin on human glioma was evaluated and the mechanism was investigated in the present study.
Materials and Methods
Reagents
Salinomycin, MTT, propidium iodide (PI), DCFH-DA probes were purchased from Sigma. DMEM, FBS, Parenzyme and penicillin–streptomycin were bought from Gibco. Any antibodies used for Western blotting and immunohistochemistry staining were purchased from Abcam company (Abcam, United Kingdom). The water mentioned in this study was produced by a Milli-Q water purification system (Millipore, USA). The grade of all solvents is high-performance liquid chromatography (HPLC).
Cell Culture
U87 and U251 cells were cultivated in conventional DMEM medium which supplemented with 1% penicillin/streptomycin and 10% fetal bovine serum (FBS) at 37 °C in 5% CO2. The cell growth situation was observed daily and the medium was changed twice a week.
Cell Viability
Cell viability was evaluated via MTT method. In brief, 6 × 103 cells were seeded per well in 96-well plate and pre-incubated for 24 h for adhere. Then cells were treated with salinomycin at various concentrations (0, 2, 4 and 8 μM) for 24 and 48 h. Cis-platinum, an anticancer drug widely used in clinic, was employed as the positive control. After treatment, 20 μl of MTT (5 mg/ml) was added into every well and incubated for 5 h in dark at 37 °C. Then, DMSO (150 μl/well) was added and the microplate reader (Molecular Devices, USA) was used to measure the intensity of the solvent at 570 nm. The value of each treatment group was expressed as a percentage change of control group which represents the viability of the U251 and U87 cells (as 100%).
Cell Apoptosis and Cell Cycle Distribution
Cell apoptosis and cell cycle distribution were analyzed by flow cytometry. In short, U251 cells (3 × 105 cells) were seeded in 6-well plate. Subsequently, cells were exposed to salinomycin for 48 h. Then cells were harvested, washed by PBS, fixed with chilled 70% ethanol for 12 h at night. Cells after staining with propidium iodide (PI), flow cytometry was employed to examine the apoptosis and cell cycle arrest. The cell cycle distribution (G0/G1, S and G2/M phase) was analyzed by Multi-Cycle Software.
Evaluation of Oxidative Status
Intracellular oxidative status was evaluated by examination of ROS, superoxide anion and 8-OH-deoxyguanosine (8-OHdG). ROS and superoxide anion were evaluated by DCFH-DA and Mit-SOX probe, respectively. Briefly, U251 cells were pre-incubated with 10 μM DCFH-DA probe for 15 min at 37 °C in darkness, and then cells were washed, seeded in 96-well plate (107 cells/well), and exposed to 4 μM salinomycin. The ROS generation was examined with the excitation and emission wavelength at 488 and 525 nm, respectively. Furthermore, the ROS and superoxide anion were also vividly observed by microscope. Briefly, cells seeded in 6-well plates were pre-loaded with 10 μM DCFH-DA or 10 μM MitoSOX probe for 15 min at 37 °C. Then the cells were washed with PBS and treated with 4 μM salinomycin. Then the real-time intracellular ROS (green fluorescence) and superoxide anion (red fluorescence) were vividly imaged with an inverted fluorescence microscope (magnification, ×200). The intracellular 8-OHdG was examined by an 8-OHdG ELISA Kit according to the description before [25]. Briefly, cells after treatment with salinomycin for 48 h, cells were collected and total protein was separated for quantification. Then the 8-OHdG was examined by an ELISA method, and the data was expressed as μg/g protein.
Western Blotting Analysis
Cells after treatment with salinomycin for 48 h were collected, and lysed in lysis buffer on the ice. Then the lysate was collected and centrifuged (12,000 rpm, 4 °C) and quantified by BCA kit as reported previously [26]. After denaturation, equal quantities of proteins were subjected to 10% SDS polycrylamide gel, and then electrophoretically transferred onto a polyvinylidenefluoride (PVDF) membrane. Following blocking in TBST buffer containing 5% non-fat milk for 2 h, the membranes were incubated with primary antibodies (1:1000, 4 °C, overnight) and secondary antibodies (1:2000, room temperature, 2 h) antibodies. Proteins detection was performed based on enhanced chemiluminescence reagents (Chemi Doc MP, Bio-Rad). β-actin plays the role as an internal control.
