Abstract
Hypoxia induces a cerebral inflammatory response, which contributes to brain injury. Inflammasomes are complex intracellular molecular structures that initiate the inflammatory cascade. Caspase-1 and interleukin 1-β (IL-1β), have been established as markers of inflammasome activation. Src kinase, a cytosolic non-receptor protein tyrosine kinase, is linked to cell proliferation and differentiation and is up regulated during hypoxia. The role of Src kinase in the above pathway is not fully understood. The present study tests the hypothesis that inhibition of Src kinase, by a selective inhibitor, PP2, will prevent the activation of caspase-1 and production of IL-1β acutely, as well as at 1 and 15 days after hypoxia in the cerebral cortex of the newborn piglet. Piglets were divided into: Normoxia (Nx), Hypoxia acute (Hx), Hypoxia-day 1 (Hx-day 1), and Hypoxia day 15 (Hx-day 15). Piglets pretreated with Src kinase inhibitor, PP2, 1 mg/kg IV, 30 min prior to hypoxia were divided into: Hypoxia acute (Hx + PP2), 1 day (Hx + PP2-day 1), and day 15 (Hx + PP2-day 15). Hypoxia was induced by exposing the piglets to an FiO2 of 0.07 for 1 hour. Caspase-1 activity and expression were determined with spectrophotometry and Western blot respectively, while IL-1β levels were measured by solid phase ELISA. Caspase-1 activation was achieved immediately (within 1 h) after hypoxia and persisted for 15 days. IL-1β level was also increased after hypoxia reaching a maximum level at 24 h following hypoxia and returned to baseline by 15 days. Administration of PP2 attenuated the activity acutely, but not the expression of the caspase-1. IL-1β level at 24 h after hypoxia returned to baseline in piglets that were pretreated with PP2. We provide evidence that inhibition of Src kinase in the acute phase after hypoxia involves changes in the production or processing of caspase-1 subunits. Our data suggest that Src kinase mediates hypoxia-induced caspase-1 activation in the cerebral cortex of newborn piglets. Inhibition of Src kinase may attenuate the neuroinflammatory response and could represent a potential target for neuroprotection after hypoxic injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxic-ischemic brain injury during the perinatal period is a major cause of mortality and severe neurologic morbidity in infants and children. Apoptosis is a well-established mechanism of programmed cell death following hypoxia. Hypoxia also induces a cerebral inflammatory response, which can further contribute to brain injury. In the central nervous system, both the resident immune cells (microglia) and the infiltrating macrophages play an important role in the inflammatory cascade by producing a variety of inflammatory mediators which result in changes in blood flow, capillary permeability and further recruitment of neutrophils and monocytes. A key mediator of neutrophil and monocyte recruitment is IL-1 [1]. IL-1 exists in two forms designated as IL-1α and IL-1β. Although these proteins are coded by different genes and share some homology, IL-1β is the major form of IL-1 and is involved in inflammation, while IL-1α is a non-secreted analog that does not participate in the inflammatory process [2].
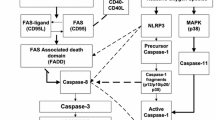
IL-1β production is achieved through the formation of complex intracellular structures, the inflammasomes, which usually are named after their specific intracellular receptor that can sense danger signals. These receptors are known as NOD-like receptors (NLRs). Although there are several different types of inflammasomes, their assembly follows a common pathway. Caspase-1 is the main inflammatory caspase associated with inflammasomes and IL-1β is the main target of caspase-1. When caspase-1 is blocked, IL-1β is released only in small amounts as an inactive, precursor form [3, 4]. Caspase-1 cleaves also the precursor of IL-18 to an active molecule. IL-1β and IL-18 share similar properties and structure and have been implicated in neuronal loss and neurodegeneration [5].
The Src family kinases are a family of non-receptor tyrosine kinases that consist of nine subtypes: Src, Yes, Fyn, Fgr, Yrk, Hck, Lck, Lyn, Blk [6]. Three of these members (Src, Fyn and Yes) are expressed extensively in all cell lines, including the central nervous system [7]. Experimental data support the role of Src kinase in numerous cellular functions including cell migration and invasion by regulating the formation of the actin rich “movement” structures called podosomes or invadosomes in macrophages and other cell types [8, 9]. Src kinases mediate neuronal differentiation [10] as well as ion channel regulation, with notable involvement in the activation of the NMDA receptor [11]. We have previously shown that hypoxia results in increased activity of Src kinase, in the brain of newborn piglets [12]. Src kinase mediates the increased tyrosine phosphorylation of caspase-9 and the related NLR (Apaf-1) [8, 13] as well as of caspase-8 [14], modulating the apoptotic cascade. Caspase-1 activation has been shown to increase after hypoxia in neurons [15, 16]. It is not clear though, whether hypoxia induced caspase-1 activation is mediated by Src kinase.
The aim of this study was to characterize the changes that occur in caspase-1 and IL-1 β after hypoxia in the acute phase, as well as over time at 1 and 15 days after hypoxia in the brain of term newborn piglets. We measured caspase-1 activity and expression as well as IL-1β expression as surrogate biological markers for the inflammasome activation. We hypothesized that hypoxia induced caspase-1 activation is mediated by Src kinase.
Results
Table 1 summarizes the baseline characteristics of the piglets in normoxic, hypoxic and the hypoxic pretreated with PP2 groups. Blood pressure, pH, partial pressure of oxygen and carbon dioxide before (pre) and after (post) the institution of hypoxia are presented. The blood pressure, pH and PaO2 were significantly decreased in the hypoxic groups as expected. Similar changes occurred also in piglets, during the reoxygenation (recovery) period. No significant side effects were recorded in animals treated with PP2.
Caspase-1 Activity
Caspase-1 activity (nmols/mg protein/hr, mean ± SD) was 0.74 ± 0.1 in Nx versus 1.2 ± 0.1 in Hx. In the recovery phase caspase-1 was 1.23 ± 0.1 in Hx-day 1, 1.14 ± 0.2 in Hx-day 15. Oxygen deprivation for 1 hour triggered an increase in caspase-1 activity which was maintained during the recovery phase (P < 0.05 vs. baseline) (Fig. 1). In piglets that were treated with PP2 and then subjected to hypoxia, caspase-1 activity was noted to be attenuated acutely (P < 0.05). In the reoxygenation phase administration of PP2 did not have any effect on caspase-1 activity as shown in Fig. 1 (P = NS). Specifically, the caspase-1 activity was 0.83 ± 0.2 in Hx + PP2, 0.98 ± 0.1 in Hx + PP2-day 1 and 1.08 ± 0.2 in Hx + PP2-day 15. In piglets that were pretreated with PP2 and remained under normoxic conditions (Nx*), caspase-1 activity was 0.83 ± 0.1 (P = NS vs. Nx, Hx + PP2, P < 0.05 vs. Hx). These data demonstrate that, by blocking Src kinase, caspase-1 activity was attenuated in the acute phase after hypoxia. This effect was not maintained in piglets that were left to recover in a normoxic environment at 1 and 15 days.
Caspase-1 activity (in nmoles/mg protein/hour) at Normoxic (Nx), Hypoxic (Hx), and hypoxic pretreated with PP2 groups (Hx + PP2). Results are expressed as mean ± SD. In this graph we also include a forth group of normoxic piglets that were pretreated with PP2 (Nx*), in order to investigate the effects of Src kinase inhibition on caspase-1 activity under normoxic conditions. Caspase-1 activity increased immediately following hypoxia and this effect was maintained until 15 days. Administration of Src kinase inhibitor resulted in attenuation of caspase-1 activity following hypoxia acutely, but this effect was not maintained on day 1 and day 15. *P < 0.05, Hypoxic groups versus Hx + PP2 and Nx. Src kinase inhibition did not affect the baseline caspase-1 activity under normoxic conditions (P = NS)
Caspase-1 Expression
Levels of caspase-1 were determined by western blot and expressed as mean ± SD. In Fig. 2a immunoblotting of caspase-1 is demonstrated. Three bands are identified, one at 45 kDa corresponding to the precursor (unprocessed) caspase-1 and two at 10–12 kDa (Fig. 2a). The 20 kDa band (heavy chain), as expected, was not visualized. Both, a 45 kDa (p45) band for the precursor caspase-1 as well as the 10 kDa (p10) band as a marker of the activated molecule were analyzed (Fig. 2a, b). Oxygen deprivation induced an increase of the precursor of caspase-1 (P < 0.05). This effect was observed acutely and maintained at 1 and 15 days post hypoxia (Fig. 2b). The p45 density (OD x mm2) expressed as % of control was 94 ± 8 in Nx, 113 ± 6 in Hx, 112 ± 3 in Hx-day 1, 115 ± 8 in Hx-day 15. During hypoxia, there were no significant changes in the levels of β-actin that served as an internal control.