In Vivo Study
Male nude mice were get acclimated for 1 week, and 107 U251 human glioma cells (in 100 μl PBS) were subcutaneously injected into the right oxter of mice. After 7-day growth, mice were randomized into three groups (n = 10/each group): vehicle control (100 μl PBS), and two SAL-treated groups (SAL, 5 and 10 mg/kg). SAL was injected from the caudal vein every other day for 2 weeks (8 times). The tumor volume was measured 3 times per week. After experiments, tumors were harvested and measured with the formula: volume = l × w2/2, with l being the maximal length and w being the width. Sections of tumors were used for western blotting and immunohistochemical (IHC) assay. All animal experiments were approved by the Animal Experimentation Ethics Committee of Shandong in China.
Statistical Analysis
All experiments were performed at least three times. Data were expressed as mean ± SD. Statistical analysis performed using Student’s t test. The difference among three or more groups was analyzed by one-way analysis of variance with multiple comparisons, and the bars with different letters imply statistically significant differences (P < 0.05). “*” or “**” were considered statistically significant P < 0.05 and P < 0.01, respectively.
Results
Salinomycin Inhibits Human Glioma Cell Growth
Initially, cell viability was evaluated using MTT method in cultured U87 and U251 cells. As shown in Fig. 1a, b, salinomycin (1, 2, 4, and 8 μM) treatment prominently inhibited U87 and U251 cells growth time- and dose-dependently. For instance, U251 cells exposed to 4 and 8 μM salinomycin for 48 h showed significant cell growth inhibition by 39.4 and 44.7%, respectively. Moreover, salinomycin treatment at 4 μM showed better growth suppressive effect than that of cis-platinum at 8 μM (Fig. 1a, b). The morphological changes of U251 cells, such as the cell shrinking and decrease in cell number, further confirmed this effect (Fig. 1c). In view of that U251 cells showed more sensibility to salinomycin than that of U87 cells, hence, U251 cells was selected for further mechanism evaluation.
Salinomycin inhibits human glioma cell growth. U87 (a) and U251 (b) cells (6000 cells/well) were seeded in 96-well plate, and cells were exposed to salinomycin at different concentration (0, 1, 2, 4, 8 µM) for 24 and 48 h. Cisplatin (8 µM) was used as the positive control. Cell viability was detected via MTT. c Phase contrast. The morphological change of U251 cells was observed by phase contrast microscope (magnification, ×200). All experiments were repeated at least three times. Bars with “*” or “**” represent significant difference at P < 0.05 or P < 0.01, respectively
Salinomycin Induces G1 Cell Cycle Arrest in U251 Cells
In order to determine whether apoptosis or/and cell cycle arrest was involved in salinomycin-induced cell growth inhibition against human glioma, flow cytometry was used to analyze its action model. As shown in Fig. 2a, after exposure to various concentrations of salinomycin for 48 h, salinomycin effectively initiated G1 phase cell cycle arrest in the U251 cells with a dose-dependent manner. For instance, U251 cells exposed to salinomycin (2, 4 and 8 μM) showed marked increase in G1 phase percentage from 44.2% (control) to 61.4, 73.2 and 76.6%, respectively. To further explore the G1 phase cell cycle arrest induced by salinomycin, cyclin D1, a pivotal modulator associated with cell cycle regulation, was analyzed by western blotting assay. The results suggested that the expression level of cyclin D1 was down-regulated by treatment with salinomycin in time- and dose-dependent manner (Fig. 2b, c). These results clearly indicated that induction of G1 phase cell cycle arrest mainly contributed to salinomycin-mediated anticancer mechanism.