Immunoblotting was performed with an antibody specific for the p10 subunit of caspase-1. Three bands were identified, one at 45 kDa corresponding to the precursor (unprocessed) caspase-1 and two at 10-12 kDa [A]. The 20 kDa band (heavy chain) was not visualized. Levels of precursor Caspase-1 (p45) at Normoxic (Nx), Normoxic pretreated with PP2 (Nx*), Hypoxic (Hx), and hypoxic pretreated with PP2 (Hx + PP2) groups are shown [A, B]. Results are expressed as OD values as % of control (mean ± SD). In this figure also we include data from piglets that were left to recover after 1 h of hypoxia (for 1 day and for 15 days). There was an increased expression of pre-caspase-1 acutely after hypoxia that was maintained up to 15 days. Pre-treatment with a Src inhibitor (PP2) did not have any effect on the expression of caspase-1 either acutely or in the recovery period. *P < 0.05 Nx, Nx* versus the hypoxic groups, # P = NS Nx versus Nx*. The density ratios of the 10/12 kDa chains [p10/p12] are shown [C]. Results are expressed as median (25th, 75th IQR). The p10 subunit forms the active caspase-1 (p50) after combining with the 20 kDa (p20) in a 1:1 ratio. During this process a 12-kDa product of moderate activity is produced. In hypoxia the p10/p12 ratio is decreased versus the normoxia. In piglets after acute hypoxia that were pretreated with a Src kinase inhibitor (PP2) there was an increased ratio in p10/p12 when compared with hypoxic controls. These differences were not maintained in piglets during the recovery period. * P < 0.05 Nx versus Hypoxic groups, # P < 0.05 Hx + PP2 versus Hx
The 12 kDa band (p12) representing either a phosphorylated form of the p10 or an intermediate of the caspase-1 production was analyzed. Based on our observation that there were differences in the relative expression of p10 and p12 subunits among the groups, we calculated the density ratios of the p10/p12 as a possible marker of activation of caspase-1 (Fig. 2c). Results are reported as median with interquartile range [IQR: 25, 75th percentile] and represented as box plots, with boxes to symbolize the IQR. The density ratios of p10/p12 were 2.2 [1.3, 2.9] in Nx, 0.84 [0.8, 1.2] in Hx, 0.98 [0.9, 1.1] in Hx-day 1, 0.99 [0.87, 1.1] in Hx-day 15. The data show that p10/p12 is decreased during hypoxia when compared with normoxia (P < 0.05) and this difference persists in the recovery phase (day 1 and 15). There was no significant difference in the expression of either p10 or p12 bands if examined separately.
In piglets in the Hx + PP2 group, the expression of p45 was increased compared to Normoxia (P < 0.05). There was no effect of Src kinase inhibition on p45 expression either acutely or in the re-oxygenation period (P = NS). The p45 chain density (% of control) was 117 ± 5 in Hx + PP2, 118 ± 9 in Hx + PP2-day 1, 118 ± 8 in Hx + PP2-day 15. The expression of caspase-1 in normoxic piglets that were pretreated with PP2 (Nx*) was 90 ± 5 and did not differ when compared to the baseline (P = NS vs. Nx, P < 0.05 vs. Hypoxic groups). The p10/p12 ratio was increased in the Hx + PP2 group, 1.2 [1.1, 1.8] (P < 0.05 vs. Nx, Hx). The p10/p12 ratios were analyzed also in hypoxic piglets, pretreated with PP2, in the recovery phase (day 1, day 15) (P < 0.05 vs. Nx, NS vs. Hx). Pretreatment with PP2 did not affect the p10/p12 ratio under normoxic conditions. Our data show that in the acute phase, piglets that were pretreated with PP2 had higher p10/p12 ratios.
Interleukin 1 Beta (IL-1β)
IL-1β levels were determined by ELISA and results were expressed in pg/mL as mean ± SD. When compared to normoxia, there was no difference in the IL-1β levels of the untreated acute phase after hypoxia groups (Nx = 89 ± 34 and Hx = 77 ± 7; P = NS). IL-1β levels in the untreated Hx-day 1 group were increased when compared to both normoxia and hypoxia in the acute phase (Hx-day 1 = 139 ± 45; P < 0.05). IL-1β levels in the Hx-day 15 group was 90 ± 33, which was lower than in Hx-day 1 (P < 0.05), but there was no difference when compared to acute hypoxia or normoxia. In piglets pretreated with PP2, IL-1β levels were as follows: Hx + PP2 = 100 ± 24, Hx + PP2-day 1 = 102 ± 10, and Hx + PP2-day 15 = 81 ± 15 (P < 0.05 vs. Hx day 1, NS vs. Nx or Hx). IL-1β level was increased after hypoxia reaching a maximum at 24 h after the acute hypoxic insult. IL-β levels returned to baseline within 2 weeks (Fig. 3). In piglets that were pretreated with PP2, hypoxia did not induce an increase in IL-1β.
IL-1β levels were determined by ELISA and results were expressed in pg/mL (mean ± SD). IL-1β production is increased after hypoxia reaching a maximum at 24 h after the acute hypoxic insult. IL-1β levels returned to baseline within 2 weeks. In piglets that were pretreated with PP2, a Src kinase inhibitor, hypoxia did not induce an increase in IL-1β. *P < 0.05 Hx-1 day versus Hx + PP2 at 1 day
Discussion
In the current study we provide evidence that caspase-1 activation occurs immediately (within 1 h) after hypoxia while IL-1β production peaks at 24 h post hypoxia. We also show that caspase-1 activation persists for 15 days while IL-1β returns to baseline at 15 days after hypoxia. These molecular events are linked to cell death, as caspase-1 deficient mice, are resistant to hypoxia and ischemia [17]. IL-1β also has a direct neurotoxic effect on the white matter of the brain [5] and has been shown to induce apoptosis via the mitogen-activated protein kinase (MAPK) transduction pathway [18–20]. Caspase-1 activation is achieved with the production of complex intracellular structures, the inflammasomes and occurs through NLRs. The central nervous system can form at least 2 types of inflammasomes, designated as NLR1 and NLR3. Reactive oxygen species (ROS) provide an important link between hypoxia and inflammation and is considered as a prerequisite for the inflammasome activation [21]. Hypoxia induces mitochondrial complex III to produce ROS. ROS are sensed by NLR and activate the inflammasome [22]. In turn, high concentrations of ROS activate cellular protective mechanisms, such as hypoxia inducible factor [23, 24].
We investigated a possible link between the activation of inflammasomes and Src kinase after hypoxia. In our experiments the hypoxic groups that were not treated with the Src kinase inhibitor demonstrated higher levels of caspase-1 activity and IL-1β expression when compared to the treated groups. The role of Src kinase in the caspase-1 pathway has only recently started to be investigated. Src kinase plays an important role in the regulation of immunity and the inflammatory response [8, 9]. Bacterial or viral pathogens have been shown to cause a Src kinase mediated activation of the NLR3 inflammasome [25]. Interestingly, Src kinase mediated autophagy has been linked to E3 ubiquitin ligase (c-Cbl), which has been shown to provide a negative feedback to the production of Src kinase. Experiments that involved gene silencing of c-Cbl resulted in increased secretion of both IL-1β and IL-18 [26]. These results suggest a possible link of c-Cbl and Src kinase in the pathway that leads to inflammasome activation. Recently, Src Kinase has been shown to modulate caspase-1 activity in hippocampal neurons derived from mice. In these experiments, Src kinase deficient neurons exhibited significantly increased caspase-1 activity [27].
There is increasing experimental evidence that increased Src kinase activation is linked to apoptosis and cellular death [28, 29]. Src and Fyn knockdown cells are resistant to apoptosis after oxygen and glucose deprivation, demonstrating an involvement of Src kinase in neuronal cell apoptosis [30]. Interestingly in cellular cultures, Src kinase was found to inhibit the extrinsic pathway of apoptosis by a direct tyrosine phosphorylation of caspase–8 [14]. Similar results have been found in sepsis. Neutrophils from septic patients, when treated with PP2, developed increased apoptosis [31]. These results need careful interpretation, since they are derived from experiments that were performed in the cellular level rather than in whole tissue and the triggering stimuli were other than hypoxia. In our study we investigated if the hypoxia-induced activation of caspase–1 in the cerebral cortex was mediated by Src kinase. We have shown that by blocking the Src kinase the hypoxia induced inflammatory response was attenuated.
We provide evidence that inhibition of Src kinase in the acute phase after hypoxia involves changes in the relative production of caspase-1 subunits. Active caspase-1 consists of two polypeptides of 20 and 10 kDa (p20 and p10) associated in a 1:1 ratio, which are processed from an inactive cytoplasmic 45 kDa precursor (p45) [4, 32]. During this process autocatalysis occurs and fragments of different molecular weights (p35, p12) are produced until the final products (p20, p10) emerge [33]. In our study, the 12 kDa band could represent either a phosphorylated chain or the intermediate chain that is moderately active and is further processed to the fully active p10 subunit. We showed that under normoxic conditions there is an increased expression of p10 subunits when compared to p12. This ratio is reversed in hypoxic piglets (Fig. 2a, c). Src Kinase exerts a variety of biologic actions through tyrosine phosphorylation of key enzymatic pathways. It has been previously described that Src kinase mediates the increased tyrosine phosphorylation of caspase-9 and caspase-8 [8, 13, 14]. Src kinase has not been shown to interfere in a similar mechanism with the activation of caspase-1. It is possible that the p10 and p12 subunits represent a phosphorylated/dephosphorylated status of the light chain subunit. We found that under normoxia, dephosphorylated chains (p10) were increased in comparison with the phosphorylated chains (p12). Upon activation of caspase-1 in hypoxia, there was a quantitative increase in the phosphorylated (p12) subunits, which could be attributed to the concurrent activation of the Src kinase [12]. By blocking the Src kinase, we were able to restore the p10/p12 ratio, achieving levels similar to normoxia. In our experiments, Src kinase appears to interfere with this process in the acute phase only. Src kinase inhibition did not result in changes in the production of the precursor caspase-1 molecule, which could be regulated by different mechanisms.
In our experiments we used PP2, which creates a reversible, ATP-competitive inhibition of the Src (IC50 = 36 nM) [34]. PP2 does not affect significantly the EGFR kinase (IC50 = 480 nM), but does inhibit certain other cellular kinases [35, 36]. PP2 also exerts biologic actions and has been shown to induce apoptosis in cell cultures of rat cortical cells [37]. Although the mechanism is not clear it has been proposed that this occurs through interference with the function of NMDA receptor [11]. Src kinase plays a role in the phosphorylation of FAK–p85, a complex that regulates NMDA receptor activation by glutamate [38]. In our study, the activity of caspase-1 in normoxic piglets that were pretreated with PP2, was not significantly different than the activity in the control group.