Salinomycin induces G1 cell cycle arrest in U251 cells. a Cell cycle distribution. U251 cells after exposure to salinomycin (1–8 μM) for 48 h were collected, washed with PBS, fixed by 70% alcohol overnight, and stained by PI solution. Then cell cycle distribution was analyzed by flow cytometry. The dose- (b) and time-dependent (c) effects of salinomycin on cyclin D1. The protein expression was examined by western blotting
Salinomycin Causes DNA Damage Via Inducing ROS Generation
DNA damage plays a crucial role in anti-cancer therapy [27]. In order to examine the role of DNA damage in salinomycin-induced anticancer effects, several DNA damage markers (Ser139-H2A, Ser15-p53, p21 and p27) were all detected by western blotting. As shown in Fig. 3a, treatment with different concentrations salinomycin significantly increased the expression level of those proteins in a dose-dependent manner. For further evaluation salinomycin-induced DNA damage, we examined ROS generation which may cause DNA damage and induce cancer cells apoptosis [26, 28, 29]. As shown in Fig. 3b, U251 cells treated salinomycin only for 2 h showed obvious intracellular ROS accumulation with a time-dependent manner (Fig. 3b). The immunofluorescent staining of intracellular ROS and superoxide anion further vividly confirmed this tendency (Fig. 3d). Moreover, 8-OHdG, a marker of oxidative damage, was also observed in salinomycin-treated U251 cells (Fig. 3c). These data distinctly demonstrated that salinomycin causes DNA damage via inducing ROS generation.
Salinomycin causes DNA damage via inducing ROS generation. a Effects of salinomycin on DNA damage axis. U251 cells were treated with salinomycin for 48 h, and the expression of Ser139-H2A, Ser15-p53, p21, and p27 was analyzed by western blotting. b Salinomycin induces ROS accumulation. Cells were treated with 4 µM salinomycin for 0–120 min, and the ROS generation was measured by DCFH-DA probe as described in section of methods. c Examination of 8-OHdG. The experimental detail was processed as described in section of method. d Real-time imaging of ROS and superoxide anion. Cells were pre-loaded with DCFH-DA or Mito-SOX probe for 15 min, and then cells were washed and incubated with 4 µM salinomycin. Then the ROS or superoxide anion generation within 2 h was vividly observed by fluorescence microscope (magnification, ×200). Bars with “*” or “**” represent significant difference at P < 0.05 or P < 0.01, respectively
Inhibition of ROS Suppresses Salinomycin-Induced DNA Damage and G1 Cell Cycle Arrest
To further characterize the significance of ROS, we employed ROS inhibitor (glutathione, GSH) to evaluate the role of ROS in salinomycin-induced DNA damage and cell cycle arrest. As shown in Fig. 4a, GSH addition effectively attenuated salinomycin-induced DNA damage, as convinced by the decrease expression of Ser139-H2A, Ser15-p53, p21 and p27. As expected, ROS inhibition eventually blocked U251 cells from salinomycin-induced cell killing through attenuation of G1 cell cycle arrest. These data fully proved that salinomycin inhibited human glioma cell growth by initiating G1-phase cell cycle arrest through triggering ROS-mediated DNA damage.