We found that IL-1β production was increased after hypoxia, reaching a maximum level at 24 h and then returned to baseline by 15 days, following a different pattern of production than that of caspase-1. The timing of the activation of caspase-1 with production of IL-1β as end point after hypoxic insult is conflicting. When transient global ischemia was induced in rats by bilateral carotid artery occlusion, IL-1 mRNA in the brain increased within 15 min. This effect persisted for 7 days [39]. In other studies changes in IL-1β levels were not seen until 3–6 h post-occlusion and these changes did not involve all parts of the brain [40]. In a model of cardiac arrest, a prolonged increase of IL-1 in hippocampus was observed with a maximal level at 14 days. This increase was maintained for at least 28 days after injury [41]. Our experimental model is designed to evaluate the brain injury caused by hypoxia. During the period of hypoxia, we observed that there is a decrease of the blood pressure of about 40 % from baseline. Specifically within 20 min after the initiation of the experiment, the mean arterial blood pressure (as measured directly by an arterial catheter) was noted to fall to levels near 50 mmHg (Table 1). In newborn piglets under normoxic conditions, this level correlates with loss of auto-regulation [42]. This decrease of blood pressure could result in global ischemia, especially in lieu of hypoxia.
We found that caspase-1 remained activated at 15 days. IL-1β expression decreased to levels similar to baseline. These differences could be attributed to dynamic temporal changes in immune cells populations, after hypoxic-ischemic brain injury [43]. Changes in the inflammatory cells could result in different patterns of cytokine production overtime [44]. It is also possible that in the recovery phase the IL-1β is produced through a caspase-1 independent pathway. There is recent evidence that IL-1β can be activated via alternative routes. One of these caspase-1 independent pathways involves caspase-8. Caspase-8 was found to stimulate IL-1β in murine bone marrow derived dendritic cells stimulated by TLR4 agonists and chemotherapeutic drugs such as doxorubicin [45]. A caspase-1 intermediate (p12) also enhanced FAS-mediated apoptosis in part by activating caspase-8 [46], showing that there is a bidirectional connection in the functions of Caspase-1 and 8.
Conclusions
We have demonstrated involvement of Src kinase in the activation of the caspase-1/IL-1β pathway after hypoxia in the cortex of the brain of newborn piglets. Administration of PP2 prior to hypoxia prevented hypoxia-induced increased activity of caspase-1 at 1 hour and IL-1β expression at 24 h, but not long term (at 15 days). These changes could occur because of changes in the production or processing of the caspase-1 subunits (p10/p12). Our study suggests that Src kinase mediates hypoxia-induced caspase-1 activation, and that inhibition of Src kinase may attenuate the neuroinflammatory response that leads to delayed hypoxia-induced cell death following cerebral hypoxia.
Methods and Materials
Animal Experiments
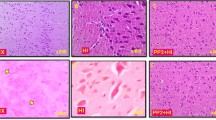
The experimental protocol had the approval of the Institutional Animal Care and Use Committee of Drexel University. Studies were conducted on anesthetized, ventilated 3–5 days old term newborn piglets. Piglets were divided into three groups: normoxic (Nx), hypoxic (Hx) and hypoxic pre-treated with Src kinase inhibitor PP2 (Hx + PP2) (acute phase). Piglets that were left to recover after hypoxia were followed, under normoxic conditions, for either 1 or 15 days (recovery). Five piglets were included in each group. We also included a forth group of normoxic piglets that were pretreated with PP2 (Nx*), in order to investigate the effects of Src kinase inhibition on caspase-1 activation under physiologic (normoxic) conditions. Anesthesia was induced with isoflurane and maintained with nitrous oxide and fentanyl (50 μg/kg, IV). Pancuronium (0.3 mg/kg, IV) was administered after placing the animal in pressure control ventilator. Core body temperature was maintained at 38.5–39.5 °C. After stabilization following surgery, the piglets assigned to the hypoxic group were exposed to hypoxia (FiO2 = 7 %) for 1 hour, while the piglets assigned to normoxia group were ventilated at FiO2 = 21 % for 1 hour. Piglets assigned to the Hx + PP2 group received the Src kinase inhibitor (PP2, 1 mg/kg, IV), 30 min prior to the hypoxic exposure. At the end of the study, the animal was sacrificed; cerebral cortex was removed and placed either in homogenization buffer for isolation of the cytosolic fraction or in liquid nitrogen and then stored at −80 °C for later biochemical studies. The post-hypoxia recovery animals were anesthetized and their brain was removed on day 1 and 15 of the recovery period for analysis.
Isolation of the Cytosolic Fraction
The cytosolic fraction of the cerebral tissue was isolated by homogenizing one gram of cerebral cortical tissue by a Dounce-type glass homogenizer. The homogenate was centrifuged at 1,000×g for 10 min 4 °C and then again at 15,000×g for 1 h at 4 °C. The supernatant was centrifuged at 100,000×g for 60 min 4 °C to obtain the cytosolic fraction.
Caspase-1
Cytosolic caspase-1 activity was determined in a medium containing 0.32 M sucrose, 10 mM Tris–HCl buffer (ph 7.0), 3 mM MgCl2, 500 μg cytosolic protein and 75 μΜ of a specific fluorogenic substrate for caspase-1 (Alexis Biochemicals, San Diego, Ca). The activity of caspase-1 was measured by spectrophotometry at 460 nm at 37 °C continuously for 400 s. The rate of reaction was measured and the activity was calculated using amino-4-methyl-coumarin as a standard.