Inhibition of ROS suppresses salinomycin-induced DNA damage and G1 cell cycle arrest. a Inhibition of ROS blocked salinomycin-induced DNA damage. U251 cells were pre-treated with 2 mM GSH for 2 h prior to salinomycin treatment. b Inhibition of ROS attenuated salinomycin-induced cytotoxicity in U251 cells. U251 cells were pre-treated with 2 mM GSH for 2 h prior to salinomycin treatment, and cell viability was assayed by MTT method. c GSH addition repressed salinomycin-induced G1 cell cycle arrest. U251 cells were pre-treated with 2 mM GSH for 2 h prior to salinomycin treatment, and the cell cycle distribution was analyzed by flow cytometry. All experiments were done at least triple. Bars with different letters indicate the statistical significance (P < 0.05)
Salinomycin Inhibits U251 Tumor Xenograft Growth In Vivo
The in vivo growth inhibitory effect of salinomycin on U251 tumor xenograft growth was also evaluated. As shown in Fig. 5, salinomycin treatment effectively inhibited the U251 glioma xenograft tumor volume (Fig. 5a) and weight (Fig. 5b). The mice body weight showed no significant change (data not shown). The immunostaining results showed that salinomycin could suppress the U251 cells proliferation (Ki-67 staining) and angiogenesis (CD-31 and VEGF staining) in vivo. The western blotting studies in vivo further revealed that salinomycin activated Ser15-p53 and Ser139-H2A, and decreased cyclin D1 and CD-31 expression, which were consistent with the mechanism in vitro. These results confirmed that salinomycin inhibited human glioma growth in vivo through triggering DNA damage-mediated cell cycle arrest, which further validated the potential application of salinomycin in therapy of human glioma.
Salinomycin inhibits the glioma growth in vivo. Salinomycin inhibits tumor volume (a) and tumor weight (b) of U251 human glioma xenografts in nude mice. c Effects of SAL on cyclin D1, Ser139-H2A and Ser15-p53 in vivo. The protein expression in vivo was detected by western blotting method. d SAL inhibited the cell proliferation and angiogenesis in vivo. The Ki-67, VEGF and CD-31 expression in vivo were examined by IHC method. All experiments were done at least three times. Bars with different letters represent statistically difference at P < 0.05
Discussion
Accumulated studies have revealed that salinomycin displayed novel growth inhibition activities against human various cancer cells in vitro and in vivo, including human glioma cells [14–18]. Several researchers has been aware of the significance of ROS in salinomycin-mediated anticancer effects [17, 30]. Qin et al. had discovered that salinomycin could induce programmed necrosis via ROS-p53-cyclophilin-D signaling in human glioma cells [19]. However, the underlying mechanisms of salinomycin on human glioma cells remain unclear. Especially, salinomycin-induced cell cycle arrest has not been reported. Herein, in the current study, the anticancer effect of salinomycin on human glioma was examined, and the mechanism was evaluated.
Induction of cell cycle arrest has been commonly proved to be involved in cancer chemotherapy. Growing evidences reported that lots of novel agents had the potential to inhibit cancer cells growth by triggering cell cycle arrest. For instance, indole-3-carbinol (I3C) could induce G1-phase cell cycle arrest in prostate cancer cells [31]. Metformin also exhibited properities in inhibiting breast cancer cell growth by induction of cell cycle arrest [32]. Multiple factors, such as cyclins, cyclin-dependent kinases (CDKs) and cyclin-dependent kinase inhibitors (CDKIs), were all involved in cell cycle regulation. The G1/S transition which gets involved in external stimuli, DNA replication and mitosis maintains the genomic integrity. Cyclin D1 as an important regulator of cell cycle protein dependent kinase CDKs plays key role in regulating the cell cycle transition from G1 to S phase [33]. In the present study, salinomycin induced obvious G1-phase cell cycle arrest with involvement of cyclin D1 inhibition dose- and time-dependent in human glioma cells. Our results validated the possibility that salinomycin had the potential to inhibit human glioma by hunting cell cycle progression.
It is reported that a variety of anti-tumor agents widely used in clinical inhibited cancer cells growth dependent ROS overproduction. Excess of intracellular ROS may lead to changes of certain intracellular protein kinase activity, subsequently stimulate a series of phosphorylation and dephosphorylation reactions signaling processes, which plays an important role in the process of cancer cell apoptosis induced by chemotherapy drugs. For instance, the anticancer drugs doxorubicin, cisplatin and taxol all inhibited human cancer cells growth by induction of ROS production, thereby caused oxidative damage on DNA and eventually leaded to cell apoptosis [34–36]. Many studies have reported that salinomycin could induce ROS accumulation in inhibition of human cancers, and salinomycin even act as chemo-sensitizer to enhance the efficacy of doxorubicin and etoposide for human breast cancer cell line MCF7 and Hs578T through triggering DNA damage [37]. In the present study, salinomycin caused notable ROS overproduction and subsequently induced DNA damage. Interestingly, GSH, a robust free radical scavenger, effectively attenuated salinomycin-induced DNA damage, cell survival and reversed salinomycin-induced cell cycle arrest. These finding clearly demonstrated that ROS generation acted as up-stream mediator for DNA damage and cell cycle arrest. Our finding provided the proof that ROS-mediated DNA damage was the main action model for illuminating salinomycin-induced cell killing against human glioma cells.
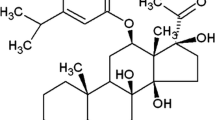
In summary, our finding revealed that salinomycin has the potential to inhibit human glioma cells growth by induction of G1 cell cycle arrest through triggering ROS-mediated DNA damage in vitro and in vivo (Fig. 6). Even though evidences convinced that salinomycin exhibited neurotoxic effects in vivo, studies also revealed that 5 mg/kg of salinomycin is tolerated in mice, and inhibition of Na+/Ca2+ exchangers can prevent salinomycin-induced neuropathy and meanwhile dose not impair its antineoplastic efficacy [38], which further validated its potential application in clinic for treatment of human glioma.
References
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507
Niu CS, Li DX, Liu YH, Fu XM, Tang SF, Li J (2011) Expression of NANOG in human gliomas and its relationship with undifferentiated glioma cells. Oncol Rer 26(3):593–601
Aghi MK, Nahed BV, Sloan AE, Ryken TC, Kalkanis SN, Olson JJ (2015) The role of surgery in the management of patients with diffuse low grade glioma: a systematic review and evidence-based clinical practice guideline. J Neurooncol 125:503–530
Ryken TC, Parney I, Buatti J, Kalkanis SN, Olson JJ (2015) The role of radiotherapy in the management of patients with diffuse low grade glioma: a systematic review and evidence-based clinical practice guideline. J Neurooncol 125:551–583
Tsao MN, Mehta MP, Whelan TJ, Morris DE, Hayman JA, Flickinger JC, Mills M, Rogers CL, Souhami L (2005) The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for malignant glioma. Int J Radiat Oncol Biol Phys 63:47–55
Bourkoula E, Mangoni D, Ius T, Pucer A, Isola M, Musiello D, Marzinotto S, Toffoletto B, Sorrentino M, Palma A (2014) Glioma-associated stem cells: a novel class of tumor-supporting cells able to predict prognosis of human low-grade gliomas. Stem Cells 32:1239–1253
Mitani M, Yamanishi T, Miyazaki Y (1975) Salinomycin: a new monovalent cation ionophore. Biochem Biophys Res Commun 66:1231–1236