The expression of pro- and caspase-1 chains was assessed by Western Blot analysis. Equal amount of each cytosolic sample was separated by 12 % sodium dodecyl sulphate-polyacrylamide gel electrophoresis (SDS-PAGE) and was transferred by electrophoresis to nitrocellulose membranes. The membranes were subsequently incubated with an anti- caspase-1 rabbit polyclonal antibody directed against the p10 subunit (Santa Cruz Biotechnology, Ca). Immunoreactivity was then detected by incubation with horseradish peroxidase conjugated anti-rabbit secondary antibody (Rockland, Gilbertsville, PA). Specific immunocomplexes were detected by chemiluminence method using the ECL detection system (GE Healthcare, Buckinghamshire, England). The bands were analyzed by imaging densitometry (GS-700 densitometer, Bio-Rad) and expressed as autoradiographic values (OD × mm2) per immunoblot protein. β-actin was used to verify homogenous loading transfer. The data were expressed as percent of a specific Normoxia sample.
IL-1β
Commercially available enzyme-linked immunosorbent assay kits (R&D Systems, Minneapolis, Minnesota) were used to measure IL-1β concentrations. Protein concentration was determined by Lowry et al. [47]. The cytosolic preparation was diluted to a final concentration of 200 μg protein/100 μl for all samples. An enzyme-linked polyclonal antibody specific for porcine IL-1β (mature molecule), was added to the wells as per manufacturer’s recommendations. The sample values were read off the standard curve. Results were reported as pg/ml.
Statistical Analysis
One-way analysis of variance was used for comparisons between the treatment groups at each time point. For post hoc analysis, the Holm–Sidak test was used. For non-parametric data, the Kruskal–Wallis analysis of variance on ranks was used. For post hoc analysis in these cases, the Newman–Keuls method was used. Values are presented as mean ± SD for normal distributions, or median with interquartile range (25–75 %) for skewed data. Statistical analysis was performed using Sigma Stat version 3.0 (Systat Software, San Jose, California).
Abbreviations
- IL-1β:
-
Interleukin 1 beta
- NMDA:
-
N-methyl-d-aspartate
- PP2:
-
4-Amino-5-(4-chlorophenyl)-7-(t-butyl) pyrazolo [3,4-d] pyrimidine
- NLR:
-
Nucleotide-binding oligomerization domain receptors
- SD:
-
Standard deviation
References
Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL (2007) Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med 13(7):851–856. doi:10.1038/nm1603
Gray PW, Glaister D, Chen E, Goeddel DV, Pennica D (1986) Two interleukin 1 genes in the mouse: cloning and expression of the cDNA for murine interleukin 1 beta. J Immunol 137(11):3644–3648
Fletcher DS, Agarwal L, Chapman KT, Chin J, Egger LA, Limjuco G, Luell S, MacIntyre DE, Peterson EP, Thornberry NA et al (1995) A synthetic inhibitor of interleukin-1 beta converting enzyme prevents endotoxin-induced interleukin-1 beta production in vitro and in vivo. J Interferon Cytokine Res 15(3):243–248
Thornberry NA, Bull HG, Calaycay JR, Chapman KT, Howard AD, Kostura MJ, Miller DK, Molineaux SM, Weidner JR, Aunins J et al (1992) A novel heterodimeric cysteine protease is required for interleukin-1 beta processing in monocytes. Nature 356(6372):768–774. doi:10.1038/356768a0
Wang CX, Shuaib A (2002) Involvement of inflammatory cytokines in central nervous system injury. Prog Neurobiol 67(2):161–172
Monack DM, Raupach B, Hromockyj AE, Falkow S (1996) Salmonella typhimurium invasion induces apoptosis in infected macrophages. Proc Natl Acad Sci USA 93(18):9833–9838
Salter MW, Kalia LV (2004) Src kinases: a hub for NMDA receptor regulation. Nat Rev Neurosci 5(4):317–328. doi:10.1038/nrn1368
Boateng LR, Cortesio CL, Huttenlocher A (2012) Src-mediated phosphorylation of mammalian Abp1 (DBNL) regulates podosome rosette formation in transformed fibroblasts. J Cell Sci 125(Pt 5):1329–1341. doi:10.1242/jcs.096529
Gatesman A, Walker VG, Baisden JM, Weed SA, Flynn DC (2004) Protein kinase Calpha activates c-Src and induces podosome formation via AFAP-110. Mol Cell Biol 24(17):7578–7597. doi:10.1128/MCB.24.17.7578-7597.2004
Kuo WL, Chung KC, Rosner MR (1997) Differentiation of central nervous system neuronal cells by fibroblast-derived growth factor requires at least two signaling pathways: roles for Ras and Src. Mol Cell Biol 17(8):4633–4643