Butaye P, Devriese LA, Haesebrouck F (2003) Antimicrobial growth promoters used in animal feed: effects of less well known antibiotics on gram-positive bacteria. Clin Microbiol Rev 16:175–188
Miyazaki Y, Shibuya M, Sugawara H, Kawaguchi O, Hirsoe C (1974) Salinomycin, a new polyether antibiotic. J Antibiot (Tokyo) 27:814–821
Gupta PB, Onder TT, Jiang G, Tao K, Kuperwasser C, Weinberg RA, Lander ES (2009) Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell 138:645–659
Schenk M, Aykut B, Teske C, Giese NA, Weitz J, Welsch T (2015) Salinomycin inhibits growth of pancreatic cancer and cancer cell migration by disruption of actin stress fiber integrity. Cancer Lett 358:161–169
Zhang B, Wang X, Cai F, Chen W, Loesch U, Bitzer J, Zhong XY (2012) Effects of salinomycin on human ovarian cancer cell line OV2008 are associated with modulating p38 MAPK. Tumour Biol 33:1855–1862
Zhi QM, Chen XH, Ji J, Zhang JN, Li JF, Cai Q, Liu BY, Gu QL, Zhu ZG, Yu YY (2011) Salinomycin can effectively kill ALDH(high) stem-like cells on gastric cancer. Biomed Pharmacother 65:509–515
Al DY, Attoub S, Arafat K, Abuqamar S, Eid A, Al FN, Iratni R (2013) Salinomycin induces apoptosis and senescence in breast cancer: upregulation of p21, downregulation of survivin and histone H3 and H4 hyperacetylation. Biochim Biophys Acta 1830:3121–3135
Yu SM, Kim SJ (2016) Salinomycin causes migration and invasion of human fibrosarcoma cells by inducing MMP-2 expression via PI3-kinase, ERK-1/2 and p38 kinase pathways. Int J Oncol 48:2686–2692
Xipell E, Gonzalez-Huarriz M, de Irujo JJ, Garcia-Garzon A, Lang FF, Jiang H, Fueyo J, Gomez-Manzano C, Alonso MM (2016) Salinomycin induced ROS results in abortive autophagy and leads to regulated necrosis in glioblastoma. Oncotarget 7:30626–30641
Chen T, Yi L, Li F, Hu R, Hu SL, Yin Y, Lan C, Li Z, Fu CH, Cao L, Chen Z, Xian JH, Feng H (2015) Salinomycin inhibits the tumor growth of glioma stem cells by selectively suppressing glioma-initiating cells. Mol Med Rep 11:2407–2412
Qin LS, Jia PF, Zhang ZQ, Zhang SM (2015) ROS-p53-cyclophilin-D signaling mediates salinomycin-induced glioma cell necrosis. J Exp Clin Cancer Res 34:57
Lu D, Carson DA (2011) Inhibition of Wnt signaling and cancer stem cells. Oncotarget 2:587
Li T, Liu X, Shen Q, Yang W, Huo Z, Liu Q, Jiao H, Chen J (2016) Salinomycin exerts anti-angiogenic and anti-tumorigenic activities by inhibiting vascular endothelial growth factor receptor 2-mediated angiogenesis. Oncotarget 7:26580–26592
Fuchs D, Heinold A, Opelz G, Daniel V, Naujokat C (2009) Salinomycin induces apoptosis and overcomes apoptosis resistance in human cancer cells. Biochem Biophys Res Commun 390:743–749
Jangamreddy JR, Ghavami S, Grabarek J, Kratz G, Wiechec E, Fredriksson BA, Rao PR, Cieslar-Pobuda A, Panigrahi S, Los MJ (2013) Salinomycin induces activation of autophagy, mitophagy and affects mitochondrial polarity: differences between primary and cancer cells. Biochim Biophys Acta 1833:2057–2069
Wang K, Fu XT, Li Y, Hou YJ, Yang MF, Sun JY, Yi SY, Fan CD, Fu XY, Zhai J, Sun BL (2016) Induction of S-phase arrest in human glioma cells by selenocystine, a natural selenium-containing agent via triggering reactive oxygen species-mediated DNA damage and modulating MAPKs and AKT pathways. Neurochem Res 41:1439–1447
Abudayyak M, Gurkaynak TA, Özhan G (2016) In vitro toxicological assessment of cobalt ferrite nanoparticles in several mammalian cell types. Biol Trace Elem Res. doi:10.1007/s12011-016-0803-3
Fu XY, Zhang S, Wang K, Yang MF, Fan CD, Sun BL (2015) Caudatin inhibits human glioma cells growth through triggering DNA damage-mediated cell cycle arrest. Cell Mol Neurobiol 35:953–959
Fan C, Zheng W, Fu X, Li X, Wong YS, Chen T (2014) Enhancement of auranofin-induced lung cancer cell apoptosis by selenocystine, a natural inhibitor of TrxR1 in vitro and in vivo. Cell Death Dis 5:e1191
Fan C, Zheng W, Fu X, Li X, Wong YS, Chen T (2014) Strategy to enhance the therapeutic effect of doxorubicin in human hepatocellular carcinoma by selenocystine, a synergistic agent that regulates the ROS-mediated signaling. Oncotarget 5:2853–2863
Zhu LZ, Hou YJ, Zhao M, Yang MF, Fu XT, Sun JY, Fu XY, Shao LR, Zhang HF, Fan CD, Gao HL, Sun BL (2016) Caudatin induces caspase-dependent apoptosis in human glioma cells with involvement of mitochondrial dysfunction and reactive oxygen species generation. Cell Mol Toxicol 32:333–345
Verdoodt B, Vogt M, Schmitz I, Liffers ST, Tannapfel A, Mirmohammadsadegh A (2012) Salinomycin induces autophagy in colon and breast cancer cells with concomitant generation of reactive oxygen species. PloS One 7:e44132
Chinni SR, Li Y, Upadhyay S, Koppolu PK, Sarkar FH (2001) Indole-3-carbinol (I3C) induced cell growth inhibition, G1 cell cycle arrest and apoptosis in prostate cancer cells. Oncogene 20:2927–2936
Alimova IN, Liu B, Fan Z, Edgerton SM, Dillon T, Lind SE, Thor AD (2009) Metformin inhibits breast cancer cell growth, colony formation and induces cell cycle arrest in vitro. Cell Cycle 8:909–915
Baldin V, Lukas J, Marcote MJ, Pagano M, Draetta G (1993) Cyclin D1 is a nuclear protein required for cell cycle progression in G1. Genes Dev 7:812–821
Tian HL, Yu T, Xu NN, Feng C, Zhou LY, Luo HW, Chang DC, Le XF, Luo KQ (2010) A novel compound modified from tanshinone inhibits tumor growth in vivo via activation of the intrinsic apoptotic pathway. Cancer Lett 297:18–30
Kim BM, Choi YJ, Lee YH, Joe YA, Hong SH (2010) N,N-dimethyl phytosphingosine sensitizes HL-60/MX2, a multidrug-resistant variant of HL-60 cells, to doxorubicin-induced cytotoxicity through ROS-mediated release of cytochrome c and AIF. Apoptosis 15:982–993
Bennett MR (2001) Reactive oxygen species and death: oxidative DNA damage in atherosclerosis. Circ Res 88:648–650
Kim JH, Chae M, Kim WK, Kim YJ, Kang HS, Kim HS, Yoon S (2011) Salinomycin sensitizes cancer cells to the effects of doxorubicin and etoposide treatment by increasing DNA damage and reducing p21 protein. Br J Pharmacol 162:773–784
Boehmerle W, Muenzfeld Hanna, Springer A, Huehnchen P, Endres M (2014) Specific targeting of neurotoxic side effects and pharmacological profile of the novel cancer stem cell drug salinomycin in mice. J Mol Med 92:889–900
Acknowledgements
The study was supported by Key Research and Development Program of Shandong No. 2016GSF202036 to C.-D. Fan and No. 2015GSF119023 to J. Zhai. Natural Science Foundation of Shandong No. ZR2015HL050 to D.-W. Li and ZR2011HL046 to J. Zhai.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest for all the authors.
Additional information
S.-J. Zhao and X.-J. Wang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhao, SJ., Wang, XJ., Wu, QJ. et al. Induction of G1 Cell Cycle Arrest in Human Glioma Cells by Salinomycin Through Triggering ROS-Mediated DNA Damage In Vitro and In Vivo. Neurochem Res 42, 997–1005 (2017). https://doi.org/10.1007/s11064-016-2132-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-016-2132-5