Wang YT, Salter MW (1994) Regulation of NMDA receptors by tyrosine kinases and phosphatases. Nature 369(6477):233–235. doi:10.1038/369233a0
Mishra OP, Ashraf QM, Delivoria-Papadopoulos M (2009) NO-mediated activation of Src kinase during hypoxia in the cerebral cortex of newborn piglets. Neurosci Lett 460(1):61–65. doi:10.1016/j.neulet.2009.05.041
Mishra OP, Delivoria-Papadopoulos M (2010) Mechanism of tyrosine phosphorylation of procaspase-9 and Apaf-1 in cytosolic fractions of the cerebral cortex of newborn piglets during hypoxia. Neurosci Lett 480(1):35–39. doi:10.1016/j.neulet.2010.05.081
Cursi S, Rufini A, Stagni V, Condo I, Matafora V, Bachi A, Bonifazi AP, Coppola L, Superti-Furga G, Testi R, Barila D (2006) Src kinase phosphorylates Caspase-8 on Tyr380: a novel mechanism of apoptosis suppression. EMBO J 25(9):1895–1905. doi:10.1038/sj.emboj.7601085
Bossenmeyer-Pourie C, Koziel V, Daval JL (2000) Involvement of caspase-1 proteases in hypoxic brain injury. Effects of their inhibitors in developing neurons. Neuroscience 95(4):1157–1165
Kim NG, Lee H, Son E, Kwon OY, Park JY, Park JH, Cho GJ, Choi WS, Suk K (2003) Hypoxic induction of caspase-11/caspase-1/interleukin-1beta in brain microglia. Brain Res Mol Brain Res 114(2):107–114
Liu XH, Kwon D, Schielke GP, Yang GY, Silverstein FS, Barks JD (1999) Mice deficient in interleukin-1 converting enzyme are resistant to neonatal hypoxic-ischemic brain damage. J Cereb Blood Flow Metab 19(10):1099–1108. doi:10.1097/00004647-199910000-00006
Dimmeler S, Haendeler J, Nehls M, Zeiher AM (1997) Suppression of apoptosis by nitric oxide via inhibition of interleukin-1beta-converting enzyme (ICE)-like and cysteine protease protein (CPP)-32-like proteases. J Exp Med 185(4):601–607
Kofler S, Nickel T, Weis M (2005) Role of cytokines in cardiovascular diseases: a focus on endothelial responses to inflammation. Clin Sci 108(3):205–213. doi:10.1042/CS20040174
Cuenda A, Rousseau S (2007) p38 MAP-kinases pathway regulation, function and role in human diseases. Biochim Biophys Acta 1773(8):1358–1375. doi:10.1016/j.bbamcr.2007.03.010
Tschopp J (2011) Mitochondria: sovereign of inflammation? Eur J Immunol 41(5):1196–1202. doi:10.1002/eji.201141436
Zhou R, Yazdi AS, Menu P, Tschopp J (2011) A role for mitochondria in NLRP3 inflammasome activation. Nature 469(7329):221–225. doi:10.1038/nature09663
Chandel NS, McClintock DS, Feliciano CE, Wood TM, Melendez JA, Rodriguez AM, Schumacker PT (2000) Reactive oxygen species generated at mitochondrial complex III stabilize hypoxia-inducible factor-1alpha during hypoxia: a mechanism of O2 sensing. J Biol Chem 275(33):25130–25138. doi:10.1074/jbc.M001914200
Guzy RD, Hoyos B, Robin E, Chen H, Liu L, Mansfield KD, Simon MC, Hammerling U, Schumacker PT (2005) Mitochondrial complex III is required for hypoxia-induced ROS production and cellular oxygen sensing. Cell Metab 1(6):401–408. doi:10.1016/j.cmet.2005.05.001
Kankkunen P, Valimaki E, Rintahaka J, Palomaki J, Nyman T, Alenius H, Wolff H, Matikainen S (2014) Trichothecene mycotoxins activate NLRP3 inflammasome through a P2X7 receptor and Src tyrosine kinase dependent pathway. Hum Immunol 75(2):134–140. doi:10.1016/j.humimm.2013.11.010
Sandilands E, Serrels B, McEwan DG, Morton JP, Macagno JP, McLeod K, Stevens C, Brunton VG, Langdon WY, Vidal M, Sansom OJ, Dikic I, Wilkinson S, Frame MC (2012) Autophagic targeting of Src promotes cancer cell survival following reduced FAK signalling. Nat Cell Biol 14(1):51–60. doi:10.1038/ncb2386
Chong ZZ, Lin SH, Kang JQ, Maiese K (2003) The tyrosine phosphatase SHP2 modulates MAP kinase p38 and caspase 1 and 3 to foster neuronal survival. Cell Mol Neurobiol 23(4–5):561–578
Jiang X, Mu D, Biran V, Faustino J, Chang S, Rincon CM, Sheldon RA, Ferriero DM (2008) Activated Src kinases interact with the N-methyl-D-aspartate receptor after neonatal brain ischemia. Ann Neurol 63(5):632–641. doi:10.1002/ana.21365
Knox R, Zhao C, Miguel-Perez D, Wang S, Yuan J, Ferriero D, Jiang X (2013) Enhanced NMDA receptor tyrosine phosphorylation and increased brain injury following neonatal hypoxia-ischemia in mice with neuronal Fyn overexpression. Neurobiol Dis 51:113–119. doi:10.1016/j.nbd.2012.10.024
Du CP, Tan R, Hou XY (2012) Fyn kinases play a critical role in neuronal apoptosis induced by oxygen and glucose deprivation or amyloid-beta peptide treatment. CNS Neurosci Ther 18(9):754–761. doi:10.1111/j.1755-5949.2012.00357.x
Jia SH, Parodo J, Kapus A, Rotstein OD, Marshall JC (2008) Dynamic regulation of neutrophil survival through tyrosine phosphorylation or dephosphorylation of caspase-8. J Biol Chem 283(9):5402–5413. doi:10.1074/jbc.M706462200
Ayala JM, Yamin TT, Egger LA, Chin J, Kostura MJ, Miller DK (1994) IL-1 beta-converting enzyme is present in monocytic cells as an inactive 45-kDa precursor. J Immunol 153(6):2592–2599
Yamin TT, Ayala JM, Miller DK (1996) Activation of the native 45-kDa precursor form of interleukin-1-converting enzyme. J Biol Chem 271(22):13273–13282
Kraker AJ, Hartl BG, Amar AM, Barvian MR, Showalter HD, Moore CW (2000) Biochemical and cellular effects of c-Src kinase-selective pyrido[2, 3-d]pyrimidine tyrosine kinase inhibitors. Biochem Pharmacol 60(7):885–898
Bain J, Plater L, Elliott M, Shpiro N, Hastie CJ, McLauchlan H, Klevernic I, Arthur JS, Alessi DR, Cohen P (2007) The selectivity of protein kinase inhibitors: a further update. Biochem J 408(3):297–315. doi:10.1042/BJ20070797
Brandvold KR, Steffey ME, Fox CC, Soellner MB (2012) Development of a highly selective c-Src kinase inhibitor. ACS Chem Biol 7(8):1393–1398. doi:10.1021/cb300172e
Takadera T, Fujibayashi M, Koriyama Y, Kato S (2012) Apoptosis induced by SRC-family tyrosine kinase inhibitors in cultured rat cortical cells. Neurotox Res 21(3):309–316. doi:10.1007/s12640-011-9284-5
Crossthwaite AJ, Valli H, Williams RJ (2004) Inhibiting Src family tyrosine kinase activity blocks glutamate signalling to ERK1/2 and Akt/PKB but not JNK in cultured striatal neurones. J Neurochem 88(5):1127–1139
Minami M, Kuraishi Y, Yabuuchi K, Yamazaki A, Satoh M (1992) Induction of interleukin-1 beta mRNA in rat brain after transient forebrain ischemia. J Neurochem 58(1):390–392
Saito K, Suyama K, Nishida K, Sei Y, Basile AS (1996) Early increases in TNF-alpha, IL-6 and IL-1 beta levels following transient cerebral ischemia in gerbil brain. Neurosci Lett 206(2–3):149–152
Orzylowska O, Oderfeld-Nowak B, Zaremba M, Januszewski S, Mossakowski M (1999) Prolonged and concomitant induction of astroglial immunoreactivity of interleukin-1beta and interleukin-6 in the rat hippocampus after transient global ischemia. Neurosci Lett 263(1):72–76
Laptook A, Stonestreet BS, Oh W (1982) Autoregulation of brain blood flow in the newborn piglet: regional differences in flow reduction during hypotension. Early Hum Dev 6(1):99–107
Winerdal M, Winerdal ME, Kinn J, Urmaliya V, Winqvist O, Aden U (2012) Long lasting local and systemic inflammation after cerebral hypoxic ischemia in newborn mice. PLoS One 7(5):e36422. doi:10.1371/journal.pone.0036422
Hedtjarn M, Mallard C, Hagberg H (2004) Inflammatory gene profiling in the developing mouse brain after hypoxia-ischemia. J Cereb Blood Flow Metab 24(12):1333–1351. doi:10.1097/01.WCB.0000141559.17620.36
Antonopoulos C, El Sanadi C, Kaiser WJ, Mocarski ES, Dubyak GR (2013) Proapoptotic chemotherapeutic drugs induce noncanonical processing and release of IL-1beta via caspase-8 in dendritic cells. J Immunol 191(9):4789–4803. doi:10.4049/jimmunol.1300645
Tatsuta T, Shiraishi A, Mountz JD (2000) The prodomain of caspase-1 enhances Fas-mediated apoptosis through facilitation of caspase-8 activation. J Biol Chem 275(19):14248–14254
Lowry OR, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with Folin phenol reagent. J Biol Chem 32:265–275
Acknowledgments
We gratefully acknowledge Dr. Qazi Ashraf for his technical assistance and Dr. Jane McGowan, who carefully read and revised this manuscript.
Conflict of interest
The authors declare that they have no competing financial interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angelis, D., Fontánez-Nieves, T.D. & Delivoria-Papadopoulos, M. The Role of Src Kinase in the Caspase-1 Pathway After Hypoxia in the Brain of Newborn Piglets. Neurochem Res 39, 2118–2126 (2014). https://doi.org/10.1007/s11064-014-1404-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-014-1404-1